Abstract
Purpose of Review
Brain-directed critical care for children is a relatively new area of sub specialization in Pediatric Critical Care. Pediatric neurocritical care teams combine the expertise of neurology, neurosurgery, and critical care medicine. The positive impact of delivering specialized care to pediatric patients with acute neurological illness is becoming more apparent, but the optimum way to implement and sustain the delivery of this is complicated and poorly understood. We aim to provide emerging evidence supporting that effective implementation of pediatric neurocritical care pathways can improve patient survival and outcomes. We also provide an overview of the most effective strategies across the field of implementation science that can facilitate deployment of neurocritical care pathways in the Pediatric Intensive Care Unit.
Recent Findings
Implementation strategies can broadly be grouped according to six categories: planning, educating, restructuring, financing, managing quality, and attending to the policy context. Using a combination of these strategies in the last decade, several institutions have improved patient morbidity and mortality. While much work remains to be done, emerging evidence supports that implementation of evidence based care pathways for critically ill children with two common neurological diagnoses-status epilepticus and traumatic brain injury-improves outcomes.
Summary
Pediatric and neonatal neurocritical care programs that support evidence based care can be effectively structured using appropriately sequenced implementation strategies to improve outcomes across a variety of patient populations and in a variety of health care settings.
Keywords: Pediatric neurocritical care, Implementation science, Pediatric traumatic brain injury, Neonatal status epilepticus
Introduction
Neurological outcome is a strong determinant of quality of life in children surviving critical illness. About 1:5 children admitted to the Pediatric Intensive Care Unit (PICU) have acute brain injury or a neurologic complication of critical illness (1). In recent years, several centers in the United States have established neurocritical care services to facilitate multidisciplinary care for critically ill children with acute neurological injury (1–7). One of the goals of such teams is to deploy evidence based pathways of care. Effective implementation of such pathways may reduce variability in practice and outcomes, with an overall positive impact on patient care. While the spectrum of neurological diagnosis in critically ill children is diverse and evidence for treatment for most of them is lacking, recent evidence supports best clinical practice pathways for children with severe traumatic brain injury (TBI), status epilepticus and brain injury from cardiac arrest.
Severe TBI is a leading cause of morbidity and mortality in children (7). Bench research in TBI has focused on developing pharmacological neuroprotective therapies and studying secondary insults that aggravate primary injury (i.e. hypoxemia, hypotension, hyperventilation and intracranial hypertension). While no effective pharmacological therapies have translated to the bedside, the association between secondary insults and poor outcome is consistently reported in clinical studies. Guidelines published by the Brain Trauma Foundation recommend avoidance of such secondary insults, and guideline based care has been associated with improved outcomes in both adult and pediatric patients with severe TBI (7–10).
While much less evidence is available for effective treatment of status epilepticus and neuroprotection after cardiac arrest, emerging clinical data shows progress. For example, two recent randomized clinical trials reported that maintenance of therapeutic normothermia after pediatric cardiac arrest is as effective as the induction of hypothermia (11, 12). For status epilepticus, seizure burden has been associated with short term outcome in critically ill children (13). While further study is needed to determine the impact on patient outcomes, initiation of electroencephalography monitoring and administration of antiepileptic therapy through a standardized protocol can reduce time to treatment by 50% and increased the rate of electrographic seizure termination (14, 15).
In addition to the above disease specific examples, there is evidence supporting improved outcomes by specialized teams providing care to pediatric patients with severe trauma or congenital heart disease (16–18). In the past decade, the initial successes observed with centers of excellence in trauma and congenital heart disease have been realized in the arena of adult neurocritical care (2). Of note, a recent meta-analysis of more than 40,000 adult patients with brain injury concluded that patients treated in a neurocritical care unit had improved mortality as well as improved neurological outcomes. The authors of the study attributed improved patient care to the specific expertise gained from health care providers in repeatedly caring for this specific patient population, reduction of unnecessary practice variation with adherence to protocols, and multi-modal neuromonitoring (19). Much remains to be learned about specific implementation strategies and metrics utilized at such centers, and their link to patient outcomes.
Implementation science is emerging as an important resource in the quest for sustainable reduction of the well-known gap between innovations in health care and their actual delivery in daily practice. In fact, the Institute of Medicine has identified the assessment of dissemination and implementation science as one of it’s top-quartile priorities in comparative effectiveness research. However, the field is relatively young and there are some key challenges that have been identified as barriers to widespread use of dissemination and implementation research in clinical practice (20). In this review we describe broad strategies within implementation science that may prove useful in the field of pediatric neurocritical care.
Implementation Strategies
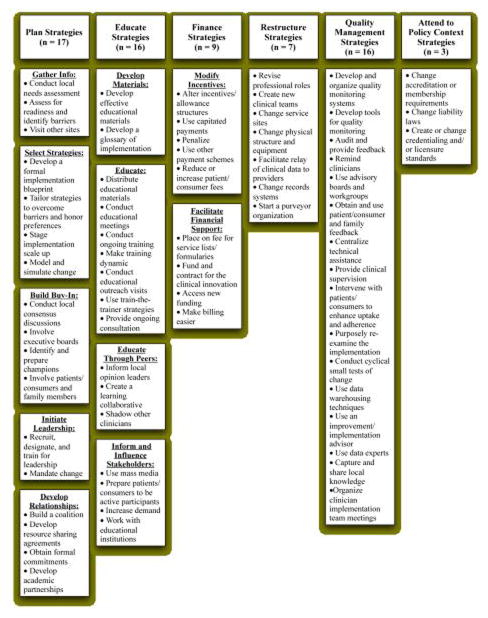
A recent review of the implementation literature by Powell and colleagues provides depth and clarity to implementation research and practice, providing a resource for those wishing to implement innovations in healthcare (20). The team defined an implementation strategy as a systematic intervention process to adopt and integrate evidence-based health innovations into usual care. They condensed 205 published implementation strategies into 68 discrete strategies arranged in 6 broad categories: planning, educating, restructuring, financing, managing quality, and attending to the policy context. Figure 1 (reproduced from Powell et al.) provides a concise summary of these 68 strategies. “Plan” strategies are meant to help stakeholders gather data, decide between implementation approaches, build buy-in, initiate leadership, and develop the relationships needed for successful implementation. “Educate” strategies focus on methods to inform relevant stakeholders about the innovation(s) in care and the implementation effort. “Finance” strategies are meant to incentivize adoption of new practices as well as provide the resources for training and ongoing programmatic support. “Restructure” strategies change the staffing availability, professional roles, physical workspace, equipment, and data systems. “Quality management” strategies ensure that it is impossible to deliver care in a way that is inappropriate or significantly different from the clinical innovation. Finally, strategies that “attend to the policy context” leverage the use of accrediting bodies, licensing boards, and legal systems to facilitate adoption of clinical innovations (20).
Figure 1.
A concise summary of the compilation of over 205 implementation strategies. (reproduced with permission from [20] Powell et al MCRR. 2012;69(2):123–57).
A successful implementation framework will include strategies from a variety of these groups. For example, sustainability of a historically successful method of improving outcomes for brain-injured patients will involve blending strategies from “plan”, “educate”, “finance”, and “restructure” in a cohesive and financially viable framework. (7). Below we explore recent examples of strategies used in fields related to neurocritical care and their impact on outcomes.
Application of implementation strategies in pediatric neurocritical care
In the past five years, there have been nine neurocritical care related papers showcasing improved patient care with the use of implementation strategies—four in the setting of traumatic brain injury, three in the setting of neonatal seizures, and one in the setting of general neurocritical care (7, 8, 21–27). These papers highlight the use of strategies in the “plan”, “educate”, “finance” and “restructure” groups to establish innovations in care and then utilize “quality management” to maintain this improvement in care. To date, there do not appear to be any strategies that “attend to the policy context”.
The five papers in severe TBI targeted patient outcomes, improved adherence to the BTF guidelines, and a decision support system for anesthesia during neurosurgical procedures. Three groups reported improvements in mortality and likelihood of discharge home with good neurologic outcome after severe TBI (7, 21). These teams relied extensively on the implementation strategies of planning, education, and restructuring of the health care delivery system in order to establish and/or disseminate protocols for effective prevention of secondary injury in traumatic brain injury. They restructured their hospital with a focus on facilitating a shared mental model and rapid communication among members of a multi-disciplinary team. Of note, these papers support that effective implementation strategies are feasible in either a large academic setting or in a community hospital setting. In the academic setting, probability of death decreased from 21% to 9.9% and probability of discharge home without assistance increased from 10.1% to 21.4% after the implementation of a pediatric neurocritical care program (7). At a second academic center O’Lynnger and colleagues reported similarly improved outcomes after standardizing ICU management of pediatric TBI by implementing best practice guidelines (8). In the community hospital setting, mortality decreased from 43% to 16%, severe disability decreased from 29.7% to 14.3%, and good outcomes improved from 27% to 69.6% (21). These papers support the use of guideline based implementation strategies to facilitate major improvements in both mortality and outcomes for severe TBI.
More recently, using a Plan-Do-Check-Act (PDCA) cycle, a continuous quality improvement model, Rakes and colleagues reported increased clinical guideline adherence (from 64% to 80%) in the PICU (27). Finally, using an existing anesthesia information management system, Kiatchai reported the development of a real-time pediatric TBI clinical decision support system that captures key performance indicators and generates alerts and guidance messages for anesthesia care during urgent neurosurgery procedures (26). These two important manuscripts also illustrate the value and feasibility of applying implementation science strategies to pediatric TBI care. The Brain Trauma Foundation guidelines for severe TBI are a good example of limited implementation despite wide dissemination and increasing evidence of effectiveness (28, 29). The examples above constitute progress in the field and highlight the importance of coupling implementation science strategies with progress in both basic and clinical research to achieve optimum impact.
The three papers improving outcomes in neonatal status epilepticus report decreased administration of seizure medications with possible adverse effects on neurodevelopment (22–24). Bashir’s group and Wiestock’s group specifically focus their implementation strategies on the development of a neonatal neurocritical care team in order to improve recognition and standardize treatment of seizures for patients with hypoxic ischemic encephalopathy. With the use of implementation strategies heavily focused on planning, educating, and restructuring healthcare delivery, these groups were able to significantly decrease the cumulative doses of phenobarbital without needing to prescribe additional or increased doses of other anti-epileptic medicines (22, 24). Haris’ group also used strategies focused on planning and educating, but did not rely as heavily on restructuring healthcare delivery at their institution. With the development of a protocol for management of neonatal status epilepticus, they were able to significantly decrease the progression of seizures from 46% to 36% of patients, serum phenobarbital concentration from 56.8 micrograms/mL to 41micrograms/mL, and length of stay by 9.7 days in survivors (23).
Given the global impact of acute neurological disease in critically ill children (30), wide dissemination of evidenced based practices continues to be an important aspect of practice. Wolbrink et al. recently developed an open-access, peer-reviewed, not-for-profit online learning platform (OPENPediatrics) with the goal of promoting postgraduate education for physicians, nurses, and others caring for critically ill children, opening opportunities for rapid, open-access dissemination of knowledge (25). As knowledge continues to be disseminated and tested for effectiveness, rigorous studies testing implementation strategies and the incorporation of implementation outcomes (i.e. acceptability, appropriateness, cost, feasibility, fidelity and sustainability) into clinical research will be needed to close the gap between knowledge and practice (31–33).
Conclusion
The field of pediatric neurocritical care is in the early stages of realizing the potential of implementation science. Effective implementation strategies can amplify the crucial work done in basic and translational research by closing the gap between knowledge and practice, increasing the impact of on patient survival and outcomes. A rigorous scientific approach to the development and testing of implementation strategies will be required, and barriers such as guideline credibility and applicability to individual patients, provider culture, communication style and attitudes towards care protocols will have to be addressed (34). As translational and clinical research continue to generate knowledge and strengthen clinical evidence, effective implementation science strategies will facilitate the application of precision medicine to neurocritical care, allowing care providers to identify, select and schedule therapies that are most likely to yield a favorable outcome for and individual patient (35). The small sample of studies reviewed here indicate that implementation strategies can be applied across a variety of demographics, neurological injury states and disease severity. Furthermore, these tools are a means for stakeholders in both academic and community hospital settings to improve the care they are able to deliver.
Effective implementation of pediatric neurocritical care pathways can improve patient survival and outcomes
Several institutions have improved patient morbidity and mortality with the following implementation strategies: planning, educating, restructuring, financing, and managing quality
These implementation strategies can be used across a variety of pathophysiologic processes (TBI, status epilepticus, post cardiac arrest) as well as in a variety of settings (small and large academic and community medical systems)
Acknowledgments
We would like to thank Dr Byron J. Powell for his permission to reproduce the figure used in this review.
Financial support and sponsorship: This work was supported by the St. Louis Children’s Hospital Foundation.
Footnotes
Conflicts of interest: None
References
- 1.Wainwright MS, Hansen G, Piantino J. Pediatric neurocritical care in the 21st century: from empiricism to evidence. Current opinion in critical care. 2016;22(2):106–12. doi: 10.1097/MCC.0000000000000288. [DOI] [PubMed] [Google Scholar]
- 2.Bell MJ, Carpenter J, Au AK, Keating RF, Myseros JS, Yaun A, et al. Development of a pediatric neurocritical care service. Neurocritical care. 2009;10(1):4–10. doi: 10.1007/s12028-008-9061-3. [DOI] [PubMed] [Google Scholar]
- 3.Cappell J, Kernie SG. Advances in pediatric neurocritical care. Pediatr Clin North Am. 2013;60(3):709–24. doi: 10.1016/j.pcl.2013.02.008. [DOI] [PubMed] [Google Scholar]
- 4.LaRovere KL, Graham RJ, Tasker RC Pediatric Critical Nervous System P. Pediatric neurocritical care: a neurology consultation model and implication for education and training. Pediatric neurology. 2013;48(3):206–11. doi: 10.1016/j.pediatrneurol.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 5.Murphy SA, Bell MJ, Clark ME, Whalen MJ, Noviski N. Pediatric Neurocritical Care: A Short Survey of Current Perceptions and Practices. Neurocritical care. 2015;23(2):149–58. doi: 10.1007/s12028-015-0120-2. [DOI] [PubMed] [Google Scholar]
- 6.Overby PJ, Beal JC, Yozawitz EG, Moshe SL. Introduction of a Pediatric Neurology Hospitalist Service With Continuous Electroencephalography Monitoring at a Children’s Hospital. Neurohospitalist. 2014;4(2):74–9. doi: 10.1177/1941874413519803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Pineda JA, Leonard JR, Mazotas IG, Noetzel M, Limbrick DD, Keller MS, et al. Effect of implementation of a paediatric neurocritical care programme on outcomes after severe traumatic brain injury: a retrospective cohort study. The Lancet Neurology. 2013;12(1):45–52. doi: 10.1016/S1474-4422(12)70269-7. [DOI] [PubMed] [Google Scholar]
- 8*.O’Lynnger TM, Shannon CN, Le TM, Greeno A, Chung D, Lamb FS, et al. Standardizing ICU management of pediatric traumatic brain injury is associated with improved outcomes at discharge. J Neurosurg Pediatr. 2015:1–8. doi: 10.3171/2015.5.PEDS1544. In this report the authors report were able to reproduce the results reported by Pineda et.al. [DOI] [PubMed] [Google Scholar]
- 9.Vavilala MS, Kernic MA, Wang J, Kannan N, Mink RB, Wainwright MS, et al. Acute care clinical indicators associated with discharge outcomes in children with severe traumatic brain injury. Crit Care Med. 2014;42(10):2258–66. doi: 10.1097/CCM.0000000000000507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gerber LM, Chiu Y-L, Carney N, Härtl R, Ghajar J. Marked reduction in mortality in patients with severe traumatic brain injury. Journal of Neurosurgery. 2013;119(6):1583–90. doi: 10.3171/2013.8.JNS13276. [DOI] [PubMed] [Google Scholar]
- 11**.Moler FW, Silverstein FS, Holubkov R, Slomine BS, Christensen JR, Nadkarni VM, et al. Therapeutic Hypothermia after In-Hospital Cardiac Arrest in Children. N Engl J Med. 2017;376(4):318–29. doi: 10.1056/NEJMoa1610493. This randomized clincal trial supports that outcomes are not different when using therapeutic normothermia after in-hospital cardiac arrest compared to hypothermia, a more intense temperature management strategy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12**.Moler FW, Silverstein FS, Holubkov R, Slomine BS, Christensen JR, Nadkarni VM, et al. Therapeutic hypothermia after out-of-hospital cardiac arrest in children. N Engl J Med. 2015;372(20):1898–908. doi: 10.1056/NEJMoa1411480. This randomized clincal trial supports that outcomes are not different when using therapeutic normothermia after out of hospital cardiac arrest compared to hypothermia, a more intense temperature management strategy. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Payne ET, Zhao XY, Frndova H, McBain K, Sharma R, Hutchison JS, et al. Seizure burden is independently associated with short term outcome in critically ill children. Brain. 2014;137(Pt 5):1429–38. doi: 10.1093/brain/awu042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14**.Williams RP, Banwell B, Berg RA, Dlugos DJ, Donnelly M, Ichord R, et al. Impact of an ICU EEG monitoring pathway on timeliness of therapeutic intervention and electrographic seizure termination. Epilepsia. 2016;57(5):786–95. doi: 10.1111/epi.13354. This report supports the feasibility and impact of timely administration of therapy for status epilepticus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Xie Y, Morgan R, Schiff L, Hannah D, Wheless J. A computerized standard protocol order entry for pediatric inpatient acute seizure emergencies reduces time to treatment. Journal of child neurology. 2014;29(2):162–6. doi: 10.1177/0883073812474950. [DOI] [PubMed] [Google Scholar]
- 16.Potoka DA, Schall LC, Gardner MJ, Stafford PW, Peitzman AB, Ford HR. Impact of pediatric trauma centers on mortality in a statewide system. The Journal of trauma. 2000;49(2):237–45. doi: 10.1097/00005373-200008000-00009. [DOI] [PubMed] [Google Scholar]
- 17.Kugler JD, Beekman RH, Iii, Rosenthal GL, Jenkins KJ, Klitzner TS, Martin GR, et al. Development of a pediatric cardiology quality improvement collaborative: from inception to implementation. From the Joint Council on Congenital Heart Disease Quality Improvement Task Force. Congenit Heart Dis. 2009;4(5):318–28. doi: 10.1111/j.1747-0803.2009.00328.x. [DOI] [PubMed] [Google Scholar]
- 18.Srinivasan C, Sachdeva R, Morrow WR, Gossett J, Chipman CW, Imamura M, et al. Standardized management improves outcomes after the Norwood procedure. Congenit Heart Dis. 2009;4(5):329–37. doi: 10.1111/j.1747-0803.2009.00323.x. [DOI] [PubMed] [Google Scholar]
- 19.Kramer AH, Zygun DA. Neurocritical care: why does it make a difference? Current opinion in critical care. 2014;20(2):174–81. doi: 10.1097/MCC.0000000000000076. [DOI] [PubMed] [Google Scholar]
- 20.Powell BJ, McMillen JC, Proctor EK, Carpenter CR, Griffey RT, Bunger AC, et al. A compilation of strategies for implementing clinical innovations in health and mental health. Medical care research and review: MCRR. 2012;69(2):123–57. doi: 10.1177/1077558711430690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bader MK, Stutzman SE, Palmer S, Nwagwu CI, Goodman G, Whittaker M, et al. The Adam Williams initiative: collaborating with community resources to improve care for traumatic brain injury. Critical care nurse. 2014;34(6):39–47. doi: 10.4037/ccn2014112. [DOI] [PubMed] [Google Scholar]
- 22*.Bashir RA, Espinoza L, Vayalthrikkovil S, Buchhalter J, Irvine L, Bello-Espinosa L, et al. Implementation of a Neurocritical Care Program: Improved Seizure Detection and Decreased Antiseizure Medication at Discharge in Neonates With Hypoxic-Ischemic Encephalopathy. Pediatric neurology. 2016;64:38–43. doi: 10.1016/j.pediatrneurol.2016.07.007. Demonstration of effective neurocritical care team implementation to improve outcomes in neonatal status epilepticus. [DOI] [PubMed] [Google Scholar]
- 23*.Harris ML, Malloy KM, Lawson SN, Rose RS, Buss WF, Mietzsch U. Standardized Treatment of Neonatal Status Epilepticus Improves Outcome. Journal of child neurology. 2016;31(14):1546–54. doi: 10.1177/0883073816664670. Demonstration of effective standardized protocol implementation to improve outcomes in neonatal status epilepticus. [DOI] [PubMed] [Google Scholar]
- 24**.Wietstock SO, Bonifacio SL, McCulloch CE, Kuzniewicz MW, Glass HC. Neonatal Neurocritical Care Service Is Associated With Decreased Administration of Seizure Medication. Journal of child neurology. 2015;30(9):1135–41. doi: 10.1177/0883073814553799. Demonstration of effective neurocritical care team implementation to improve outcomes in neonatal status epilepticus. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wolbrink TA, Kissoon N, Burns JP. The development of an internet-based knowledge exchange platform for pediatric critical care clinicians worldwide. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2014;15(3):197–205. doi: 10.1097/PCC.0000000000000051. [DOI] [PubMed] [Google Scholar]
- 26.Kiatchai T, Colletti AA, Lyons VH, Grant RM, Vavilala MS, Nair BG. Development and Feasibility of a Real-Time Clinical Decision Support System for Traumatic Brain Injury Anesthesia Care. Appl Clin Inform. 2017;8(1):80–96. doi: 10.4338/ACI-2016-10-RA-0164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27*.Rakes L, King M, Johnston B, Chesnut R, Grant R, Vavilala M. Development and implementation of a standardized pathway in the Pediatric Intensive Care Unit for children with severe traumatic brain injuries. BMJ Qual Improv Rep. 2016;5(1) doi: 10.1136/bmjquality.u213581.w5431. Systematic approach to improve guideline compliance. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bennett TD, Riva-Cambrin J, Keenan HT, Korgenski EK, Bratton SL. Variation in intracranial pressure monitoring and outcomes in pediatric traumatic brain injury. Arch Pediatr Adolesc Med. 2012;166(7):641–7. doi: 10.1001/archpediatrics.2012.322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bennett TD, Statler KD, Korgenski EK, Bratton SL. Osmolar therapy in pediatric traumatic brain injury. Crit Care Med. 2012;40(1):208–15. doi: 10.1097/CCM.0b013e31822e9d31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30*.Fink EL, Kochanek PM, Tasker RC, Beca J, Bell MJ, Clark RS, et al. International Survey of Critically Ill Children With Acute Neurologic Insults: The Prevalence of Acute Critical Neurological Disease in Children: A Global Epidemiological Assessment Study. Pediatric critical care medicine: a journal of the Society of Critical Care Medicine and the World Federation of Pediatric Intensive and Critical Care Societies. 2017 doi: 10.1097/PCC.0000000000001093. Emphasizes worldwide opportunities to optimize care for critically ill children with neurological diseases. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, et al. Outcomes for implementation research: conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Health. 2011;38(2):65–76. doi: 10.1007/s10488-010-0319-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Glasgow RE, Vinson C, Chambers D, Khoury MJ, Kaplan RM, Hunter C. National Institutes of Health approaches to dissemination and implementation science: current and future directions. American journal of public health. 2012;102(7):1274–81. doi: 10.2105/AJPH.2012.300755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33*.Borgert MJ, Goossens A, Dongelmans DA. What are effective strategies for the implementation of care bundles on ICUs: a systematic review. Implement Sci. 2015;10:119. doi: 10.1186/s13012-015-0306-1. Highlights inherent characteristics of the ICU environment relevant to implementation science efforts. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Brolliar SM, Moore M, Thompson HJ, Whiteside LK, Mink RB, Wainwright MS, et al. A Qualitative Study Exploring Factors Associated with Provider Adherence to Severe Pediatric Traumatic Brain Injury Guidelines. J Neurotrauma. 2016;33(16):1554–60. doi: 10.1089/neu.2015.4183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buchman TG, Billiar TR, Elster E, Kirk AD, Rimawi RH, Vodovotz Y, et al. Precision Medicine for Critical Illness and Injury. Crit Care Med. 2016;44(9):1635–8. doi: 10.1097/CCM.0000000000002028. [DOI] [PubMed] [Google Scholar]