Abstract
Methylprednisolone (MP) is currently the only drug confirmed to exhibit a neuroprotective effect on acute spinal cord injury (SCI). Vitamin C (VC) is a natural water-soluble antioxidant that exerts neuroprotective effects through eliminating free radical damage to nerve cells. Bone marrow mesenchymal stem cells (BMMSCs), as multipotent stem cells, are promising candidates in SCI repair. To evaluate the therapeutic effects of MP, VC and BMMSCs on traumatic SCI, 80 adult male rats were randomly divided into seven groups: control, SCI (SCI induction by weight-drop method), MP (SCI induction, followed by administration of 30 mg/kg MP via the tail vein, once every other 6 hours, for five times), VC (SCI induction, followed by intraperitoneal administration of 100 mg/kg VC once a day, for 28 days), MP + VC (SCI induction, followed by administration of MP and VC as the former), BMMSCs (SCI induction, followed by injection of 3 × 106 BMMSCs at the injury site), and BMMSCs + VC (SCI induction, followed by BMMSCs injection and VC administration as the former). Locomotor recovery was assessed using the Basso Mouse Scale. Injured spinal cord tissue was evaluated using hematoxylin-eosin staining and immunohistochemical staining. Expression of transforming growth factor-beta, tumor necrosis factor-alpha, and matrix metalloproteinase-2 genes was determined using real-time quantitative PCR. BMMSCs intervention better promoted recovery of nerve function of rats with SCI, mitigated nerve cell damage, and decreased expression of transforming growth factor-beta, tumor necrosis factor-alpha, and matrix metalloproteinase-2 genes than MP and/or VC. More importantly, BMMSCs in combination with VC induced more obvious improvements. These results suggest that VC can enhance the neuroprotective effects of BMMSCs against SCI.
Keywords: nerve regeneration, spinal cord injury, vitamin C, methylprednisolone, bone marrow mesenchymal stem cells, locotmotor, neural regeneration
Introduction
Spinal cord injury (SCI), which results from trauma or neurodegeneration, is a destructive injury. It often affects young and healthy individuals and debilitates them. It also creates a significant financial burden to the society (Song et al., 2014). Motor vehicle crashes and violence are the most common causes of traumatic spinal cord injury (TSCI), which is an irreversible condition that affects millions of people worldwide each year (Middletonet al., 2014). SCI has two phases: primary, followed by secondary injury. The primary injury is due to mechanical injury to cells, damages the spinal cord by interrupting its blood supply, and is usually severe at onset. Secondary injury includes neurogenic shock, respiratory failure (Lo et al., 2013), and bladder, bowel, cardiovascular, and sexual function disturbance (Harvey, 2016). Injuries to the spinal cord are accompanied by many problems which include neural cell death, inflammation, scar formation, and disturbance of neurovascular supply (Liu et al., 2013). The therapeutic effects of medical, surgical, and natural therapies are usually unsatisfactory (Li et al., 2015).
Corticosteroids contain naturally secreted steroid hormones which are produced from the adrenal cortex and synthetic hormones (Ngeow and Lim, 2016). Glucocorticoids are widely used in the treatment of many autoimmune and allergic diseases such as asthma and rheumatoid arthritis due to their well-authenticated anti-inflammatory effects (Peek et al., 2005). Methylprednisolone (MP), a synthetic glucocorticoid hormone, has anti-inflammatory, immunosuppressive, and antiallergic effects and acts through inhibition of prostaglandins which are the main mediators of inflammation. So it is used for treatment of inflammatory diseases (Jafari et al., 2016). MP, like other corticosteroids, is associated with potentially serious complications such as anaphylactic shock, cardiac arrhythmias, abnormal behavior (mood alteration, hyperactivity, and sleep disturbance), hyperglycemia, hypokalemia, and infections. Adverse effects of MP often occur in a dose-dependent manner (Sinha and Bagga, 2008; Jongen et al., 2016).
Plants can synthesize vitamin C (VC) for themselves, but humans and some other animals must obtain it from fruits and vegetables (Duan et al., 2016). VC is an essential dietary micronutrient that has many biological functions (Carr et al., 2016). VC is an important antioxidant against oxidative stress (Su et al., 2016) and was used successfully to treat many diseases as common cold (Lykkesfeldt and Poulsen, 2010), cancer (Aguilera et al., 2016; Frajese et al., 2016) and myocardial ischemia (El-Shitany and El-Desoky, 2016; Hao et al., 2016; Moradi-Arzeloo et al., 2016). Deficiency of VC in diet leads to scurvy which is a serious disease (Carr et al., 2016).
Mesenchymal stem cells (MSCs) are adherent multipotent fibroblast-type stem cells which have the capacity of self-renewal and differentiation into mesodermal and ectodermal cells. MSCs are present in several tissues, including bone marrow, umbilical cord, and adipose tissue (Wang et al., 2016). Bone marrow-derived mesenchymal stem cells (BMMSCs) have anti-inflammatory, immunomodulatory, antiapoptotic, and antifibrotic effects through the secretion of bioactive trophic factors which make them suitable candidates for cell therapy. BMMSCs can survive for long periods after transplantation without inducing an immune response (Dhoke et al., 2016; Kim et al., 2016).
The present study was conducted to evaluate the therapeutic potential of MP, VC, and BMMSCs in experimentally induced traumatic SCI in rats.
Materials and Methods
Animals
Eighty healthy adult Albino male rats weighing 180 ± 30 g were bred and maintained in an air-conditioned animal house with specific pathogen-free conditions. Rats received a balanced diet with free access to water. All animal procedures were performed according to approved protocols of the Animal Committee of the Faculty of Medicine, Cairo University (Cuf/F/Sur/2014/28 (10/4/2014)). This study was carried out in strict accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (NIH publication No. 85-23, revised 1996). They were kept under observation for one week before beginning of the experiment.
Experimental procedure
Rats were randomly divided into seven groups. Control group: twenty rats were subdivided equally into five subgroups: subgroup I (negative control rats) and subgroup II (sham operated controls), where rats were exposed to T9–10 laminectomy without contusion injury and received no pharmacological treatment; subgroup III (MP vehicle control), where rats were injected with 0.5 mL of 0.9% saline via the caudal vein; subgroup IV (VC vehicle control), where rats were injected with 0.5 mL of 0.9% saline intraperitoneally; subgroup V, as sham operated control with rats being injected once with 0.5 mL of phosphate buffered saline (PBS) locally at the site of laminectomy. SCI group: Ten rats were exposed to surgical induction of SCI. MP group: Ten rats were exposed to surgical induction of SCI and after one hour, MP sodium succinate in 0.9% saline (Solu-Medrol 1-gram vial, Pfizer, Boulevard de la Plaine, Ixelles, Belgium) was injected as 30 mg/kg intravenous bolus via rat tail vein followed by administration of MP for four subsequent times into a tail vein (30 mg/kg) at the 6-hour interval (Nash et al., 2002). VC group: Ten rats were exposed to surgical induction of SCI and after one hour, rats were injected intraperitoneally with VC (Cevarol ampoule containing 500 mg VC) obtained from Memphis Company (8 EL-Sawah Square, EL-Amyria, Cairo, Egypt) at 100 mg/kg per day (Yan et al., 2014), and then further treated once a day for 28 days. MP + VC group: Ten rats were exposed to surgical induction of SCI and treated with combined MP and VC as in groups III and IV. BMMSCs group: Ten rats were exposed to surgical induction of SCI and received BMMSCs injection locally at the site of SCI at a single dose of 3 × 106 cells suspended in 0.5 mL phosphate buffered saline (PBS) (Attia et al., 2015). BMMSCs + VC group: Ten rats were exposed to surgical induction of SCI and treated with BMMSCs and VC as in VC and BMMSCs groups.
Induction of SCI
Surgical SCI induction was performed according to a previous study (Erbayraktar et al., 2013). In brief, aseptic T9–10 laminectomy under anesthesia was performed. Spinal cord contusion was induced using a weight-drop apparatus, where a guided 10 g rod was dropped from a height of 12.5 mm onto the exposed dura mater, representing moderate SCI.
Preparation of BMMSCs
BMMSCs were flushed from rat tibia and fibula (these male healthy rats were not involved in experimental procedures) with phosphate buffered solution (PBS) containing 2 mL EDTA (Department of Biochemistry, Faculty of Medicine, Cairo University). 35 mL of the diluted sample was carefully layered using 15 mL Ficoll-Paque (Gibco-Invitrogen, Grand Island, NY, USA). Then, the mixture was centrifuged at 400 × g for 35 minutes. The upper layer was aspirated, leaving the mononuclear cell layer undisturbed at the interphase. The mononuclear cell layer was aspirated, washed twice in PBS containing 2 mL EDTA, and then centrifuged for 10 minutes at 200 × g at 10°C. The cell pellets were re-suspended in a final volume of 300 μL of buffer. Isolated BMMSCs were cultured in a 25 mL culture flask in minimal essential medium supplemented with 15% fetal bovine serum (FBS) and incubated for 2 hours at 37°C in 5% CO2 atmosphere. Adherent BMMSCs were cultured in minimal essential medium supplemented with 30% fetal bovine serum and 0.5% penicillin and streptomycin at 37°C in 5% CO2 atmosphere (Yamazoe et al., 2007; Abdel Aziz et al., 2011). Cultured BMMSCs were confirmed using an inverted microscope: Leica DM IL LED with camera Leica DFC295 (Leica Microsystems CMS GmbH, Ernst-Leitz-Straße 17-37, Wetzlar, D-35578, Germany).
Labeling stem cells with GFP
BMMSCs were labeled with GFP (pAcGFP1-N1 Vector, Clontech Laboratories, Inc. (USA) catalog # 632469) for in vivo tracing and observed in unstained spinal cord tissue cryosections (at T9–10) using fluorescence microscope (Niki et al., 2004) (Leica Microsystems CMS GmbH, Ernst-Leitz-Straße, Wetzlar, D-35578, Germany).
Behavioral assessment
Hind limb locomotor recovery was assessed using the Basso Mouse Scale (BMS). The scale ranges from 0, indicating complete paralysis, to 9, indicating normal movement of the hind limbs (Basso et al., 2006). Rats of all groups were tested for hind limb functional deficits at 1, 7, 14, 21, and 28 days after SCI. All outcome measures were obtained in a blinded fashion by two investigators and averaged. The score was assessed at 1, 7, 14, 21 and 28 days postoperatively.
Histological and immunohistochemical staining
The fasted rats were anesthetized by 1.9% ether presented on a cotton ball or gauze pad for 5 to 10 minutes, and sacrificed by cervical decapitation four weeks after induction of SCI. Spinal cord tissue at the site of injury was excised. The specimens were fixed in 10% buffered formol saline, processed for 4–6 µm-thick paraffin sections, mounted on glass slides for hematoxylin-eosin staining (Bancroft and Layton, 2013). Other sections were mounted on positively charged slides for immunohistochemical staining (Jacksonand Blythe, 2013).
Immunohistochemical staining was performed to detect nestin. Sections were incubated using primary antibody nestin (rat-401) at 4°C for 12 hours at 1–5 µg/mL. Then these sections were incubated with neurofilament (200 kDa) (lysine-serine-proline repeat) antibody (rabbit polyclonal, Catalog Number: AB1991, dilution: 1:1,000 using IHC-TekTM antibody diluent (Cat# IW-1000 or IW-1001) at room temperature for 60 minutes to reduce background and unspecific staining. Serum blocking step was not needed.
Immunohistochemical reactions were performed using the horseradish peroxidase-labeled streptavidin-biotin method. Paraffin sections were mounted on positively charged slides. They were deparaffinized in xylene, rehydrated in descending grades of ethyl alcohol, and then immersed in 0.3% hydrogen peroxide in methyl alcohol to block endogenous peroxidase activity. The sections were washed in PBS and 10% normal rat serum was applied for 30 minutes to reduce nonspecific binding. After incubation for 1 hour with antiserum-containing primary antibody, the sections were counterstained with Mayer's hematoxylin, dehydrated in ascending grades of ethyl alcohol, cleared in xylene, and mounted in Canada balsam.
Morphometric study
The mean area percentage of nestin and NF-200 immunoreactive expression was quantified in five images from five nonoverlapping fields of each rat using Image-Pro Plus program version 6.0 (Media Cybernetics Inc., Bethesda, Maryland, USA).
Real-time quantitative PCR (RT-qPCR)
Spinal cord tissue of all studied groups was homogenized. Total RNA was isolated with RNeasy Mini Kit (Qiagen, Hilden, Germany) and further analyzed for quantity and quality with a dual beam spectrophotometer (Beckman Coulter, Fullerton, California, USA). For quantitative expression of transforming growth factor-beta (TGF-β), tumor necrosis factor-alpha (TNF-α), and matrix metalloproteinase-2 (MMP-2) genes, the following procedure was performed. 200 ng of the total RNA from each sample was used for cDNA synthesis by reverse transcription using High Capacity cDNA Reverse Transcriptase kit (Applied Biosystems Inc., Foster City, CA, USA). The cDNA was subsequently amplified with the SYBR Green One-Step PCR Master Kit in a 48-well plate (Applied Biosystems Inc., Foster City, CA, USA) as follows: 10 minutes at 95°C for enzyme activation followed by 40 cycles of 15 seconds at 95°C, 20 seconds at 55°C, and 30 seconds at 72°C for the amplification step. Changes in the expression of each target gene were normalized relative to the mean critical threshold (CT) values of GAPDH housekeeping gene by the 2–ΔΔCt method (Livak and Schmittgen, 2001). We used 1 μL of both primers specific for each target gene. Primer sequence and annealing temperature specific for each gene are demonstrated in Table 1.
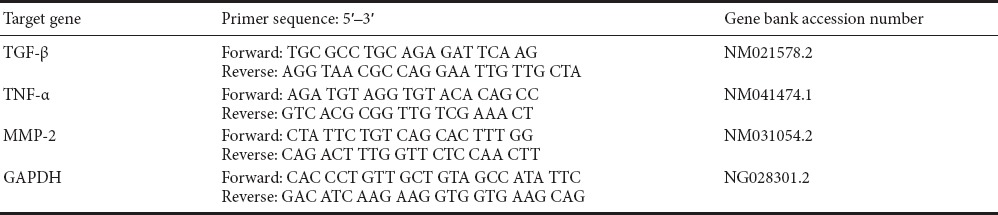
Table 1.
Primer sequence and specific for each gene
Statistical analysis
All data collected from the experiment were recorded and analyzed using SPSS 20.0 software (IBM Corp., Armonk, NY, USA). One-way analysis of variance (ANOVA) with post hoc Scheffe's test was used to compare differences among the groups. In each test, the data were expressed as the mean ± standard deviation (SD) and differences were considered to be significant at P < 0.01.
Results
Behavior changes in SCI rats
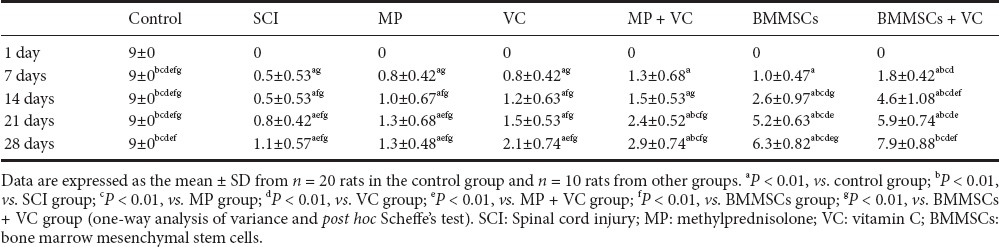
All data of BMS score for all groups and at all time points are shown in Table 2. Rats in the control group showed normal rat locomotor function with a BMS score of 9 at all time points. Rats in other groups did not show any recovery at 1 day. Slight recovery in rats from the SCI group began from day 7 and continued until day 28. There were no significant differences in BMS score at all time points between SCI group and MP and VC groups. BMS score increased significantly in the MP + VC group at 21 and 28 days, in the BMMSCs group at 14, 21 and 28 days, and in the BMMSCs + VC group at 7, 14, 21 and 28 days (P < 0.01).
Table 2.
Basso Mouse Scale (BMS) score at 1, 7, 14, 21, and 28 days after SCI in all groups
BMMSCs identification in culture and tracking
BMMSCs were identified in culture under an inverted microscope as spindle shaped cells between rounded cells (Figure 1A). Locally injected BMMSCs labeled with GFP were observed in spinal cord tissue using a fluorescent microscope (Figure 1B).
Figure 1.

Identification of cultured rat bone marrow mesenchymal stem cells (BMMSCs).
(A) Many spindle shaped stem cells (arrows) from primary culture at 14 days (inverted microscope). (B) BMMSCs labeled with green fluorescent protein (arrows) from stem cell groups (BMMSCs and BMMSCs + VC groups) (fluorescent microscope). Original magnification 400× in A and B. VC: Vitamin C.
Hematoxylin-eosin staining
In the control group, all subgroups showed nearly the same histological images. They showed central gray matter and peripheral white matter. The white matter contained thick fibers and neuroglial cells. The gray matter contained nerve fibers, nerve cells, and neuroglial cells (Figure 2A). A higher magnification of the gray matter showed a number of multipolar cells with central nuclei and multiple Nissl's granules in their cytoplasm. Neuroglial cells could be seen (Figure 2B). SCI group showed areas of complete destruction of nerve cells with marked vacuolation, congested dilated blood vessels and excess neuroglial cells (gliosis). Few apparently normal neurons with wide perineural space and some dark disfigured neurons were noticed (Figure 2C). MP group showed areas of complete destructed neurons. Some neurons appeared normal and others appeared disfigured with wide perineural space. Blood vessels appeared slightly dilated and congested. There were many neuroglial cells. Thick fibers in gray and white matters were noticed (Figure 2D). VC group showed few apparently normal neurons but most of the neurons were disfigured with wide perineural space. Blood vessels appeared dilated and congested. There were many neuroglial cells (Figure 2E). MP + VC group showed some apparently normal neurons, and others were disfigured neurons with slightly wide perineural space. Blood vessels appeared slightly congested. There were many neuroglial cells (Figure 2F). BMMSCs group showed apparently normal neurons with central nuclei and Nissl's granules in their cytoplasm, many neuroglial cells and small blood vessels. Few disfigured neurons and wide perineural space were observed (Figure 2G). BMMSCs + VC group showed a similar image to the control group. There were a number of apparently normal neurons with central nuclei, multiple Nissl's granules in their cytoplasm, many neuroglial cells and small blood vessels (Figure 2H).
Figure 2.
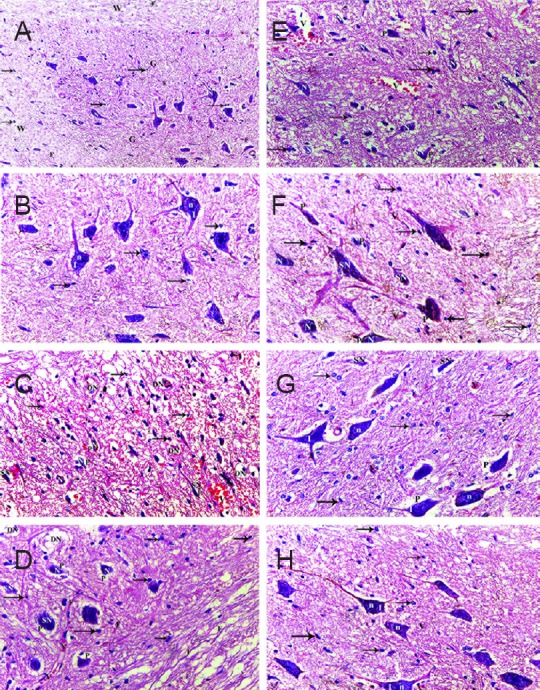
Representative micrographs of hematoxylin-eosin-stained rat spinal cord tissue sections.
(A) Control group: showing central gray matter (G) and peripheral white matter (W). The white matter contained nerve fibers (F) and neuroglia cells (arrow). The gray matter contained nerve fibers (F), nerve cells (N), and neuroglial cells (arrow). (B) In higher magnification of (A), gray matter shows apparently normal neurons with central nuclei (n) and Nissl's granules (I) in their cytoplasm and neuroglial cells (arrow). (C) Spinal cord injury (SCI) group: showing areas of complete destruction of nerve cells with marked vacuolation (DN), congested dilated blood vessels (V) and excess neuroglial cells (arrow). Few apparently normal neurons (N) with wide perineural space (P) and some dark disfigured neurons (SN) are observed. (D) Methylprednisolone (MP) group: showing few areas of complete destructed neurons (DN), some neurons appear normal (N) and others appear disfigured (SN) with wide perineural space (P). Blood vessels appear slightly dilated and congested (V). There are multiple neuroglial cells (arrow) and thick nerve fibers (F) in gray and white matters. (E) Vitamin C (VC) group: showing few apparently normal neurons (N), many disfigured neurons (SN) with wide perineural space (P). Blood vessels appear dilated and congested (V). There are multiple neuroglial cells (arrow). (F) MP + VC group: showing some apparently normal neurons (N) and other disfigured (SN) neurons with slightly wide perineural space (P). Blood vessels (V) appeared slightly congested. There were multiple neuroglial cells (arrow). (G) Bone marrow mesenchymal stem cells (BMMSCs) group: showing apparently normal neurons (N) with central nuclei and Nissl's granules (I) in their cytoplasm, many neuroglial cells (arrow) and small blood vessels (V). Few disfigured neurons and wide perineural space (P) are observed. (H) BMMSCs + VC group: showing apparently normal neurons with central nuclei (n), and multiple Nissl's granules (I) in their cytoplasm, many neuroglial cells (arrow) and small blood vessels (V). Original magnification, A: 200×; B–H: 400×.
Nestin immunoreactivity
Nestin, a class VI intermediate filament protein is expressed in adult neural progenitor cells (NPCs). Nestin-immunoreactive cells showed brown cytoplasmic staining. Control, SCI, and MP groups showed negative nestin expression (Figure 3A–C). VC and MP + VC groups showed minimal nestin-immunoreactive expression (Figure 3D, E). BMMSCs and BMMSCs + VC groups showed marked nestin-immunoreactive expression (Figure 3F, G).
Figure 3.
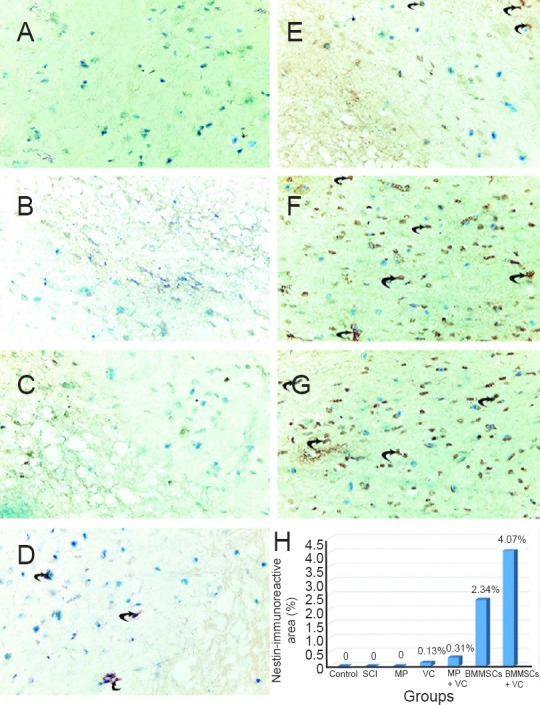
Nestin immunoreactivity in spinal cord tissue section.
(A–G) Immunohistochemical staining for nestin (original magnification, 400×). No nestin immunoreactivity was observed in the control (A), SCI (B), and MP (C) groups. Weak nestin immunoreactivity (arrows) was observed in the VC (D) and MP + VC groups (E). Obvious nestin immunoreactivity was observed in the BMMSCs (F) and BMMSCs + VC groups (G). (H) Quantification of nestin immunoreactivity. All data are expressed as the mean ± SD. SCI: Spinal cord injury; MP: methylprednisolone; VC: vitamin C; BMMSCs: bone marrow mesenchymal stem cells.
Neurofilament 200 (NF200) immunoreactivity
NF200 was expressed in somal and axonal membranes as brown staining particles. Control group showed apparent NF200 immunoreactivity (Figure 4A). SCI group showed marked depletion in NF immunoreactivity (Figure 4B). MP, VC, and MP + VC groups showed increased NF immunoreactivity compared with SCI group (Figure 4C–E). NF200 immunoreactivity was obviously increased in the BMMSCs and BMMSCs + VC groups than in the SCI group (Figure 4F, G).
Figure 4.
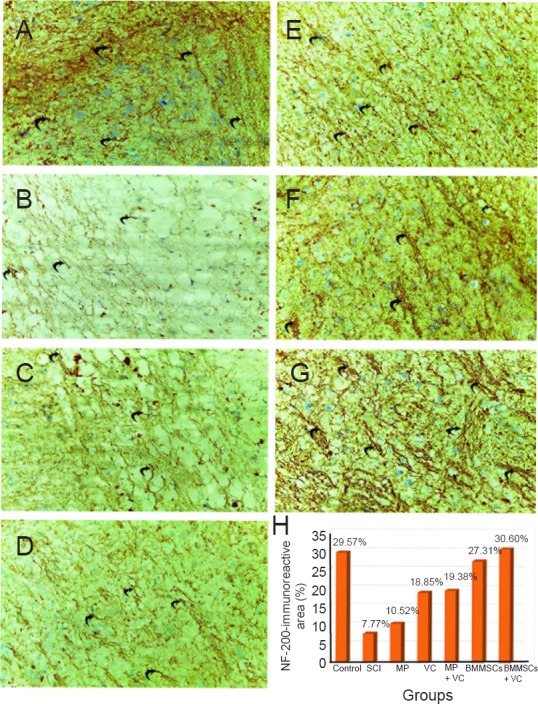
Neurofilament 200 (NF200) immunoreactivity in spinal cord tissue section.
(A–G) Immunohistochemical staining for NF200 (original magnification, 400×). Strong NF200 immunoreactivity (arrow) was observed in the control (A), BMMSCs (F), BMMSCs + VC (G) groups. Moderate NF200 immunoreactivity (arrows) was observed in the SCI (B), MP (C), VC (D), and MP + VC (E) groups. (H) Quantification of NF200 immunoreactivity. All data are expressed as the mean ± SD. SCI: Spinal cord injury; MP: methylprednisolone; VC: vitamin C; BMMSCs: bone marrow mesenchymal stem cells.
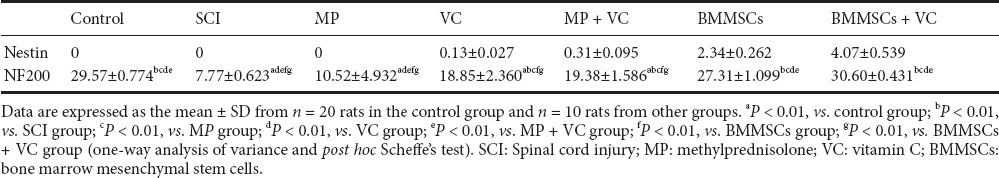
Nestin and NF200 immunoreactivity in all groups is shown in Table 3 and Figures 3H, 4H. NF200 immunoreactivity in the VC, MP + VC, BMMSCs, and BMMSCs + VC groups was significantly higher than that in the SCI group (P < 0.01).
Table 3.
Nestin- and neurofilament 200 (NF200)-immunoreactive area (%) in the spinal cord of rats
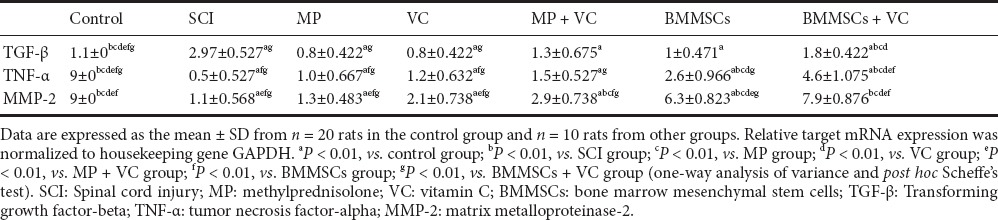
Quantitative gene expression
Gene expression of TGF-β (pro-fibrotic and inflammatory marker), TNF-α (inflammatory marker) and MMP-2 (fibrosis marker) in all groups is shown in Table 4. The expression levels of TGF-β, TNF-α and MMP-2 gene were not significantly decreased in the MP, VC, and MP + VC groups than in the SCI group. However, the expression level of these three genes was significantly decreased in the BMMSCs, and BMMSCs + VC groups (P < 0.01).
Table 4.
TGF-β, TNF-α and MMP-2 gene expression in the spinal cord of rats
Discussion
Traumatic SCI is a serious and destructive condition which leads to loss of function below the injury site, with considerable effects on the quality and expectancy of life. There is no ideal or effective cure for SCI at this time (Lee et al., 2016).
The SCI group in the present study demonstrated slight increase in BMS score at 7 days which continued until 28 days, areas of complete destruction of nerve cells with excess neuroglial cells (gliosis), negative nestin expression, marked depletion in NF expression, and high TGF-β, TNF-α, and MMP-2 gene expression. In accordance with these results, an early study (Pajoohesh-Ganji et al., 2010) revealed that BMS scores slightly increased at 7 days and stabilized until day 42. There was acute functional loss one day after the injury followed by progressively restricted recovery. Several studies (Yan et al., 2016; Zhang et al., 2016; Zhou et al., 2016) reported that SCI rats showed posttraumatic progressive neuron cell loss, glial proliferation, and degeneration of the injured spinal cord. The levels of oxidative stress and apoptosis are believed to be two of the most serious factors leading to nervous tissue destruction. Likewise, Jiang et al. (2014) stated that real-time PCR showed a significant increase in TNF-α in the spinal cord after injury. Shibuya et al. (2002) reported that in rats with SCI, nestin immunoreactivity was noticed at the pial surface surrounding the spinal cord and at the lesion site. In spite of the fact that nestin expression was negligible at 24 hours, and it expanded definitely at 1 and 4 weeks after injury. However, some scholars (Namiki and Tator, 1999; Cizkova et al., 2009) reported that nestin expression was detected around the central canal 4 days after SCI, increased and surrounded the lesion site, and then decreased by day 7 to return to its basal level by day 14; thus only limited nestin labeling around lesion site could be seen. Also, one recent study (Geng et al., 2015) showed that after SCI, nestin protein expression was suppressed, and nestin-immunoreactive cells were limited and localized to the ependymal canal. In the present study, no inflammatory cells (neutrophilic) infiltrated in the hematoxylin-eosin-stained sections. Fleming et al. (2006) reported that, in rats, neutrophilic infiltrations occurred early (4–6 hours) after SCI and disappeared within 5 days, and macrophages (derived from blood-borne monocytes and resident microglia) penetrated the lesion 2 days after SCI in rats and continued for weeks to months.
Our results showed that in the MP group, BMS score was not significantly increased at all time points compared with the SCI group, some neurons completely destroyed, and the other neurons were disfigured with wide perineural space and negative nestin expression. In addition, there were no significant differences in NF200 expression and TGF-β, TNF-α, and MMP-2 gene expression between MP and SCI groups. All these findings suggest that MP exhibits slight, but not significant therapeutic effects on SCI. These results are in consistent with those reported by some scholars (Lankhorst et al., 2000; Marcon et al., 2010; Harrop, 2014) who demonstrated that MP-treated rats did not show significant locomotor recovery after SCI. Moreover, Is et al. (2006) reported that MP-treated rats showed no improvement in the histopathological findings compared with rats in the SCI group except for a mild decrease in edema formation in spinal cord tissue. However, some scholars (Hugenholtz, 2003; Sharma et al., 2004) reported that MP was effective in enhancing locomotor and histological recovery and reducing edema when given early after SCI. Others (Evaniew et al., 2015; Sámano et al., 2016) attributed this controversy to the variation of the studies in MP dose timing and duration, species and age of animals, degree and extent of SCI, and the methods of evaluations and outcome analysis. Several studies (Sayer et al., 2006; Hurlbert et al., 2013; Lim and Choi, 2017) reported that there is no convenient medical evidence of any class to warrant the utilization of MP for acute SCI. MP administration is associated with many serious complications and even death and should not be routinely used in the treatment of patients with acute SCI as it is not recommended for use in acute SCI according to the USA Food and Drug Administration.
Our results showed that in the VC group, histological manifestation was slightly improved, there was minimal nestin expression, and NF200 expression was significantly increased compared with the SCI group. This is consistent with the findings reported by Cristante et al. (2009) that VC only relieved histopathological injury, but not neurological performance after SCI. However, Yan et al. (2014) reported that a higher dose of VC (200 mg/kg per day) after SCI significantly diminished the secondary damage-induced tissue necrosis and enhanced the behavioral function of rats. This impact of VC on SCI was attributed to its antioxidant and oxygen free radical's scavenger impact as the pathologic course of spinal cord contusion incorporates primary and secondary mechanisms of damage and the oxygen free radicals were recommended as essential factors in secondary injury (Jia et al., 2012; Chen et al., 2014; Fatima et al., 2015).
Our results showed that in the MP + VC group, histological manifestation was greatly improved compared with the MP or VC group alone. In the MP + VC group, there was minimal nestin expression, BMS scores increased significantly at 21 and 28 days only, and NF200 expression was significantly increased compared with the SCI group. Is et al. (2016) revealed that MP or antioxidant alone had a mild beneficial effect but the combination was more effective and produced an additive effect on improving histopathological and locomotor changes after SCI. Recent studies (Anwar et al., 2016; Li et al., 2016) demonstrated that since the wide range of pathogenic procedures is included in SCI, it is improbable that treatment with a single agent will lead to maximum recovery and combined multiple agents should be applied in treatment strategies.
In this study, BMMSCs were injected locally into the lesion site in SCI rats as some previous studies (Takahashi et al., 2011; Elawady et al., 2016; Liu et al., 2016) have demonstrated that direct injection of stem cells into a spinal cord lesion site is more successful than intravenous injection in functional recovery of injured spinal cord in rats. Amemori et al. (2015) showed that direct injection of mesenchymal stem cells into a spinal cord compression lesion promoted locomotor recovery. In the BMMSCs group in the current study, locomotor activity was obviously increased, as confirmed by significant increase in BMS score at 14, 21 and 28 days, compared with the SCI group. In the BMMSCs group, there was much nestin expression, NF200 expression was significantly increased, and TGF-β, TNF-α, and MMP-2 gene expression was significantly decreased compared with the SCI group. Several previous studies (Tohda and Kuboyama, 2011; Park et al., 2012; Oliveri et al., 2014; Kim et al., 2015; Anna et al., 2017) demonstrated that transplantation of mesenchymal stem cells into SCI models promoted functional recovery after SCI, and the optimal dose, timing, and route of BMMSCs administration were important factors for achieving therapeutic results. Saini et al. (2016) reported that transplantation of BMMSCs in rats with SCI increased NF200 expression and promoted functional recovery. Xie et al. (2015) reported that BMMSCs exhibited positive nestin expression. The mechanisms underlying recovery include differentiation of BMMSCs into neuronal cells which express neural cell marker. BMMSCs are likewise ready to regulate the injured microenvironment of the central nervous system and to enhance healing by paracrine as they secrete anti-apoptotic and anti-inflammatory factors and trophic molecules. These trophic molecules can support axonal growth, immunomodulation, to enhance angiogenesis, remyelination, and to protect against apoptotic cell death (Quertainmont et al., 2012; Zhu et al., 2013; Kakabadze et al., 2016; Uchida et al., 2016).
Combined therapies for the treatment of SCI are more effective than monotherapy due to the complexity of SCI (Butenschön et al., 2016; Jin et al., 2016). Low efficacy of stem cell transplantation was attributed to the unsuitable pathological microenvironment at the injured sites as oxidative stress, inflammation, and using antioxidants result in an increase in stem cell survival and efficacy after transplantation (Saparov et al., 2013; Yang et al., 2015). Likewise, more improvement in all parameters were observed in the BMMSCS + VC group than in the BMMSCs group.
Taken together, MP or VC alone had a little therapeutic effect on traumatic SCI in rats, and their combination was capable of improving the locomotor activity and had some beneficial effects on modulating the histopathological manifestation of rats with SCI. However, BMMSCs transplantation had an effective role in functional and histological reconstruction of the spinal cord in rats after injury and BMMSCs in combination with VC was more therapeutically effective.
Footnotes
Funding: This work was funded by Project Management Unit, Banha University, Banha, Egypt.
Conflicts of interest: None declared.
Research ethics: The study procedures were performed in accordance with the recommendations in the Guide for the Care and Use of Laboratory Animals of the National Institutes of Health (NIH publication No. 85-23, revised 1996) and were approved by the Animal Committee of the Faculty of Medicine, Cairo University (Cuf/F/Sur/2014/28 (10/4/2014)).
Data sharing statement: Datasets analyzed during the current study are available from the corresponding author on reasonable request.
Plagiarism check: Checked twice by iThenticate.
Peer review: Externally peer reviewed.
Copyedited by Li CH, Song LP, Zhao M
References
- Abdel Aziz MT, El Asmar MF, Atta HM, Fouad HH, Roshdy NK, Rashed LA, Sabry D, Hassouna AA, Taha FM. Efficacy of mesenchymal stem cells in suppression of hepatocarcinorigenesis in rats: possible role of Wnt signaling. J Exp Clin Cancer Res. 2011;30:49. doi: 10.1186/1756-9966-30-49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aguilera O, Muñoz-Sagastibelza M, Torrejón B, Borrero-Palacios A, Del Puerto-Nevado L, Martínez-Useros J, Rodriguez-Remirez M, Zazo S, García E, Fraga M, Rojo F, García-Foncillas J. Vitamin C uncouples the Warburg metabolic switch in KRAS mutant colon cancer. Oncotarget. 2016;7:47954–47965. doi: 10.18632/oncotarget.10087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amemori T, Ruzicka J, Romanyuk N, Jhanwar-Uniyal M, Sykova E, Jendelova P. Comparison of intraspinal and intrathecal implantation of induced pluripotent stem cell-derived neural precursors for the treatment of spinal cord injury in rats. Stem Cell Res Ther. 2015;6:257. doi: 10.1186/s13287-015-0255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anna Z, Katarzyna JW, Joanna C, Barczewska M, Joanna W, Wojciech M. Therapeutic potential of olfactory ensheathing cells and mesenchymal stem cells in spinal cord injuries. Stem Cells Int. 2017;2017:3978595. doi: 10.1155/2017/3978595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anwar MA, Al Shehabi TS, Eid AH. Inflammogenesis of secondary spinal cord injury. Front Cell Neurosci. 2016;10:98. doi: 10.3389/fncel.2016.00098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Attia MM, Shehab Eldien AA, Haiba DA, Mohamed SM. Effect of stem cell transplantation on amiodarone-induced hepatic changes in adult male albino rats: a histological and immunohistochemical study. Egypt J Histol. 2015;38:295–307. [Google Scholar]
- Bancroft JD, Layton C. The hematoxylin and eosin. In: Suvarna SK, Layton C, Bancroft JD, editors. Theory and Practice of Histological Techniques. Philadelphia: Churchill Livingstone of Elsevier; 2013. [Google Scholar]
- Basso DM, Fisher LC, Anderson AJ, Popovich P. Bassomouse scale for locomotion detects differences in recovery after spinal cord injury in five common mouse strains. J Neurotrauma. 2006;23:635–659. doi: 10.1089/neu.2006.23.635. [DOI] [PubMed] [Google Scholar]
- Butenschön J, Zimmermann T, Schmarowski N, Leschik J. PSA-NCAM positive neural progenitors stably expressing BDNF promotes functional recovery in a mouse model of spinal cord injury. Stem Cell Res Ther. 2016;7:17. doi: 10.1186/s13287-015-0268-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr AC, Pullar JM, Bozonet SM, Vissers MC. Marginal ascorbate status (hypovitaminosis C) results in an attenuated response to vitamin C supplementation. Nutrients. 2016;8:pii: E341. doi: 10.3390/nu8060341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen HC, Hsu PW, Tzaan WC, Lee AW. Effects of the combined administration of vitamins C and E on the oxidative stress status and programmed cell death pathways after experimental spinal cord injury. Spinal Cord. 2014;52:24–28. doi: 10.1038/sc.2013.140. [DOI] [PubMed] [Google Scholar]
- Cizkova D, Nagyova M, Slovinska L, Novotna I, Radonak J, Cizek M, Mechirova E, Tomori Z, Hlucilova J, Motlik J, Sulla I, Jr, Vanicky I. Response of ependymal progenitors to spinal cord injury or enhanced physical activity in adult rat. Cell Mol Neurobiol. 2009;29(6-7):999–1013. doi: 10.1007/s10571-009-9387-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cristante AF, Barros Filho TE, Oliveira RP, Daci K. Antioxidative therapy in contusion spinal cord injury. Spinal Cord. 2009;47:458–463. doi: 10.1038/sc.2008.155. [DOI] [PubMed] [Google Scholar]
- Dhoke NR, Kalabathula E, Kaushik K, Geesala R, Sravani B, Das A. Histone deacetylases differentially regulate the proliferative phenotype of mouse bone marrow stromal and hematopoietic stem/progenitor cells. Stem Cell Res. 2016;17:170–180. doi: 10.1016/j.scr.2016.07.001. [DOI] [PubMed] [Google Scholar]
- Duan W, Ren J, Li Y, Liu T1 Song X, Chen Z, Huang Z, Hou X, Li Y. Conservation and expression patterns divergence of ascorbic acid d-mannose/l-galactose pathway genes in Brassica rapa. Front Plant Sci. 2016;7:778. doi: 10.3389/fpls.2016.00778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elawady MA, Elmaghrabi MM, Ebrahim N, Elawady MA, Sabry D, Shamaa A, Ragae A. Therapeutic potential of bone marrow derived mesenchymal stem cells in modulating astroglyosis of surgical induced experimental spinal cord injury. Adv Biosci Biotechnol. 2016;7:251–265. [Google Scholar]
- El-Shitany NA, El-Desoky K. Protective effects of carvedilol and vitamin C against azithromycin-induced cardiotoxicity in rats via decreasing ROS, IL1-β, and TNF-α production and inhibiting NF-κB and Caspase-3 expression. Oxid Med Cell Longev. 2016;2016:1874762. doi: 10.1155/2016/1874762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erbayraktar Z, Gokmen N, Yilmaz O, Erbayraktar S. Experimental traumatic spinal cord injury. Methods Mol Biol. 2013;982:103–112. doi: 10.1007/978-1-62703-308-4_6. [DOI] [PubMed] [Google Scholar]
- Evaniew N, Noonan VK, Fallah N, Kwon BK, Rivers GS, Ahn H, Bailey CS, Christie SD, Fourney DR, Hurlbert RJ, Linassi AG, Fehlings MG, Dvorak MF. Methylprednisolone for the treatment of patients with acute spinal cord injuries: a propensity score-matched cohort study from a Canadian multi-center spinal cord injury registry. J Neurotrauma. 2015;32:1674–1683. doi: 10.1089/neu.2015.3963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fatima G, Sharma GP, Das SK, Mahdi AA. Oxidative stress and antioxidative parameters in patients with spinal cord injury: implications in the pathogenesis of disease. Spinal Cord. 2015;53:3–6. doi: 10.1038/sc.2014.178. [DOI] [PubMed] [Google Scholar]
- Fleming JC, Norenberg MD, Ramsay DA, Dekaban G, Marcillo AE, Saenz AD, Pasquale-Styles M, Dietrich WD, Weaver LC. The cellular inflammatory response in human spinal cords after injury. Brain. 2006;129:3249–3269. doi: 10.1093/brain/awl296. [DOI] [PubMed] [Google Scholar]
- Frajese GV, Benvenuto M, Fantini M, Ambrosin E, Sacchetti P, Masuelli L, Giganti MG, Modesti A, Bei R. Potassium increases the antitumor effects of ascorbic acid in breast cancer cell lines in vitro. Oncol Lett. 2016;11:4224–4234. doi: 10.3892/ol.2016.4506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geng X, Sun T, Li JH, Zhao N, Wang Y, Yu HL. Electroacupuncture in the repair of spinal cord injury: inhibiting the Notch signaling pathway and promoting neural stem cell proliferation. Neural Regen Res. 2015;10:394–403. doi: 10.4103/1673-5374.153687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hao J, Li WW, Du H, Zhao ZF, Liu F, Lu JC, Yang XC, Cui W. Role of vitamin C in cardioprotection of ischemia/reperfusion injury by activation of mitochondrial KATP channel. Chem Pharm Bull (Tokyo) 2016;64:548–557. doi: 10.1248/cpb.c15-00693. [DOI] [PubMed] [Google Scholar]
- Harrop JS. Spinal cord injury: debating the efficacy of methylprednisolone. Neurosurgery. 2014;61:30–31. doi: 10.1227/NEU.0000000000000391. [DOI] [PubMed] [Google Scholar]
- Harvey LA. Physiotherapy rehabilitation for people with spinal cord injuries. J Physiother. 2016;62:4–11. doi: 10.1016/j.jphys.2015.11.004. [DOI] [PubMed] [Google Scholar]
- Hugenholtz H. Methylprednisolone for acute spinal cord injury: not a standard of care. CMAJ. 2003;168:1145–1146. [PMC free article] [PubMed] [Google Scholar]
- Hurlbert RJ, Hadley MN, Walters BC, AarabiB, Dhall SS, Gelb DE, Rozzelle CJ, Ryken TC, Theodore N. Pharmacological therapy for acute spinal cord injury. Neurosurgery. 2013;72:93–105. doi: 10.1227/NEU.0b013e31827765c6. [DOI] [PubMed] [Google Scholar]
- Is M, Ulu MO, Tanriverd T, Uzan M. The use of methylprednisolone, vitamin E and their combination in acute spinal cord injury: An experimental study. Turk Neurosurg. 2006;16:2–8. [Google Scholar]
- Jackson P, Blythe D. Immunohistochemical techniques. In: Suvarna SK, Layton C, Bancroft JD, editors. Theory and Practice of Histological Techniques. 7th ed. Philadelphia: Churchill Livingstone of Elsevier; 2013. [Google Scholar]
- Jafari S, Maleki-Dizaji N, Barar J, Barzegar-Jalali M, Rameshrad M, Adibkia K. Methylprednisolone acetate-loaded hydroxyapatite nanoparticles as a potential drug delivery system for treatment of rheumatoid arthritis: In vitro and in vivo evaluations. Eur J Pharm Sci. 2016;91:225–235. doi: 10.1016/j.ejps.2016.05.014. [DOI] [PubMed] [Google Scholar]
- Jia Z, Zhu H, Li J, Wang X, Misra H, Li Y. Oxidative stress in spinal cord injury and antioxidant-based intervention. Spinal Cord. 2012;50:264–274. doi: 10.1038/sc.2011.111. [DOI] [PubMed] [Google Scholar]
- Jiang SH, Tu WZ, Zou EM, Hu J, Wang S, Li JR, Wang WS, He R, Cheng RD, Liao WJ. Neuroprotective effects of different modalities of acupuncture on traumatic spinal cord injury in rats. Evid Based Complement Alternat Med. 2014;2014:431580. doi: 10.1155/2014/431580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jin Y, Bouyer J, Shumsky JS, Haas C, Fischer I. Transplantation of neural progenitor cells in chronic spinal cord injury. Neuroscience. 2016;320:69–82. doi: 10.1016/j.neuroscience.2016.01.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jongen PJ, Stavrakaki I, Voet B, Hoogervorst E, van Munster E, Linssen WH, Sinnige LG, Verhagen WI, Visser LH, van der Kruijk R, Verheul F, Boringa J, Heerings M, Gladdines W, Lonnqvist F, Gaillard P. Patient-reported adverse effects of high-dose intravenous methylprednisolone treatment: a prospective web-based multi-center study in multiple sclerosis patients with a relapse. J Neurol. 2016;263:1641–1651. doi: 10.1007/s00415-016-8183-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kakabadze Z, Kipshidze N, Mardaleishvili K, Chutkerashvili G, Chelishvili I, Harders A, Loladze G, Shatirishvili G, Kipshidze N, Chakhunashvili D, Chutkerashvili1 K. Phase 1 trial of autologous bone marrow stem cell transplantation in patients with spinal cord injury. Stem Cells Int. 2016;2016:6768274. doi: 10.1155/2016/6768274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JH, Lee HJ, Song YS. Mesenchymal stem cell-based gene therapy for erectile dysfunction. Int J Impot Res. 2016;28:81–87. doi: 10.1038/ijir.2016.3. [DOI] [PubMed] [Google Scholar]
- Kim Y, Jo SH, Kim WH, Kweon OK. Antioxidant and anti-inflammatory effects of intravenously injected adipose derived mesenchymal stem cells in dogs with acute spinal cord injury. Stem Cell Res Ther. 2015;6:229. doi: 10.1186/s13287-015-0236-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lankhorst AJ, Laak MP, Hamers FP, Gispen WH. Combined treatment with alpha MSH and methylprednisolone fails to improve functional recovery after spinal injury in the rat. Brain Res. 2000;859:334–340. doi: 10.1016/s0006-8993(00)02025-4. [DOI] [PubMed] [Google Scholar]
- Lee JY, Choi HY, Yune TY. Fluoxetine and vitamin C synergistically inhibits blood-spinal cord barrier disruption and improves functional recovery after spinal cord injury. Neuropharmacology. 2016;109:78–87. doi: 10.1016/j.neuropharm.2016.05.018. [DOI] [PubMed] [Google Scholar]
- Li H, Ham TR, Neill N, Farrag M, Mohrman AE, Koenig AM, Leipzig ND. A hydrogel bridge incorporating immobilized growth factors and neural stem/progenitor cells to treat spinal cord injury. Adv Healthc Mater. 2016;5:802–812. doi: 10.1002/adhm.201500810. [DOI] [PubMed] [Google Scholar]
- Li X, Yang C, Li L, Xiong J, Xie L, Yang B, Yu M, Feng L, Jiang Z, Guo W, Tian W. A therapeutic strategy for spinal cord defect: human dental follicle cells combined with aligned PCL/PLGA electrospun material. Biomed Res Int. 2015;2015:197183. doi: 10.1155/2015/197183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lim W, Choi B. Current therapeutic approaches in spinal cord injury: pharmacological, rehabilitation, cell-based, and psychological intervention. Korean J Str Res. 2017;25:1–7. [Google Scholar]
- Liu H, Schwarz EM, Xie C. Dual differentiation-exogenous mesenchymal stem cell therapy for traumatic spinal cord injury repair in a murine hemisection model. Stem Cells Int. 2013;2013:928982. doi: 10.1155/2013/928982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu S, Zhou J, Zhang X, Liu Y, Chen J, Hu B, Song J, Zhang Y. Strategies to optimize adult stem cell therapy for tissue regeneration. Int J Mol Sci. 2016;17:pii: E982. doi: 10.3390/ijms17060982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C (T)) Method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- Lo V, Esquenazi Y, Han MK, Lee K. Critical care management of patients with acute spinal cord injury. J Neurosurg Sci. 2013;57:281–292. [PubMed] [Google Scholar]
- Lykkesfeldt J, Poulsen HE. Is vitamin C supplementation beneficial? Lessons learned from randomised controlled trials. Br J Nutr. 2010;103:1251–1259. doi: 10.1017/S0007114509993229. [DOI] [PubMed] [Google Scholar]
- Marcon RM, Barros Filho TP, Oliveira RP, Cristante AF, Taricco MA, Colares G, Barbarini AF, Teixeira WJ, de Souza FI. Experimental study on the action of methylprednisolone on Wistar rats before spinal cord injury. Acta Ortop Bras. 2010;18:26–30. [Google Scholar]
- Middleton JM, Sharwood LN, Cameron P, Middleton PM, Harrison JE, Brown D, McClure R, Smith K, Muecke S, Healy S. Right care, right time, right place: improving outcomes for people with spinal cord injury through early access to intervention and improved access to specialised care: study protocol. BMC Health Serv Res. 2014;14:600. doi: 10.1186/s12913-014-0600-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moradi-Arzeloo M, Farshid AA, Tamaddonfard E, Asri-Rezaei S. Effects of histidine and vitamin C on isoproterenol-induced acute myocardial infarction in rats. Vet Res Forum. 2016;7:47–54. [PMC free article] [PubMed] [Google Scholar]
- Namiki J, Tator CH. Cell proliferation and nestin expression in the ependyma of the adult rat spinal cord after injury. J Neuropathol Exp Neurol. 1999;58:489–498. doi: 10.1097/00005072-199905000-00008. [DOI] [PubMed] [Google Scholar]
- Nash HH, Borke RC, Anders JJ. Ensheathing cells and methylprednisolone promote axonal regeneration and functional recovery in the lesioned adult rat spinal cord. J Neurosci. 2002;22:7111–7120. doi: 10.1523/JNEUROSCI.22-16-07111.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngeow WC, Lim D. Do corticosteroids still have a role in the management of third molar surgery? Adv Ther. 2016;33:1105–1139. doi: 10.1007/s12325-016-0357-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niki H, Hosokawa S, Nagaike K, Tagawa T. A new immunofluorostaining method using red fluorescence of PerCP on formalin fixed paraffin-embedded tissues. J Immunol Methods. 2004;293(1-2):143–151. doi: 10.1016/j.jim.2004.07.009. [DOI] [PubMed] [Google Scholar]
- Oliveri RS, Bello S, Biering-Sørensen F. Mesenchymal stem cells improve locomotor recovery in traumatic spinal cord injury: systematic review with meta-analyses of rat models. Neurobiol Dis. 2014;62:338–353. doi: 10.1016/j.nbd.2013.10.014. [DOI] [PubMed] [Google Scholar]
- Pajoohesh-Ganji A, Byrnes KR, Fatemi G, Faden AI. A combined scoring method to assess behavioral recovery after mouse spinal cord injury. Neurosci Res. 2010;67:117–125. doi: 10.1016/j.neures.2010.02.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park SI, Lim JY, Jeong CH, Kim SM, Jun JE, Jeun SS, Oh WI. Human umbilical cord blood-derived mesenchymal stem cell therapy promotes functional recovery of contused rat spinal cord through enhancement of endogenous cell proliferation and oligogenesis. J Biomed Biotechnol. 2012;2012:362473. doi: 10.1155/2012/362473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peek EJ, Richards DF, Faith A, Lavender P, Lee TH, Corrigan CJ, Hawrylowicz CM. Interleukin-10-secreting ‘regulatory’ T-cells induced by glucocorticoids and beta2-agonists. Am J Respir Cell Mol Biol. 2005;33:105–111. doi: 10.1165/rcmb.2005-0100OC. [DOI] [PubMed] [Google Scholar]
- Quertainmont R, Cantinieaux D, Botman O, Sid S, Schoenen J, Franzen R. Mesenchymal stem cell graft improves recovery after spinal cord injury in adult rats through neurotrophic and pro-angiogenic actions. PLoS One. 2012;7:e39500. doi: 10.1371/journal.pone.0039500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saini V, Lutz D, Kataria H, Kaur G, Schachner M, Loers G. The polysialic acid mimetics 5-nonyloxytryptamine and vinorelbine facilitate nervous system repair. Sci Rep. 2016;6:26927. doi: 10.1038/srep26927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sámano C, Kaur J, Nistri A. A study of methylprednisolone neuroprotection against acute injury to the rat spinal cord in vitro. Neuroscience. 2016;315:136–149. doi: 10.1016/j.neuroscience.2015.12.003. [DOI] [PubMed] [Google Scholar]
- Saparov A, Chen CW, Beckman SA, Wang Y, Huard J. The role of antioxidation and immunomodulation in postnatal multipotent stem cell-mediated cardiac repair. Int J Mol Sci. 2013;14:16258–16279. doi: 10.3390/ijms140816258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sayer FT, Kronvall E, Nilsson OG. Methylprednisolone treatment in acute spinal cord injury: the myth challenged through a structured analysis of published literature. Spine J. 2006;6:335–343. doi: 10.1016/j.spinee.2005.11.001. [DOI] [PubMed] [Google Scholar]
- Sharma A, Tiwari R, Badhe P, Sharma G. Comparison of methylprednisolone with dexamethasone in treatment of acute spinal injury in rats. Indian J Exp Biol. 2004;42:476–480. [PubMed] [Google Scholar]
- Sharma A. Pharmacological management of acute spinal cord injury. J Assoc Physicians India. 2012;60(Suppl):13–18. [PubMed] [Google Scholar]
- Shibuya S, Miyamoto O, Auer RN, Itano T, Mori S, Norimatsu H. Embryonic intermediate filament, nestin, expression following traumatic spinal cord injury in adult rats. Neuroscience. 2002;114:905–916. doi: 10.1016/s0306-4522(02)00323-8. [DOI] [PubMed] [Google Scholar]
- Sinha A, Bagga A. Pulse steroid therapy. Indian J Pediatr. 2008;75:1057–1066. doi: 10.1007/s12098-008-0210-7. [DOI] [PubMed] [Google Scholar]
- Song F, Tian M, Zhang H. Molecular imaging in stem cell therapy for spinal cord injury. Biomed Res Int. 2014;2014:759514. doi: 10.1155/2014/759514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Su M, Chao G, Liang M, Song J, Wu K. Anticytoproliferative effect of vitamin C on rat hepatic stellate cell. Am J Transl Res. 2016;8:2820–2825. [PMC free article] [PubMed] [Google Scholar]
- Suberviola B, González-Castro A, Llorca J, Miñambres E. Early complications of high dose methylprednisolone in acute spinal cord injury patients. Injury. 2008;39:748–752. doi: 10.1016/j.injury.2007.12.005. [DOI] [PubMed] [Google Scholar]
- Takahashi Y, Tsuji O, Kumagai G, Hara CM, Okano HJ, Miyawaki A, Toyama Y, Okano H, Nakamura M. Comparative study of methods for administering neural stem/progenitor cells to treat spinal cord injury in mice. Cell Transplant. 2011;20:727–739. doi: 10.3727/096368910X536554. [DOI] [PubMed] [Google Scholar]
- Tohda C, Kuboyama T. Current and future therapeutic strategies for functional repair of spinal cord injury. Pharmacol Ther. 2011;132:57–71. doi: 10.1016/j.pharmthera.2011.05.006. [DOI] [PubMed] [Google Scholar]
- Uchida S, Hayakawa K, Ogata T, Tanaka S, Kataoka K, Itaka K. Treatment of spinal cord injury by an advanced cell transplantation technology using brain-derived neurotrophic factor-transfected mesenchymal stem cell spheroids. Biomaterials. 2016;109:1–11. doi: 10.1016/j.biomaterials.2016.09.007. [DOI] [PubMed] [Google Scholar]
- Wang Y, Yu X, Chen E, Li L. Liver-derived human mesenchymal stem cells: a novel therapeutic source for liver diseases. Stem Cell Res Ther. 2016;7:71. doi: 10.1186/s13287-016-0330-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xie L, Zeng X, Hu J, Chen Q. Characterization of nestin, a selective marker for bone marrow derived mesenchymal stem cells. Stem Cells Int 2015. 2015:762098. doi: 10.1155/2015/762098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yamazoe K, Mishima H, Torigoe K, Jima H, Watanabe K, Sakai H, Kudo T. Effects of atelocollagen gel containing bone marrow-derived stromal cells on repair of osteochondral defect in a dog. J Vet Med Sci. 2007;69:835–839. doi: 10.1292/jvms.69.835. [DOI] [PubMed] [Google Scholar]
- Yan M, Yang M, Shao W, Mao XG, Yuan B, Chen YF, Ye ZX, Liang W, Luo ZJ. High-dose ascorbic acid administration improves functional recovery in rats with spinal cord contusion injury. Spinal Cord. 2014;52:803–808. doi: 10.1038/sc.2014.135. [DOI] [PubMed] [Google Scholar]
- Yan M, Liu YW, Shao W, Luo ZJ. EGb761 improves histological and functional recovery in rats with acute spinal cord contusion injury. Spinal Cord. 2016;54:259–265. doi: 10.1038/sc.2015.156. [DOI] [PubMed] [Google Scholar]
- Yang M, Xiao J, Liu Y. Endogenous antioxidant level of stem cell is important for the transplantation efficacy. Inflamm Cell Signal. 2015;2:e946. [Google Scholar]
- Zhang D, Ma G, Hou M, Zhang TA, Chen LA, Zhao C. The neuroprotective effect of puerarin in acute spinal cord injury rats. Cell Physiol Biochem. 2016;39:1152–1164. doi: 10.1159/000447822. [DOI] [PubMed] [Google Scholar]
- Zhou KL, Chen DH, Jin HM, Zhang X. Effects of calcitriol on experimental spinal cord injury in rats. Spinal Cord. 2016;54:510–516. doi: 10.1038/sc.2015.217. [DOI] [PubMed] [Google Scholar]
- Zhu SF, Zhong ZN, Fu XF, Peng DX, Lu GH, Li WH, Xu HY, Hu HB, He JM, Su WY, He YL. Comparison of cell proliferation, apoptosis, cellular morphology and ultrastructure between human umbilical cord and placenta-derived mesenchymal stem cells. Neurosci Lett. 2013;541:77–82. doi: 10.1016/j.neulet.2013.03.018. [DOI] [PubMed] [Google Scholar]


