Abstract
The data combine objectively measured sleep and thrice-daily salivary cortisol collected from a four-day diary study in a large Midwestern city with location data on all violent crimes recorded during the same time period for N=82 children (mean age=14.90; range=11.27 to 18.11). The primary empirical strategy uses a within-person design to measure the change in sleep and cortisol from the person’s typical pattern on the night/day immediately following a local violent crime. On the night following a violent crime, children have later bedtimes. Children also have disrupted cortisol patterns the following morning. Supplementary analyses using varying distances of the crime to the child’s home address confirm more proximate crimes correspond to later bedtimes.
Keywords: violent crime, neighborhood violence, sleep
Children exposed to recent incidents of local violence perform worse on assessments of academic skills, executive function, and effortful control, relative to children from the same or similar neighborhoods who were not recently exposed to violence (Gershenson & Tekin, 2015; Sharkey, 2010; Sharkey, Tirado-Strayer, Papachristos, & Raver, 2012). Despite evidence that violence has an acute, causal impact on academic performance, the mechanisms explaining how environmental stressors get “under the skin” or “into the minds” of children have received little attention. This study examines two potential causal pathways that might explain the effects of acute violent crime: sleep and the hypothalamic-pituitary-adrenal (HPA) axis.
Sleep is a stress-sensitive system (Hicken, Lee, Ailshire, Burgard, & Williams, 2013; Sadeh, 1996). Under the opponent processes model of sleep, individuals must suspend arousal to transition from wakefulness to sleep (Edgar, Dement, & Fuller, 1993). Crime may affect sleep through heightened vigilance arising from fear or stress, or through noise and disruption from gunfire, shouting, and expanded police presence (Dahl, 1996; Hale et al., 2013; Lacoe & Sharkey, 2016). Insufficient sleep is associated with greater fatigue, more difficulty concentrating, and reduced executive functioning (Alapin et al., 2000; Sadeh, Gruber, & Raviv, 2003; Talbot, McGlinchey, Kaplan, Dahl, & Harvey, 2010).
Stress exposure can also affect the HPA axis, a key biological stress response system, and its primary hormonal product, cortisol. Cortisol levels follow a predictable daily pattern. A sharp increase in cortisol about 30 minutes after waking is called the cortisol awakening response, or CAR (Pruessner et al., 1997). Normally, the CAR assists in the transition from sleep to waking and may provide a boost to help meet the expected demands of the upcoming day (Adam, Hawkley, Kudielka, & Cacioppo, 2006; Clow, Hucklebridge, Stalder, Evans, & Thorn, 2010; Fries, Dettenborn, & Kirschbaum, 2009; Vrshek-Schallhorn et al., 2012). Following the CAR, basal activity of the HPA axis typically decreases during waking hours, reaching the lowest levels shortly after sleep begins (Adam et al., 2006).
Stress exposure can change typical diurnal cortisol patterns (Adam, 2012; Sapolsky, Romero, & Munck, 2000). Acute stress is associated with an elevated CAR, with more chronic stress and burnout associated with a blunted CAR (Chida & Steptoe, 2009). High daily stress is associated with low waking cortisol, a low CAR, slower memory speed, and reduced attention continuity (Maldonado et al., 2008).
Although exposure to traumatic events such as hurricanes is associated with long-term changes to sleep and the HPA axis (Lavie, 2001; Vigil, Geary, Granger, & Flinn, 2010), it is unclear whether somewhat more common stressors such as violent crime have similar effects. To our knowledge this is the first study examining the short-term effects of proximity to nearby violent crime on sleep and cortisol.
Our primary empirical strategy uses a within-person design. It measures the change in sleep or cortisol on the night and morning immediately following a local violent crime, relative to that same person’s typical pattern. Because the comparison occurs within individuals, any changes to the outcomes cannot be caused by characteristics that are constant for a person (e.g., neighborhood quality). The important assumption in the design is that, within a given person, the timing of violent crime is random with respect to the timing of the diary study. Exogenous variation in the timing of local crime allows for causal inference.
Methods
Participants
The present study involves a sample of 82 adolescents (49% female) who participated in a take-home diary study in a large Midwestern city in fall 2012. Diary subjects were drawn from participants of a larger study of adolescent stress (N=379) submitted through the DePaul University and Northwestern University Institutional Review Boards. Adolescents were recruited through three public schools selected for having racially, ethnically, and socioeconomically diverse student bodies drawn from across the city. Information about the study was presented orally and in writing to potential participants during homeroom or lunch periods at their school. Parents were informed about the study at parent meetings, at report card pick-up days, and through parent consent forms. Parents were invited to contact the final author and/or school administrators if they had questions and/or wished to see copies of the measures. Participants with parental consent completed assent forms before data collection.
A sub-sample of 138 adolescents participated in the take-home diary study, including 94 adolescents who also received activity-tracking watches. One adolescent did not return a watch and 11 watches contained no usable data, leaving 82 adolescents with at least one full night of sleep data. We obtained 87% of four expected nights of sleep data from the 82 adolescents. The mean age was 14.90 (SD=1.87, range=11.27 to 18.11), with 17% of participants identifying as black (n=14), 20% identifying as Hispanic white (n=16), 18% identifying as non-Hispanic white (n=15), 27% identifying as multi-ethnic (n=22), and the remainder identifying as another category or missing race information. Table 1 provides descriptive statistics. Table 2 provides a correlation matrix.
Table 1.
Descriptive Statistics
| Mean | SD | Minimum | Maximum | Weekday Cronbach’s Alpha |
N | |
|---|---|---|---|---|---|---|
| Black | 0.17 | 0.38 | 0.00 | 1.00 | 82 | |
| Hispanic white | 0.20 | 0.40 | 0.00 | 1.00 | 82 | |
| Non-Hispanic white | 0.18 | 0.39 | 0.00 | 1.00 | 82 | |
| Multiethnic | 0.27 | 0.45 | 0.00 | 1.00 | 82 | |
| Other | 0.18 | 0.39 | 0.00 | 1.00 | 82 | |
| Age | 14.90 | 1.86 | 11.27 | 18.11 | 82 | |
| Male | 0.51 | 0.50 | 0.00 | 1.00 | 82 | |
| Violent crime ever=1 | 0.51 | 0.50 | 0.00 | 1.00 | 82 | |
| Mean bedtime | 23.12 | 1.07 | 20.17 | 26.12 | 0.72 | 82 |
| Mean latency | 0.43 | 0.47 | 0.04 | 3.03 | 0.44 | 82 |
| Mean sleep duration | 6.54 | 0.87 | 3.98 | 9.13 | 0.61 | 82 |
| Mean wake time | 7.00 | 0.98 | 4.89 | 10.33 | 0.76 | 82 |
| Mean waking cortisol | 0.27 | 0.19 | 0.01 | 1.48 | 0.88 | 76 |
| Mean CAR | 0.12 | 0.17 | −0.23 | 0.65 | 0.53 | 74 |
| Mean bedtime cortisol | 0.07 | 0.07 | 0.00 | 0.37 | 0.66 | 76 |
Sleep outcomes measured in hours. Cortisol outcomes measured in µg/dl. Includes Cronbach’s alpha of outcome measures during the week.
Table 2.
Correlation Matrix for Outcome Measures
| Bedtime | Latency | Sleep duration |
Wake time |
Bedtime cortisol |
Waking cortisol |
CAR | |
|---|---|---|---|---|---|---|---|
| Bedtime | 1.000 | ||||||
| Latency | −0.261 | 1.000 | |||||
| Sleep duration | −0.672 | −0.106 | 1.000 | ||||
| Wake time | 0.303 | 0.073 | 0.328 | 1.000 | |||
| Bedtime cortisol | −0.073 | 0.066 | 0.002 | 0.074 | 1.000 | ||
| Waking cortisol (next day) | −0.112 | 0.056 | 0.206 | 0.227 | 0.222 | 1.000 | |
| CAR | 0.145 | −0.230 | −0.204 | −0.235 | −0.154 | −0.457 | 1.000 |
Correlations between outcomes measured in the main analysis. Note that some measures are mathematically related to each other.
Measures
Sleep
Adolescents participated in one of six collection periods in fall 2012. Participants wore an Actiwatch-64 (Mini-Mitter Respironics, Inc.) for four consecutive nights to objectively measure sleep. Each period began on a Saturday. Participants were instructed to register bedtime and wake time by pressing a button on the Actiwatch immediately before they went to bed and immediately after they woke up, respectively. These timestamps were cross-checked using adolescent self-report diaries. The validated Actiware Sleep software (version 3.4, Mini-Mitter/Philips Respironics) calculated various sleep parameters using 1-minute epochs, based on significant movement after at least 10 min of inactivity (Oakley, 1997).
The software calculated sleep measures including bedtime (time when adolescent got into bed; mean=11:07 PM), sleep latency (lag from bedtime to sleep onset; mean=26 minutes), wake time (time at which the adolescent woke up for the last time in the morning; mean=7:00 AM), and sleep duration (time actually spent asleep from sleep onset to final waking; mean=6.54 hours). Adolescents completed a make-up day on Wednesday night if they missed a day of data collection. The adolescents had a mean of 3.4 nights of data out of an expected 4 nights.
Cortisol
Participants collected three salivary cortisol samples (immediately after waking, 30 minutes after waking, and at bedtime) each day for three consecutive days (typically Sunday, Monday, and Tuesday) during the same period as the sleep study. They also collected an evening sample on Saturday and wake and 30 minutes post-awakening samples on the final day (typically Wednesday). Participants used a passive drool technique by which they expressed unstimulated saliva through a small straw into a vial. Participants watched a saliva sample demonstration prior to the study and received reminder calls from the research team during the data collection to ensure they followed the protocol. Participants were instructed to avoid eating, drinking, and brushing their teeth 30 minutes prior to each sample collection. A kitchen timer pre-set to 30 minutes was provided to aid in the timing of the second daily sample. Participants were instructed to refrigerate their samples as soon as possible after collection. Most samples were taken at home and thus immediately refrigerated. Adolescents returned their samples to school at the end of the study week, at which point the research team paid the participants. Six of the 82 sleep participants returned no usable saliva samples, leaving N=76 cortisol participants. Cortisol participants completed 91% of expected samples. Samples were stored at −20°C before shipment to Trier, Germany, where they were assayed in duplicate using time-resolved fluorescent-detection immunoassay (Dressendörfer, Kirschbaum, Rohde, Stahl, & Strasburger, 1992).
Measures included waking cortisol (cortisol level at wake; mean=0.27 µg/dl; mean samples per person=3.7 out of an expected 4), CAR (increase from waking measurement to the measure occurring about 30 minutes later; mean=0.12 µg/dl; 3.2 of 4), and bedtime cortisol (cortisol level at bedtime; mean=0.07 µg/dl; 3.7 of 4). Analyses dropped any CAR samples taken more than 60 or less than 15 minutes after the waking sample. All 76 cortisol participants had at least one morning and bedtime sample, and 74 participants had data to calculate at least one CAR.
Violent crime
Crime data were obtained from a geocoded file identifying the date and location of every violent crime reported to the city police department. We created an indicator variable equal to one if a violent crime occurred in a participant’s home police beat in a given day, from midnight to midnight. Police beats are sub-divisions of police districts that represent areas that officers can patrol by foot. Our city is divided into over 250 police beats. We had 80 instances of violent crime (43 assaults, 31 robberies, 4 criminal sexual assaults, and 2 homicides) in a participant’s beat from Saturday through Wednesday of the study, with 51% of adolescents (N=42) having at least one crime in their beat during their participation period. For sensitivity analyses, exact distances between participants’ addresses and crime locations were calculated.
Empirical Strategy
Our analysis uses individual fixed effects to measure the change in outcome from the person’s typical pattern on the day following a local violent crime, as follows:
where Yit is the adolescent’s objectively measured sleep or cortisol on a given day, Crimeit is an indicator for whether crime occurred the preceding day, νt is a fixed effect for the day of the week, γi is an individual fixed effect, and εit is an idiosyncratic error term. The parameter of interest is β; it captures the causal effect of exposure to crime on the outcome. The inclusion of individual fixed effects enables us to compare sleep and cortisol outcomes for the same adolescent in a day with proximity to crime relative to a day without proximity to crime. Only those adolescents who experience a nearby crime during the study period contribute to this estimate (N=42). We control for day of the week to account for daily differences in sleep and cortisol patterns; participants with and without local violent crime contribute to this estimate. All standard errors are robust and clustered within individuals. We examine outcomes described in the measures section in separate analyses.
Additional analyses add indicators for two and three days after the violent crime to measure the persistence of changes in the response to the acute crime event. We add an indicator for the day before a violent crime as a placebo test: outcomes should not change in anticipation of a crime occurring the following day.
We also separate the analysis by type of violent crime (robbery, assault, criminal sexual assault, and homicide) to test whether responses differ by severity of crime. This analysis should be interpreted cautiously given the low N for certain types of crime. We also examine whether using distance cutoffs rather than an indicator for crime within a police beat provides similar estimates.
Results
Sleep
Table 3 displays the sleep results. Because some measures are mechanically related to each other, these should be viewed as related outcomes rather than independent tests. From Panel A, adolescents had significantly later bedtime (by 26 minutes, p=0.043) on evenings immediately following a violent crime in their police beat, relative to their typical bedtime, controlling for day of the week. A robustness check tested whether weekends (defined as Saturday night sleep) drove the results. When running the same estimate but excluding weekend sleep, the estimated bedtime effect was 38 minutes later (p=0.027). The standard error was also larger, at least partly because the number of observations dropped from 281 to 211. This estimate did not statistically differ from the estimate including weekends.
Table 3.
Effect of Acute Violence on Sleep Measures
| Bedtime | Latency | Sleep Duration |
Wake Time |
|
|---|---|---|---|---|
| Panel A: Overall Violent Crime | ||||
| Crime | 0.438* | 0.017 | −0.293 | 0.176 |
| (0.213) | (0.067) | (0.259) | (0.195) | |
| Panel B: Type of Violent Crime | ||||
| Assault | 0.645* | −0.062 | −0.429 | 0.129 |
| (0.312) | (0.080) | (0.377) | (0.248) | |
| Criminal Sexual | 0.686 | 0.499* | −1.042** | 0.050 |
| Assault | (1.075) | (0.220) | (0.327) | (0.223) |
| Homicide | 1.811*** | −0.053 | −1.138*** | 0.242 |
| (0.198) | (0.090) | (0.257) | (0.206) | |
| Robbery | 0.164 | 0.073 | −0.073 | 0.235 |
| (0.272) | (0.107) | (0.260) | (0.254) | |
|
| ||||
| N Adolescents | 82 | 82 | 82 | 82 |
| Observations | 281 | 281 | 281 | 281 |
p < 0.05,
p < 0.01,
p < 0.001
Robust standard errors clustered at the individual level and included in parentheses. Models include individual and day of the week fixed effects. Outcomes measured in hours. Bedtime defined as time when adolescent got into bed, sleep latency defined as lag from bedtime to sleep onset, wake time defined as time at which the adolescent woke up for the last time in the morning, and sleep duration defined as time actually spent asleep from sleep onset to final waking.
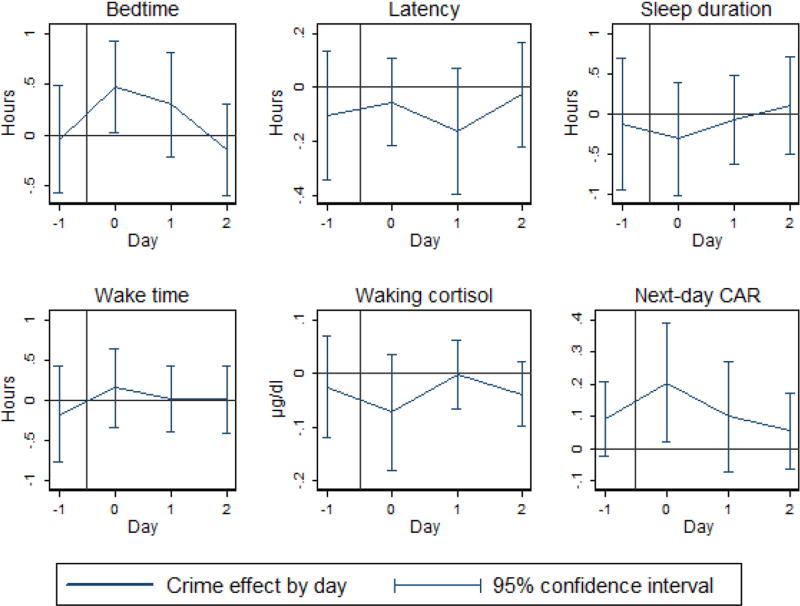
The first four panels of Figure 1 display the effects of violent crime on sleep for days subsequent and prior to acute crime. Each chart was derived from a regression that included interactions between lagged indicators for whether a crime occurred within an individual’s police beat during a given day, as well as individual and day-of-the-week fixed effects. Participants’ bedtime increased on the night immediately following a crime (p-value=0.041), but the effect dissipated by the second night. Day −1 tested a placebo: sleep should not have changed in anticipation of a crime occurring the following day. We found no evidence of an effect in the placebo days or for any of the other outcomes on any day.
Fig. 1.
Effect of crime on sleep and cortisol by day relative to an acute crime event (vertical line). Each chart is derived from a regression that includes interactions between lagged indicators for whether a crime occurred within an individual’s police beat during a given time period. All regressions include individual and day-of-the-week fixed effects. Includes 95% confidence intervals.
Panel B in Table 3 displays the analysis by type of crime. Results should be interpreted with caution, given the small number of severe crimes (especially homicide and criminal sexual assault) during the study. Homicide generated the strongest effect on sleep: bedtime increased by 1.81 hours (p=0.000) and total sleep decreased by 1.14 hours (p=0.000). Criminal sexual assault had a large effect on sleep latency (increased by 29 minutes, p=0.026) and total sleep (decreased by 1.04 hours, p=0.002). Coefficients for assault were generally large relative to Panel A, but the standard errors were large. Specifically, bedtime increased by 39 minutes (p=0.042). Effects for robbery were never statistically significant. As a check, we removed robbery from the Panel A estimate. This check resulted in larger estimated effects, but also larger standard errors for bedtime (estimated at 39 minutes, p=0.030). The other estimates remained null.
In separate analyses, we tested whether adolescents who resided in high-crime areas were more sensitive to local violence. We defined high-crime areas as those that had an above-median number of violent crimes in their police beat in the months of the study. When we interacted acute exposure to crime (Crimeit) with residence in high-crime areas, we found no difference in the estimated change in sleep across adolescents living in high- and low-crime areas. Given the small sample size, this test should be interpreted with caution.
Cortisol
Next, we reviewed the effects of violent crime on same-night bedtime, next-day waking, and next-day CAR cortisol measures (Table 4). We found a 0.13 µg/dl increase in next-day CAR in Panel A, representing a 111% increase over the mean CAR (p=0.025). We found no effects for other cortisol outcomes. Robustness checks that dropped two CAR outliers, controlled for prior night sleep and wake time, or excluded weekends (defined as Sunday morning) did not substantially change the results.
Table 4.
Effect of Acute Violence on Cortisol Measures
| Same-day Bedtime Cortisol |
Next-day Waking Cortisol |
Next-day CAR |
|
|---|---|---|---|
| Panel A: Overall Violent Crime | |||
| Crime | 0.005 | −0.048 | 0.133* |
| (0.019) | (0.038) | (0.058) | |
| Panel B: Type of Violent Crime | |||
| Assault | −0.019 | −0.085+ | 0.221* |
| (0.028) | (0.044) | (0.085) | |
| Criminal Sexual | 0.177* | 0.056 | 0.190 |
| Assault | (0.069) | (0.119) | (0.119) |
| Homicide | 0.033+ | −0.038 | 0.453*** |
| (0.018) | (0.057) | (0.076) | |
| Robbery | 0.019 | −0.020 | 0.019 |
| (0.023) | (0.041) | (0.051) | |
|
| |||
| N Adolescents | 76 | 76 | 74 |
| Observations | 283 | 281 | 244 |
p < 0.10,
p < 0.05,
p < 0.001
Robust standard errors clustered at the individual level and included in parentheses. Models include individual and day of the week fixed effects. Outcomes measured in µg/dl.
The final two panels of Figure 1 display cortisol effects over time. Each chart was derived from a regression that included interactions between lagged indicators for whether a crime occurred within an individual’s police beat during a given time period, as well as individual and day-of-the-week fixed effects. The effect was limited to the CAR on the day following violent crime (p=0.032), and effects dissipated by the next day. As in the sleep panels in Figure 1, prior-day placebo tests did not show anticipatory effects.
Panel B of Table 4 separates crime by type. Homicide was associated with the largest effects, with a 0.45 µg/dl increase in CAR the day following a homicide, relative to an individual’s typical CAR (p=0.000). Same-night cortisol also increased by a marginally significant 0.03 µg/dl (p=0.80). Assault was associated with a 0.22 µg/dl increase in CAR (p=0.011) and a marginally significant 0.09 µg/dl decrease in waking cortisol (p=0.059). Criminal sexual assault was associated with a 0.18 µg/dl increase in cortisol on the night of the crime (p=0.012). Effects for robbery were never statistically significant. Removing robbery from the Panel A estimate resulted in a larger coefficient for the effect on CAR (estimated at 0.22 µg/dl, p=0.003).
Sensitivity to Distance of Crime from Home
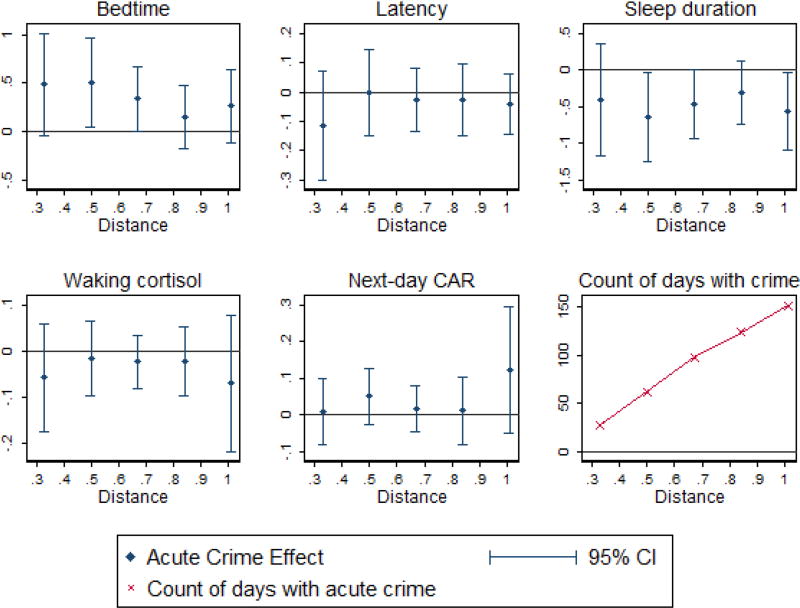
Our primary analyses used police beats as measures of local neighborhoods, as they account for local landmarks and roads that separate different localities. Here, we consider a violent crime as local if it occurred within various distance cutoffs from a participant’s home (see Figure 2; range=0.33 to 1.00 miles). Each line represents the estimated coefficient from a separate regression. The figure includes five outcomes: bedtime, sleep latency, sleep duration, next-day waking cortisol, and next-day CAR.
Fig. 2.
Effect of acute violent crimes on bedtime, sleep latency, and sleep duration (in hours) and next-day morning cortisol and CAR (in µg/dl) by various crime distance cutoffs, relative to days without crime within the distance cutoff. Each line represents a separate regression that includes individual and day-of-the-week fixed effects. Includes 95% confidence intervals. Also displays a count of individual study-days with a crime for each distance; as the radius expands the count increases.
More proximate crimes were necessarily rarer and generally had larger standard errors. Forty percent of adolescents experienced a violent crime within 0.33 miles of their home during their study participation, while the rate was 67% by 0.50 miles.
Coefficients were generally farther from zero at closer cutoffs. A violent crime within a half mile of an adolescent’s home (equivalent to four city blocks) corresponded to a 30 minute increase in bedtime (p=0.036), null effects for latency and wake time, and a 39 minute decrease in sleep duration (p=0.043). There were no consistent cortisol effects using the distance measure.
Discussion
We explored the relation between an acute external stressor (prior-day local violent crime) and two stress-responsive systems: sleep and the HPA axis. There were nearly 1.2 million violent crimes in the United States in 2015 (U.S. Department of Justice, 2016). Crimes may affect victims, but our study indicates that they may also affect nearby residents. Local prior-day violence disrupted sleep and increased next-day CAR. We argue that our findings are causal because, within a person, whether local violent crime happens to occur on a given day in our study is random from the perspective of each participant.
The effects on sleep and the CAR were generally large for homicide, moderate for assault, and null for robbery. These patterns could occur either because adolescents reacted more strongly to more violent crime, or because news of such crimes spread more prominently through social networks, media, or police presence. The analysis by type of crime should be interpreted cautiously, given the low number of participants who experienced local criminal sexual assault or homicide in this study.
Estimated effect sizes for sleep were generally larger for more proximate crimes; such crimes may be more likely to be communicated or even directly overheard. The effects for CAR were not statistically significant across distance measures, making these results less robust than the sleep analyses. This difference may be partially related to differences in reliability across measures; the Cronbach’s alpha for CAR was 0.53, compared to 0.72 for bedtime.
Many of our estimates were not statistically significant. Latency did not change following a crime, perhaps because the students went to bed later. Wake time increased by a statistically insignificant 11 minutes. Inflexible school start times may prevent adolescents from adjusting their wake time. We predicted an increase in same-day bedtime cortisol and a decrease in next-day waking cortisol, though neither was statistically significant.
A key limitation of our study is the low N. We view our results as preliminary, and we call for replication to confirm the patterns in larger samples. Larger sample sizes would also allow analysis of subgroup differences by gender and race/ethnicity. Moreover, the 18 minute decrease in sleep duration and 18% decrease in waking cortisol in the main specification are meaningfully-sized, but the large standard errors prevented us from differentiating them from zero (p=0.260 and 0.202, respectively). Future research should reexamine these outcomes.
Because our data do not allow identification of adolescents who were direct witnesses of violent events, our estimates are averaged across exposed and non-exposed adolescents. If the effect of violence is heterogeneous across these two types of adolescents (with direct witnesses arguably experiencing more stress), our estimates should be considered a lower bound for the effect that directly exposed adolescents would have experienced. Similarly, if robberies and assaults are underreported and measured with error, the true estimates would be larger in absolute value.
One way to test why crime affects adolescents is to test if the timing of crime matters. Evening crime mattering more, for instance, may provide more support for the opponent processes model of sleep (Edgar et al., 1993). In preliminary tests, crimes that occurred later in the day (after 4:00 PM, when the child was more likely to be home) had larger effects on bedtime and sleep duration than the baseline specification, but we do not have the power to formally test this difference. Future research should investigate whether it is near-bedtime crime or crime that occurs while the child is home that most affects sleep.
Changes in puberty may change the association between acute stressors, sleep, and cortisol. An initial review found no differences in the association between acute violent crime and the stress response by pubertal status. Given the low N, this analysis should be interpreted with caution. For example, the CAR estimate is 0.05 µg/dl for participants at the lowest end of the pubertal scale (meaning the pubertal transition hasn’t started) and 0.14 µg/dl for those at the top end of the scale (meaning the pubertal transition has completed). Although the difference between these estimates is not statistically significant, the difference is intriguing for future research, especially given prior research indicating that adolescence is associated with increased cortisol reactivity relative to children (e.g., Stroud et al., 2009). Future researchers with larger sample sizes should explore differences by pubertal status in more detail.
Future research should add objective measures of cognitive functioning to examine relations between semi-random stressful events, sleep, cortisol, and daily cognitive functioning. Such research may help uncover the mechanisms explaining some of the prior findings on acute local violence and performance on standardized tests (Gershenson & Tekin, 2015; Sharkey, 2010; Sharkey et al., 2012).
Acknowledgments
We thank conference participants at the Association for Psychological Sciences Annual Meeting. We acknowledge the Institute for Policy Research Faculty Fellowship to Emma K. Adam, the Institute for Policy Research and the Sybil N. Heide Fellowship for their graduate support for Jennifer A. Heissel, and NIH grant R21 AA021073.
References
- Adam EK. Emotion-cortisol transactions occur over multiple time scales in development: Implications for research on emotion and the development of emotional disorders. Monographs of the Society for Research in Child Development. 2012;77:17–27. doi: 10.1111/j.1540-5834.2012.00657.x. [DOI] [Google Scholar]
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience-cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alapin I, Fichten CS, Libman E, Creti L, Bailes S, Wright J. How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? Journal of Psychosomatic Research. 2000;49:381–390. doi: 10.1016/S0022-3999(00)00194-X. [DOI] [PubMed] [Google Scholar]
- Chida Y, Steptoe A. Cortisol awakening response and psychosocial factors: A systematic review and meta-analysis. Biological Psychology. 2009;80:265–278. doi: 10.1016/j.biopsycho.2008.10.004. [DOI] [PubMed] [Google Scholar]
- Clow A, Hucklebridge F, Stalder T, Evans P, Thorn L. The cortisol awakening response: More than a measure of HPA axis function. Neuroscience & Biobehavioral Reviews. 2010;35:97–103. doi: 10.1016/j.neubiorev.2009.12.011. [DOI] [PubMed] [Google Scholar]
- Dahl RE. The regulation of sleep and arousal: Development and psychopathology. Development and Psychopathology. 1996;8:3–27. doi: 10.1017/S0954579400006945. [DOI] [Google Scholar]
- Dressendörfer RA, Kirschbaum C, Rohde W, Stahl F, Strasburger CJ. Synthesis of a cortisol-biotin conjugate and evaluation as a tracer in an immunoassay for salivary cortisol measurement. The Journal of Steroid Biochemistry and Molecular Biology. 1992;43:683–692. doi: 10.1016/0960-0760(92)90294-S. [DOI] [PubMed] [Google Scholar]
- Edgar DM, Dement WC, Fuller CA. Effect of SCN lesions on sleep in squirrel monkeys: evidence for opponent processes in sleep-wake regulation. Journal of Neuroscience. 1993;13:1065–1079. doi: 10.1523/JNEUROSCI.13-03-01065.1993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fries E, Dettenborn L, Kirschbaum C. The cortisol awakening response (CAR): Facts and future directions. International Journal of Psychophysiology. 2009;72:67–73. doi: 10.1016/j.ijpsycho.2008.03.014. [DOI] [PubMed] [Google Scholar]
- Gershenson S, Tekin E. The Effect of Community Traumatic Events on Student Achievement: Evidence from the Beltway Sniper Attacks (Working Paper No. 21055) National Bureau of Economic Research; 2015. Retrieved from http://www.nber.org/papers/w21055. [Google Scholar]
- Hale L, Hill TD, Friedman E, Javier Nieto F, Galvao LW, Engelman CD, Peppard PE. Perceived neighborhood quality, sleep quality, and health status: Evidence from the Survey of the Health of Wisconsin. Social Science & Medicine. 2013;79:16–22. doi: 10.1016/j.socscimed.2012.07.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicken MT, Lee H, Ailshire J, Burgard SA, Williams DR. “Every shut eye, ain’t sleep”: The role of racism-related vigilance in racial/ethnic disparities in sleep difficulty. Race and Social Problems. 2013;5:100–112. doi: 10.1007/s12552-013-9095-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lacoe J, Sharkey PT. Life in a crime scene: Stop, question, and frisk activity in New York City neighborhoods in the aftermath of homicides. Sociological Science. 2016;3:116–134. doi: 10.15195/v3.a7. [DOI] [Google Scholar]
- Lavie P. Sleep Disturbances in the Wake of Traumatic Events. New England Journal of Medicine. 2001;345:1825–1832. doi: 10.1056/NEJMra012893. [DOI] [PubMed] [Google Scholar]
- Maldonado EF, Fernandez FJ, Trianes MV, Wesnes K, Petrini O, Zangara A, Ambrosetti L. Cognitive performance and morning levels of salivary cortisol and alpha-amylase in children reporting high vs. low daily stress perception. The Spanish Journal of Psychology. 2008;11:3–15. doi: 10.1017/S1138741600004066. [DOI] [PubMed] [Google Scholar]
- Oakley NR. Validation with polysomnography of the sleepwatch sleep/wake scoring algorithm used by the Actiwatch activity monitoring system. Bend: Mini Mitter, Cambridge Neurotechnology; 1997. [Google Scholar]
- Pruessner JC, Wolf OT, Hellhammer DH, Buske-Kirschbaum A, von Auer K, Jobst S, Kirschbaum C. Free cortisol levels after awakening: A reliable biological marker for the assessment of adrenocortical activity. Life Sciences. 1997;61:2539–2549. doi: 10.1016/S0024-3205(97)01008-4. [DOI] [PubMed] [Google Scholar]
- Sadeh A. Stress, trauma, and sleep in children. Child and Adolescent Psychiatric Clinics of North America. 1996;5:685–700. [Google Scholar]
- Sadeh A, Gruber R, Raviv A. The effects of sleep restriction and extension on school-age children: What a difference an hour makes. Child Development. 2003;74:444–455. doi: 10.1111/1467-8624.7402008. [DOI] [PubMed] [Google Scholar]
- Sapolsky RM, Romero LM, Munck AU. How do glucocorticoids influence stress responses? Integrating permissive, suppressive, stimulatory, and preparative actions. Endocrine Reviews. 2000;21:55–89. doi: 10.1210/er.21.1.55. [DOI] [PubMed] [Google Scholar]
- Sharkey PT. The acute effect of local homicides on children’s cognitive performance. Proceedings of the National Academy of Sciences. 2010;107:11733–11738. doi: 10.1073/pnas.1000690107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharkey PT, Tirado-Strayer N, Papachristos AV, Raver CC. The effect of local violence on children’s attention and impulse control. American Journal of Public Health. 2012;102:2287–2293. doi: 10.2105/AJPH.2012.300789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stroud LR, Foster E, Papandonatos GD, Handwerger K, Granger DA, Kivlighan KT, Niaura R. Stress response and the adolescent transition: Performance versus peer rejection stressors. Development and Psychopathology. 2009;21:47–68. doi: 10.1017/S0954579409000042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Talbot LS, McGlinchey EL, Kaplan KA, Dahl RE, Harvey AG. Sleep deprivation in adolescents and adults: Changes in affect. Emotion. 2010;10:831–841. doi: 10.1037/a0020138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Justice. Uniform Crime Report: Crime in the United States, 2015. Federal Bureau of Investigation; 2016. Retrieved from https://ucr.fbi.gov/crime-in-the-u.s/2015/crime-in-the-u.s.-2015/offenses-known-to-law-enforcement/violent-crime. [Google Scholar]
- Vigil JM, Geary DC, Granger DA, Flinn MV. Sex Differences in Salivary Cortisol, Alpha-Amylase, and Psychological Functioning Following Hurricane Katrina. Child Development. 2010;81:1228–1240. doi: 10.1111/j.1467-8624.2010.01464.x. [DOI] [PubMed] [Google Scholar]
- Vrshek-Schallhorn S, Doane LD, Mineka S, Zinbarg RE, Craske MG, Adam EK. The cortisol awakening response predicts major depression: Predictive stability over a 4-year follow-up and effect of depression history. Psychological Medicine. 2012;43:483–493. doi: 10.1017/S0033291712001213. [DOI] [PMC free article] [PubMed] [Google Scholar]