Abstract
WHO has recommended use of the partograph, a low-tech paper form that has been hailed as an effective tool for the early detection of maternal and fetal complications during childbirth. Yet despite decades of training and investment, implementation rates and capacity to correctly use the partograph remain low in resource-limited settings. Nevertheless, competent use of the partograph, especially using newer technologies, can save maternal and fetal lives by ensuring that labor is closely monitored and that life-threatening complications such as obstructed labor are identified and treated. To address the challenges for using partograph among health workers, health-care systems must establish an environment that supports its correct use. Health-care staff should be updated by providing training and asking them about the difficulties faced at their health center. Then only the real potential of this wonderful tool will be maximally utilized.
Keywords: Partograph, Partogram, Labor monitoring, Normal labor, Abnormal labor
Introduction
The partograph or partogram has been established as the “gold standard” labor monitoring tool universally. It has recommended by the World Health Organization (WHO) for use in active labor [1]. The function of the partograph is to monitor the progress of labor and identify and intervene in cases of abnormal labor.
Even though the partograph has been utilized for over four decades in obstetric practice, reports of obstructed labor and its serious maternal and fetal sequelae have questioned the efficacy of the partograph at times. Moreover, evidence of efficacy of partograph is equivocal as suggested by a Cochrane review [2]. However, some of the trials studied in this Cochrane review have limitations with respect to the settings, population studied and conduct of labor. The partograph is an “easy-to-use” tool, but if not used correctly it will affect the final outcome.
In this context, we aim to decipher the efficacy and the utility of the partograph in the contemporary conduct of childbirth across all resource settings and health-care personnel and to suggest solutions to further enhance its efficacy in the optimizing labor outcomes.
Evolution of the Partograph
The development of partograph provided health workers a pictorial overview of labor which can identify pathological labor to allow early intervention.
Most guidelines for normal human labor progress are derived from Friedman’s clinical observations of women in labor. In 1954, he introduced the concept of partogram by graphically plotting cervical dilatation against time. The curve obtained was a sigmoid curve. He divided the first stage of labor into latent phase and active phase. Active phase was further divided into acceleration, maximum slope and deceleration. From his observations, he obtained the following values [3].
Progress of spontaneous labor at term
| Parameter | Median | 5th percentile |
|---|---|---|
| Nullipara | ||
| Total duration | 10.1 h | 25.8 h |
| First stage | 9.7 h | 24.7 h |
| Second stage | 33 min | 117.5 min |
| Third stage | 5 min | 30 min |
| Latent phase | 6.4 h | 20.6 h |
| Maximum dilatation rate | 3 cm/h | 1.2 cm/h |
| Descent rate | 3.3 cm/h | 1 cm/h |
| Multipara | ||
| Total duration | 6.2 h | 19.5 h |
| First stage | 8 h | 18.8 h |
| Second stage | 8.5 min | 46.5 min |
| Third stage | 5 min | 30 min |
| Latent phase | 4.8 h | 13.6 h |
| Maximum dilatation rate | 5.7 cm/h | 1.5 cm/h |
| Descent rate | 6.6 cm/h | 2.1 cm/h |
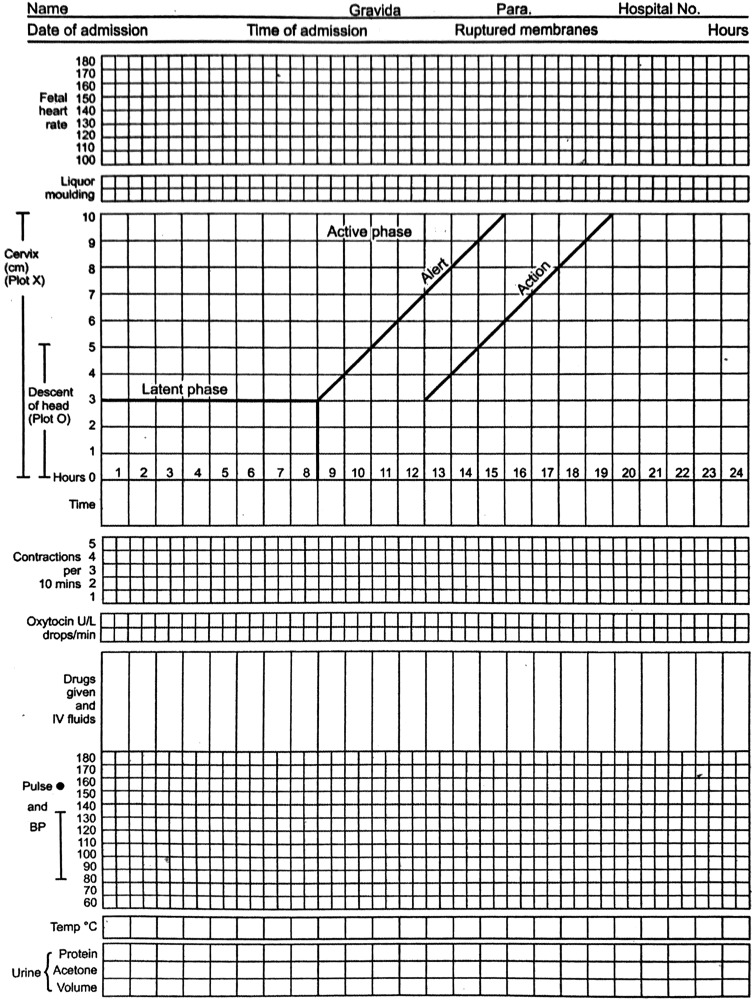
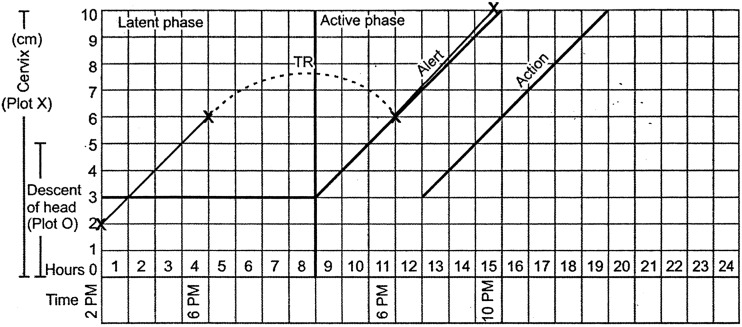
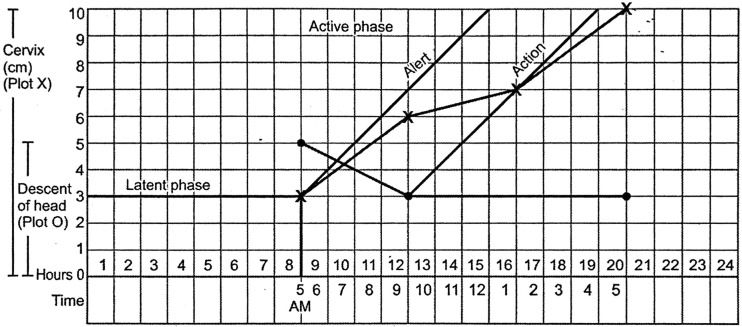
Philpott’s partograph is an improved version of the labor curve. He introduced the alert line and action line. In 1987, WHO launched the safe motherhood initiative, since then WHO has published three different types of partographs. The first of these partograms also known as composite partograph includes latent phase of 8 h and an active phase starting at 3-cm cervical dilatation. It has an alert line with a slope at 1 cm/h and the action line 4 h to the right and parallel to alert line. It also provides space for recording descent of fetal head, maternal condition, fetal condition and medicines administered (Fig. 1).
Fig. 1.
WHO composite partograph
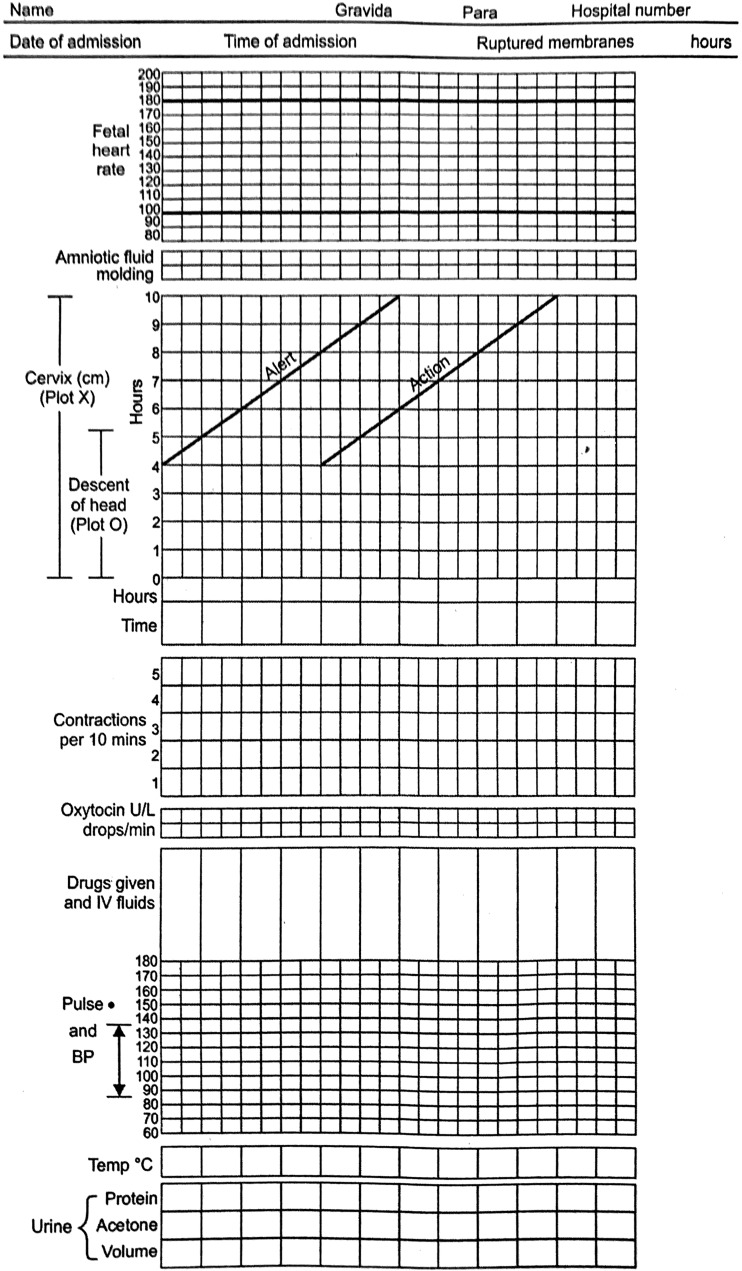
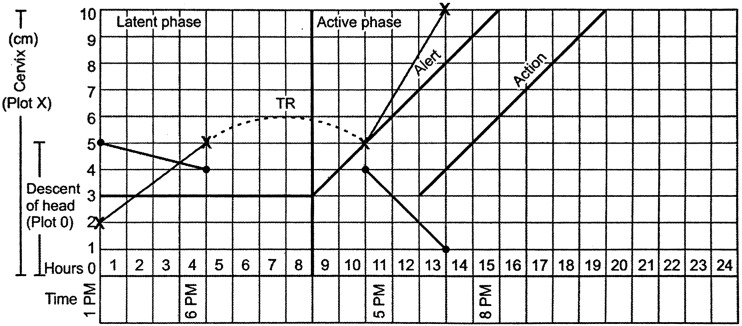
WHO modified the partograph in 2000, the latent phase was excluded, and the active phase commenced at 4-cm cervical dilatation [4]. The other features remained the same. The reason for excluding the latent phase was more likelihood of interventions due to prolonged latent phase which was overdiagnosed. There was also difficulty reported in transferring the dilatation from latent phase to active phase (Fig. 2).
Fig. 2.
WHO modified partograph 2000
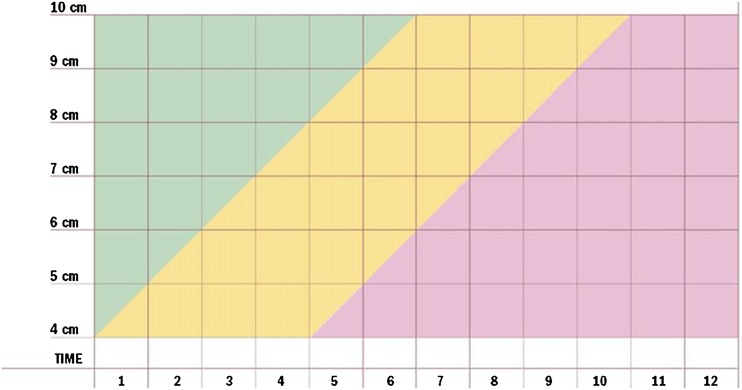
WHO further modified the partograph for the third time. This simplified partograph is color-coded. The area to the left of the alert line is colored green representing the normal progress. The area to the right of action line is colored red indicating dangerously slow progress. The area between the alert and action line is colored amber indicating the need for greater vigilance [5] In the trial conducted at Vellore, simplified partogram was rated more user-friendly over composite partogram (Fig. 3).
Fig. 3.
WHO simplified partograph
The graph section of composite partograph [6]:
A partogram is used to record all observations made when the woman is in labor. It records the following points.
The progress of labor is monitored by cervical dilatation, descent of head and uterine contractions
The fetal condition is monitored by fetal heart rate, color of amniotic fluid and molding of the fetal skull
Maternal condition is assessed by pulse, BP, temperature, urine output and urine for protein and acetone
A separate space is given to enter drugs, IV fluids and oxytocin
Progress of Labor
Cervical Dilatation
The central feature of the partogram is a graph where cervical dilatation is plotted. Along the left side, there are squares from 0 to 10, each representing 1-cm dilatation. Along the bottom of graph are numbers 0–24 each presenting 1 h.
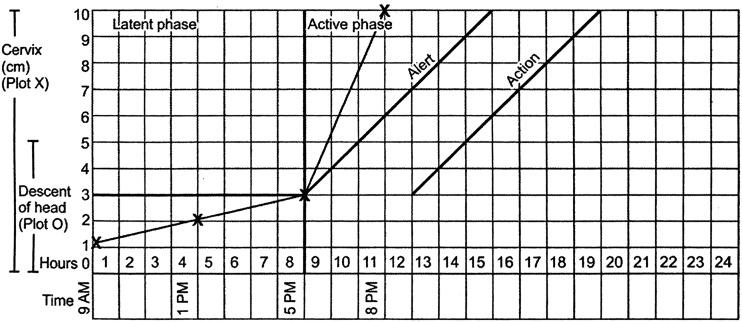
The first stage of labor is divided into latent and active phase. The latent phase is from 0 to 3 cm, and it lasts up to 8 h. The active phase is from 3 to 10 cm (full cervical dilatation). The dilatation of cervix is plotted with “x.”
When a woman is admitted in the active phase, the cervical dilatation is plotted on the alert line. If progress of labor is satisfactory, the plotting of cervical dilatation will remain on the left of alert line (Fig. 4).
Fig. 4.
Normal progress of labor
When woman is admitted in the latent phase, dilatation between 0 and 3 cm should be plotted in latent phase. But when woman goes into active phase, the recording must be transferred to the alert line as shown by the broken line (Fig. 5).
Fig. 5.
Transferring dilatation onto the alert line in the active phase of labor
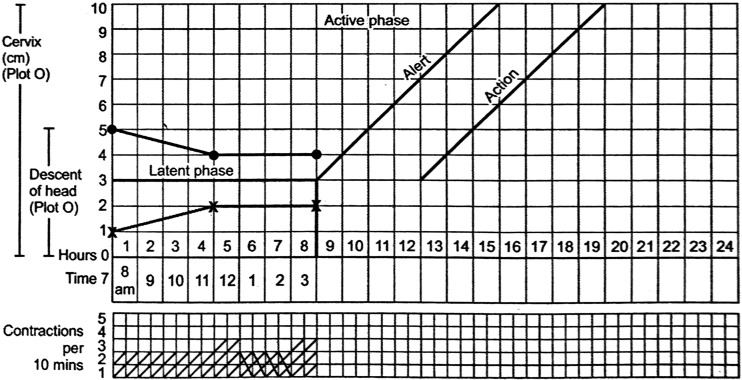
Descent of Fetal Head
Descent of the head should always be assessed by abdominal examination before doing a vaginal examination as the large caput may give a false judgment about the station. The level of the fetal head by abdominal palpitation is expressed in terms of fifths above the brims.
On the left side of the graph is the word descent with numbers from 5 to 0. Descent is plotted with “O” on cervicograph (Fig. 6).
Fig. 6.
Plotting descent of the head
Uterine Contractions
Below the cervical dilatation, there is a space for recording uterine contractions per 10 min and the scale is numbered from 1 to 5. Each square represents one contraction. So if two contractions are felt in 10 min, two squares are shaded. Duration of contraction is indicated by the following symbols: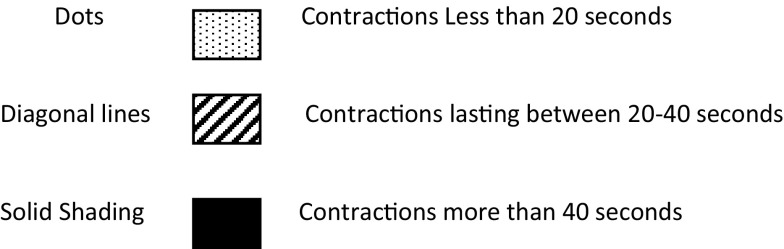
The Fetal Condition
Fetal Heart Rate
Immediately below the patient’s identification details, there is fetal heart rate record. The scale for fetal heart rate ranges from 100 to 180 beats/min.
Liquor
Below the fetal heart rate, there are two rows, and the first is for liquor. Once the membranes rupture, the color of amniotic fluid is noted
If the membranes are intact, write ‘I’
If the liquor is clear, write ‘C’
If the liquor is meconium-stained, write ‘M’
If the liquor is absent, write ‘A’
Molding
The row below the liquor is assigned for molding. Increasing molding with high head in pelvis is an ominous sign. It is recorded as follows.
0 Bones are separated, and the sutures can be felt easily.
- +
Bones are just touching each other
- ++
Bones are overlapping
- +++
Bones are overlapping severely
Maternal Condition
All the recordings for the maternal condition are entered at the foot of the partograph below the recording of uterine contraction. Maternal vital signs such as temperature, pulse, BP, urine output and urine for protein and acetone are monitored.
Importance of alert and action lines
In normal labor during the active phase, plotting of cervical dilatation will remain on the left of or on the alert line. If it moves to the right of the alert line, labor may be prolonged. In this situation, transfer the patient if facility for emergency intervention is not available. Transfer allows adequate time for assessment or intervention till she reaches the action line. Action line is 4 h to the right of alert line. Assess the cause of slow progress, and take necessary action. Action should be taken in a place where facility for dealing with obstetric emergencies is available.
Use of Partogram in Different Resource Settings
The partogram has been heralded as one of the most important advances in modern obstetric care. WHO advocates its use as a necessary tool in the management of labor and recommends its universal use during labor. In under-resourced settings, prolonged labor and delay in decision-making are important causes of adverse obstetric outcomes. Owing to resource constraints in such settings, it is usually not possible to monitor each woman continuously throughout the duration of labor. In such settings, the partogram serves a simple and inexpensive tool to monitor labor in a cost-effective way. However, some health-care practitioners, especially in high-income countries, have questioned its effectiveness. For example, Walraven has suggested that use of the partogram can be an unnecessary interference in clinical work. The present Cochrane review suggests use of a partogram as part of routine care is not associated with improvements in the rates of cesarean section, instrumental vaginal delivery or Apgar scores [2]. Partogram use may have some utility in low-resource settings. Additional evidence is needed to definitively determine the efficacy of partogram use.
Abnormal Labor Patterns
Abnormal labor includes the following patterns.
Prolonged latent phase
Protraction disorders
Arrest disorders
Precipitate labor
Prolonged Latent Phase
The average duration of latent phase is 6.4 h in primiparas and 4.8 h in multiparas. An abnormally long latent phase is defined as 20 h in nulliparous and 14 h in multiparous patients. The treatment includes therapeutic rest, oxytocin, amniotomy and cervical ripening (Fig. 7).
Fig. 7.
Prolonged latent phase
Protraction Disorders
Protracted disorders refer to a series of events including protracted active phase dilatation and protracted descent. Cervical dilatation rate of <1.2 cm/h for primiparas and <1.5 cm/h for multiparas is considered as protracted. Descent <1 cm/h in primiparas and <2 cm/h in multiparas is protracted descent.
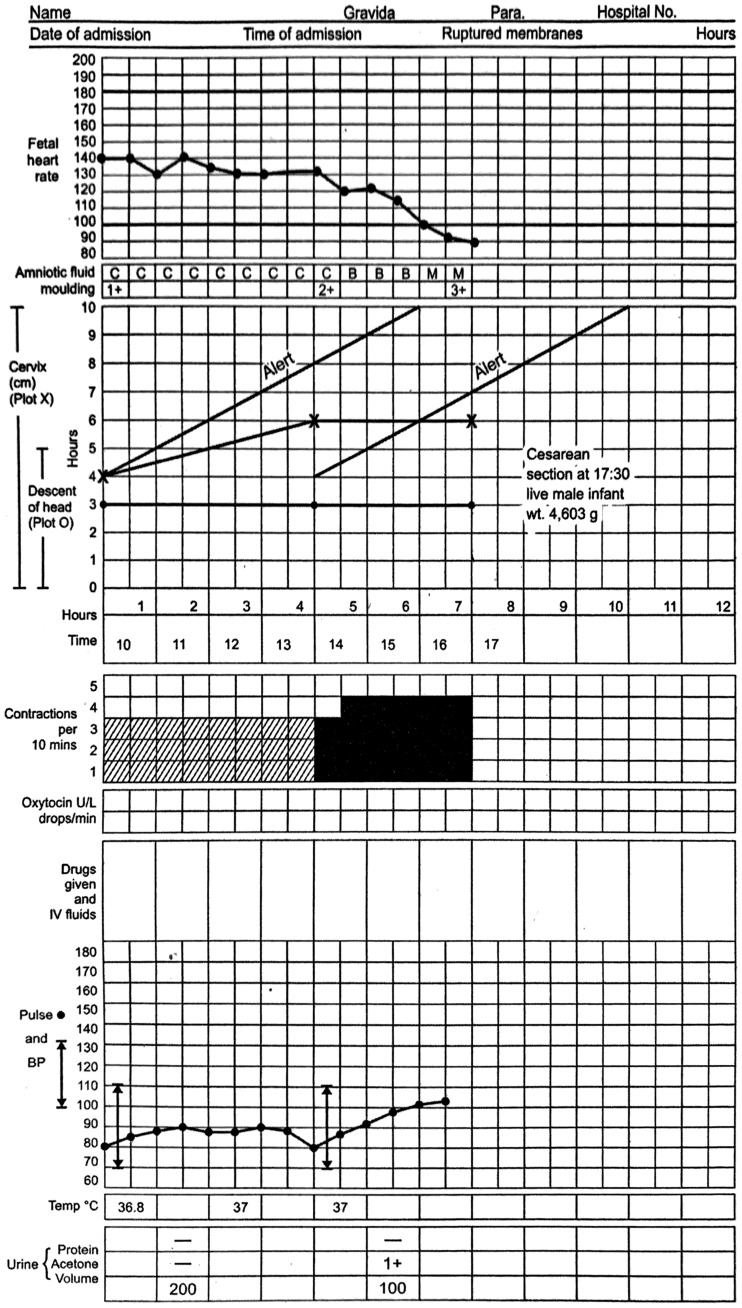
Arrest Disorders
They include secondary arrest of dilatation that means no progress of cervical dilatation for more than 2 h and arrest of descent that is fetal head does not descend for more than 1 h. If there is no descent in second stage, it is labeled as failure of descent (Figs. 8, 9).
Fig. 8.
Arrest of dilatation
Fig. 9.
Arrest of descent
Precipitate Labor
Labor which is completed within 3 h is called precipitate labor.
Efficacy of the Partograph
As stated earlier, the Cochrane review of the partograph seems to conclude that evidence reveals that partograph use in labors affects the improvement in clinical outcomes partially. Contrary to this, other studies conclude that partograph use results in shorter labors and better maternal and fetal outcomes [7].
Health-care providers in labor wards experienced the modified partograph to be much more user-friendly [8], as compared to the composite partograph in which they found the latent phase difficult to complete. The modified partograph was found to significantly improve various intrapartum outcomes like a reduced cesarean section rate, augmentation of labor and admissions to neonatal unit as compared to the composite partograph in especially low-resource settings [8].
Overall completion of the partograph to the expected standards is poor which affects its use in clinical practice. Analysis of completed partographs shows that the cervical dilatation and fetal heart rate are usually duly filled as compared to maternal well-being findings [9]. Obviously, this is due to fact that some sections are easier to complete due to equipment availability or better understanding of the partograph, rather than the tool itself [10]. Some obstetricians view the partograph as difficult or time-consuming to complete [9], and evidence shows that other cadres of staff can complete the partograph effectively [11].
There is no doubt as envisioned by its founders, and partograph still works as a trigger for referral and transfer [12] and hence fulfills its primary objectives. Unfortunately, evidence related to augmentation of labor based on partograph findings is limited and on many an occasion there is failure to act on an evident finding shown on a partograph. One reality is that the utility of the partograph as a document of communication tool during the “handover of care” is minimal [8] and transfers to tertiary units are sent without the partograph; hence, vital information about progress of labor thus far is not known [13].
Evidence is conflicting about the utility of the partograph in general, although studies in low-resource settings suggest that it may have positive impact [14]. Obviously, no detrimental effect of partograph use to outcome is known [2]. In some studies, use of partograph has resulted in fewer vaginal examinations, reduced length of labor and referral reflected as betterment in quality of care during labor and delivery [15].
Generally, midwives and doctors have expressed positive attitudes toward the use of the partograph [16]. However, it is not always that positive attitudes translate into the actual partograph use in practice, which may be due factors like availability, time, workload and hospital policy [17].
An extremely vital view we wish to put forth is that health workers can take individual responsibility for labor management by using the partograph [18]. This will surely lead to better communication and working, enabling appropriate and timely decision-making and resulting in improved outcomes. Training and supervision of partograph use will enable both wider and standardized use [19]. Hence, partograph use should be an essential part of any obstetric residency or midwife training program.
Although there is no evidence of the cost-effectiveness of the partograph in the literature, we believe that the partograph is a cost-effective tool in any resource setting due to the minimal costs being involved.
Even though the partograph is globally accepted, the prevalence of its use in reality is variable across the world. The reasons for this variation are multiple like lack of or limited availability, busy obstetric units with less staff and finally absence of a uniform policy or guideline for its mandatory implementation [20]. The partograph is mostly used in urban tertiary public health-care facilities by professionally qualified and trained staff as these setups have both adequate human resource and funding. More importantly, these centers have a protocol mandating its use in all labors [21]. Ongoing supervision and support will improve partograph usage [12]. Additionally, regular audits will enhance greater usage and accuracy in labor monitoring [22].
Partograph in Labor: Challenges and Solutions
The greatest challenge in partograph use is to enhance its effective implantation in the management of all labors universally. Unfortunately, the partograph is still not considered as mandatory or central in routine care of all laboring women [23]. This may be because of lack of commitment and inconsistent acceptability for the usage of the partograph in labor rooms. At present though a majority of health-care workers do possess positive attitudes toward the partograph, a few challenges need to be tackled to ensure a favorable environment. These challenges are support by the health system, availability of resources, competence in use and monitoring and evaluation of the partograph in practice.
Positive validation, facility level guidance, evaluation and audit of partographs from experienced seniors and supervisors will enhance the value of the partograph in clinical practice. Adequate availability of resources, (i.e., the partograph and accessory equipment) will result in completion, which is essential to ensure consistent use, but sadly this is still lacking. Individualized training improves knowledge about the partograph [24], but the use of multidisciplinary training strategies results in understanding of roles and promotes coordinated team work [25]. Hands-on training methods improve patient outcomes [26, 27]. All staff members providing care for women in labor should be trained and regularly updated in partograph use. Training should consist of completion and decision-making, like when to start the partograph, when to take action and appropriate referral. A limitation with the partograph use in current practice is the failure to evaluate the tool at facility level in terms of outcomes. This is paramount in evaluating the level of impact partograph use has on care provision and referrals as well as on specific labor outcomes. Hence, if positive outcomes from partograph use are observed and informed to all involved in the birthing process, then certainly it will be embedded into routine labor ward practice.
Paperless Partograph
Even after the WHO simplified the partograph, it is rarely used in rural parts of India. The main reasons being it may be too time-consuming for overburdened doctors and may be too complicated for the birth attendants present in rural settings. Therefore, there is an urgent need to make the partograph more user-friendly.
Dr. A.K Debdas from India has proposed a new low-skill method called paperless partogram to adapt to local needs [28]. In the paperless partograph, the birth attendant calculates two times, an ALERT ETD (estimated time of delivery) and an ACTION ETD.
The ALERT calculation uses the principal that cervix dilates 1 cm/h when woman is in active phase. So the birth attendant simply adds 6 h to the time at which a woman becomes 4 cm dilated. This way ALERT ETD is calculated. To calculate ACTION ETD, 4 h is added to ALERT ETD. Both the timings are written on patient’s indoor paper. The ACTION ETD is circled in red.
At the time of ALERT ETD, if the patient has not delivered and the current setup lacks the operative facility, then the arrangement for transportation should be made. At the time of ACTION ETD, the woman is at risk of prolonged labor. So an immediate action must be taken to deliver her promptly.
This strategy is cheap and easy to use. It takes only few seconds for calculation, requires only basic addition and has the potential for preventing prolonged labor.
ePartograph
Jhpiego and the Johns Hopkins Center for Bioengineering Innovation and Design (JHU-CBID) have developed the ePartograph, a handheld device and software platform based on the current partograph recommended by the World Health Organization [29].
The device, which incorporates traditional best practices and clinical algorithms from the paper partograph, facilitates broader use and expands the benefits of the paper-based version through the following improvements:
Features efficient data entry, automatic plotting of observations
Provides instant graphing of data
Reminds providers when to measure and record critical observations
Stores multiple patient data in one device
Provides indicators when complications arise
Limits retroactive data entry after delivery (a current practice that reduces the current paper partograph into a mere recording tool)
Transmits data to off-site experts who can provide guidance and support
Jhpiego and JHU-CBID engineers are working with end-users to refine the device interface and gather data about user needs and preferences for device improvements, manufacturing and additional field studies.
The Jiv Daya Foundation launched the India Maternal Health Initiative aimed to strengthen hospital based care of mothers and newborns during labor and delivery and partnered with over 15 hospitals all over India [30]. The Foundation has devised an electronic partograph system to facilitate the early detection of labor abnormalities and initiation of timely interventions, as unmanaged complications often result in preventable death.
Mobile Partograph
Founded in 2002 out of MIT’s Media Lab, Dimagi is a software social enterprise that develops technologies to improve service delivery in underserved communities.
Through an iterative process of user-focused design, Dimagi’s technology aims to reduce the partograph’s barriers by focusing on improving interpretability, applicability, time, and minimizing complexity. The mobile partograph acts as a job aid by prompting intrapartum care providers to report the necessary information at the appropriate time while calculating and producing timely reports on labor status.
Health clinics receive partographs that are filled out after the labor, and data take too long to reach decision makers such that up-to-date statistics are not always available. Real-time data reporting enables supervisors to detect data irregularities and observe whether recommended actions were taken, including identifying providers whose clinical practices in labor monitoring and management need improvement. Live partograph reports enable district health centers and health authorities to view and monitor complete labor records, including the full computer-plotted partograph. Monthly and quarterly reports allow health administrators to assess labor monitoring, timely provision of care for abnormal labors, and maternal and fetal health outcomes. Key alerts on emergency action can be sent to supervisors, and/or referral facilities, who can provide immediate backup support on appropriate next steps.
Many intrapartum care providers find the paper partograph challenging to fill in and see it as a burden rather than a job aid, filling it out retrospectively. Easy input of labor monitoring data (e.g., cervical dilation, fetal heart rate, status of membranes, amniotic fluid, etc.) in alphanumeric form improves usability as compared to paper-based form. Data are displayed in graphical or nongraphical format for use by a wide range of health workers. Minimal training is needed due to embedded training videos and quizzes. An integrated library of obstetric clinical protocols, such as WHO and national guidelines, prompts information entry at appropriate times. Automatic alerts from data collected during labor and delivery facilitate workflow, and warnings when data entered fall beyond set parameters support intrapartum care providers to maintain data accuracy. Up-to-date information about available referral facilities informs decision-making to transfer a patient.
Dimagi launched this mobile partograph in India as a mobile application in both English and Hindi and was tried in few health-care facilities in 2015 [31]. Through this mobile application, key alerts on urgent emergency action are sent to supervisors, staff and/or referral facilities, who can provide backup advice on appropriate next steps by making immediate phone calls to providers. Monthly and quarterly reports are generated for health administrators to assess labor monitoring, timely provision of care for abnormal labors, and maternal and fetal health outcomes.
Recommendations for Clinical Practice
We would like to make the following recommendations for clinical practice:
The partograph should be the main labor record, and a policy/guidance should be issued at all facility levels for health-care workers’ reference.
The modified partograph is more user-friendly as compared to the composite partograph.
The partograph and the accessory equipment needed for its completion should be provided in all labor wards.
Effective supervision by health-care workers/managers with training and clinical experience in partograph use is necessary for sustaining successful implementation.
Regular training and updating should be provided for all health-care workers using the partograph, using proven effective training techniques, e.g., multidisciplinary, practical/clinical application.
Training should include understanding of when to commence the partograph, decision-making based on findings and understanding of role.
Monitoring and audit of the partograph in practice, including completion, decision-making and referral and outcomes, are recommended.
Conclusion
Competent use of the partograph can save maternal and fetal lives by ensuring that labor is closely monitored and that life-threatening complications such as obstructed labor are identified and treated. To address the challenges for using partograph among health workers, health-care systems must establish an environment that supports its correct use. Health-care staff should be updated by providing training and asking them about the difficulties faced at their health center. Then only the real potential of this wonderful tool will be maximally utilized.
Dr. Asha R. Dalal
is the Consultant and Head of Department at the HN Reliance Foundation Hospital, Mumbai. She was the former Professor and Head of the Department at the TN Medical College and the BYL Nair Hospital, Mumbai. She was the President of AMOGS (Association of Maharashtra Obstetrics and Gynecological Societies) in 2014–2016, a UNICEF expert in PPTCT, member of the State Task Force on maternal death review, an ex-ad hoc Chairman of the Board of Studies in Ob/Gyn, Mumbai University, and has also been a National editor of The Journal of Obstetrics and Gynecology of India between 2011 and 2014. She has also been an ex-member of the managing committees of the MOGS and the IAGE. She has also been the ex-secretary of the west zone chapter of ISOPARB. Dr. Dalal has been a teacher and examiner at the undergraduate and postgraduate level in Obstetrics and Gynecology at the Mumbai University and the MUHS for more than three decades. She has been an inspector for the MCI on several occasions. She has had an excellent academic career with gold medals in Obstetrics and Gynecology at the third MBBS and the DGO examinations. She stood first at the MD (Ob/Gyn) examinations as well. Dr. Dalal has participated as an invited speaker innumerable times at national and international conferences. She has organized three international workshops in endoscopic surgery and has participated as faculty in several operative workshops all over the country. She has to her credit more than thirty publications in esteemed journals. Dr. Dalal has a deep interest in endoscopic surgery, infertility and high-risk pregnancy. Her personal hobby though is reading—both fiction and nonfiction.
Compliance with Ethical Standards
Conflicts of interest
The authors declare that they have no conflict of interest.
Footnotes
Professor Asha R. Dalal is the MD, DGO, Consultant Obstetrician and Gynecologist, Head in Department of Obstetrics and Gynecology, Sir HN Reliance Foundation Hospital and Research Centre, Mumbai, India, and Dr. Ameya C. Purandare, MD, DNBE, FICOG, FCPS, DGO, DFP, MNAMS, Consultant Obstetrician and Gynecologist in Purandare’s Chowpatty Maternity and Gynecological Hospital, K J Somaiya Medical College and Superspeciality Hospital, Bhatia General Hospital, Masina Hospital, Apollo Spectra Hospital, Police Hospital, Mumbai.
References
- 1.World Health Organization . WHO recommendations for augmentation of labor. Geneva: WHO; 2014. [Google Scholar]
- 2.Lavender T, Hart A, Smyth RMD. Effect of partogram use on outcomes for women in spontaneous labor at term. Cochrane Database of Systematic Reviews. 2013 doi: 10.1002/14651858.CD005461.pub4. [DOI] [PubMed] [Google Scholar]
- 3.Friedman EA. Primigravid labor: a graphicostatistical analysis. Obstet Gynecol. 1955;6:567. doi: 10.1097/00006250-195512000-00001. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization . Managing complications in pregnancy and childbirth. Geneva: WHO; 2000. [Google Scholar]
- 5.Magon N. Partograph revisited. Int J Clin Cases Investig. 2011;3(1):1:6. [Google Scholar]
- 6.The Partograph. A Managerial tool for the prevention of prolonged labor. The World Health Organization, Geneva; 1998 (section 2, A User’s manual).
- 7.Tayade S, Jadhao P. The impact of use of modified who partograph on maternal and perinatal outcome. Int J Biomed Adv Res. 2002;3(4):256–262. [Google Scholar]
- 8.Lavender T, Omoni G, Lee K, et al. Student nurses experiences of using the partograph in labor wards in Kenya: a qualitative study. Afr J Midwifery Womens Health. 2011;5(3):117–122. doi: 10.12968/ajmw.2011.5.3.117. [DOI] [Google Scholar]
- 9.Yisma E, Dessalegn B, Astatkie A, et al. Completion of the modified World Health Organization (WHO) partograph during labor in public health institutions of Addis Ababa, Ethiopia. Reprod Health J. 2013;10(23):1–7. doi: 10.1186/1742-4755-10-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rakotonirina JEC, Randrianantenainjatovo CH, Elyan Edwige BB, et al. Assessment of the use of partographs in the region of Analamanga. Int J Reprod Contracept Obstet Gynecol. 2013;2(3):257–262. doi: 10.5455/2320-1770.ijrcog20130901. [DOI] [Google Scholar]
- 11.Fatusi AO, Makinde ON, Adetemi AB. Evaluation of health workers’ training in use of the partogram. Int J Gynecol Obstet. 2008;100(1):41–44. doi: 10.1016/j.ijgo.2007.07.020. [DOI] [PubMed] [Google Scholar]
- 12.Fahdhy M, Chongsuvivatwong V. Evaluation of World Health Organization partograph implementation by midwives for maternity home birth in Medan, Indonesia. Midwifery. 2005;21(4):301–310. doi: 10.1016/j.midw.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 13.Nkyekyer K. Peripartum referrals to Korle Bu teaching hospital, Ghana—a descriptive study. Trop Med Int Health. 2000;5(11):811–817. doi: 10.1046/j.1365-3156.2000.00640.x. [DOI] [PubMed] [Google Scholar]
- 14.Orji EO, Fatusi AA, Maknde NO, et al. Impact of training on the use of partograph on maternal and perinatal outcome in peripheral health centers. J Turk Ger Gynecol Assoc. 2007;8(2):148–152. [Google Scholar]
- 15.Javad I, Bhutta S, Shoaib T. Role of the partogram in preventing prolonged labor. J Pak Med Assoc. 2007;57(8):408–411. [PubMed] [Google Scholar]
- 16.Badjie B, Kao C-H, Gua M-l, Lin K-C. Partograph use among midwives in the Gambia. Afr J Midwifery Womens Health. 2013;7(2):65–69. doi: 10.12968/ajmw.2013.7.2.65. [DOI] [Google Scholar]
- 17.Qureshi ZP, Sekadde-Kigondu C, Mutiso SM. Rapid assessment of partograph utilization in selected maternity units in Kenya. East Afr Med J. 2010;87(6):235–241. doi: 10.4314/eamj.v87i6.63081. [DOI] [PubMed] [Google Scholar]
- 18.Orhue AAE, Aziken ME, Osemwenkha AP. Partograph as a tool for team work management of spontaneous labor. Niger J Clin Pract. 2012;15(1):1–8. doi: 10.4103/1119-3077.94087. [DOI] [PubMed] [Google Scholar]
- 19.Ogwang S, Karyabakabo Z, Rutebemberwa E. Assessment of partogram use during labor in Rujumbura Health sub district, Rukungiri District, Uganda. Afr Health Sci. 2009;9(1):s27–s34. [PMC free article] [PubMed] [Google Scholar]
- 20.Okokon IB, Oku AO, Agan TU, et al. An evaluation of the knowledge and utilization of the partogragh in primary, secondary, and tertiary care settings in Calabar, South-South Nigeria. Int J Fam Med. 2014 doi: 10.1155/2014/105853. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Opiah MM, Ofi AB, Essien EJ, et al. Knowledge and utilization of the partograph among midwives in the Niger Delta Region of Nigeria. Afr J Reprod Health. 2012;16(1):125–132. [PubMed] [Google Scholar]
- 22.Mercer WM, Sevar K, Sadutshan TD. Using clinical audit to improve the quality of obstetric care at the Tibetan Dalek Hospital in North India: a longitudinal study. Reprod Health. 2006;3(4):1–4. doi: 10.1186/1742-4755-3-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Groeschel N, Glover P. The partograph. Used daily but rarely questioned. Aust J Midwifery. 2001;14(3):22–27. doi: 10.1016/S1445-4386(01)80021-5. [DOI] [PubMed] [Google Scholar]
- 24.Prem A, Smitha MV. Effectiveness of individual teaching on knowledge regarding partograph among staff nurses working in maternity wards of selected hospitals at Mangalore. Int J Recent Sci Res. 2013;4(7):1163–1166. [Google Scholar]
- 25.Robertson B, Schumacher L, Gosman G, et al. Crisis-based team training for multidisciplinary obstetric providers. Empir Investig. 2009;4(2):77–83. doi: 10.1097/SIH.0b013e31819171cd. [DOI] [PubMed] [Google Scholar]
- 26.Guise GM, Segal S. Teamwork in obstetric critical care. Best practice & research. Clin Obstet Gynaecol. 2008;22(5):937–951. doi: 10.1016/j.bpobgyn.2008.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Siassakos D, Crofts JF, Winter C, et al. The active components of effective training in obstetric emergencies. BJOG. 2009;116(8):1028–1032. doi: 10.1111/j.1471-0528.2009.02178.x. [DOI] [PubMed] [Google Scholar]
- 28.Debdas AK. Paperless partogram. 41st annual scientific session 2008; Sri Lanka College of Obstetrics and Gynecologists: SLJOG: vol 30 2008; 1(1):124.
- 29.Jhpiego. The E-Partogram. Retrieved on May 10, 2012 from http://savinglivesatbirth.net/summaries/35.
- 30.India Maternal Health Initiative by Jiva Diya Founation. http://www.jivdayafound.org/maternal-health/.
- 31.Chhugani M, Khalid M, James MM, et al. Experiences of nurses on implementation of a mobile partograph: a novel tool supporting safer deliveries in India. Int J Nurs Midwif Res. 2016;3(4):32–39. [Google Scholar]