Abstract
Although the Nobel Prize for the discovery of nitric oxide (NO) dates back almost 20 years now, the knowledge about cGMP signaling is still constantly increasing. It looks even so that our understanding of the role of the soluble guanylyl cyclase (sGC) and particulate guanylyl cyclase (pGC) in health and disease is in many aspects at the beginning and far from being understood. This holds even true for the therapeutic impact of innovative drugs acting on both the NO/sGC and the pGC pathways. Since cGMP, as second messenger, is involved in the pathogenesis of numerous diseases within the cardiovascular, pulmonary, renal, and endocrine systems and also plays a role in neuronal, sensory, and tumor processes, drug applications might be quite broad. On the 8th International Conference on cGMP, held in Bamberg, Germany, world leading experts came together to discuss these topics. All aspects of cGMP research from the basic understanding of cGMP signaling to clinical applicability were discussed in depth. In addition, present and future therapeutic applications of cGMP-modulating pharmacotherapy were presented (http://www.cyclicgmp.net/index.html).
Keywords: cGMP, Guanylyl cyclases, Phosphodiesterases, Nitric oxide, Natriuretic peptides
Introduction
Roughly 170 scientists including the two Nobel laureates Ferid Murad and Stefan Hell, from all over the world, from academia and industry including not only basic and translational researchers but also drug discovery experts and clinical scientists, convened at Bamberg (Fig. 1), close to the old medieval city center and UNESCO World Heritage. Within almost three fully packed days, more than 40 talks and about 55 posters were presented and discussed. The meeting was held in an inspiring atmosphere also providing completely novel insights and understandings of “cGMP, generators, effectors, and therapeutic implications” (http://www.cyclicgmp.net/pages/2017/program.html).
Fig. 1.
Participants of the 8th International Conference on cGMP in front of Welcome Hotel Congress Venue at Bamberg, Germany
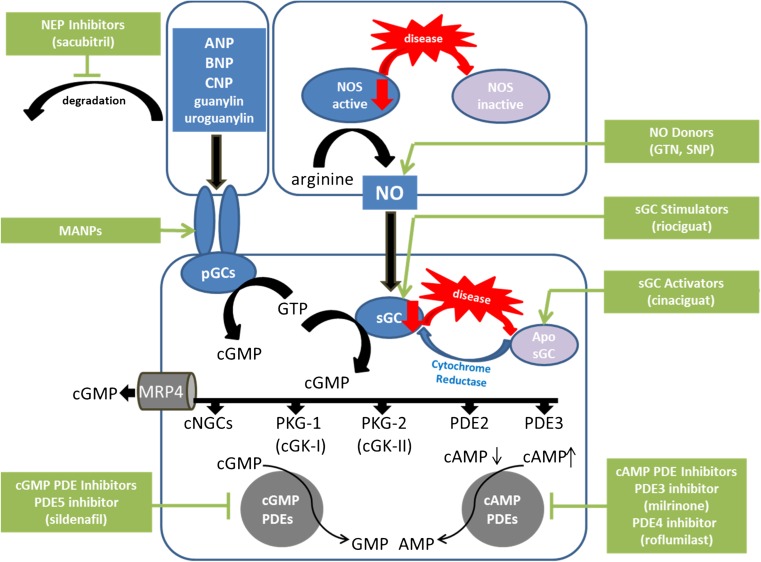
Before deep-diving into cGMP (cyclic guanosine 3′,5′ monophosphate) signaling and its role in physiology and pathophysiology, a brief introduction into this field should be given. As a key intracellular second messenger, cGMP is involved in the regulation of many cellular functions. Intracellular levels of cGMP are tightly regulated. Synthesis of cGMP by soluble guanylyl cyclases (sGC) and particulate guanylyl cyclases (pGC) and degradation by phosphodiesterases (PDE) provide the basis for maintenance of body homeostasis. Consequently, dysregulation of cGMP signaling is likely to induce pathological states in many organs (Rainer and Kass 2016; Kraehling and Sessa 2017; Aka et al. 2017; Ben Aissa et al. 2016). Investigation of cGMP turnover by cyclases and phosphodiesterases as well as knowledge of cGMP effectors and their downstream targets are of key importance to understand the molecular physiology and pathophysiology of this signaling cascade. Knowledge of basic mechanisms is, thus, a prerequisite for the development of drugs within this pathway which have substantial therapeutic implications and help to improve the life of patients (Oettrich et al. 2016; Buglioni and Burnett 2016).
The production of cGMP from GTP results from the enzymatic activity of sGC and pGC. Whereas sGC is stimulated by nitric oxide (NO) formed from L-arginine by NO synthases (eNOS, nNOS, iNOS), pGCs are activated by peptides (such as ANP, BNP, CNP, guanylin, and uroguanylin) and other mechanisms (Koesling et al. 2016; Kuhn 2016). Several effectors are known to convey the cGMP signal: cGMP-dependent protein kinases (cGK or PKG), PDE, and cGMP-gated ion channels. In addition, cGMP extrusion by MRP4 has been shown to actively decrease the intracellular cGMP levels (Krawutschke et al. 2015).
Pharmacologically, cGMP signaling can be increased by either stimulation of cGMP production or inhibition of cGMP degradation. Organic nitrates and NO donors like glyceryl trinitrate, sodium nitroprusside (SNP), or molsidomine have been long known to release NO spontaneously or after metabolic conversion. Applications for NO donors include patients suffering from coronary heart disease to treat angina pectoris as well as patients suffering from hypertensive crisis and other emergencies requiring rapid relaxation of smooth muscle cells. As a member of a novel class of drugs, riociguat effectively and potently increases cGMP production by selectively stimulating sGC. This compound has been approved for the treatment of pulmonary hypertension (Ghofrani et al. 2017). Sildenafil, the first selective PDE5 inhibitor, was introduced approximately 20 years ago for the treatment of erectile dysfunction and was later on also approved for the treatment of pulmonary hypertension (Boolell et al. 1996; Doumas et al. 2015).
The options to target pGCs pharmacologically are still limited. The introduction of sacubitril/valsartan, a dual-acting angiotensin receptor neprilysin inhibitor, which augments the effects of natriuretic peptides, was shown to be effective in heart-failure patients (Jhund et al. 2015; Singh et al. 2017). Figure 2 provides an overview on some aspects of NO/cGMP signaling and pharmacological interventions.
Fig. 2.
Schematic overview on NO/cGMP and natriuretic peptide-pGC signaling and current pharmacological interventions. For further details on the exponentially growing complexity and diversity of cGMP signaling in health and disease, the reader is referred to the main text
Due to the substantial body of new data and space constraints, it is not possible to discuss all topics here in this report. Therefore, the authors apologize to our colleagues whose work is not covered or not covered comprehensively here. For the complete publication of all abstracts, the reader is referred to BMC Pharmacology and Toxicology, volume (Reference not yet available, to be included after publication of abstracts in BMC).
Cardiovascular function and heart diseases
Originally, NO was discovered as a signaling molecule in the cardiovascular system leading to relaxation of the blood vessels. Caused by the still very high unmet medical need in cardiovascular diseases, there are substantial efforts in research, drug discovery, and clinical development ongoing; these are aimed at fully understanding the role of cGMP in the cardiovascular system and at fully exploiting the therapeutic potential of cGMP-enhancing drugs for the treatment of cardiovascular diseases and heart failure. This is even more important since not only both NO/sGC and natriuretic peptide/pGC but also PDEs (e.g., PDE2, PDE5, and PDE9) affect cardiovascular function. Therefore, cardiovascular aspects including compartmentalization and GC/PDE interconnection were among the broadly discussed topics in talks and poster sessions.
Ischemia reperfusion injury, myocardial infarction, and acute heart failure
A major problem in the treatment of patients undergoing lysis therapy after myocardial infarction is due to damage resulting from reperfusion of the occluded vessel. Several members of the NO/cGMP cascade have been shown to influence cardiac ischemia/reperfusion (I/R) injury. sGC as well as the calcium-activated K+ channel of the BK type (BK channel) play a clear role in the protection against I/R injury (Robert Lukowski, Tübingen). Mice lacking sGC specifically in cardiomyocytes (CM-sGC-KO) were subjected to 300 min ischemia followed by 120 min reperfusion. Although lack of sGC in cardiomyocytes did not influence basal infarct size, the cardioprotective role of sGC became obvious after postconditioning. Pharmacological activation of BK channels also led to cardioprotection and cardiomyocyte-specific deletion of this channel (CM-BKKO), which in these cells is only found in mitochondria, prevented the protective effect. Interestingly, all cGMP-elevating compounds (GC activators, PDE inhibitors) that reduced I/R injury were ineffective in CM-BKKO mice indicating BK channels to be the main downstream target of cGMP signaling.
The role of sGC in atherosclerosis is obvious (Thorsten Kessler and coworkers, München, Lübeck). In a genome-wide association study, a SNP (rs7692387; located within intron 8 of the GUCY1A3 gene) was shown to associate with a higher risk for coronary artery disease (Deloukas et al. 2013). In this study, rs7692387 affected NO-GC α1 mRNA expression. Sixty percent of the Western European population are homozygous carriers of a NO-GC1 risk allele (GG allele) which leads to a reduced mRNA expression of the α1 subunit. rs7692387 seems to modulate gene regulation rather than alter protein function or activity. The mutated region (GG instead of AA) is thought to be part of an enhancer element, and in fact, transcription factors such as IRF8 and ZEB1 were shown to differentially bind to this site. Indeed, ZEB1 binds preferentially to the non-risk allele (A allele), leading to an increase in sGC mRNA transcription and, thus, higher sGC levels (Kessler et al. 2017). From these data, it becomes evident that preservation of sGC/cGMP signaling is critical for the reduction of coronary risk.
Chronic heart failure
Chronic heart failure is still one of the major health burdens worldwide and intense research and development efforts are ongoing to improve outcome in chronic-heart-failure patients. In recent years, our knowledge for heart failure with reduced ejection fraction (HFrEF) is emerging and with Entresto™, a sodium salt complex of the NEP inhibitor sacubitril and the angiotensin AT1 receptor blocker valsartan, a new pharmacological treatment principal has been introduced (Khder et al. 2017). More recently, the novel sGC stimulator vericiguat (Follmann et al. 2017) completed two phase II trials in patients with heart failure, one trial in HFrEF (SOCRATES-reduced, NCT01951625), but also one trial in patients suffering from heart failure with preserved ejection fraction (HFpEF) (SOCRATES-preserved, NCT01951638). Vericiguat showed efficacy in SOCRATES-reduced (Gheorghiade et al. 2015) and a consecutive phase III clinical program (VICTORIA Trial, NCT02861534) was started in September last year. However, the trial in HFpEF patients showed no significant improvement in the primary endpoint which was NT-pro BNP (Filippatos et al. 2017). There is still little understanding of HFpEF and all clinical trials failed so far (Lewis et al. 2017). Therefore, it is mandatory to improve our understanding of HFpEF to investigate how cGMP might contribute to HFpEF and also if sGC stimulators and sGC activators could be effective in HFpEF.
HFpEF is associated with coronary microvascular endothelial activation and oxidative stress (Nazha Hamdani, Bochum). These lead to uncoupling of endothelial nitric oxide synthase, inhibition of NO-dependent signaling from endothelial cells to cardiomyocytes, and reduction of sGC and PKG activity in cardiomyocytes. Reduced PKG-mediated phosphorylation of titin, a giant protein that forms a continuous filament network in the sarcomeres of striated muscle cells, contributes to the high cardiomyocyte stiffness and hypertrophy observed in HFpEF patients, especially in women. Thus, targeting PKG/titin signaling might be a novel treatment strategy in chronic heart failure.
The cardiac myosin-binding protein-C (cMyBP-C) was identified in a screen for myocardial proteins interacting with the leucine zipper (LZ)-binding domain of PKGIα (Robert Blanton, Boston). cMyBP-C is a cardiac myocyte-specific protein that in the phosphorylated state inhibits cardiac remodeling, and when mutated at the LZ-binding domain, leads to hypertrophic cardiomyopathy in humans. In mice subjected to left ventricular pressure overload, cGMP elevation with sildenafil increased cMyBP-C phosphorylation. These data suggest that cMyBP-C is an anti-remodeling PKGIα kinase substrate and support further exploration of PKGIα myocardial LZ substrates as potential therapeutic targets for the treatment of heart failure.
In recent meetings, the role of cGMP-degrading phosphodiesterases, such as PDE5 and PDE9, was intensively discussed, especially with a focus on the impact of cardiovascular disease and heart function. However, PDE2 and the cGMP/cAMP crosstalk may play a crucial role in healthy and diseased myocardium and may have impact on the development of cardiac hypertrophy and heart failure. PDE2 expression and activity is increased in failing hearts of rats, dogs, and also in patients with ischemic or dilated cardiomyopathy. Preclinical in vitro and in vivo data demonstrated that overexpression of PDE2 protects cardiomyocytes and reduces the hypertrophic response (Rodolphe Fischmeister, Paris). Very importantly, mice with myocyte-specific overexpression of PDE2 show higher cardiac contractility and reduced heart rate and have a significantly longer life span compared to WT. Mechanistically, these effects are linked to calcium signaling via the L-type calcium channel in cardiomyocytes. Overexpression of PDE2 decreased the effect on intracellular calcium compared to WT which could be fully removed by using the specific PDE2 inhibitor BAY 60-7550 (Wunder et al. 2009). Overall, these data suggest that pharmacological activation of PDE2 in the heart could represent a potential new therapeutic strategy in heart failure.
In search of novel ways to treat overload-induced cardiac remodeling, mixed-lineage kinase 3 (MLK3), a PKGIα substrate, appears to be a possible target (Timothy Calamaras, Boston). As PKGIα is known to oppose cardiac hypertrophy by unknown mechanisms, MLK3 and its downstream signaling were investigated as potential part of this protective signaling cascade. PKGIα was shown to interact on the protein level with MLK3 in myocardial tissue. With JNK being a substrate of MLK3, PKGIα was shown to mediate cGMP-induced JNK phosphorylation in cultivated cardiomyocytes. Inhibitors of MLK3 led to cardiomyocyte hypertrophy. In line with this, cardiac hypertrophy was seen in MLK3-deficient mice, although these mice showed a preserved cardiac function. Upon pressure overload, however, MLK3-KO mice developed increased cardiac dysfunction which was paralleled by an increase in ANP and collagen expression indicating fibrosis and hypertrophy. In addition, JNK activation in MLK3-KO mice under pressure overload was impaired. These results suggest that PKGIα can mediate its cardioprotective effect via MLK3 and subsequent myocardial JNK signaling.
Cardiovascular functions of CNP
C-type natriuretic peptide (CNP) released from the endothelium plays a fundamental role in regulating vascular homeostasis by controlling local blood flow, systemic blood pressure, and the reactivity of leukocytes and platelets (Moyes et al. 2014). However, the role of endogenous CNP in the heart remains poorly understood. Two novel mouse strains with specific deletion of CNP in endothelial cells or cardiomyocytes have been generated (Amie Moyes, London). Interestingly, these mouse strains demonstrated distinct, and partly opposing, impairments in cardiac functions. The available data suggest that CNP exerts specific protective functions on coronary vascular reactivity and the response to pressure overload, and that some of the CNP effects are mediated in a GC-B-independent manner by activation of NPR-C.
Protective effects of CNP in a mouse model of acute pressure overload were also reported (Konstanze Michel, Würzburg). A role of GC-B in this context was discovered using mice with cardiomyocyte-restricted deletion of GC-B. Their ongoing research attempts to elucidate the downstream targets of CNP/GC-B/cGMP signaling in cardiomyocytes.
With the help of novel mouse models with conditional, cell-restricted deletion of GC-B, so far unknown functions of CNP/GC-B signaling are being discovered (Michaela Kuhn, Würzburg). Preliminary data indicate that GC-B is expressed in endothelial cells, pericytes, and mast cells. It remains to be elucidated how GC-B localized in different tissues affects vascular functions.
Thrombosis and platelet function
An introduction into platelet proteomics was given by Ulrich Walter (Mainz). In previous studies, the sGC stimulator riociguat was shown to effectively increase platelet cGMP levels and VASP phosphorylation, an effect absent in platelet-specific sGC-KO animals (Reiss et al. 2015). In this novel project, the aim was to analyze the human platelet phosphoproteome after stimulation with riociguat. More than 8000 phosphorylation sites in approximately 2250 proteins were detected. Phosphorylation was increased in 345 and decreased in 94 proteins. Comparison with the phosphoproteome after iloprost stimulation revealed a large overlap in cGMP- and cAMP-induced phosphorylation sites. Riociguat strongly increased the phosphorylation of established PKG substrates such as VASP, MYLK, or PDE5. In addition, several new targets were identified. Taken together, these studies are a step forward in elucidating the signaling network of cGMP/PKG-induced phosphorylation of human platelet proteins.
Lung diseases and pulmonary hypertension
Besides prostacyclins and endothelin receptor antagonists, therapies increasing cGMP are part of the standard care for the treatment of pulmonary arterial hypertension (PAH). The PDE5 inhibitors sildenafil and tadalafil have been approved for the treatment of PAH and are distributed as Revatio™ and Adcirca™, respectively (Humbert and Ghofrani 2016). However, a certain proportion of patients does not reach or maintain treatment goals with PDE5 inhibitors. More recently, the sGC stimulator riociguat was approved as Adempas™ not only for the treatment of PAH but also for chronic thromboembolic pulmonary hypertension (CTEPH) (Hoeper 2015). The RESPITE clinical trial (Hoeper et al. 2017) investigated safety, feasibility, and beneficial effects of replacing PDE5 inhibitor with riociguat in patients with PAH who do not respond adequately to PDE5 inhibitors (James Klinger, Providence).
Renal diseases
Kidney diseases, especially chronic and diabetic kidney diseases (CKD/DKD), are major health care problems in the aging population and at least in part closely linked to cardiovascular diseases and heart failure. Atrial natriuretic peptide (ANP) is critically involved in regulation of sodium and water balance. In the kidney, ANP increases the glomerular filtration rate, decreases sodium reabsorption, and inhibits renin secretion, thereby also impacting on the RAAS system. In addition, stimulating the NO/sGC cascade can increase renal blood flow and cGMP increase could help to maintain kidney function (Stasch et al. 2015). Since the medical need in chronic and diabetic kidney diseases is still high, it is an intriguing concept that cGMP elevation could improve kidney function and constitute a new pharmacological treatment approach.
In the last cGMP meeting held in Trier 2015, reno-protective effects of the sGC activator BI 703704 (Boustany-Kari et al. 2016) in ZSF-1 rats were presented by Steven Pullen (Ridgefield). Being a crossbreed of the Zucker diabetic fatty (ZDF) rat and the spontaneously hypertensive heart failure rat, these animals are characterized by obesity, hyperglycemia, and dyslipidemia and develop a progressive proteinuria and glomerulosclerosis. Since this phenotype is reflected also in DKD/CKD patients, this chronic rat model might be ideal to profile new treatments for DKD. The 2015 data indicated that sGC activator treatment could slow progression of proteinuria and cause a significant reduction in the incidence of glomerulosclerosis and interstitial lesions (Boustany-Kari et al. 2016). In this meeting, the optimal dose of BI 703704 was compared to a high and a low dose of an sGC stimulator, a high and a low dose of a PDE5 inhibitor, and enalapril. The blood pressure lowering effects were roughly similar (around − 8 mmHg) in all treatment groups. Interestingly, only the treatment with BI 703704 caused a significant reduction of proteinuria whereas all other treatments had no effect. In addition, only the sGC activator reduced renal damage indicated by reduction of glomerulosclerosis and interstitial lesions. There was also the observation that the sGC activator reduced renal myofibroblasts and increased the number of healthy podocytes without any effect of either enalapril or the sGC stimulator or the PDE5 inhibitor on those cell types. These data confirm the beneficial effects of sGC activators in ZDF-1 rats which should be validated now in the clinics. However, these data also indicate that there might be a mechanistic difference between sGC activators on one end and sGC stimulators and PDE5 inhibitors.
Therefore, despite these very convincing preclinical data, the beneficial action of cGMP in kidney diseases is still unresolved. Various effects ranging from renal blood flow increase, over suppression of renin secretion, to improvement of tubular function and protection of endothelial cells and podocytes are discussed. Potentially, the mode of action is multifactorial. However, this is difficult to study in long-term chronic treatment studies. New methods and mechanistic models characterized by acute decrease in kidney function could help to elucidate such mechanisms. In fact, it was shown that in a model with acute onset of albuminuria induced by angiotensin infusion, cGMP effects could be studied more mechanistically. In this model, both sGC stimulators and sGC activators could reduce albuminuria.
Fibrotic diseases
The effects of cGMP on vascular smooth muscle cells and the implications for the regulation of blood vessel tone and blood pressure are very well established. However, in more recent years, there is emerging evidence that cGMP increases could target a variety of other cell types, including fibroblasts and myofibroblasts (Sandner et al. 2017). Understanding these effects will not only extend the mode of action of cGMP beyond vasodilation but might also provide the basis for completely new applications of cGMP-enhancing drugs.
Systemic sclerosis
Systemic sclerosis (SSc) is a rare connective tissue disease characterized by not only excessive skin fibrosis but also fibrosis of internal organs such as the lungs and kidneys, causing a high morbidity and increased mortality. There is still a significant unmet medical need for antifibrotic treatments since only symptomatic treatment options and treatment recommendations are currently available. The effects of cGMP on skin fibroblasts and on skin fibrosis in vivo have been intensively studied in recent years and the effects of the sGC stimulators BAY 41-2272 (Straub et al. 2001) and BAY 63-2521 (riociguat) were profiled in vitro and in vivo in preclinical models of SSc and skin fibrosis (Peter Sandner, Wuppertal). In vitro, the sGC stimulators not only reduced collagen production and fibroblast-to-myofibroblast differentiation of dermal fibroblasts but were also able to reduce the number of established myofibroblasts and inhibit transforming growth factor beta (TGFß) signaling. In vivo, the sGC stimulators prevented TGFß-induced skin fibrosis, prevented skin fibrosis in the murine bleomycin model, reduced skin fibrosis in the genetic tight skin mouse model, and reduced skin and intestinal fibrosis in the chronic graft versus host disease mouse model. These promising preclinical results led to a randomized, double-blind, placebo-controlled clinical phase II study to investigate the efficacy and safety of riociguat in patients with SSc. This RISE-SSc is currently ongoing (NCT02283762).
Liver fibrosis and non-alcoholic steatohepatitis
In recent years, it has become obvious that cGMP might also have antifibrotic effects in the liver as the use of sGC activators and sGC stimulators turned out to be beneficial in preclinical models of liver fibrosis (Knorr et al. 2008, Sandner and Stasch 2017). The non-alcoholic steatohepatitis (NASH), which is characterized by liver fibrosis, inflammation, and steatosis, could result in liver cirrhosis and might therefore be also sensitive to treatment with sGC modulators. A new potent and selective sGC stimulator, IW-1973, was profiled in vitro and in vivo in animal models of liver fibrosis and NASH (Jaime Masferrer, Boston). In vivo, IW-1973, was investigated in methionine/choline-deficient mice fed with a high-fat diet. In addition, IW-1973 was tested in the so-called STAM model, a mouse NASH model induced by high-fat cholesterol-enriched diet. IW-1973 increased cGMP in rat hepatic stellate cells and reversed TGFß-induced αSMA production. These data suggest that sGC stimulators such as IW-1973 might be a novel treatment approach for liver fibrosis and NASH.
Lung fibrosis
Lung diseases are commonly associated with inflammation and development of fibrotic tissue scars. Therefore, targeting lung fibrosis could improve treatment of various lung diseases. It is well established that sGC stimulators and sGC activator could decrease pulmonary fibrosis in a variety of preclinical animal models.
Global and cell-specific knockout models for sGC are being used to investigate the enzyme’s cellular contribution to the development of lung fibrosis (Andreas Friebe, Würzburg). The major cell type expressing sGC appears to be the lung pericyte. Interestingly, pericytes are also a major sGC expression site in other tissues such as retina, heart, and skeletal muscle. Pericytes have been recently taken into focus as a primary precursor for myofibroblasts (MF) during fibrosis (Rowley and Johnson 2014). MF are the primary cells that promote fibrosis by producing collagen and other matrix proteins as well as a smooth muscle actin. Using the bleomycin model of pulmonary fibrosis, the role of sGC in pulmonary fibrosis turns out to be twofold: Mice lacking the enzyme globally showed increased fibrotic foci after bleomycin treatment. In addition, with the bleomycin model being reversible, resolution of fibrosis was delayed in the absence of sGC. These data clearly point towards the usability of GC stimulators/activators for the therapy of lung fibrosis. However, a clinical phase II study in patients with pulmonary hypertension with complicating idiopathic interstitial pneumonias and interstitial lung fibrosis (NCT02138825) was terminated prematurely due to an unfavorable risk/benefit ratio in these severely ill patients (Nathan et al. 2017) which led to contraindication for riociguat. Therefore, it is still unclear if these antifibrotic effects in vitro and in vivo in the lung will translate into the clinics.
The role of natriuretic peptides and the pGC system for the development of lung fibrosis is less understood. Continuous delivery of ANP using an osmotic pump decreased lung fibrotic area and infiltration of inflammatory cells in the murine bleomycin model of pulmonary fibrosis (Yasutake Tanaka, Osaka). Similar effects of ANP were observed in transgenic mice overexpressing the ANP receptor GC-A in vascular endothelium cells (Okamoto et al. 2017). Moreover, ANP treatment also suppressed exacerbation of acute pulmonary fibrosis in a modified mouse model. Therefore, ANP/GC-A signaling seems to exert protective effects on pulmonary fibrosis.
Sensory systems and neurophysiology
Glaucoma
Being a degenerative disease with poorly understood pathological mechanisms, glaucoma is still widespread in the world’s population (Buys et al. 2014). sGC has been shown to regulate aqueous humor outflow and, thus, intraocular pressure (IOP). In line with this, preclinical studies have proven NO donors and NO gas (40 ppm) to be an effective option for lowering IOP (Emmanuel Buys, Boston). As these effects were absent in mice lacking NO-GC1, sGC stimulators/activators may be a further alternative.
Achromatopsia
In the 7th cGMP meeting in 2015, very early results were presented, demonstrating that abnormalities in cGMP signaling play a role in the pathogenesis of several hereditary forms of visual impairment. Loss-of-function mutations in CNG channels (CNGA3) can cause achromatopsia and CNG channel knockout mice constitute a model system for human achromatopsia. Based on these findings, a recombinant adeno-associated virus (rAAV)-mediated gene supplementation therapy for the treatment of CNGA3-linked achromatopsia was developed (Stylianos Michalakis, München). This system can deliver full-length CNGA3 under control of the human cone-specific cone arrestin promoter packaged in AAV8 capsid (rAAV8.CNGA3). After tests of this rAAV8.CNGA3 vector in the CNGA3 KO mouse achromatopsia model and consecutive toxicological and pharmacokinetic tests, an interventional phase I/II clinical trial has been initiated. This trial is focusing on safety and efficacy of a single subretinal injection of rAAV8.CNGA3 in patients at three different doses. First results in single patients look promising but the trial is still ongoing (NCT02610582).
Auditory system
In 2012, it was demonstrated for the first time that sGC is important for hearing function by showing that sGC-KO mice are more vulnerable to noise-induced hearing loss and that PDE5 inhibitors can prevent noise-induced hearing loss in mice (Jaumann et al. 2012). New evidence now suggest that the deletion of NO-GC1 or NO-GC2 does not influence electromechanical outer hair cell properties, measured by distortion product otoacoustic emissions, neither before nor after noise exposure (Möhrle et al. 2017). In contrast, inner hair cell ribbons and auditory nerve responses were significantly less deteriorated in NO-GC1 KO and NO-GC2 KO mice after noise exposure. The use of sGC stimulators had no effect on hearing function, but demonstrated an age-dependent effect on inner hair cell synaptopathy. These data suggested that sGC may become a future pharmacological target for early treatment of noise trauma and prevention of hidden hearing loss. However, these effects have to be investigated more in detail in the future since PDE5 expression in the cochlea could be age dependent as well, thus also influencing sGC response.
Pharmacology and applications of cGMP-enhancing drugs
sGC stimulators and sGC activators
Johannes-Peter Stasch, previously Bayer, who is one of the pioneers of sGC modulator pharmacology and who discovered sGC stimulators like BAY 41-2272, riociguat, nelociguat, and vericiguat and sGC activators like BAY 60-2770 (Knorr et al. 2008) or cinaciguat, gave a keynote lecture on the discovery, research, and development of these two new classes of compounds. The sGC stimulators are able to stimulate heme-containing sGC via binding to the alpha subunit, whereas sGC activators target the oxidized and heme-free apo-sGC via binding to the heme-site on the beta subunit. These two classes of compounds can stimulate sGC and apo-sGC directly also in the absence of NO. Within this talk, it became very obvious how our understanding of NO/sGC signaling is tightly linked to the discovery of these new classes of compounds. Currently, heme-containing sGC and oxidized and heme-free apo-sGC can be distinguished and characterized only by these compound classes. In addition, riociguat was the first member of this compound class to be approved for medical therapy in 2013 for the treatment of PAH and CTEPH. Currently, a couple of sGC stimulators are in clinical development and vericiguat, a once daily oral sGC stimulator, is most advanced in phase III for the treatment of heart failure with reduced ejection fraction (HFrEF).
New sGC stimulators
In addition, a couple of new sGC stimulators, namely IW-1973, IW-1701, and IW-6463, were introduced which show the classical sGC stimulator profile in vitro (Todd Milne, Boston). These compounds can be applied orally and exhibit not only different kinetics but also different tissue distributions. The once-daily oral sGC stimulator IW-1973 is in phase II clinical development in patients with stable type 2 diabetes and hypertension (NCT03091920). Additional clinical trials in patients with diabetic nephropathy and diabetic kidney disease are planned for IW-1973 (NCT03217591). Moreover, additional indications like HFpEF or resistant hypertension are potential future indications for this compound. IW-1701, another once-daily sGC stimulator, is currently in phase II clinical development for the treatment of achalasia (NCT02931565), and for this compound, sickle cell disease might be a future indication. Finally, IW-6463 is in preclinical development for vascular and Alzheimer’s dementia since this compound was reported to penetrate into the CNS.
New sGC activators
Up to now, the pharmacological differences of sGC stimulators and sGC activators in translational in vivo models and their impact in specific diseases are not well characterized. Preclinical data with an oral sGC activator (BI 703704) were presented (see above). However, new sGC activators were not presented at this conference but clinical testing of a BI sGC activator should start in the near future. This concept might be then also investigated and substantiated in human diseases.
Natriuretic peptide receptor modulators
After the N-methylanthraniloyl compounds (MANT; 6th cGMP conference 2013; Hoffmann and Chen, 2014) and the introduction of NEP inhibitors (7th cGMP conference 2015; Friebe et al. 2015), the research and development of compounds acting on pGC signaling is still lagging behind compared to sGC stimulators and sGC activators. Positive allosteric modulators of the natriuretic peptide receptor-A (GC-A) may be a novel option (Henriette Andresen, Oslo). Based on a high-throughput screening approach with 30.000 compounds, a single hit was identified which could significantly enhance cGMP production in GC-A-expressing cells. In the presence of BNP, this compound increased cGMP production in a concentration-dependent manner suggesting an allosteric binding site. The compound was selective towards GC-A with no effect on GC-B. The compound might be able to enhance natriuretic peptide effects and turn out to be an alternative to natriuretic peptide analogues and NEP inhibitors, although a possible inhibitory effect on PDEs has to be thoroughly checked.
Modified variants of natriuretic peptides
Achondroplasia (ACH), the most common form of human dwarfism, is caused by an activating autosomal dominant mutation in the fibroblast growth factor receptor-3 (FGFR3) gene. Genetic overexpression of C-type natriuretic peptide (CNP), which signals through GC-B and modulates the activity of FGFR3, prevents dwarfism in mouse models of ACH. However, administration of exogenous CNP is compromised by its rapid clearance in vivo through receptor-mediated and proteolytic pathways. Modified variants of human CNP were shown to be resistant to proteolytic degradation and to have significantly longer serum half-lives than native CNP (Stuart Bunting, Los Angeles). Interestingly, one of these CNP variants, BMN 111 (Lorget et al. 2012), corrected the dwarfism phenotype in a mouse model of ACH and accelerated the bone growth in juvenile monkeys (Wendt et al. 2015). While high doses of BMN 111 affect blood pressure and heart rate, low doses seem to be well tolerated. Notably, the first results of low-dose BMN 111 in phase I and II clinical trials are encouraging. Thus, modified CNP variants might represent a new approach for treatment of patients with ACH.
Novel GC and cGMP functions
Diabetes
The cardiac natriuretic peptides ANP and BNP exert well-characterized renal and cardiovascular actions which are mediated by activation of GC-A. There is increasing evidence that ANP and BNP also affect the functions of the adipose tissue, skeletal muscle, liver, and endocrine pancreas (Kuhn 2016). A new mouse model with conditional, cell-restricted deletion of GC-A in pancreatic beta cells showed an improvement of glucose handling and glucose-stimulated insulin release when compared to controls (Sabine Tauscher, Würzburg). These data point to a protective role of the cardiac hormones in the endocrine pancreas with regard to beta cell proliferation and apoptosis.
Colon cancer and obesity
The role of the GC-C/cGMP system was also broadly discussed with regards to its function in adenoma, gut-brain axis, and obesity (Scott Waldman, Philadelphia). In the gastrointestinal tract, GC-C is expressed selectively in intestinal epithelial cells of the brush border membrane (Blomain et al. 2016). Uroguanylin and guanylin act as physiological activators whereas heat-stable enterotoxin from E. coli stimulates the enzyme under pathophysiological conditions. As GC-C is found in colonic stem cells, it might represent a novel tumor suppressor. In fact, data from Waldman’s 2015 talk in Trier indicate that GC-C regulates intestinal crypt-surface proliferation and deletion of guanylin expression increased tumor growth in several colon cancer models. These data are underlined by the phenotype of GC-C-deficient mice in which cancer instance and burden are increased compared to WT animals.
Separate from the GI function, GC-C appears to be involved in the regulation of eating behavior, satiety, and body weight. GC-C-KO animals show increased food uptake and are therefore obese, based on an impaired satiety reflex. In WT animals, instillation of GC-C ligands led to reduced eating. A possible mechanism may include a food-induced release of guanylin which is then transported to the CNS to act on GC-C-expressing nuclei in the hypothalamus. Also, high fat as well as high carbohydrate diet may reduce guanylin levels to be involved in the onset of obesity. Clearly, GC-C ligands may constitute attractive compounds not only for the treatment of colorectal cancer but also to restore appetite control in order to oppose obesity.
Malaria
cGMP signaling in malaria parasites is an interesting but rarely discussed topic (Andrew Tobin, Glasgow). Recent phosphoproteomic studies in Plasmodium falciparum have revealed that the parasite protein kinases phosphorylate proteins involved in both asexual and sexual stages of the parasite life cycle. This finding together with the high degree of phylogenetic distance between the human and malaria protein kinases supports the notion that targeting parasite protein kinases would present therapeutic opportunities not only for the treatment of malaria but also in preventing onward transmission. Interestingly, one of the essential protein kinases in P. falciparum is the cGMP-dependent protein kinase, PfPKG. Among the PfPKG targets identified to date are proteins involved in cell signaling, proteolysis, gene regulation, protein export, and ion and protein transport (Alam et al. 2015). Therefore, compounds that specifically inhibit PfPKG might be novel tools for malaria therapy and prevention (Baker et al. 2017).
Aortic aneurysm
Gene mutations that lead to decreased contraction of vascular smooth muscle cells can cause inherited aortic aneurysms. A recent exome sequencing study identified a heterozygous mutation (R117Q) in PKG1 as the cause of early-onset familial thoracic aortic aneurysms and dissections in four families. Although the R177Q mutation disrupts cGMP binding within the regulatory domain, the altered PKG1 is constitutively active even in the absence of cGMP (Guo et al. 2013). Generation of a mouse line carrying a R117Q knock-in mutation to further explore the underlying mechanisms was reported (Gerburg Schwaertzer, San Diego). Interestingly, she observed increased generation of reactive oxygen species in aortic smooth muscle cells of the knock-in mice. These preliminary data suggest that increased oxidative damage might contribute to the thoracic aortic aneurysms and dissections observed in patients carrying the R117Q mutation.
Non-canonical signaling
The beneficial action of NO· (NO radical) released from various NO donors has been therapeutically exploited for a very long time. Recently, as described above, GC-stimulating/activating compounds have been introduced into clinical pharmacology. Apart from these, PDE inhibitors are a major albeit diverse group of compounds to elevate cGMP signaling. However, still further options exist to increase cGMP-mediated cellular effects by pathways that may be summarized as non-canonical.
Alternative pathways to deliver NO or at least an sGC-activating NO metabolite are inorganic nitrates (Vikas Kapil, London) and nitroxyl (Nazareno Paolocci, Baltimore). Inorganic nitrates are commonly found in various vegetables such as spinach or beet root. These inorganic nitrates require chemical reduction to nitrite and NO. Elegant studies have shown that commensal bacteria in the oral cavity are a main source of nitrate-derived nitrite which is then transformed to NO in the acidic milieu of the stomach (Lundberg et al. 1994). Evidence suggests that dietary inorganic nitrite provides beneficial effects acutely. These include a decrease in blood pressure, platelet inhibition, and anti-inflammatory effects. As tachyphylaxis is not observed within this reaction mechanism, inorganic nitrates might be a useful option for chronic therapies.
Nitroxyl (as HNO or NO−), being the one electron reduction product of NO, has attracted much attention due to its effects in the cardiovascular system. HNO from either Angeli’s salt or newly developed nitroxyl donors such as CXL-1020 (Sabbah et al. 2013) reduce blood pressure by dilation of arterial as well as venous dilation, an effect dependent on sGC. In addition, HNO exerts a positive inotropic effect which is present in mice deficient for sGC (Zhu et al. 2015). A possible mechanism of action, activation of the ryanodine receptor RYR2 in a redox active manner, is being discussed. This would include phospholamban dimerization/tetramerization reducing SERCA inhibition leading to an accelerated calcium uptake (Sivakumaran et al. 2013). Accordingly, nitroxyl donors are currently being evaluated as options for the treatment of acute decompensated heart failure (Sabbah et al. 2013).
Redox regulation of PKG is still an intriguing and strongly discussed mechanism to modulate cGMP-induced signaling cascade. A novel compound named G1 (Burgoyne et al. 2017) was introduced (Phil Eaton, London), which appears to target the PKG and to rely on the redox mechanism involving disulfide formation via the enzyme’s cysteine 42 (Prysyazhna et al. 2012). G1 was shown to dilate isolated arterial vessels from WT mice and to lower blood pressure in an angiotensin II-induced hypertension model in WT mice, both effects being absent in a Cys-mutant PKG knock-in line. Selective phosphorylation of phospholamban at Ser-16 by disulfide-PKG may underlie this effect. As proof of principle, these data indicate that this or related compounds may become attractive alternatives for the treatment of diastolic heart failure (Burgoyne et al. 2017).
Although sGC has been known to be a hemoprotein for over 30 years (Gerzer et al. 1981), the exact mechanism(s) of heme insertion and heme redox regulation are still not elucidated. On the 6th cGMP conference 2013, the mechanism of heme insertion into sGC by the chaperone hsp90 was reported (Ghosh et al. 2014). sGC can be present in two redox states containing either a reduced or oxidized heme (Fe2+ vs Fe3+). Oxidation of sGC heme is thought to be caused by reactive oxygen species, and under pathological situations with concomitant oxidative stress, the oxidized sGC is being exploited as target for GC activators. In Bamberg, novel data on the regulation of the redox state were presented (Adam Straub, Pittsburgh). Cytochrome b5 reductase 3 (Cyb5R3), a flavoprotein known for its ability to transfer electrons, regulates various physiological processes but is mostly involved in cellular heme reduction. In smooth muscle cells, the enzyme is membrane-bound, but its function is elusive so far. Evidence was presented that Cyb5r3 can directly reduce oxidized sGC in SMC. Knockdown of Cyb5r3 in SMC reduced sGC expression and cGMP levels and inhibited NO-stimulated cGMP production and VASP phosphorylation (Rahaman et al. 2017). Taken together, better understanding of the basic mechanisms of sGC heme redox regulation by Cyb5r3 may introduce a novel target to treat cardiovascular diseases that involve altered cGMP metabolism.
Conclusion and future directions
It is very obvious that the understanding on the upstream pathways leading to generation of cGMP as well as the signaling induced by this cyclic nucleotide is far from being complete. This does relate not only to the basic science which will surely unveil new regulatory principles governed by cGMP but also to the clinical aspects comprising the identification of novel targets, indications, and compounds within cGMP signaling. Beneficial effects in cardiac, vascular, pulmonary, and urogenital medicine are clearly anchored by the use of respective pharmacological compounds; other areas are getting more relevant for these drugs such as neuronal disorders, malaria, diabetes, cancer, or obesity. The enthusiasm for cGMP and cGMP-related research is still unbroken and there is much more to discover in this field in the years to come. The authors of this conference report are definitely looking forward to all novel basic findings, clinical developments, and applications that will be presented on the next cGMP conference in 2019!
Acknowledgements
The organization of the 8th cGMP meeting 2017 would not have been possible without financial sponsorship of research organizations and companies. Therefore, the organizers wish to thank Bayer AG, MSD, the Deutsche Forschungsgemeinschaft (DFG), Ironwood, the DFG Forschergruppe FOR 2060, Harvard Apparatus, Biomol, PolyGene, DSI, Bio Trend, Bio Log, and Immune Diagnostic.
Footnotes
Authors are listed in alphabetical order and contributed equally to this report.
A correction to this article is available online at https://doi.org/10.1007/s00210-018-1472-x.
Contributor Information
Andreas Friebe, Email: andreas.friebe@uni-wuerzburg.de.
Peter Sandner, Email: peter.sandner@bayer.com.
Achim Schmidtko, Email: schmidtko@em.uni-frankfrut.de.
References
- Aka AA, Rappaport JA, Pattison AM, Sato T, Snook AE, Waldman SA. Guanylate cyclase C as a target for prevention, detection, and therapy in colorectal cancer. Expert Rev Clin Pharmacol. 2017;10(5):549–557. doi: 10.1080/17512433.2017.1292124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam MM, Solyakov L, Bottrill AR, Flueck C, Siddiqui FA, Singh S, Mistry S, Viskaduraki M, Lee K, Hopp CS, Chitnis CE, Doerig C, Moon RW, Green JL, Holder AA, Baker DA, Tobin AB. Phosphoproteomics reveals malaria parasite protein kinase G as a signalling hub regulating egress and invasion. Nat Commun. 2015;6:7285. doi: 10.1038/ncomms8285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baker DA, Stewart LB, Large JM, Bowyer PW, Ansell KH, Jiménez-Díaz MB, El Bakkouri M, Birchall K, Dechering KJ, Bouloc NS, Coombs PJ, Whalley D, Harding DJ, Smiljanic-Hurley E, Wheldon MC, Walker EM, Dessens JT, Lafuente MJ, Sanz LM, Gamo FJ, Ferrer SB, Hui R, Bousema T, Angulo-Barturén I, Merritt AT, Croft SL, Gutteridge WE, Kettleborough CA, Osborne SA. A potent series targeting the malarial cGMP-dependent protein kinase clears infection and blocks transmission. Nat Commun. 2017;8(1):430. doi: 10.1038/s41467-017-00572-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ben Aissa M, Lee SH, Bennett BM, Thatcher GR. Targeting NO/cGMP signaling in the CNS for neurodegeneration and Alzheimer’s disease. Curr Med Chem. 2016;23(24):2770–2788. doi: 10.2174/0929867323666160812145454. [DOI] [PubMed] [Google Scholar]
- Blomain ES, Merlino DJ, Pattison AM, Snook AE, Waldman SA, Guanylyl Cyclase C. Hormone axis at the intersection of obesity and colorectal cancer. Mol Pharmacol. 2016;90(3):199–204. doi: 10.1124/mol.115.103192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boolell M, Allen MJ, Ballard SA, Gepi-Attee S, Muirhead GJ, Naylor AM, Osterloh IH, Gingell C. Sildenafil: an orally active type 5 cyclic GMP-specific phosphodiesterase inhibitor for the treatment of penile erectile dysfunction. Int J Impot Res. 1996;8(2):47–52. [PubMed] [Google Scholar]
- Boustany-Kari CM, Harrison PC, Chen H, Lincoln KA, Qian HS, Clifford H, Wang H, Zhang X, Gueneva-Boucheva K, Bosanac T, Wong D, Fryer RM, Richman JG, Sarko C, Pullen SS. A soluble guanylate cyclase activator inhibits the progression of diabetic nephropathy in the ZSF1 rat. J Pharmacol Exp Ther. 2016;356(3):712–719. doi: 10.1124/jpet.115.230706. [DOI] [PubMed] [Google Scholar]
- Buglioni A, Burnett JC., Jr New pharmacological strategies to increase cGMP. Annu Rev Med. 2016;67:229–243. doi: 10.1146/annurev-med-052914-091923. [DOI] [PubMed] [Google Scholar]
- Burgoyne JR, Prysyazhna O, Richards DA, Eaton P. Proof of principle for a novel class of antihypertensives that target the oxidative activation of PKG Iα (protein kinase G Iα) Hypertension. 2017;70(3):577–586. doi: 10.1161/HYPERTENSIONAHA.117.09670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buys ES, Potter LR, Pasquale LR, Ksander BR. Regulation of intraocular pressure by soluble and membrane guanylate cyclases and their role in glaucoma. Front Mol Neurosci. 2014;7:38. doi: 10.3389/fnmol.2014.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deloukas, et al. Large-scale association analysis identifies new risk loci for coronary artery disease. Nat Genet. 2013;45(1):25–33. doi: 10.1038/ng.2480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Doumas M, Lazaridis A, Katsiki N, Athyros V. PDE-5 inhibitors: clinical points. Curr Drug Targets. 2015;16(5):420–426. doi: 10.2174/1389450115666141111111301. [DOI] [PubMed] [Google Scholar]
- Filippatos G, Maggioni AP, Lam CSP, Pieske-Kraigher E, Butler J, Spertus J, Ponikowski P, Shah SJ, Solomon SD, Scalise AV, Mueller K, Roessig L, Bamber L, Gheorghiade M, Pieske B. Patient-reported outcomes in the SOluble guanylate Cyclase stimulatoR in heArT failurE patientS with PRESERVED ejection fraction (SOCRATES-PRESERVED) study. Eur J Heart Fail. 2017;19(6):782–791. doi: 10.1002/ejhf.800. [DOI] [PubMed] [Google Scholar]
- Follmann M, Ackerstaff J, Redlich G, Wunder F, Lang D, Kern A, Fey P, Griebenow N, Kroh W, Becker-Pelster EM, Kretschmer A, Geiss V, Li V, Straub A, Mittendorf J, Jautelat R, Schirok H, Schlemmer KH, Lustig K, Gerisch M, Knorr A, Tinel H, Mondritzki T, Trübel H, Sandner P, Stasch JP. Discovery of the soluble guanylate cyclase stimulator vericiguat (BAY 1021189) for the treatment of chronic heart failure. J Med Chem. 2017;60(12):5146–5161. doi: 10.1021/acs.jmedchem.7b00449. [DOI] [PubMed] [Google Scholar]
- Friebe A, Sandner P, Seifert R. From bedside to bench—meeting report of the 7th International Conference on cGMP “cGMP: generators, effectors and therapeutic implications” in Trier, Germany, from June 19th to 21st 2015. Naunyn Schmiedeberg's Arch Pharmacol. 2015;388(12):1237–1246. doi: 10.1007/s00210-015-1176-4. [DOI] [PubMed] [Google Scholar]
- Gerzer R, Böhme E, Hofmann F, Schultz G. Soluble guanylate cyclase purified from bovine lung contains heme and copper. FEBS Lett. 1981;132(1):71–74. doi: 10.1016/0014-5793(81)80429-2. [DOI] [PubMed] [Google Scholar]
- Gheorghiade M, Greene SJ, Butler J, Filippatos G, Lam CS, Maggioni AP, Ponikowski P, Shah SJ, Solomon SD, Kraigher-Krainer E, Samano ET, Müller K, Roessig L, Pieske B, SOCRATES-REDUCED Investigators and Coordinators Effect of vericiguat, a soluble guanylate cyclase stimulator, on natriuretic peptide levels in patients with worsening chronic heart failure and reduced ejection fraction: the SOCRATES-REDUCED Randomized Trial. JAMA. 2015;314(21):2251–2262. doi: 10.1001/jama.2015.15734. [DOI] [PubMed] [Google Scholar]
- Ghofrani HA, Humbert M, Langleben D, Schermuly R, Stasch JP, Wilkins MR, Klinger JR. Riociguat: mode of action and clinical development in pulmonary hypertension. Chest. 2017;151(2):468–480. doi: 10.1016/j.chest.2016.05.024. [DOI] [PubMed] [Google Scholar]
- Ghosh A, Stasch JP, Papapetropoulos A, Stuehr DJ. Nitric oxide and heat shock protein 90 activate soluble guanylate cyclase by driving rapid change in its subunit interactions and heme content. J Biol Chem. 2014;289(22):15259–15271. doi: 10.1074/jbc.M114.559393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo DC, Regalado E, Casteel DE, Santos-Cortez RL, Gong L, Kim JJ, Dyack S, Horne SG, Chang G, Jondeau G, Boileau C, Coselli JS, Li Z, Leal SM, Shendure J, Rieder MJ, Bamshad MJ, Nickerson DA, GenTAC Registry Consortium. National Heart, Lung, and Blood Institute Grand Opportunity Exome Sequencing Project. Kim C, Milewicz DM. Recurrent gain-of-function mutation in PRKG1 causes thoracic aortic aneurysms and acute aortic dissections. Am J Hum Genet. 2013;93(2):398–404. doi: 10.1016/j.ajhg.2013.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoeper MM, Simonneau G, Corris PA, Ghofrani HA, Klinger JR, Langleben D, Naeije R, Jansa P, Rosenkranz S, Scelsi L, Grünig E, Vizza CD, Chang M, Colorado P, Meier C, Busse D, Benza RL (2017) RESPITE: switching to riociguat in pulmonary arterial hypertension patients with inadequate response to phosphodiesterase-5 inhibitors. Eur Respir J 50(3) [DOI] [PMC free article] [PubMed]
- Hoeper MM. Pharmacological therapy for patients with chronic thromboembolic pulmonary hypertension. Eur Respir Rev. 2015;24:272–282. doi: 10.1183/16000617.00001015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoffmann LS, Chen HH. cGMP: transition from bench to bedside: a report of the 6th International Conference on cGMP Generators, Effectors and Therapeutic Implications. Naunyn Schmiedeberg's Arch Pharmacol. 2014;387(8):707–718. doi: 10.1007/s00210-014-0999-8. [DOI] [PubMed] [Google Scholar]
- Humbert M, Ghofrani HA. The molecular targets of approved treatments for pulmonary arterial hypertension. Thorax. 2016;71(1):73–83. doi: 10.1136/thoraxjnl-2015-207170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaumann M, Dettling J, Gubelt M, Zimmermann U, Gerling A, Paquet-Durand F, Feil S, Wolpert S, Franz C, Varakina K, Xiong H, Brandt N, Kuhn S, Geisler HS, Rohbock K, Ruth P, Schlossmann J, Hütter J, Sandner P, Feil R, Engel J, Knipper M, Rüttiger L. cGMP-Prkg1 signaling and Pde5 inhibition shelter cochlear hair cells and hearing function. Nat Med. 2012;18(2):252–259. doi: 10.1038/nm.2634. [DOI] [PubMed] [Google Scholar]
- Jhund PS, Fu M, Bayram E, Chen CH, Negrusz-Kawecka M, Rosenthal A, Desai AS, Lefkowitz MP, Rizkala AR, Rouleau JL, Shi VC, Solomon SD, Swedberg K, Zile MR, McMurray JJ, Packer M, PARADIGM-HF Investigators and Committees Efficacy and safety of LCZ696 (sacubitril-valsartan) according to age: insights from PARADIGM-HF. Eur Heart J. 2015;36(38):2576–2584. doi: 10.1093/eurheartj/ehv330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler T, Wobst J, Wolf B, Eckhold J, Vilne B, Hollstein R, von Ameln S, Dang TA, Sager HB, Moritz Rumpf P, Aherrahrou R, Kastrati A, Björkegren JLM, Erdmann J, Lusis AJ, Civelek M, Kaiser FJ, Schunkert H. Functional characterization of the GUCY1A3 coronary artery disease risk locus. Circulation. 2017;136(5):476–489. doi: 10.1161/CIRCULATIONAHA.116.024152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khder Y, Shi V, McMurray JJV, Lefkowitz MP. Sacubitril/valsartan (LCZ696) in heart failure. Handb Exp Pharmacol. 2017;243:133–165. doi: 10.1007/164_2016_77. [DOI] [PubMed] [Google Scholar]
- Knorr A, Hirth-Dietrich C, Alonso-Alija C, Härter M, Hahn M, Keim Y, Wunder F, Stasch JP. Nitric oxide-independent activation of soluble guanylate cyclase by BAY 60-2770 in experimental liver fibrosis. Arzneimittelforschung. 2008;58(2):71–80. doi: 10.1055/s-0031-1296471. [DOI] [PubMed] [Google Scholar]
- Koesling D, Mergia E, Russwurm M. Physiological functions of NO-sensitive guanylyl cyclase isoforms. Curr Med Chem. 2016;23(24):2653–2665. doi: 10.2174/0929867323666160812145050. [DOI] [PubMed] [Google Scholar]
- Kraehling JR, Sessa WC. Contemporary approaches to modulating the nitric oxide-cGMP pathway in cardiovascular disease. Circ Res. 2017;120(7):1174–1182. doi: 10.1161/CIRCRESAHA.117.303776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krawutschke C, Koesling D, Russwurm M. Cyclic GMP in vascular relaxation: export is of similar importance as degradation. Arterioscler Thromb Vasc Biol. 2015;35(9):2011–2019. doi: 10.1161/ATVBAHA.115.306133. [DOI] [PubMed] [Google Scholar]
- Kuhn M. Molecular physiology of membrane guanylyl cyclase receptors. Physiol Rev. 2016;96(2):751–804. doi: 10.1152/physrev.00022.2015. [DOI] [PubMed] [Google Scholar]
- Lewis KS, Butler J, Bauersachs J, Sandner P. The three-decade long journey in heart failure drug development. Handb Exp Pharmacol. 2017;243:1–14. doi: 10.1007/164_2016_101. [DOI] [PubMed] [Google Scholar]
- Lorget F, Kaci N, Peng J, Benoist-Lasselin C, Mugniery E, Oppeneer T, Wendt DJ, Bell SM, Bullens S, Bunting S, Tsuruda LS, O’Neill CA, Di Rocco F, Munnich A, Legeai-Mallet L. Evaluation of the therapeutic potential of a CNP analog in a Fgfr3 mouse model recapitulating achondroplasia. Am J Hum Genet. 2012;91(6):1108–1114. doi: 10.1016/j.ajhg.2012.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lundberg JO, Weitzberg E, Lundberg JM, Alving K. Intragastric nitric oxide production in humans: measurements in expelled air. Gut. 1994;35(11):1543–1546. doi: 10.1136/gut.35.11.1543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Möhrle D, Reimann K, Wolter S, Wolters M, Varakina K, Mergia E, Eichert N, Geisler HS, Sandner P, Ruth P, Friebe A, Feil R, Zimmermann U, Koesling D, Knipper M, Rüttiger L. NO-sensitive guanylate cyclase isoforms NO-GC1 and NO-GC2 contribute to noise-induced inner hair cell synaptopathy. Mol Pharmacol. 2017;92(4):375–388. doi: 10.1124/mol.117.108548. [DOI] [PubMed] [Google Scholar]
- Moyes AJ, Khambata RS, Villar I, Bubb KJ, Baliga RS, Lumsden NG, Xiao F, Gane PJ, Rebstock AS, Worthington RJ, Simone MI, Mota F, Rivilla F, Vallejo S, Peiró C, Sánchez Ferrer CF, Djordjevic S, Caulfield MJ, MacAllister RJ, Selwood DL, Ahluwalia A, Hobbs AJ. Endothelial C-type natriuretic peptide maintains vascular homeostasis. J Clin Invest. 2014;124(9):4039–4051. doi: 10.1172/JCI74281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nathan SD, Behr J, Collard HR, Cottin V, Hoeper MM, Martinez F, Corte T, Keogh A, Leuchte H, Mogulkoc N, Ulrich S, Wuyts W, Malcolm S, Shah S, Yao M, Wells A. RISE-IIP: Riociguat for the treatment of pulmonary hypertension associated with idiopathic interstitial pneumonia. Eur Respir J. 2017;50(suppl 61):OA1985. doi: 10.1016/S2213-2600(19)30250-4. [DOI] [PubMed] [Google Scholar]
- Oettrich JM, Dao VT, Frijhoff J, Kleikers P, Casas AI, Hobbs AJ, Schmidt HH. Clinical relevance of cyclic GMP modulators: a translational success story of network pharmacology. Clin Pharmacol Ther. 2016;99(4):360–362. doi: 10.1002/cpt.336. [DOI] [PubMed] [Google Scholar]
- Okamoto A, Nojiri T, Konishi K, Tokudome T, Miura K, Hosoda H, Hino J, Miyazato M, Kyomoto Y, Asai K, Hirata K, Kangawa K. Atrial natriuretic peptide protects against bleomycin-induced pulmonary fibrosis via vascular endothelial cells in mice: ANP for pulmonary fibrosis. Respir Res. 2017;18(1):1. doi: 10.1186/s12931-016-0492-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prysyazhna O, Rudyk O, Eaton P. Single atom substitution in mouse protein kinase G eliminates oxidant sensing to cause hypertension. Nat Med. 2012;18(2):286–290. doi: 10.1038/nm.2603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rahaman MM, Nguyen AT, Miller MP, Hahn SA, Sparacino-Watkins C, Jobbagy S, Carew NT, Cantu-Medellin N, Wood KC, Baty CJ, Schopfer FJ, Kelley EE, Gladwin MT, Martin E, Straub AC. Cytochrome b5 reductase 3 modulates soluble guanylate cyclase redox state and cGMP signaling. Circ Res. 2017;121(2):137–148. doi: 10.1161/CIRCRESAHA.117.310705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rainer PP, Kass DA. Old dog, new tricks: novel cardiac targets and stress regulation by protein kinase G. Cardiovasc Res. 2016;111(2):154–162. doi: 10.1093/cvr/cvw107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss C, Mindukshev I, Bischoff V, Subramanian H, Kehrer L, Friebe A, Stasch JP, Gambaryan S, Walter U. The sGC stimulator riociguat inhibits platelet function in washed platelets but not in whole blood. Br J Pharmacol. 2015;172(21):5199–5210. doi: 10.1111/bph.13286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowley JE, Johnson JR. Pericytes in chronic lung disease. Int Arch Allergy Immunol. 2014;164(3):178–188. doi: 10.1159/000365051. [DOI] [PubMed] [Google Scholar]
- Sabbah HN, Tocchetti CG, Wang M, Daya S, Gupta RC, Tunin RS, Mazhari R, Takimoto E, Paolocci N, Cowart D, Colucci WS, Kass DA. Nitroxyl (HNO): a novel approach for the acute treatment of heart failure. Circ Heart Fail. 2013;6(6):1250–1258. doi: 10.1161/CIRCHEARTFAILURE.113.000632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandner P, Berger P, Zenzmaier C. The potential of sGC modulators for the treatment of age-related fibrosis: a mini-review. Gerontology. 2017;63(3):216–227. doi: 10.1159/000450946. [DOI] [PubMed] [Google Scholar]
- Sandner P, Stasch JP. Anti-fibrotic effects of soluble guanylate cyclase stimulators and activators: a review of the preclinical evidence. Respir Med. 2017;122(Suppl 1):S1–S9. doi: 10.1016/j.rmed.2016.08.022. [DOI] [PubMed] [Google Scholar]
- Singh JSS, Burrell LM, Cherif M, Squire IB, Clark AL, Lang CC (2017) Sacubitril/valsartan: beyond natriuretic peptides. Heart [DOI] [PubMed]
- Sivakumaran V, Stanley BA, Tocchetti CG, Ballin JD, Caceres V, Zhou L, Keceli G, Rainer PP, Lee DI, Huke S, Ziolo MT, Kranias EG, Toscano JP, Wilson GM, O’Rourke B, Kass DA, Mahaney JE, Paolocci N. HNO enhances SERCA2a activity and cardiomyocyte function by promoting redox-dependent phospholamban oligomerization. Antioxid Redox Signal. 2013;19(11):1185–1197. doi: 10.1089/ars.2012.5057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stasch JP, Schlossmann J, Hocher B. Renal effects of soluble guanylate cyclase stimulators and activators: a review of the preclinical evidence. Curr Opin Pharmacol. 2015;21:95–104. doi: 10.1016/j.coph.2014.12.014. [DOI] [PubMed] [Google Scholar]
- Straub A, Stasch JP, Alonso-Alija C, Benet-Buchholz J, Ducke B, Feurer A, Fürstner C. NO-independent stimulators of soluble guanylate cyclase. Bioorg Med Chem Lett. 2001;11(6):781–784. doi: 10.1016/S0960-894X(01)00073-7. [DOI] [PubMed] [Google Scholar]
- Wendt DJ, Dvorak-Ewell M, Bullens S, Lorget F, Bell SM, Peng J, Castillo S, Aoyagi-Scharber M, O’Neill CA, Krejci P, Wilcox WR, Rimoin DL, Bunting S. Neutral endopeptidase-resistant C-type natriuretic peptide variant represents a new therapeutic approach for treatment of fibroblast growth factor receptor 3-related dwarfism. J Pharmacol Exp Ther. 2015;353(1):132–149. doi: 10.1124/jpet.114.218560. [DOI] [PubMed] [Google Scholar]
- Wunder F, Gnoth MJ, Geerts A, Barufe D. A novel PDE2A reporter cell line: characterization of the cellular activity of PDE inhibitors. Mol Pharm. 2009;6(1):326–336. doi: 10.1021/mp800127n. [DOI] [PubMed] [Google Scholar]
- Zhu G, Groneberg D, Sikka G, Hori D, Ranek MJ, Nakamura T, Takimoto E, Paolocci N, Berkowitz DE, Friebe A, Kass DA. Soluble guanylate cyclase is required for systemic vasodilation but not positive inotropy induced by nitroxyl in the mouse. Hypertension. 2015;65(2):385–392. doi: 10.1161/HYPERTENSIONAHA.114.04285. [DOI] [PMC free article] [PubMed] [Google Scholar]