Abstract
Background
This study aims to compare the value of the Bishop score and cervical length measurement by transvaginal ultrasonography in predicting active labor within 6 h, induction-to-delivery interval, and the duration of active labor and to estimate the most useful cutoff points for the two methods.
Methods
This is a prospective comparative study of Bishop score and cervical length measured by transvaginal sonography on 62 nulliparous subjects who underwent induction of labor.
Results
The Bishop score of the subjects ranged from two to seven (2–7). The mean Bishop in this study population was 4.37 + 1.23. The mean cervical length in this study was 25.59 + 6.07. Bishop score was highly significant (P value < 0.0001) in predicting active phase of labor as compared to cervical length (P = 0.004). The best cutoff value for Bishop score to predict induction of labor within 6 h was more than 4 with sensitivity of 69% and specificity of 79%. Similarly, best cutoff value for cervical length to predict induction of labor within 6 h was less than or equal to 25 mm with sensitivity of 51% and specificity of 70%. Bishop score was more significant (P = 0.001) in predicting induction-to-delivery interval within 12 h as compared to cervical length (P = 0.01).
Conclusion
The Bishop score was superior in predicting the response to induction as compared to the cervical length measured by transvaginal ultrasonography.
Keywords: Labor induction, Induction active phase interval, Bishop score, Transvaginal cervical length
Introduction
Bishop score, based on the pre-induction favorability of the cervix, has been traditionally used, predicting whether an induced labor will result in successful vaginal delivery. Labor induction with a low cervical score has been associated with failure of induction, prolonged labor, and a high rate of cesarean deliveries. However, this assessment is subjective and several studies have demonstrated a poor predictive value for the outcome of induction, especially in women with a low Bishop score [1].
Measurement of transvaginal cervical length has primarily been used to detect cervical changes in women at risk of preterm delivery. However, the same cervical changes can be detected to predict the success of induction of labor. Theoretically, transvaginal ultrasonographic measurement of the cervix could represent a more accurate and objective assessment of the cervix than digital examination, because the supra-vaginal portion of the cervix usually comprised about 50% of the cervical length is very difficult to assess digitally in a closed cervix [2]. In addition, the assessment of the effacement, which starts at the internal os, will be difficult to predict in a closed cervix. Also, sonographic measurement of the cervical length is quantitative and easily reproducible method of assessing the cervix, which can be achieved easily with minimal discomfort to the patient.
This study was designed to compare the value of the Bishop score and cervical length measurement by transvaginal ultrasonography in predicting active labor within 6 h, induction-to-delivery interval and to estimate the most useful cutoff points for the two methods.
Subjects and Methods
This prospective comparative study was carried out at the Department of Obstetrics and Gynecology, Medical College and SSG Hospital, Baroda, during 1-year period from November 1, 2014, to October 30, 2015, after the approval from the Institutional Ethics Committee for Human Research (IECHR).
Sample Size Estimation
A pilot study of 25 cases was carried out from September 1, 2014, to October 30, 2014. The results were analyzed, and ROC curves were drawn for both Bishop and transvaginal cervical length. Correlation in both negative and positive groups was derived. Using MedCalc software with an alpha of 0.05 and power 0.8, it was calculated that a minimum of 48 women needed to be recruited for an adequately powered study.
Inclusion Criteria
Primigravid women with singleton pregnancy with 37–42 weeks of gestation
Cephalic presentation
Exclusion Criteria
<37 weeks of gestation
Fetal mal-presentations
Multi-fetal gestation
Non-reassuring fetal heart rate tracing
Congenital anomalies of the fetus
Intrauterine death of the fetus
Previous cesarean delivery or other uterine surgery (myomectomy, hysterotomy)
History of antepartum hemorrhage
Cephalopelvic disproportion
Any contraindication of vaginal delivery.
Among the subjects presenting to our unit and requiring labor induction, those who fulfilled the inclusion and exclusion criteria of the study were enrolled in the study. The eligible subjects were enrolled in the study after obtaining written and informed consent to participate in the study. Baseline characteristics such as age, gestational age at induction, and indication of induction were noted. After careful history and general examination, transvaginal ultrasonographic measurement of cervical length in mm was taken with the standard longitudinal view of the cervix after the patient’s bladder was emptied. The image was enlarged so that the cervix occupies at least two-third of the image, and external os and internal os were well seen. The cervical length was measured from the internal os to the external os along the endocervical canal. A single observer taken cervical length measurement. Three consecutive cervical images were obtained and three separate readings of cervical length were taken and then average cervical length in mm was considered for the study.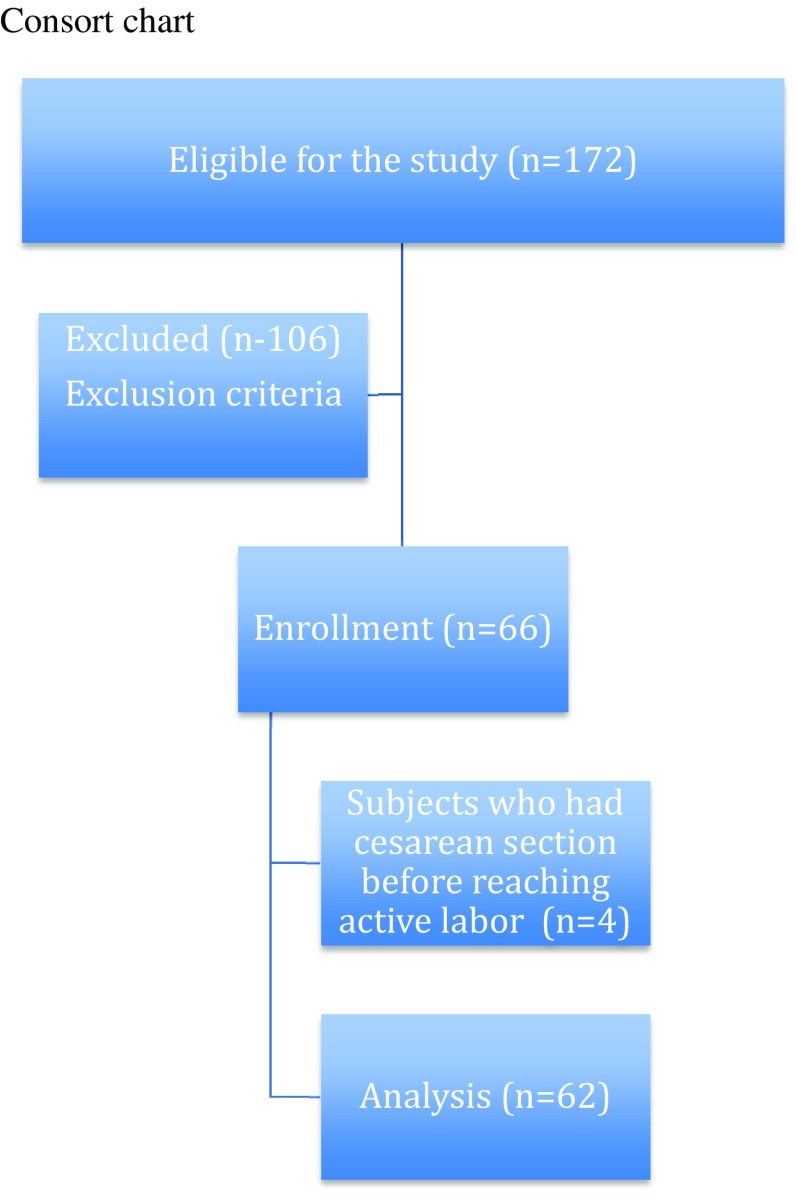
After sonography, the Bishop score was determined by digital examination by another observer. Induction of labor was carried out in a uniform manner for all the women enrolled in the study. A Foley bulb was inserted by direct visualization with the aid of a sterile speculum. The Foley was inserted through the internal cervical os, filled with 30 mL of normal saline, and then pulled snugly against the internal os. The catheter of the Foley bulb was taped to the patient’s inner thigh under gentle traction. In addition, the women received vaginal misoprostol 25 micrograms every 4 h. Once the patient entered active labor (cervical dilatation more than 4 cm with uterine contractions), misoprostol administration was discontinued. Further management of labor was expectant management (if regular uterine contractions are present), amniotomy and/or intravenous (IV) oxytocin (if regular uterine contractions are not present, i.e., <3 contractions/10 min). If indicated, IV oxytocin was started as per standard protocol after 6 h from the last misoprostol dose. Oxytocin was administered as per standard protocol starting at 2 mU/min increasing by 2 mU every 20 min until regular uterine contractions occurred. Electronic fetal heart rate monitoring was carried out for all subjects.
The induction active phase interval, induction-to-delivery interval, and the mode of delivery were noted. Failed induction was defined as an inability to achieve the active phase of labor corresponding to cervical dilatation of ≥4 cm within 24 h of onset of induction. Failure to progress was defined as no cervical dilation during the active phase of labor for the last 2 h or no descent of the fetus’ head during the second stage of labor for at least 1 h despite adequate uterine contractions. This was considered as an indication of cesarean delivery for failure to progress.
Data Analysis: All statistical calculations were done using the MedCalc software version 12.5.0. The t test was used to analyze means, Fisher’s exact test was used for categorical datasets, and relative risk with 95% CI was calculated. Mann–Whitney U Test was applied for independent variables (e.g., Bishop score). The two variables were compared using standard error of difference between two means. P < 0.05 was taken as a significant level. Receiver operator characteristic (ROC) curves were constructed for both Bishop score and transvaginal cervical length with active phase interval within 6 h. The area under the curve (AUC) was then calculated, and confidence intervals (CIs) for this area were established. Sensitivity and specificity at different cutoff points were calculated for both cervical length and Bishop score. A p value of <0.05 was considered to be statistically significant.
Results
The estimated sample size for this study was 48 but since we could enroll more subjects in the time available for the study, a total of demographically similar 66 subjects were enrolled this study.
The most common indication of induction of labor was 39.4% subjects had post-datism, i.e., gestational age more than 40 weeks {n = 26 (39.4%)}. The other indications were oligohydramnios {n = 14 (21.2%)}, preeclampsia {n = 18 (27.3%)}, and premature rupture of membranes {n = 8 (12.1%)}. Some studies have considered the cases of PROM as contraindication of labor induction. However, unpublished data of our own experience at the institute found no difference in response to induction in cases of PROM when compared with other indications. The results of the FOLCROM trial [3] (Foley Catheter Versus Oxytocin for Labor Induction in Women With Term and Near Term Premature Rupture of Membranes: A Randomized Clinical Trial) will probably give us more insight into the matter.
Out of the 66 subjects, 55 (83.3%) underwent normal vaginal delivery, and 11 (16.7%) subjects were delivered by cesarean section. The indications of cesarean section were fetal distress (n = 03), pathological cardiotocography (n = 01), non-progressive first stage (n = 02), non-progressive second stage (n = 02), deep transverse arrest (n = 02), and persistent occipito-posterior position (n = 01). Four subjects underwent cesarean section before the onset of active labor for fetal indications. There were no cases of failed induction.
Four subjects underwent cesarean section before the onset of active labor, and hence, we excluded those four subjects from the data analysis. Data were analyzed for 62 subjects.
The Bishop score of the subjects ranged from two to seven (2–7). The mean Bishop in this study population was 4.37 ± 1.23. The mean cervical length in this study was 25.59 + 6.07.
Generally studies comparing predictability of Bishop score evaluate the likelihood of vaginal delivery or the total duration of labor as a primary outcome variable. However, the mode of delivery and the total duration of labor can be affected by multiple factors other than cervical status, such as parity, BMI, fetal weight, and indications of cesarean delivery. Labor induction is defined as ability to initiate labor. Clinically, it is difficult to identify the precise time of onset of true labor. Instead, active labor as recognized by cervical dilatation of 3 to 4 cm or greater in the presence of uterine contractions is easier to identify. Hence, in this study we considered the onset of active labor as the final outcome of labor induction. We compared the predictability of Bishop score and the transvaginal cervical length for induction active phase interval of 6 h and induction delivery interval of 12 h.
In this study, a combination of mechanical method (intracervical Foley’s catheter) and vaginal misoprostol was used as method of induction of labor. This induction protocol shortens the time required for induction of labor and is safe and efficacious as compared to either of the method singly. As a result, in this study, we found shorter induction active phase intervals as compared to other studies.
Table 1 compares the two methods as regards induction active phase interval of less than 6 h and less than 12 h. This table excludes 4 patients who underwent cesarean section before reaching active phase of labor. Median Bishop score for the nulliparous subjects was 5.0; corresponding mean cervical length was 23.53 with standard deviation of 5.76. Median Bishop score for nulliparous subjects whose induction active phase interval is more than 6 h was 4.0, and corresponding mean cervical length was 27.84 with SD of 5.54. Applying Mann–Whitney U test for these two medians, it was found that Bishop score is highly significant (P value < 0.0001) in predicting active phase of labor. P value for cervical length was 0.004, which is also highly significant but less as compared to Bishop score.
Table 1.
Predictability of Bishop score and cervical length for induction active phase interval
| Induction active phase interval ≤6 h (n = 35) | Induction active phase interval >6 h (n = 27) | P value | |
|---|---|---|---|
| Median Bishop | 5.0 | 4.0 | <0.0001 |
| Mean cervical length | 23.53 ± 5.76 | 27.84 ± 5.54 | 0.0043 |
| Induction-to-delivery interval <12 h (n = 45) | Induction-to-delivery interval ≥12 h (n = 21) | P value | |
| Median Bishop | 5.0 | 4.0 | <0.0002 |
| Mean cervical length | 24.1 ± 5.71 | 28.9 ± 5.63 | 0.002 |
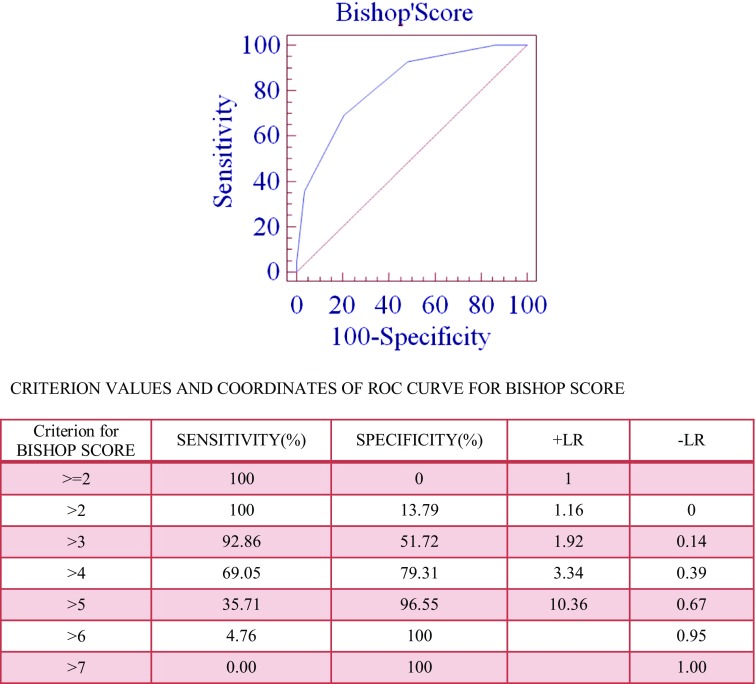
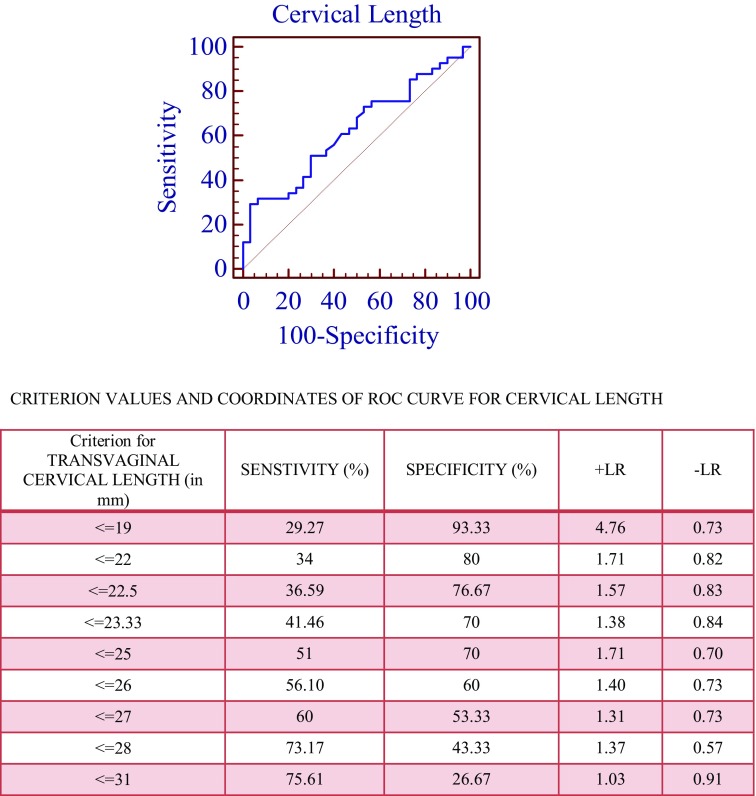
We constructed ROC curves for Bishop score and cervical length with active phase interval within 6 h (Figs. 1 and 2). The curves constructed for the Bishop score and cervical length were above the 45° line, indicating that there was a significant relationship between these variables and prediction of labor. AUC for Bishop score with active phase interval within 6 h was calculated to be 0.824 (95% CI 0.715–0.904). P value for this curve is <0.0001 which is highly significant. AUC for TVUS cervical length with active phase interval within 6 h is 0.625 (95% CI 0.50–0.737). P value for this curve is 0.06, which is not significant. Optimized cutoff points for Bishop score and cervical length were determined by ROC curves. In this study, the best cutoff value for Bishop score to predict induction of labor within 6 h was more than four with sensitivity of 69%, specificity of 79%, positive likelihood ratio of 3.34, and negative likelihood ratio of 0.39. Similarly, best cutoff value for cervical length to predict induction of labor within 6 h was less than or equal to 25 mm with sensitivity of 51%, specificity of 70%, positive likelihood ration of 1.71, and negative likelihood ratio of 0.70.
Fig. 1.
ROC curve of Bishop score with active phase labor within 6 h
Fig. 2.
ROC curve of cervical length by TVUS with active phase within 6 h
Table 1 also shows predictability of Bishop score and cervical length for delivery within 12 h of induction. Median Bishop score of this subgroup was 5; corresponding mean cervical length was 24.4 with standard deviation of 5.54. Median Bishop score of nulliparous subjects whose induction active phase interval is more than 12 h was 3.0, and corresponding mean cervical length was 29.1 with SD of 5.65. Independent t test has been applied to get the P value of mean cervical length (continuous variable) and Chi-square test for Bishop score. It was found that Bishop score is highly significant (P value 0.007) in predicting induction-to-delivery interval. P value for cervical length was 0.004, which is also highly significant.
Table 2 depicts comparison of induction active phase interval based on cutoff values of Bishop score and cervical length. Taking cutoff values as 4 for Bishop score and 25 mm for transvaginal cervical length, we divided study population into two groups and mean induction active phase interval was calculated for each. This table excludes four patients who underwent cesarean section before reaching active phase of labor. The statistical significance was calculated using independent t test, and it was found that P value for Bishop score was 0.002, which is highly significant. For transvaginal cervical length, P value was 0.034.
Table 2.
Comparison of induction active phase interval based on the cutoff values of Bishop score and cervical length
| Bishop score | No. of patients | Mean induction active phase interval in hours | SD | P value |
|---|---|---|---|---|
| <4 | 15 | 10.00 | 4.21 | |
| ≥4 | 47 | 5.96 | 4.26 | 0.002 |
| Transvaginal cervical length | ||||
| ≤25 mm | 28 | 5.60 | 3.72 | |
| >25 mm | 34 | 8.04 | 4.93 | 0.034 |
Table 3 indicates comparison of induction-to-delivery interval based on cutoff values of Bishop score and cervical length. Considering cutoff values as four for Bishop score and 25 mm for transvaginal cervical length, we divided study population into two groups and mean induction-to-delivery interval was calculated for each. The statistical significance was calculated by independent t test, and P value for Bishop Score was 0.001, which is highly significant. For transvaginal cervical length, P value was 0.01, which is also significant.
Table 3.
Prediction of induction-to-delivery interval based on the cutoff values of Bishop score and cervical length
| Bishop | No. of patients | Mean induction-to-delivery interval in hours | SD | P value |
|---|---|---|---|---|
| <4 | 17 | 13.71 | 4.60 | |
| ≥4 | 49 | 9.10 | 4.43 | 0.0005 |
| Transvaginal cervical length | ||||
| ≤25 mm | 30 | 8.58 | 3.80 | |
| >25 mm | 36 | 11.71 | 5.26 | 0.0084 |
Discussion
Our results suggest that both Bishop score and cervical length are good predictors of successful induction of labor in nulliparous women. But Bishop score had statistically better significance than cervical length. Although cervical length measured by ultrasonography appears to be a more objective and precise measure, other cervical variables might be involved in predicting ripeness of the cervix; this probably explains the results of this study.
Bahadori et al. [4] also a found stronger correlation of Bishop (0.001) than of cervical length (0.04) for predicting cervical ripening in 12 h. Cutoff for Bishop was ≥4 with a sensitivity of 57.9% and a specificity of 28.7% and for cervical length was ≥19 mm with a sensitivity of 66.7% and a specificity of 65%. Similar results were found by Cengiz H et al. [5].
Parvin Bastani et al. [6] found that induction-to-delivery interval positively correlated with cervical length with P value of <0.01. They showed that ROC for cervical length was significantly better than Bishop score and posterior cervical angle. There have been similar studies, suggesting that cervical length is a better predictor than the Bishop score [7–10].
Abdelazim et al. [11] found similar predictability for prolonged induction-to-delivery interval.
A Cochrane review [12] did not demonstrate superiority of one method over the other in terms of the main outcomes assessed. While use of TVUS was associated with an increased need for misoprostol for cervical ripening, both methods could be complementary. The choice of a particular method of assessing pre-induction cervical ripening may differ depending on the environment and need where one is practicing since some methods (i.e., TVUS) may not be readily available and affordable in resource-poor settings.
Conclusions
This study concluded that the Bishop score was superior in predicting the response to induction as compared to the cervical length measured by transvaginal ultrasonography. In this study, the best cutoff value for Bishop score to predict induction of labor within 6 h was more than four with sensitivity of 69% and specificity of 79%. Similarly, best cutoff value for cervical length to predict induction of labor within 6 h was less than equal to 25 mm with sensitivity of 51% and specificity of 70%.
Ronak Khandelwal
completed MS (Ob-Gyn) in August 2016 from Medical College, Baroda. She is currently working as a Senior Resident in the Department of Obstetrics and Gynecology, UCMS college and GTB Hospital, Delhi University, Delhi.
Compliance with Ethical Standards
Conflict of interest
Ronak Khandelwal, Purvi Patel, Dipa Pitre, Tosha Sheth, and Nandita Maitra have no conflict of interest.
Ethical Approval
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Footnotes
Ronak Khandelwal is a Senior Resident in the Department of Obstetrics and Gynecology, UCMS College and GTB Hospital, New Delhi; Purvi Patel is an Associate Professor in the Department of Obstetrics and Gynecology, Medical College, Baroda; Dipa Pitre is an Associate Professor in the Department of Obstetrics and Gynecology, GMERS Medical College, Baroda; Tosha Sheth is an Associate Professor in the Department of Obstetrics and Gynecology, Medical College, Baroda; Nandita Maitra is an Associate Professor in the Department of Obstetrics and Gynecology, Medical College, Baroda.
References
- 1.Pandis GK, Papageorghiou AT, Ramanathan VG, et al. Preinduction sonographic measurement of cervical length in the prediction of successful induction of labor. Ultrasound Obstet Gynecol. 2001;18:623–628. doi: 10.1046/j.0960-7692.2001.00580.x. [DOI] [PubMed] [Google Scholar]
- 2.Banu S, Jaysahree V, Latha K. Study of comparison of transvaginal cervical length and modified Bishop’s score in predicting the mode of delivery at term following induction of labor. IJCRD. 2016;4(2):134–140. [Google Scholar]
- 3.FOLCROM Trial: Foley Catheter in Rupture of Membranes (FOLCROM). Online: https://clinicaltrials.gov/ct2/show/NCT01973036.
- 4.Bahadori F, Ayatollahi H, Naghavi-Behzad M, et al. Predicting factors on cervical ripening and response to induction in women pregnant over 37 weeks. Med Ultrasonogr. 2013;15(3):191. doi: 10.11152/mu.2013.2066.153.fb1ha2. [DOI] [PubMed] [Google Scholar]
- 5.Cengiz H, Yalvac S, Yavuzcan A, Kandemir O, Haberal A. Prediction of successful induction of labour with dinoprostone in a homogeneous group of patients. S Afr J Obstet Gynaecol. 2012;18(1):19–22. [Google Scholar]
- 6.Bastani P, Hamdi K, Abasalizadeh F, et al. Transvaginal ultrasonography compared with Bishop score for predicting cesarean section after induction of Labour. Int J Womens Health. 2011;3:277–280. doi: 10.2147/IJWH.S20387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Park KH, Kim SN, Lee SY, et al. Comparison between sonographic cervical length and Bishop score in preinduction cervical assessment: a randomized trial. Ultrasound Obstet Gynecol. 2011;38(2):198–204. doi: 10.1002/uog.9020. [DOI] [PubMed] [Google Scholar]
- 8.Kanwar SN, Reena P, Priya BK. A comparative study of trans vaginal sonography and modified Bishop score for cervical assessment before induction of labour. Sch J App Med Sci. 2015;3(6B):2284–2288. [Google Scholar]
- 9.Chandran SS, Shivan H, Bharathi D, et al. Comparison of cervical characteristics assessed by TVUS (with and without saline) with digital method in prediction of labour induction outcome: a prospective study. Int J Reprod Contracept Obstet Gynecol. 2015;4(3):634–640. doi: 10.18203/2320-1770.ijrcog20150065. [DOI] [Google Scholar]
- 10.Kehila M, Bougmiza I, Ben Hmid R, et al. Bishop score VS ultrasound cervical length in the prediction of cervical ripening success and vaginal delivery in nulliparous women. Minerva Gynecol. 2015;67(6):499–505. [PubMed] [Google Scholar]
- 11.Abdelazim IA. Sonographic assessment of the cervical length before induction of labour. Asian Pac J Reprod. 2012;1(4):253–257. doi: 10.1016/S2305-0500(13)60087-1. [DOI] [Google Scholar]
- 12.Ezebialu IU, Eke AC, Eleje GU, Nwachukwu CE. Methods for assessing pre-induction cervical ripening. Cochrane Database Syst Rev. 2015;(6):1–31. doi:10.1002/14651858.CD010762.pub2. [DOI] [PMC free article] [PubMed]