Abstract
Background
Suicide is among the leading causes of death for adults diagnosed with schizophrenia, with risk estimates being over eight folds greater than the general population. While the majority of research to date focuses on the role of symptoms of depression in suicide risk, there is a lack of consensus and understanding of the relationship between positive symptoms of psychosis and both suicidal ideation and attempt. The current study examined pathways of influence between symptoms of depression, positive symptoms of psychosis (i.e. hallucinations and delusions), hopelessness, and suicidal ideation among a population of adults diagnosed with schizophrenia.
Methods
Data were obtained from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE; n = 1460) at baseline. Suicidal ideation, hopelessness, and symptoms of depression were measured by the Calgary Depression Scale (CDRS) and hallucinations and delusions by the Positive and Negative Syndrome Scale (PANSS). Data were analyzed with Structural Equation Modeling (SEM) using Mplus 7.
Results
Symptoms of depression, positive symptoms of psychosis, and hopelessness independently predicted suicidal ideation. Hopelessness significantly mediated the relationship between symptoms of depression and suicidal ideation. Lastly, positive symptoms of psychosis were found to moderate the relationship between symptoms of depression and suicidal ideation.
Conclusions
The current study provides evidence for the role that positive symptoms of psychosis (specifically hallucinations and delusions) play in suicidal ideation, pointing towards the implication that beyond symptoms of depression, positive symptoms must be evaluated for and treated.
Keywords: Schizophrenia, Suicidal ideation, Positive symptoms of psychosis, Symptoms of depression, Structural equation modeling
1. Introduction
Suicide is among the leading causes of death for adults diagnosed with schizophrenia (De Hert et al., 2001; Lambert and Naber, 2012; Tarrier et al., 2013), with risk estimates being over eight times greater than among the general population (American Psychiatric Association, 2003). Data illustrate that up to 50% of individuals diagnosed with schizophrenia experience suicidal thoughts (Simms et al., 2007), up to 50% make suicide attempts (Pompili et al., 2007), and 4–13% end life by suicide (De Hert et al., 2001; Simms et al., 2007). These rates are comparable to lifetime prevalence of suicidal behavior among adults diagnosed with major depression (attempt: 30–40%, completion: 15–19%; Baca-Garcia et al., 2005; Isometsa, 2014) and bipolar disorder (attempt: 25–50%, completion: 11–19%; da Silva Costa et al., 2015; Jamison, 2000). The high suicide rate among adults diagnosed with schizophrenia is a major public health problem with limited understandings of risk and an absence of effective evidence-based interventions.
Demographic characteristics associated with suicidal ideation and attempt include race, gender, education, and poverty level. More specifically, findings indicate that risk is increased when an individual is single, male, White/Caucasian, unemployed, and has a higher level of education (Lambert and Naber, 2012; Tarrier et al., 2013). However, aside from these demographic associations, the leading research on risk for suicide among adults diagnosed with schizophrenia focuses on psychiatric factors, most specifically symptoms of depression. Data illustrate that up to 75% of adults diagnosed with schizophrenia experience symptoms of depression (Birchwood and Jackson, 2001). Within the same vein, hopelessness is an empirically established characteristic of depression (Kim et al., 2003) and substantial empirical evidence support the role of hopelessness, with or without the presence of a depression diagnosis, in suicidal ideation and attempt (Beck et al., 1975; Wasserman and Wasserman, 2009; Wenzel et al., 2009).
While research has largely examined the roles of symptoms of depression and hopelessness, there is a lack of consensus and understanding of the relationship between positive symptoms of psychosis and both suicidal ideation and attempt (Taylor et al., 2010). The few studies with supportive results found delusions and hallucinations to be independently associated with increased suicidal ideation and attempt (Hor and Taylor, 2010; Kaplan and Harrow, 1999; Siris, 2001). In accordance with Beck’s Cognitive Theory of Suicide, it is posited that hallucinations and delusions from a cognitive perspective may serve as events to which an individual ascribes meaning. This may subsequently result in negative emotional and behavioral reactions such as low mood, hopelessness, or suicidal thoughts and behaviors (Chadwick and Birchwood, 1994; Iqbal and Birchwood, 2006). A potential mechanism of influence between suicide and hallucinations are command auditory hallucinations (Kjelby et al., 2015). Epidemiologic data show that 50–66% of individuals diagnosed with schizophrenia hear auditory hallucinations (Resnick, 2015; Simms et al., 2007) and 18–50% of which report hallucinations to be command in nature (Harkavy-Friedman et al., 2003; Zisook et al., 1995). Rates of compliance with command auditory hallucinations have been shown to range from 40 to 88% and have the potential to include suicide related content (American Psychiatric Association, 2003; Hersh and Borum, 1998; Junginger, 1990).
The primary focus on symptoms of depression in research and limited understandings of the role positive symptoms of psychosis play in suicide risk highlight the need for research to clarify understandings (Taylor et al., 2010) and solidify symptoms to address in the future development of suicide prevention-focused interventions (American Psychiatric Association, 2003). Accordingly, the aims of the current study are to: (1) examine the relationships between symptoms of depression, positive symptoms of psychosis (i.e. hallucinations and delusions), hopelessness, and suicidal ideation among adults diagnosed with schizophrenia; (2) examine hopelessness as a mechanism by which symptoms of depression and suicidal ideation relate among adults diagnosed with schizophrenia; and, (3) examine how positive symptoms of psychosis (i.e. hallucinations and delusions) condition the way in which symptoms of depression and suicidal ideation relate among adults diagnosed with schizophrenia. It is hypothesized that: (1) as symptoms of depression, positive symptoms of psychosis, and hopelessness increase, there will be associated independent increases in suicidal ideation; (2) hopelessness will mediate the relationship between symptoms of depression and suicidal ideation; and, (3) the relationship between symptoms of depression and suicidal ideation will vary as a function of positive symptoms of psychosis, with increased positive symptoms worsening the effect of depression on suicidal ideation.
2. Methods
2.1. Study design
Data were obtained from the Clinical Antipsychotic Trials of Intervention Effectiveness (CATIE), a National Institute of Mental Health (NIMH) longitudinal randomized controlled trial comparing the effectiveness and tolerability of typical and atypical antipsychotic medications between 2001 and 2004 (Lieberman et al., 2003). Data in the current study were examined at baseline. Although the data included multiple time points, formal longitudinal modeling of lagged and prospective effects were not pursued because of the introduction of medications into the trial after baseline (which disrupts naturally occurring longitudinal dynamics) and because the amount of missing data post-baseline made prospective analyses problematic due to inadequate covariance coverage.
2.2. Procedure
Participants (n = 1460) were recruited from 57 clinical sites across the United States and completed screening before enrollment in the study. Individuals interested in participating in the study completed a screening visit to determine eligibility and appropriateness for enrollment, consisting of physical and psychiatric exams, laboratory tests, collection of patient history, and diagnostic assessments. All individuals interested in participating in the CATIE were also assessed for decision-making capacity using the MacArthur Competence Assessment Tool-Clinical Research (MacCAT-CR) to determine adequate capacity to consent in the study if deemed appropriate for enrollment after screening (Appelbaum and Grisso, 2001; Stroup and Lieberman, 2010). Inclusion criteria required that participants were adults (i.e. 18–65 years of age), residents of the United States, deemed appropriate for treatment with oral medication according to own judgment in consultation with treating physician, and met diagnostic criteria for schizophrenia based upon the DSM-IV using the Structured Clinical Interview for DSM-IV Axis I Disorders (Stroup et al., 2003) Exclusion criteria are presented in Lieberman et al. (2003), several of which include: (1) in first episode of schizophrenia, meaning first antipsychotic has been taken in the past 12 months or symptoms have been present for <3 years; (2) with well documented, drug-related, serious adverse reactions to at least one of the treatment arms; and, (3) with a medical condition that is serious and acutely unstable.
Individuals who met all criteria for enrollment continued to a baseline visit 21 days after screening and were randomized to a medication in Phase 1. During the baseline visit, participants were scheduled for a baseline assessment and evaluated with measures from the domains of clinical and functional status, neurocognition, and services utilization. All assessment raters were clinicians experienced in the clinical evaluation of patients with psychiatric disorders (e.g. physicians, psychologists, nurses, and social workers). All clinicians attended a several day training to receive detailed information on how to conduct interviews and complete scales including practice groups and evaluation for accuracy (Lieberman et al., 2003).
2.3. Measurement
Consistent with the Centers for Disease Control (CDC) definitions (Crosby et al., 2011) suicidal ideation was defined in the CATIE as thoughts of engaging in suicidal behavior with or without a definitive plan but with no evidence of current suicidal behavior (Witt et al., 2014). The outcome of suicidal ideation was measured at baseline by a single item from the Calgary Depression Scale (CDRS; Addington et al., 1990, 1993). The CDRS was administered by a trained clinician and originally coded as absent, mild, moderate, or severe. A positive rating of reported suicidal ideation was indicated by a score of mild or moderate (Addington et al., 1990; Witt et al., 2014), and was subsequently recoded as a dichotomous yes or no to experiencing suicidal ideation (incidence) in the past week.
The Calgary Depression Scale (CDRS; Addington et al., 1990) was used to measure symptoms of depression at baseline. The CDRS is a widely used well-validated scale to assess severity of depressive symptoms in individuals diagnosed with schizophrenia (Addington et al., 1993). As a result of hopelessness (mediating variable) and suicidal ideation (dependent variable) being measured within the CDRS, those two variables were removed from the scale. Thus, symptoms of depression were measured in the past week using 7 of the 9 items of the CDRS, including: depression, self-depreciation, guilty ideas of reference, pathological guilt, morning depression, early wakening, and observed depression. The scale was completed by a trained clinician and the total score was summed from each of the 7 individual items with higher scores indicating greater presence and severity of symptoms of depression are present. Reliability analyses indicated minimal change from this removal (original scale alpha was 0.83 at baseline and revised scale alpha was 0.78 at baseline). In addition, confirmatory factor analysis was applied to evaluate the psychometric properties of the revised scale. The global fit indices for the revised CDRS models pointed towards good model fit (χ2 = 7.042, df = 9, p-value <0.633; CFI = 1.000, RMSEA = 0.000, p-value for close fit = 1.000, standardized RMR = 0.010). All items loaded significantly onto their respective factor, with loadings ranging from 0.43 to 0.78, thus, treating them as unidimensional seemed reasonable.
A single item from the Calgary Depression Scale (CDRS; Addington et al., 1990) was used to measure hopelessness at baseline as there was no formal measure of hopelessness in the CATIE dataset. The hopelessness item within the CDRS specifically measured in the past week how a participant sees the future for him or herself, if a future can be seen or if life seems hopeless, and if the participant has given up or feels there is still a reason to keep trying. This item within the CDRS was completed by a trained clinician and scores ranged from 1 to 4 with scores indicating greater presence and severity of hopelessness.
Two positive symptoms of psychosis were of interest in the current study: hallucinations and delusions. Both hallucinations and delusions were measured with the Positive and Negative Syndrome Scale (PANSS; Kay et al., 1987) at baseline. Widely used in clinical studies of psychosis with strong reliability and validity, the PANSS is clinician administered and contains 30 items assessing symptoms including positive, negative, and general psychopathology. A continuous item from the PANSS represented a single indicator of hallucinations and specifically assessed for the verbal report or behavior indicating perceptions that were not generated by external stimuli (i.e. auditory, visual, olfactory, or somatic hallucinations). A separate continuous item from the PANSS represented a single indicator of delusions and specifically assessed for beliefs that are unfounded and idiosyncratic. Both variables ranged from 1 to 7 with higher scores indicating greater presence and severity of hallucinations and delusions. As a result of descriptive data indicating minimal ratings of extreme in the dataset, the categories of severe and extreme for each indicator were collapsed into one entitled severe, consistent with winsorising (Hasings et al., 1947).
2.4. Quantitative modeling and data analysis
Data were analyzed using Structural Equation Modeling (SEM) with Mplus 7 using a robust (Huber-White) maximum likelihood algorithm to deal with nonnormalty and variance heterogeneity. Missing data were treated using Full Information Maximum Likelihood (FIML) methods. For multi-item measures, coefficients alphas/composite reliabilities and factor structures were evaluated using confirmatory factor analyses. The fit of the SEM model was evaluated using both global (chi square, CFI, standardized RMR, RMSEA) and focused (standardized residuals and modification indices) fit indices. For good global fit, the Chi-Square test of fit should be non-significant, yet because of the large sample size, this global fit test is of marginal utility in the current study. A more appropriate significance test is the p value for close fit (PCLOSE), which tests for close fitting rather than perfect fitting models (Kenny et al., 2015).
The following covariates were included for the endogenous variables as they have been demonstrated in the literature to associate with suicidal ideation: demographic characteristics (race, gender, age, education, and public health insurance status as a proxy for socioeconomic status) and substance use and misuse. Although literature consistently supports a history of suicide attempt being the strongest predictor for future suicidal attempt (Goldsmith et al., 2002; Joiner et al., 2005; Nock et al., 2012), it was not possible in the current study to control for history of suicide attempt as a result of low base rates in the dataset (only 1.3% of the sample responded to this question). Lastly, correlations between hallucinations and delusions at baseline (r = 0.475, p < 0.01) were moderate and statistically significant, thus, the common variance of hallucinations and delusions were modeled by specifying a latent positive symptoms of psychosis variable.
3. Results
Demographic characteristics of participants at baseline are presented in Table 1. Of the 1460 participants in the sample, the mean age was 40.6 (±11.1) and 74% were male. The majority of the sample identified as White/Caucasian (60%) and non-Hispanic/Latino (88%). Eighty-eight percent were unmarried, 74% completed high school, and 92% did not work full time. About half of the sample (51%) reported having public health insurance and the mean duration of illness was 14.4 (±10.70), as measured by the number of years between the first antipsychotic was taken until randomization into the CATIE. The majority of the sample endorsed being abstinent to both drug (75.8%) and alcohol use (64.8%).
Table 1.
Demographic characteristics of the CATIE sample at baseline.
| Characteristic | n | % |
|---|---|---|
| Age (M ± SD) | 1460 | 40.55 ± 11.10 |
| Gender | ||
| Male | 1080 | 74 |
| Female | 380 | 26 |
| Race | ||
| Black | 513 | 35.1 |
| White | 874 | 59.9 |
| American Indian or Alaska native | 8 | 0.5 |
| Asian | 33 | 2.3 |
| Two or more races | 26 | 1.8 |
| Ethnicity | ||
| Hispanic/Latino/Spanish | 170 | 11.6 |
| Non-Hispanic/Latino/Spanish | 1290 | 88.4 |
| Marital status | ||
| Married | 167 | 11.4 |
| Not married | 1293 | 88.6 |
| Education | ||
| Completed HS | 1086 | 74.4 |
| Did not complete HS | 374 | 25.6 |
| Employment | ||
| Full time | 97 | 6.6 |
| Not full time | 1338 | 91.6 |
| Public insurance status | ||
| Have | 745 | 51.0 |
| Don’t have | 690 | 47.3 |
| Duration of illnessa (M ± SD) | 1388 | 14.37 ± 10.69 |
| Drug use | ||
| Use or misuse | 351 | 24.3 |
| Don’t use | 1097 | 75.8 |
| Alcohol use | ||
| Use or misuse | 509 | 35.1 |
| Don’t use | 939 | 64.8 |
Measured by the number of years between the first antipsychotic was taken until randomization into the CATIE.
As for clinical characteristics, the majority of participants experienced hallucinations (76%) and delusions (85%), while less than half of participants experienced varying severities of depression (44.4%) and hopelessness (42.1%) at baseline. As for the outcome, 17.1% of participants reported suicidal ideation. Participants who reported suicidal ideation had significantly greater severity of hopelessness (t(1444) = −15.59, p < 0.001), symptoms of depression (t(1444) = −19.06, p < 0.001), hallucinations (t(1442) = −5.364, p < 0.001), and delusions (t(1442) = −3.82, p < 0.001) as compared to participants who did not report suicidal ideation.
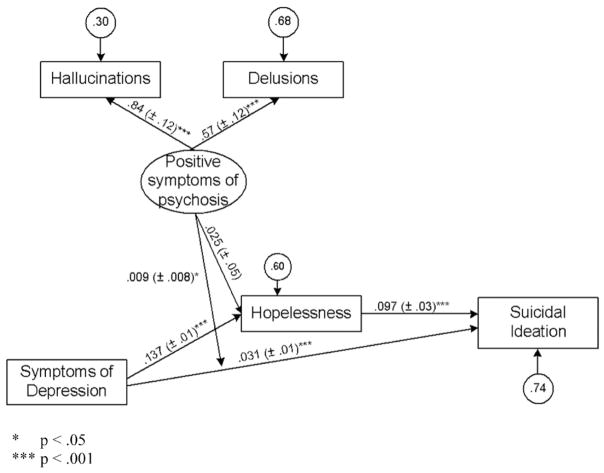
Fig. 1 presents the unstandardized parameter estimates for the structural model and standardized parameter estimates for the measurement model with margins of error in parentheses. Parameter estimates of each path are also reported in Table 2. Global fit indices all pointed to good model fit (χ2 = 68.34, df = 22, p-value = 0.001; CFI = 0.972, RMSEA = 0.038, p-value for close fit = 0.971, standardized RMR = 0.016) and focused fit indices (standardized residuals and modification indices) revealed no theoretically meaningful points of stress. Symptoms of depression, positive symptoms of psychosis, and hopelessness accounted for 26% of the variance in suicidal ideation.
Fig. 1.
Unstandardized and standardized parameter estimates with margins of error in parentheses. *p < 0.05 ***p < 0.001.
Table 2.
Parameter estimates of model paths.
| Parameter estimate | b | Margin of error | Critical ratio | p |
|---|---|---|---|---|
| Measurement modela | ||||
| Positive symptoms of psychosis → hallucinations | 0.838 | 0.12 | 10.65 | *** |
| Positive symptoms of psychosis → delusions | 0.568 | 0.12 | 9.70 | *** |
| Structural modelb | ||||
| Suicidal ideation → hopelessness | 0.097 | 0.03 | 5.67 | *** |
| Suicidal ideation → depression | 0.031 | 0.01 | 7.88 | |
| Suicidal ideation → positive symptoms of psychosis × depression (interaction) | 0.009 | 0.01 | 2.09 | * |
| Hopelessness → depression | 0.137 | 0.01 | 26.09 | *** |
| Hopelessness → positive symptoms of psychosis | 0.025 | 0.05 | 1.04 | |
p < 0.05.
p < 0.001.
Standardized coefficients.
Unstandardized coefficients.
3.1. Symptoms of depression and positive symptoms of psychosis
Findings indicated that symptoms of depression significantly predicted hopelessness and suicidal ideation independently. For every one unit increase in symptoms of depression, there was an associated increase in hopelessness by 0.137 units (MOE ± 0.01, critical ratio (CR) = 26.09, p < 0.001) on average, holding covariates and positive symptoms of psychosis constant. Since the estimated effects of depression on suicidal ideation were qualified by the proposed interaction effect of Aim 3, when positive symptoms of psychosis were held constant at its mean value, for every one unit increase in symptoms of depression, there was an average associated increase in suicidal ideation by 0.031 units (MOE ± 0.008, CR = 7.88, p < 0.001) holding covariates, hopelessness, and positive symptoms of psychosis constant. In other words, for every one unit increase in symptoms of depression there was, on average, an associated 3% increase in suicidal ideation holding all other variables constant.
Positive symptoms of psychosis were found to moderate the relationship between symptoms of depression and suicidal ideation (product term b = 0.009, MOE ± 0.008, CR = 2.09, p < 0.05), analyzed using the logic of product terms (Jaccard and Turrisi, 2003). This indicates that for every one unit increase in positive symptoms of psychosis, there was an associated 0.01 unit increase in the estimated effect of symptoms of depression on suicidal ideation on average, holding covariates and hopelessness constant. Essentially, the relationship between symptoms of depression on suicidal ideation fluctuated as a function of one’s severity of positive symptoms of psychosis, with greater severity of positive symptoms worsening the effect of symptoms of depression on suicidal ideation while holding covariates constant.
To further characterize the interaction effect, when positive symptoms were 2 units above the mean, for every one unit increase in symptoms of depression, there was an average associated 5% increase in suicidal ideation. When positive symptoms were 2 units below the mean, for every one unit increase in symptoms of depression there was an average associated 1% increase in suicidal ideation. As symptoms of depression increased, reporting of suicidal ideation was more pronounced for participants at greater levels of positive symptoms of psychosis.
3.2. Hopelessness
Findings indicated that hopelessness significantly predicted suicidal ideation. For every one unit increase in hopelessness, on average there was an associated increase in suicidal ideation by 0.097 units (MOE ± 0.03, CR = 5.67, p < 0.001) holding covariates, symptoms of depression, and positive symptoms of psychosis constant. Essentially, for every one unit increase in hopelessness there was, an associated 10% increase in suicidal ideation on average, holding all other variables constant. Hopelessness was found to significantly mediate the relationship between symptoms of depression and suicidal ideation as indicated by the joint significance test (MacKinnon et al., 2002).
3.3. Total effects
The total effects of depression on suicide were also investigated given that the effects of depression on suicidal ideation were both direct and indirect (mediation). When positive symptoms were at the mean, for every one unit increase in symptoms of depression, there was an average associated 4% increase in suicidal ideation holding all other variables constant. When positive symptoms were 2 units above the mean, for every one unit increase in symptoms of depression, there was an average associated 6% increase in suicidal ideation. When positive symptoms were 2 units below the mean, for every one unit increase in symptoms of depression there was an average associated 2.5% increase in suicidal ideation. The total effects of symptoms of depression on suicidal ideation show the effect of symptoms of depression on suicidal ideation to fluctuate based upon positive symptoms of psychosis.
4. Discussion
Due to the high rates of suicide and absence of effective evidence-based interventions, there is urgency in research to clarify understandings of suicide risk among adults diagnosed with schizophrenia as a first step towards solidifying symptoms to address in the future development of suicide prevention-focused interventions. The current study examined specific pathways of influence between symptoms of depression, positive symptoms of psychosis (i.e. hallucinations and delusions), hopelessness and reported suicidal ideation among a population of adults diagnosed with schizophrenia within the CATIE study. Findings indicated that: 1) symptoms of depression, positive symptoms of psychosis (i.e. hallucinations and delusions), and hopelessness independently predicted suicidal ideation; 2) hopelessness mediated the relationship between symptoms of depression and suicidal ideation; and, 3) positive symptoms of psychosis moderated the relationship between symptoms of depression and suicidal ideation. As anticipated, findings demonstrated the relationship between symptoms of depression and suicidal ideation fluctuate based upon positive symptoms of psychosis, with suicidal ideation being reported more among participants with greater levels of positive symptoms of psychosis as symptoms of depression increased.
4.1. Implications
Results support the involvement of depression, positive symptoms of psychosis, and hopelessness in suicidal ideation among adults diagnosed with schizophrenia in the CATIE study. The moderating effect of positive symptoms in the relationship between symptoms of depression and suicidal ideation supports the importance of including positive symptoms in discussions of risk factors for suicide among adults diagnosed with schizophrenia. While symptoms of depression have been consistently found in the literature to predict suicidal ideation, the current study’s findings provide support for the relationship between positive symptoms of psychosis, specifically hallucinations and delusions, and suicidal ideation over and above the relationship between depression and suicidal ideation. Furthermore, these findings point towards the implication that the subsequent risk for engaging in suicidal behaviors beyond that of depression cannot be ignored. As a result, it is recommended that clinicians to evaluate for and treat both symptoms of depression and positive symptoms of psychosis, as they both associate with suicidal ideation independently and over and above one another.
The mediating effect of hopelessness supports the consistent finding of the role that hopelessness plays in suicidal ideation and the relationship between depression and suicidal ideation. With hopelessness serving as a mechanism of suicide risk, it is recommended for clinicians to assess for and treat hopelessness in addition to other symptoms of depression due to its strong relation to suicidal ideation and attempt within the literature. An additional area of important consideration within suicide risk that ties into hopelessness is illness awareness. Studies show that risk for engagement in suicidal behaviors is heightened as insight increases (Pompili et al., 2004), and it is posited that individuals who are aware of symptoms and both cognitive and functional deterioration are more at heightened risk (Spiebl et al., 2002). Awareness of symptoms and prognosis overall may lead to feelings of hopelessness, depression, and ultimately suicide due to fears of further deterioration or beliefs that the future holds no positivity (Pompili et al., 2004). Future research should further examine and clarify the potential pathways between insight, hopelessness, depression, and suicidal behaviors as there is great potential for suicide-prevention focused interventions to consider the awareness spectrum.
Before discussing behavioral interventions, it is important to consider suicide risk assessment as a way to identify and quantify risk. Increased attention to suicide risk and systematic use of assessments are necessary for suicide prevention, however, there are little understandings of the implementation and efficacy of suicide risk assessment in clinical practice (Pedersen et al., 2014). Protocols for conducting suicide risk assessments vary greatly from setting to setting (Horowitz et al., 2009), and evidence illustrates that some individuals (e.g. those who abuse alcohol/drugs) are less likely to be assessed than others. One study in particular found that male participants with a diagnosis of schizophrenia were less likely than females to be assessed for suicide risk prior to psychiatric inpatient hospital discharge, despite literature supporting that risk increases when one is male (Goldacre et al., 1993; Pedersen et al., 2014; Rossau and Mortensen, 1997). Protocols not only need to be consistent, but also require different procedures as needed for differing populations and settings (Bourdeaux and Horowitz, 2014). In addition to protocols, it is also apparent that scales/tools to assess for suicide risk vary greatly as opposed to using universal tools. Tools may vary in number of questions asked, types of questions asked, reliability, and validity (Haney et al., 2012). Thus, it is important for future research efforts to examine varying assessments among differing patient populations and make clinical recommendations to heath care settings for protocol inclusion.
Few behavioral interventions tailored towards suicide prevention among adults diagnosed with schizophrenia have been designed and tested despite well-established risk among this population (Tarrier et al., 2014). Tarrier et al. (2013) recently developed an intervention for adults experiencing symptoms of psychosis: Cognitive Behavioral Suicide Prevention for psychosis (CBSPp). CBSPp aims to reduce suicidal behavior among individuals experiencing psychosis with specific focus on attention, appraisals, and schemas (Tarrier et al., 2014). The ultimate goal of this protocol-based intervention is to develop broad-minded attention, balanced appraisals, and alternative schemas about the self, world, and future that result in an exit from suicide schema (Tarrier et al., 2013). Case studies and a more recent small scale RCT (n = 49) have demonstrated significant improvements in positive symptoms of psychosis, symptoms of depression, and hopelessness after exposure to CBSPp (Tarrier et al., 2014). While this intervention is beginning to yield promising improvements in suicidal behaviors, future research efforts with larger samples and varying clinical settings are needed to evaluate the efficacy and impact of CBSPp.
4.2. Limitations
The current study’s findings must be considered in regards to several potential limitations. First, the CATIE study was not conducted to address the aims of the current study, thus, there were constraints in the dataset pertaining to measurement that would otherwise be modified in a primary study. Specifically, modifications were made to the Calgary Depression Scale (CDRS) as a result of hopelessness and suicidal ideation being items within the scale needed to measure other variables. Fortunately, reliability analyses indicated minimal change from this removal (original alpha = 0.83 and revised scale alpha = 0.78) and confirmatory factor analysis indicated all items functioned well together. An additional limitation pertaining to measurement was the use of single items for two constructs (hopelessness and suicidal ideation). It would be ideal if all constructs were measured by distinct scales, however, this was not possible given the absence of scales to independently measure hopelessness and suicidal ideation in the CATIE study. Future prospective research should include scales to measure each construct for more rigorous explorations of constructs within theoretical models.
Second, it has been suggested that antipsychotic effectiveness trials among individuals diagnosed with schizophrenia are less likely to recruit individuals reporting suicidal ideation and/or plans for attempt (Gilbody et al., 2002). Some studies may exclude individuals at risk for suicide and/or individuals at risk for suicide may be less interested in participating in a drug study. While the CATIE design used wide inclusion criteria and minimal exclusion criteria in comparison to many other drug trials (Stroup et al., 2003), it is important to consider that this limitation may further impact the ability to generalize findings to all adults diagnosed with schizophrenia in the U.S.
Lastly, self-report and social desirability is a common concern in mental health research and should be considered in the CATIE dataset. It is possible that participants respond to questions in a socially desirable way, especially when suicide is a topic of discussion. Some may feel ashamed or reluctant to share personal thoughts of wanting life to end and/or attempts that have been made. Future research should consider measuring social desirability with an established scale allowing for social desirability to be controlled for or collecting information from multiple sources (i.e. participant’s report, family report, medical records, and provider report).
4.3. Conclusions
While research to date largely focuses on the role of depression in suicide risk among adults diagnosed with schizophrenia, the current study provides evidence for the role that positive symptoms of psychosis (specifically hallucinations and delusions) play in suicidal ideation. Future prospective longitudinal study designs are needed to further increase understandings suicide risk within this population to ultimately inform evidence-based interventions aiming to reduce premature suicidal death.
Acknowledgments
Role of funding source
The study was funded by the National Institute of Mental Health. Funders had no role in the design, analysis, or interpretation of this study.
Data used in the preparation of this article were obtained from the limited access datasets distributed from the NIH-sponsored “Clinical Antipsychotic Trials of Intervention Effectiveness in Schizophrenia” (CATIE-Sz). This was a multisite, clinical trial of persons with schizophrenia comparing the effectiveness of randomly assigned medication treatment. The study was supported by NIMH Contract #N01MH90001 to the University of North Carolina at Chapel Hill. The ClinicalTrials.gov identifier is NCT00014001.
The CATIE project was carried out by principal investigators from the University of North Carolina, Duke University, Columbia University, the University of Southern California, the University of Rochester, and Yale University along with program staff of the Division of Interventions and Services Research, National Institutes of Mental Health (NIMH), and investigators from each of the 57 research sites in the United States. AstraZeneca Pharmaceuticals LP, Bristol-Myers Squibb Company, Forest Pharmaceuticals, Inc., Janssen Pharmaceutica Products, L.P., Eli Lilly and Company, Otsuka Pharmaceutical Co., Ltd., Pfizer Inc., and Zenith Goldline Pharmaceuticals, Inc., provided medications for the CATIE study.
This manuscript reflects the views of the authors and may not reflect the opinions or views of the CATIE-Sz Study Investigators or NIMH.
Footnotes
Contributor
LB conceptualized and designed the study, conducted analyses, interpreted findings, and generated the manuscript.
Conflict of interest
The author has no conflict of interest to declare.
References
- Addington D, Addington J, Schissel B. A depression rating scale for schizophrenics. Schizophr Res. 1990;3(4):247–251. doi: 10.1016/0920-9964(90)90005-r. [DOI] [PubMed] [Google Scholar]
- Addington D, Addington J, Maticka-Tyndale E. Assessing depression in schizophrenia: the Calgary Depression Scale. Br J Psychiatry. 1993;163(Suppl 22):39–44. [PubMed] [Google Scholar]
- American Psychiatric Association. Practice Guideline for the Assessment and Treatment of Patients With Suicidal Behaviors. 2003 Retrieved from http://psychiatryonline.org/guidelines.aspx. [PubMed]
- Appelbaum PS, Grisso T. MacArthur Competence Assessment Tool for Clinical Research. Professional Research Press; Sarasota, FL: 2001. [Google Scholar]
- Baca-Garcia E, Perez-Rodriguez MM, Sastre CD, Saiz-Ruiz J, de Leon J. Suicidal behavior in schizophrenia and depression: a comparison. Schizophr Res. 2005;75:77–81. doi: 10.1016/j.schres.2004.08.028. [DOI] [PubMed] [Google Scholar]
- Beck AT, Kovacs M, Weissman A. Hopelessness and suicidal behavior: an overview. JAMA. 1975;234:1146–1149. [PubMed] [Google Scholar]
- Birchwood M, Jackson C. Schizophrenia. Psychology Press; Philadelphia, PA: 2001. [Google Scholar]
- Bourdeaux ED, Horowitz LM. Suicide screening and assessment: designing instruments with dissemination in mind. Am J Prev Med. 2014;47:S163–S169. doi: 10.1016/j.amepre.2014.06.005. [DOI] [PubMed] [Google Scholar]
- Chadwick PD, Birchwood M. Challenging the omnipotence of voices: a cognitive approach to auditory hallucinations. Br J Psychiatry. 1994;164:190–201. doi: 10.1192/bjp.164.2.190. [DOI] [PubMed] [Google Scholar]
- Crosby AE, Ortega L, Melanson C. Self-Direction Violence Surveillance: Uniform Definitions and Recommended Data Elements. (Version 1.0) Centers for Disease Control and Prevention; National Center for Injury Prevention and Control; Atlanta, GA: 2011. [Google Scholar]
- da Silva Costa L, Alencar ÁP, Neto PJN, dos Santos MDSV, da Silva CGL, Pinheiro SDFL, … Reis AOA. Risk factors for suicide in bipolar disorder: a systematic review. J Affect Disord. 2015;170:237–254. doi: 10.1016/j.jad.2014.09.003. [DOI] [PubMed] [Google Scholar]
- De Hert M, McKenzie J, Peuskens J. Risk factors for suicide in young people suffering from schizophrenia: a long-term follow-up study. Schizophr Res. 2001;47:127–134. doi: 10.1016/s0920-9964(00)00003-7. [DOI] [PubMed] [Google Scholar]
- Gilbody S, Wahlbeck K, Adams C. Randomized controlled trials in schizophrenia: a critical perspective on the literature. Acta Psychiatr Scand. 2002;31:337–343. doi: 10.1034/j.1600-0447.2002.00242.x. [DOI] [PubMed] [Google Scholar]
- Goldacre M, Seagroatt V, Hawton K. Suicide after discharge from psychiatric inpatient care. Lancet. 1993;342:283–286. doi: 10.1016/0140-6736(93)91822-4. [DOI] [PubMed] [Google Scholar]
- Goldsmith SK, Pellmar TC, Kleinman AM, Bunney WE, editors. Reducing Suicide: A National Imperative. The National Academies Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- Haney EM, O’Neil ME, Carson S, Low A, Peterson K, Denneson LM, … Kansagra D. VA_ESP Project #05-255. Veterans Health Administration, Department of Veterans Affairs; Portland OR: 2012. Suicide risk factors and risk assessment tolls: a systematic review. [PubMed] [Google Scholar]
- Harkavy-Friedman JM, Kimhy D, Nelson EA, Venarde DF, Malaspina E, Mann JJ. Suicide attempts in schizophrenia: the role of command auditory hallucinations for suicide. J Clin Psychiatry. 2003;64:871–874. [PubMed] [Google Scholar]
- Hasings C, Mosteller F, Tukey JW, Winsor CP. Low moments for small samples: a comparative study of order statistics. Ann Math Stat. 1947;18:413–426. [Google Scholar]
- Hersh K, Borum R. Command hallucinations, compliance, and risk assessment. J Am Acad Psychiatry Law. 1998;26:353–359. [PubMed] [Google Scholar]
- Hor J, Taylor M. Suicide and schizophrenia: a systematic review of rates and risk factors. J Psychopharmacol. 2010;24(11):81–90. doi: 10.1177/1359786810385490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horowitz L, Ballard E, Paoa M. Suicide screening in schools, primary care and emergency departments. Curr Opin Pediatr. 2009;21:62–67. doi: 10.1097/MOP.0b013e3283307a89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal Z, Birchwood M. Suicide and cognition in schizophrenia. In: Ellis TE, editor. Cognition and Suicide: Theory, Research, and Therapy. American Psychiatric Association; Washington, DC: 2006. pp. 173–192. [Google Scholar]
- Isometsa E. Suicidal behavior in mood disorders: who, when, and why? Can J Psychiatr. 2014;59:120–130. doi: 10.1177/070674371405900303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jaccard J, Turrisi R. Interaction Effects in Multiple Regression. Sage Publications; Thousand Oaks, CA: 2003. [Google Scholar]
- Jamison KR. Suicide and bipolar disorder. J Clin Psychiatry. 2000;61:47–51. [PubMed] [Google Scholar]
- Joiner TE, Conwell Y, Fitzpatrick KK, Witte TK, Schmidt NN, Berlim MT, … Rudd MD. Four studies on how past and current suicidality relate even when “everything but the kitchen sink” is covaried. J Abnorm Psychol. 2005;114(2):291–303. doi: 10.1037/0021-843X.114.2.291. [DOI] [PubMed] [Google Scholar]
- Junginger J. Predicting compliance with command hallucinations. Am J Psychiatry. 1990;147:245–247. doi: 10.1176/ajp.147.2.245. [DOI] [PubMed] [Google Scholar]
- Kaplan JJ, Harrow M. Positive and negative symptoms as risk factors for later suicidal activity in schizophrenics versus depressives. Suicide Life Threat Behav. 1999;26(2):105–121. [PubMed] [Google Scholar]
- Kay SR, Fiszbein A, Opler LA. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr Bull. 1987;13(2):261–276. doi: 10.1093/schbul/13.2.261. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kaniskan B, McCoach DB. The performance of RMSEA in models with small degrees of freedom. Sociol Methods Res. 2015;44(3):486–507. [Google Scholar]
- Kim CH, Jayathilake K, Meltzer HY. Hopelessness, neurocognitive function, and insight in schizophrenia: relationship to suicidal behavior. Schizophr Res. 2003;60(1):71–80. doi: 10.1016/s0920-9964(02)00310-9. [DOI] [PubMed] [Google Scholar]
- Kjelby E, Sinkeviciute I, Gjestad R, Kroken RA, Loberg EM, Jorgensen HA, … Johnsen E. Suicidality in schizophrenia spectrum disorders: the relationship to hallucinations and persecutory delusions. Eur Psychiatry. 2015;30:830–836. doi: 10.1016/j.eurpsy.2015.07.003. [DOI] [PubMed] [Google Scholar]
- Lambert M, Naber D, editors. Current Schizophrenia. 3. Springer Healthcare; London, UK: 2012. [Google Scholar]
- Lieberman JA, McEvoy JP, Stroup TS. Comparative Effectiveness of Antipsychotic Medications in Patients With Schizophrenia (CATIE): Schizophrenia Protocol. University of North Carolina; Chapel Hill: 2003. [Google Scholar]
- MacKinnon DP, Lockwood CM, Hoffman JM, West SG, Sheets V. A comparison of methods to test mediation and other intervening variable effects. Psychol Methods. 2002;7(1):83. doi: 10.1037/1082-989x.7.1.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Borges G, Ono Y. Suicide: Global Perspectives From the WHO World Mental Health Surveys. Cambridge University Press; New York: 2012. [Google Scholar]
- Pedersen CG, Jensen SOW, Gradus J, Johnsen SP, Mainz J. Systematic suicide risk assessment for patients with schizophrenia: a national population-based study. Psychiatr Serv. 2014;65:226–231. doi: 10.1176/appi.ps.201200021. [DOI] [PubMed] [Google Scholar]
- Pompili M, Ruberto A, Kotzalidis GD, Girardi P, Tatarelli R. Suicide and awareness of illness in schizophrenia: an overview. Bull Menn Clin. 2004;68(4):297–318. doi: 10.1521/bumc.68.4.297.56643. [DOI] [PubMed] [Google Scholar]
- Pompili M, Amardor XF, Girardi P, Harkavy-Friedman J, Harrow M, Kaplan K, et al. Suicide risk in schizophrenia: learning from the past to change the future. Ann General Psychiatry. 2007;6:10–32. doi: 10.1186/1744-859X-6-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Resnick PJ. Detection of malingering. Audio-Digest Psychiatry. 2015:44. [Google Scholar]
- Rossau CD, Mortensen PB. Risk factors for suicide in patients with schizophrenia: nested case-control study. Br J Psychiatry. 1997;171:355–359. doi: 10.1192/bjp.171.4.355. [DOI] [PubMed] [Google Scholar]
- Simms J, McCormack V, Anderson R, Mulholland C. Correlates of self-harm behavior in acutely ill patients with schizophrenia. Psychol Psychother. 2007;80:39–49. doi: 10.1348/147608306X99386. [DOI] [PubMed] [Google Scholar]
- Siris SG. Suicide and schizophrenia. J Psychopharmacol. 2001;15(2):127–135. doi: 10.1177/026988110101500209. [DOI] [PubMed] [Google Scholar]
- Spiebl H, Tavacar R, Dernovesk MZ. Suicidal behavior of psychiatric inpatients. Acta Psychiatr Scand. 2002;100:383–388. [Google Scholar]
- Stroup TS, Lieberman JA, editors. Antipsychotic Trials in Schizophrenia: The CATIE Project. Cambridge University Press; 2010. [Google Scholar]
- Stroup TS, McEvoy JP, Swartz MS, Byerly MJ, Glick ID, Canive JM, … Lieberman JA. The National Institute of Mental Health clinical antipsychotic trials of intervention effectiveness (CATIE) project: schizophrenia trial design and protocol development. Schizophr Bull. 2003;29(1):15–31. doi: 10.1093/oxfordjournals.schbul.a006986. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Gooding P, Pratt D, Kelly J, Awenat Y, Maxwell J. Cognitive Behavioural Prevention of Suicide in Psychosis: A Treatment Model. Routledge; New York: 2013. [Google Scholar]
- Tarrier N, Kelly J, Maqsood S, Snelson N, Maxwell J, Law H, … Gooding P. The cognitive behavioural prevention of suicide in psychosis: a clinical trial. Schizophr Res. 2014;156:204–210. doi: 10.1016/j.schres.2014.04.029. [DOI] [PubMed] [Google Scholar]
- Taylor PJ, Gooding PA, Wood AM, Johnson J, Pratt D, Tarrier N. Defeat and entrapment in schizophrenia: the relationship with suicidal ideation and positive psychotic symptoms. Psychiatry Res. 2010;178:244–248. doi: 10.1016/j.psychres.2009.10.015. [DOI] [PubMed] [Google Scholar]
- Wasserman D, Wasserman C. Oxford Textbook of Suicidology and Suicide Prevention: A Global Perspective. Oxford University Press; New York: 2009. [Google Scholar]
- Wenzel A, Brown G, Beck AT. Cognitive Therapy for Suicidal Patients: Scientific and Clinical Applications. American Psychological Association; Washington: 2009. [Google Scholar]
- Witt K, Hawton K, Fazel S. The relationship between suicide and violence in schizophrenia: analysis of the clinical antipsychotic trials of intervention effective (CATIE) dataset. Schizophr Res. 2014;154(1–3):61–67. doi: 10.1016/j.schres.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zisook S, Byrd D, Kuck J, Jeste DV. Command hallucinations in outpatients with schizophrenia. J Clin Psychiatry. 1995;56:462–465. [PubMed] [Google Scholar]