Abstract
Introduction
Although the majority of poisoning-related cases can be managed in home settings, reduction of hospital visits and admissions are still important challenge. Thousands of interventions are involved and the appropriate management of poisoning is therefore a major task and burden to any institution. Therefore, the present study was aimed to identify the most common classes of toxic substances and route of poisoning in children and to investigate the pattern of drug and chemical poisoning in suspected case fatalities, the subsequent need for hospital admission and arrival time to hospital.
Methods
A retrospective cross-sectional descriptive study of all registered poisoning cases of children reported to drug and poison information center at King Khaled University Hospital Riyadh, Saudi Arabia during the period of January 2010–December 2016.
Results
A total of 735 children presented to Pediatric Emergency Medicine with poisoning. Most of the cases were asymptomatic, and majority of children were arrived to the hospital in less than 3 h. The drugs were the most common cause of poisoning (70%) followed by chemical materials (29%), which is more common in children under 2 years comparing to other groups (p < 0.001). The route of poisoning was oral in the majority of cases (98.8%). The drugs most frequently ingested were analgesic (18.8%). Among the chemicals, pesticide products involved in (39.6%) of the cases, followed by cleaning products (25.9%) and cosmetic (22.8%).
Conclusion
The results found that the majority of poisoning cases occurred in children under the age of six and required only observation without treatment. These results necessitate the need for close cooperation between different governmental health-sectors to establish national epidemiological surveillance of poisoning events in Saudi Arabia to help to develop national plans to decrease the financial burden of emergency department congestion and hospital crowding.
Keywords: Poison, Children, Drugs, Chemical, Saudi Arabia
1. Introduction
Poisons, also known as toxins, are potentially harmful substances that can damage and injure the human body (Thomas et al., 2007). Poisoning occurs when these toxins are either ingested, inhaled, or introduced through the skin, with exposure often occurring intentionally or accidently in homes (Mowry et al., 2014). This significant global public health problem is one of the most important causes of morbidity and mortality worldwide. (Eddleston and Phillips, 2004) A World Health Organization report in 2012 revealed that an estimated 193,460 deaths were caused annually because of unintentional poisoning worldwide, of which 84% occurred in low- and middle-income countries (Global Health Estimates, 2014, World Health Organization, 2016). Moreover, the highest mortality rates from unintentional poisonings were reported in children younger than 5 years and adults older than 55 years. In Saudi Arabia, there have been multiple reports of poisoning in children and adolescents (Ragab et al., 2015, Naguib and Al-Saigul, 2009), with the peak incidence occurring in toddlers aged 1–7 years.
Among all reported cases of poisoning, acetaminophen is the most common cause (Alanazi et al., 2015). There are some reports of direct interventions and home management recommendations from poison control centers (Ragab and Al-Mazroua, 2015). Indeed, most poisonings can be managed at home, and reducing hospital visits and admissions remains an important challenge. Appropriate patient triage and management are key to any approach designed to reduce morbidity and mortality, especially among children. Given that thousands of cases are involved annually, appropriate poisoning management is a major burden for any institution.
In the present study, we aimed to identify the most common poisons in children by class and route. We also aimed to investigate the pattern of drug and chemical poisoning in case fatalities, the need for hospital admission, and the arrival time at hospital.
2. Methodology and materials
2.1. Study design
We conducted a retrospective cross-sectional descriptive study at King Khalid University Hospital (KKUH), Riyadh, Saudi Arabia. The study was approved by the institutional review board at KKUH.
2.2. Data collection
Data were collected from all registered cases of poisoning in children reported to our Drug and Poison Information Center (DPIC) between January 2010 and December 2016. The DPIC at KKUH frequently receives queries from the emergency medicine department regarding the management of poisoning in children. The emergency medicine department has 19 dedicated beds for pediatric cases younger than 12 years. Case data reported from January 2010 to June 2015 were retrieved manually, but data reported from July 2015 to December 2016 were retrieved electronically. All reported clinical and laboratory data were collected, including the patient’s medical electronic number, demographic data (age, gender, and weight), poison characteristics (suspected poison, route, quantity, time of poisoning, and arrival time at hospital), patient medical history (signs and symptoms), management details, and poisoning parameters. During data collection, patient identifiers were replaced with random identifiers for data protection and security. Patient information was only utilized for research purposes, and investigators ensured that confidentiality was maintained throughout the study period.
2.3. Statistical analysis
All data were analyzed using IBM SPSS, Version 20 (IBM Corp., Armonk, NY, USA), with P-values of <.05 considered statistically significant. Descriptive statistics are reported as means and medians (with standard deviations) or as frequencies and percentages, as appropriate. Chi-squared tests were used to determine associations between qualitative variables.
3. Results
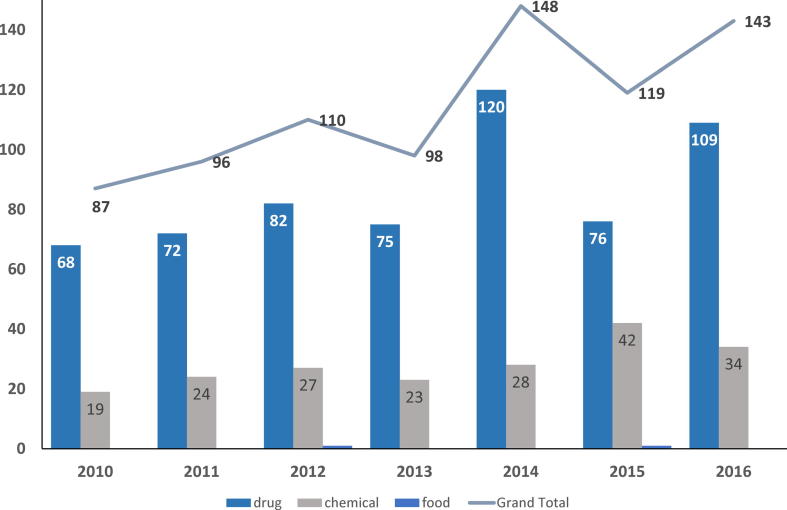
During the study period, the pediatric emergency department saw an average of 43,342 patients each year (range 32,286–50,546 per year), among which 735 presented with poisoning (mean age 2.7 ± 2.1 years, range 5 months to 13 years). Overall, there was an increasing trend in cases of reported poisoning, but the highest frequency was reported in 2014 (Fig. 1). To aid analysis, we divided patients into 0–2, 2–6, and >6 years age groups. Most children were younger than 6 years (94.3%) and almost half (49.7%) were female (Table 1).
Fig. 1.
Pattern of poisoning 2010–2016.
Table 1.
Characteristics of study population (N = 735).
| Parameters | N (%) |
|---|---|
| Age, years (±SD) | 2.7 (±2.1) |
| Age group N (%) | |
| <2 years | 459(62) |
| 2–6 years | 234(32) |
| >6 years | 42(6) |
| Gender | |
| Male | 337(45.8) |
| Female | 365(49.7) |
| Undocumented gender | 33(4.5) |
| Poison type | |
| Drug | 519(70.6) |
| Chemical | 214(29.1) |
| Food | (0.3)2 |
| Number of toxins | |
| 1 | 678(92.2) |
| 2 | 44(6) |
| >2 | 13(1.8) |
| Route of poisoning | |
| Oral | 726(98.8) |
| IV | 2(0.3) |
| DERM | 7(0.9) |
3.1. Poisoning type
Drugs were the most common cause of poisoning (70%), followed by chemicals (29%). The reported cases were more common in the 0–2 years age group than in the older age groups (p < .001). No significant differences were found between poisoning type and gender. In most cases, the route of poisoning was oral (98.8%) and children only ingested one poison (92.2%); however, 44 children ingested two drugs and 13 children ingested more than two poisons. There were 602 and 197 cases of accidently ingested medications and accidently ingested chemicals, respectively.
Analgesics (18.8%), antihistamines (13%), cardiovascular drugs (12.3%), vitamins (9.6%), antipsychotics (5.5%), oral hypoglycemics (4.7%), and oral bronchodilators (4.5%) were the most frequently ingested medications (Table 2). Other ingested medication classes included neurological medications (e.g., for attention deficit hyperactivity disorder, Parkinson’s disease, and migraine), gastrointestinal medications (e.g., proton pump inhibitors, laxatives, antacids, and probiotics), herbal products, immunosuppressants, and topical agents. Of the accidently ingested medications, acetaminophen was the most commonly ingested (8%, n = 48), followed by ibuprofen (6.8%, n = 41), loratadine (3.7%, n = 22), chlorpheniramine (3%, n = 18), angiotensin-converting enzyme inhibitors (2.5%, n = 15), and beta-blockers (1.7%, n = 10).
Table 2.
The most common drugs and chemicals children ingested.
| Drugs categories (N = 602) | N (%) |
|---|---|
| Analgesic | 113(18.8) |
| Antihistamine | 78(13) |
| Cardiovascular | 74(12.3) |
| Vitamins and supplements | 58(9.6) |
| Antipsychotics | 33(5.5) |
| Oral Hypoglycemic | 28(4.7) |
| Bronchodilators | 27(4.5) |
| Antidepressants | 21(3.5) |
| Decongestants | 18(3) |
| Antibiotics | 17(2.8) |
| Anticonvulsants | 16(2.7) |
| Oral Contraceptive | 14(2.3) |
| Thyroids | 13(2.1) |
| Cough suppressants & expectorants | 11(1.8) |
| Gastrointestinal spasmolytic | 11(1.8) |
| Other medications | 70(11.6) |
| Specified chemicals (N = 197) | N (%) |
| Pesticides | 78(39.6) |
| Cleaning | 51(25.9) |
| Personnel/cosmetic | 45(22.8) |
| Industrial | 17(8.7) |
| Stings/Bites | 6(3) |
Among the ingested chemicals, pesticides were most common (39.6%), followed by cleaning products (25.9%) and cosmetics (22.8%). Of the accidently ingested chemicals, household cleaning substances were most commonly reported (26%, n = 51), followed by insecticides (21.3%, n = 42), organophosphates (9.6%, n = 19), rodenticides (8.6%, n = 17), nail polish (7.1%, n = 14), and perfume (3.6%, n = 7).
3.2. Symptoms and management
Most cases were asymptomatic, but some children developed gastrointestinal symptoms (e.g., abdominal pain, vomiting, and diarrhea), which were most common regardless of poisoning type. However, it was notable that neurological symptoms (e.g., dizziness, drowsiness, seizure, and sedation) were more common with drug poisoning. Although no treatment was given in most cases, 28% were treated by gut decontamination with activated charcoal and 1.8% were given a specific antidote (e.g., atropine in seven cases of organophosphate poisoning, N-acetylcysteine in four cases of acetaminophen toxicity, and scorpion antivenom in two cases of scorpion bites). Systemic treatment was required for 24 children, but mainly involved intravenous fluid (Table 3).
Table 3.
Poisoning management (N = 735).
| Treatment received | N (%) |
|---|---|
| Gut decontamination | 208(28.2) |
| Antidote | 13(1.8) |
| Symptomatic management | 24(3.1) |
| Observation | 490(66.2) |
Most children arrived at hospital within 3 h of poisoning, but a small number (1%) arrived one day later (Table 4). Most the treatment took place in the pediatric emergency medicine department and most patients could be discharged without further treatment. Only 54 children were kept in for observation the pediatric emergency department and only 14 were admitted to hospital.
Table 4.
Hospital arrival time.
| Time | N (%) |
|---|---|
| 30 min | 147(20) |
| 1 h | 180(24) |
| 3 h | 188(25) |
| 6 h | 46(6.2) |
| 12 h | 25(3.3) |
| 24 h | 27(3.6) |
| 48 h | 7(1) |
| Unknown | 115(15) |
4. Discussion
Drug and chemical poisoning are typically reported among the most common reasons for unintentional injury in children (Centers for Diseases Control and Prevention, 2017, Heron, 2014). According to the 2015 annual report for the National Poison Data System (NPDS) of the American Association of Poison Control Centers, data from 55 poison centers indicated that almost half of poisonings (47%) occurred in children younger than 6 years, and that approximately 1.9% resulted in death or major negative sequelae. Overall, children aged 1–2 years were reported to be affected most often (Mowry et al., 2016), with the highest incidence in children aged 1 year (8243 exposures/100,000 children) followed by those aged 2 years (7903 exposures/100,000 children). Unintentional poisonings also occurred most often in children aged 1–2 years in the period between 1983 and 2015, with the incidence remaining fairly consistent over that time (Mowry et al., 2014, Mowry et al., 2016, Mowry et al., 2014, Veltri and Litovitz, 1984).
In our study between 2010 and 2016, more than half of all cases of poisoning (62%) occurred in children younger than 2 years. Although there have been no comprehensive epidemiological studies of the incidence of poisoning in the Kingdom of Saudi Arabia to date, studies published for different regions and time periods also indicate that children younger than 5 years are most often affected (Al-Mohamadi et al., 2013, Saddique, 2001, Mahdi et al., 1983, Al-Sekait, 1989, Al Hazmi, 1998, Izuora and Adeoye, 2001, Al-Shehri, 2004, Al-Barraq and Farahat, 2011). During the period from 1986 to 1996, the poison control center at KKUH served the entire Kingdom of Saudi Arabia and received 5984 poison calls (Al-Mohamadi et al., 2013). Among these calls, 88% concerned children, and 92% of these concerned children younger than 5 years. In a study conducted in the western region from 1994 to 1996, the 2–5 years age group was affected most (61%), while another study conducted in the northern region from 1992 to 1998 showed that the 1–3 years age group was affected most (66%) (Al-Sekait, 1989, Al Hazmi, 1998). A study from 2001 to 2003 in the southern region indicated that the 2–4 years age group accounted for 80.7% of cases (Izuora and Adeoye, 2001), while a similar study in the central region in 2010 showed that those younger than 5 years accounted for 61% of cases (Al-Shehri, 2004). Meanwhile, the most recent study conducted in the western region between 2009 and 2011 found that 70% of cases occurred in those aged younger than 4 years (Al-Barraq and Farahat, 2011). Due to the lack of unified epidemiological data regarding poisonings in Saudi Arabia, it is difficult to assess the national status of poisoning in children.
According to the 2015 NPDS report, the most common poisons in children younger than 5 years were cosmetics/personal care products (13.6%), household cleaning substances (11.2%), analgesics (9.12%), foreign bodies/toys/miscellaneous (6.45%), and topical preparations (5.33%) (Mowry et al., 2016). The same five poisons were the top ranking exposures for children younger than 5 years in the 2014 annual report (Mowry et al., 2014). We found that drug exposure (70.6%) was more common than chemical exposure (29.1%) throughout the study period (Fig. 1), which is consistent with similar regional studies showing drug ingestion, particularly analgesic ingestion, to be the most frequent exposure in children. The top five poisons in our study were analgesics (14.14%), antihistamines and pesticides (9.76% each), cardiovascular medications (9.26%), vitamins and supplements (7.26%), and household cleaning substances (6.38%). Cosmetics/personal care products, antipsychotics, and oral hypoglycemics all had lower rates. Thus, pesticides, antihistamines, and vitamins/supplements were the second, third, and fourth most common poisons, respectively; however, these corresponded to the eighth, seventh, and sixth most common poisons among children younger than 5 years in the United States in 2015. The higher ranking of unintentional poisoning due to drugs in Saudi Arabia may be due to the tendency of Saudi families to store old medications for future use. There were few documented cases (4 cases) of overexposure to expired medications in this study. In addition, it should be noted that most medications can be obtained easily and without prescription in Saudi Arabia (Al-Mohamadi et al., 2013).
Similarities exist between the top eight most common poisons in this study and data reported worldwide; however, this similarity was only apparent in local studies conducted after 2000. In one older study of young children, central nervous system (CNS) depressants were the most frequent poisons (70%) (Saddique, 2001), while in another, hydrocarbons (e.g., kerosene; 38.6%) were most frequent (Al Hazmi, 1998). The difference in these findings is probably accounted for by the fact that most CNS depressants, such as barbiturates, tricyclic antidepressants, and older anticonvulsants, are no longer used as often. Similarly, kerosene is used less frequently in homes thanks to the modernization seen in Saudi Arabia over recent years. Analgesics, specifically non-steroidal anti-inflammatory drugs, as well as household cleaning substances, were shown to be the most common poisons in children in recent local research (Al-Barraq and Farahat, 2011, Hegazy et al., 2012, Abd-Elhaleem and Al Muqhem, 2014). These findings are consistent with ours, except that antipsychotics were the most frequently reported poison in one of those studies (Hegazy et al., 2012). The observed variations might be explained by regional differences among studies, emphasizing the need for detailed national surveillance using standardized methodology to identify the poisoning patterns and characteristics in the whole kingdom.
Regardless of the child’s age, the publication year, or the place of research, most studies in Saudi Arabia have indicated that analgesics are the most common poisons (Alanazi et al., 2015, Al-Shehri, 2004, Al-Barraq and Farahat, 2011). A recent study among children younger than 15 years old with no mental disabilities showed that acetaminophen was the most common poison (27.6%), with those aged 1–7 years being the most vulnerable (74.8%) (Ragab and Al-Mazroua, 2015). Among the identified analgesics (n = 113), acetaminophen (42.5%, n = 48) and ibuprofen (41.6%, n = 41) were the most reported poisons in our study. However, other drugs were frequently ingested. For example, loratadine (28.2%, n = 22) and chlorpheniramine (23.1%, n = 18) were the most frequently ingested antihistamines (n = 78), with most taken in combination with decongestants like pseudoephedrine. Angiotensin-converting enzyme inhibitors (20.3%, n = 15) and beta-blockers (13.5%, n = 10) were the most documented cardiovascular medications (n = 74).
The second most common poisons in our study were pesticides (n = 78). Of these, insecticides accounted for most cases (53.8%, n = 42), with organophosphates (24.4%, n = 19) and rodenticides (21.8%, n = 17) accounting for the remainder. Common cosmetics/personal care products identified as poisons (n = 45) included nail polish, perfume, body and breath sprays, hair dye, cream, and hair lightening products, among others. However, nail polish (31.1%, n = 14), particularly acetone-based nail polish, and perfume (15.6%, n = 7) were the most common poisons in this class. Common poisons in among the household cleaning substances (n = 51) were soaps, disinfectants, detergents, bleaches, air-refresher balls, and specific cleaning agents for woods, kitchens, dishes, and fabrics. Bleach containing sodium hypochlorite (e.g., Clorox®; 23.5%, n = 12) and disinfectant liquids containing chloroxylenol (e.g., Dettol®; 17.7%, n = 9) were the most commonly ingested cleaning products.
Over-the-counter medications like acetaminophen, ibuprofen, loratadine, and chlorpheniramine were the most common poisons. Equally, however, readily accessible pesticides, cleaning products, and cosmetics/personal care products were also common poisons. These results therefore raise the concern of poor knowledge among caregivers regarding the potentially harmful effects of the over-counter medications and household chemicals.
In our study, approximately 28% of children were treated by gut decontamination with activated charcoal and only 1.8% (n = 13) were given specific antidotes. Also, more than half of patients (66.2%) only required observation, indicating that there may have been avoidable presentations and inflation in healthcare costs. The Ministry of Health (MOH) in Saudi Arabia launched a “937 Service” (MOH Emergency Call Center) in 2013, and a duty of this service is to answer and deal with calls regarding poisoning. In addition to this center, there are many regional poison centers under MOH control; however, there are no available reports or documents from these services to assess the efficacy of their provision. In addition, the public are unlikely to be aware of these centers, which will lead to unnecessary increases in presentations with poisoning to emergency departments.
Our study has some important limitations. Notably, this was a retrospective study that depended on data collected from records at the DPIC. These were retrieved manually for the period from January 2010 to June 2015, but were retrieved electronically for the period from July 2015 to December 2016. Because of the retrospective collection method, some data may be missing. In addition, emergency physicians may have started to manage more poison cases without contacting the DPIC for advice and documentation. Despite these limitations, our study was based on results obtained over a 7-year period and from a relatively large base sample. These results emphasize the importance of developing a national surveillance strategy for monitoring and managing poisoning events in Saudi Arabia.
5. Conclusions
In conclusion, we found that most cases of poisoning occurred in children younger than 6 years and that most children could be treated with only observation. The most common poisons were analgesics, antihistamines, pesticides, cardiovascular medications, vitamins and supplements, and household cleaning substances. However, our results are local only and indicate an urgent need for close cooperation between all stakeholders (i.e., MOH poison control centers, hospital poison control centers, and the National Drug and Poison Information Center of the Saudi Food and Drug administration) to establish a national epidemiological surveillance program for poisoning events in Saudi Arabia. Such a surveillance program could be used to develop education, research, and training for the prevention and management of poisoning, and could ultimately decrease associated financial costs, emergency department congestion, and hospital crowding. In the meantime, our results provide the most current information about the drug and chemical poisons most prevalent in children in the Kingdom of Saudi Arabia. Properly applied, this information can be used to improve not only our understanding of local risk factors but also the delivery of efficient public health campaigns and the assessment of the clinical and finical effects of poison management.
Footnotes
Peer review under responsibility of King Saud University.
Contributor Information
Sultan Alghadeer, Email: salghadeer@ksu.edu.sa.
Manal Alrohaimi, Email: manal.alrohaimi@gmail.com.
Abeer Althiban, Email: abeeralthiban@gmail.com.
Nora A. Kalagi, Email: nakalagi@ksu.edu.sa.
Bander Balkhi, Email: bbalkhi@ksu.edu.sa.
Anas A. Khan, Email: anaskhan@ksu.edu.sa.
References
- Abd-Elhaleem, Z.A., Al Muqhem, B.A., 2014. Pattern of acute poisoning in Al Majmaah Region, Saudi Arabia. Am. J. Clin. Exp. Med. 4(2), 79–85.
- Alanazi M.Q., Al-Jeriasy M.I., Al-Assiri M.H., Afesh L.Y., Alhammad F., Salam M. Hospital performance indicators and their associated factors in acute child poisoning at a Single Poison Center, Central Saudi Arabia. Medicine. 2015;94(52):e2339. doi: 10.1097/MD.0000000000002339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al Hazmi A.M. Patterns of accidental poisoning in children in Jeddah, Saudi Arabia. Ann. Saudi Med. 1998;18(5):457–459. doi: 10.5144/0256-4947.1998.457. [DOI] [PubMed] [Google Scholar]
- Al-Barraq A., Farahat F. Pattern and determinants of poisoning in a teaching hospital in Riyadh, Saudi Arabia. Saudi Pharm. J.: SPJ. 2011;19(1):57–63. doi: 10.1016/j.jsps.2010.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Mohamadi A., Badr A., Bin Mahfouz L., Samargandi D., Al Ahdal A. Dispensing medications without prescription at Saudi community pharmacy: extent and perception. Saudi Pharm. J.: SPJ. 2013;21(1):13–18. doi: 10.1016/j.jsps.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Al-Sekait, M., 1989. Accidental Poisoning of Children in Riyadh, Saudi Arabia. 6, 109. [DOI] [PubMed]
- Al-Shehri M. Pattern of childhood poisoning in Abha City – Southwestern Saudi Arabia. J. Family Community Med. 2004;11(2):59–63. [PMC free article] [PubMed] [Google Scholar]
- Centers for Diseases Control and Prevention (CDC). CDC Childhood Injury Report. Available at: <https://www.cdc.gov/safechild/child_injury_data.html> (accessed June 9, 2017).
- Eddleston M., Phillips M.R. Self poisoning with pesticides. BMJ. 2004;328:42–44. doi: 10.1136/bmj.328.7430.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Global Health Estimates 2013, 2014. Deaths by Cause, Age and Sex, Estimates for 2000–2012. World Health Organization, Geneva.
- Hegazy R., Almalki W.H., Afify R.H. Pattern of acute poisoning in Makkah Region: SAUDI ARABIA. Egypt. J. Community Med. 2012;30(1):207–220. [Google Scholar]
- Heron, M., 2014. Deaths: Leading Causes for 2014. Centers for Disease Control and Prevention (CDC). National Vital Statistics Reports National Vital Statistics Reports, Vol. 65, No. 5, June 30, 2016. Available at: <https://www.cdc.gov/nchs/data/nvsr/nvsr65/nvsr65_05.pdf> (accessed June 9, 2017). [PubMed]
- Izuora G.I., Adeoye A. A seven-year review of accidental poisoning in children at a Military Hospital in Hafr Al Batin, Saudi Arabia. Ann. Saudi Med. 2001;21(1–2):13–15. doi: 10.5144/0256-4947.2001.13. [DOI] [PubMed] [Google Scholar]
- Mahdi A.H., Taha S.A., Al Rifai M.R. Epidemiology of accidental home poisoning in Riyadh (Saudi Arabia) J. Epidemiol. Community Health. 1983;37(4):291–295. doi: 10.1136/jech.37.4.291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowry J.B., Spyker D.A., Cantilena L.R., Jr, McMillan N., Ford M. 2013 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 31st Annual Report. Clin. Toxicol. (Phila). 2014;52(10):1032–1283. doi: 10.3109/15563650.2014.987397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mowry J.B., Spyker D.A., Brooks D.E., McMillan N., Schauben J.L. Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 32nd Annual Report. Clin. Toxicol. 2014;53(10):962–1147. doi: 10.3109/15563650.2015.1102927. [DOI] [PubMed] [Google Scholar]
- Mowry J.B., Spyker D.A., Brooks D.E., Zimmerman A., Schauben J.L. 2015 Annual Report of the American Association of Poison Control Centers' National Poison Data System (NPDS): 33rd Annual Report. Clin. Toxicol. (Phila). 2016;54(10):924–1109. doi: 10.1080/15563650.2016.1245421. [DOI] [PubMed] [Google Scholar]
- Naguib, M.M., Al-Saigul, A.M., 2009. Pattern of acute poisoning in Al-Qassim region: a surveillance report from Saudi Arabia, 1999–2003. Eastern Mediterranean Health J., 15(4). [PubMed]
- Ragab A., Al-Mazroua M. Pattern of pediatric toxicity in Saudi Arabia eastern province incidence, demographics and predisposing factors. Pediat Therapeut. 2015;5:2161–2665. [Google Scholar]
- Ragab A.R., Al-Mazroua M.K., Mahmoud N.F., Al-Moagel N.M., Al-Buaijan A.Y. Poisoning-related fatalities in Eastern Province-Saudi Arabia. Ann. Forensic Res. Anal. 2015;2(2):1019. [Google Scholar]
- Saddique A. Poisoning in Saudi Arabia: ten-year experience in King Khaled University Hospital. Ann Saudi Med. 2001;21(1–2):88–91. doi: 10.5144/0256-4947.2001.88. [DOI] [PubMed] [Google Scholar]
- Thomas W.F., John H.D., Willium R.H. 28th ed. Lippincott William and Wilkins; New York: 2007. Stedman's Medical Dictionary; p. 2004. [Google Scholar]
- Veltri J.C., Litovitz T.L. 1983 Annual report of the American Association of Poison Control Centers National Data Collection System. Am. J. Emerg. Med. 1984;2(5):420–443. doi: 10.1016/0735-6757(84)90046-9. [DOI] [PubMed] [Google Scholar]
- World Health Organization, 2016. Preventing disease through healthy environments: a global assessment of the burden of disease from environmental risks; 2016. Available at: <http://apps.who.int/iris/bitstream/10665/204585/1/9789241565196_eng.pdf> (accessed May 5, 2017).