Abstract
Zirconias, the strongest of the dental ceramics, are increasingly being fabricated in monolithic form for a range of clinical applications. Y-TZP (yttria-stabilized tetragonal zirconia polycrystal) is the most widely used variant. However, current Y-TZP ceramics on the market lack the aesthetics of competitive glass-ceramics and are therefore somewhat restricted in the anterior region. This article reviews the progressive development of currently available and next-generation zirconias, representing a concerted drive toward greater translucency while preserving adequate strength and toughness. Limitations of efforts directed toward this end are examined, such as reducing the content of light-scattering alumina sintering aid or incorporating a component of optically isotropic cubic phase into the tetragonal structure. The latest fabrication routes based on refined starting powders and dopants, with innovative sintering protocols and associated surface treatments, are described. The need to understand the several, often complex, mechanisms of long-term failure in relation to routine laboratory test data is presented as a vital step in bridging the gaps among material scientist, dental manufacturer, and clinical provider.
Keywords: dental prostheses, ceramics, translucency, durability, graded structure, nanostructure
Introduction
Ceramics are increasingly being promoted as high-strength materials for dental prostheses (Denry and Kelly 2008; Kelly and Benetti 2011; Rekow et al. 2011; Zhang et al. 2016; Pieralli et al. 2017; Sulaiman et al. 2017). With the advent of digital-age chairside milling (Wiedhahn et al. 2016), coupled with novel rapid-sintering technology (Almazdi et al. 2012; Kaizer et al. 2017), fabrication of dental restorations is becoming more automated, time effective, and precise. The chief materials goal is the development of ceramics that have superior aesthetics with long-term durability. Prosthetic dentistry is an expansive and lucrative health business, so even minor improvements in material and fabrication technologies can have large economic ramifications for provider and patient.
Of all the restorative ceramics, yttria-stabilized tetragonal zirconia polycrystal (Y-TZP) is the most robust. There are several variants of Y-TZP, depending on additives and dopants, sintering profiles, and ensuing heat treatments (Green et al. 1989; Hannink et al. 2000; Kelly and Denry 2008). The main attraction is their exceptional mechanical properties, as well as their biocompatibility and resistance to corrosion. The greatest challenge is to produce them with sufficient aesthetics to match existing dentition. In this regard, Y-TZP has to compete with more translucent but weaker glass-ceramics, notably the lithia-based silicates (Pieger et al. 2014). The conventional approach to overcoming aesthetic deficiencies has been to powder-fire porcelain onto a zirconia core (Rekow et al. 2011), but bilayer structures of this kind are vulnerable to chipping and delamination, exacerbated by thermally induced residual stresses. Attempts to minimize this vulnerability have been made by milling veneer and framework separately and then joining them with either resin luting agents (Vita Rapid Layer technology) or fusion firing (Ivoclar IPS e.max CAD-on technology). However, luting agents are compliant, allowing flexure of the veneer, and fusion firing does not eliminate residual stresses. In addition, veneers increase the restoration thickness, meaning that more underlying tooth structure needs to be removed—hence, the recent push toward monolithic restorations, with focused efforts on counterbalancing durability and aesthetic requirements, as well as greater simplicity in fabrication and reduced demands on material thickness.
This article surveys the evolutionary development of current and prospective high-performing aesthetic dental zirconia ceramics. Even though Y-TZP can be manufactured with ultrahigh strengths by refined processing, it is nevertheless inherently brittle. Ceramics, including Y-TZP, do not approach the toughness of metals, meaning that fractures can propagate from any defect in a prosthetic structure. Restorations, as with the surrounding dentition, must survive bite forces that can exceed 500 N in a hostile oral environment. Long-term failure from a variety of fracture modes (Fig. 1) is a persistent concern (Zhang et al. 2013). Our focus will be on continuing attempts to introduce translucency into zirconia materials without unduly compromising mechanical integrity.
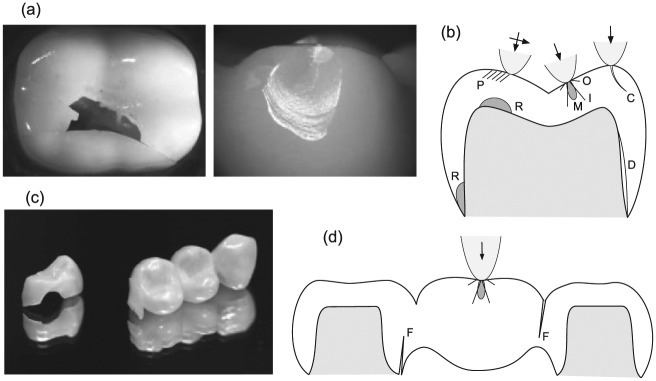
Figure 1.
Failure modes in ceramic prostheses from tensile stresses at the occlusal surface and cementation interface. (a) Images of failure in laboratory tests on crowns, splitting (left) and chipping (right), and (b) corresponding schematic diagram depicting various individual fracture modes: full cone cracks outside (O) and within (I) the contact zone; median cracks (M) beneath contact; partial cone cracks (P) from sliding; chipping cracks (C) adjacent to the side wall; flexure radial cracks (R) at the cementation surface, either below the contact or at the margins; delamination cracks (D) at the cementation/substrate interface. (c, d) Corresponding image and schematic diagram for fixed dental prosthesis, indicating dominant flexure cracks (F) at connector sites. Arrows indicate occlusal loading. Modified from Zhang et al. (2013).
Evolution of Dental Zirconias
Current Zirconia Ceramics
The advent of zirconia (ZrO2) as a high-performing ceramic has its origins in a classic paper by Garvie et al. (1975) and subsequent work of others in the materials science community (Green et al. 1989). It has evolved into several variants, depending on powder selection, sintering additives, heat treatment, and other processing factors. Pure zirconia has 3 principal phases: monoclinic (m) at room temperature, tetragonal (t) above ~1,170°C, and cubic (c) above ~2,370°C. While the m phase itself does not possess exceptional mechanical properties, enhanced strength and fracture toughness are achieved by measured incorporation of dopants into the starting powder so that the t phase is partially stabilized within the microstructure at room temperature. Reversion t → m transformations activated by externally applied stresses result in expansion and shape change within individual grains, thereby absorbing energy and affording damage resistance. Of the various dopants used, yttria (Y2O3) has proved to be the most effective in affording a combination of high strength and toughness. Thus, 3 mol% (5.2 wt%) yttria stabilized tetragonal zirconia polycrystal (3Y-TZP) has become the staple dental ceramic for prosthetic restorations (Denry and Kelly 2008; Kelly and Denry 2008).
Successive generations of commercial dental zirconias are listed in the Table. First-generation 3Y-TZPs contained 0.25 wt% alumina (Al2O3) sintering aid and exhibited strengths in excess of 1 GPa in flexure. However, those zirconias exhibited high opacity because of the inherent birefringence of noncubic zirconia phases, resulting in light scattering from grain boundaries, pores, and additive inclusions. They were chiefly indicated for framework materials in porcelain-veneered crowns and fixed dental prostheses (FDPs) in posterior and anterior regions. Long-term clinical failure rates, principally from chipping but in some cases including interfacial delamination, were higher than for metal-core counterparts (Christensen 2009; Sax et al. 2011; Larsson and Vult von Steyern 2013; Pang et al. 2015). 3Y-TZP has also been promoted as an alternative to titanium implants and abutments owing its more natural coloration, greater wear and corrosion resistance, improved biocompatibility and soft tissue integration, and lower affinity to bacterial plaque and peri- implantitis. However, clinical studies have indicated that early fracture rates of zirconia implants tend to be higher than titanium (Cionca et al. 2017; Pieralli et al. 2017), so improvement in mechanical integrity becomes an overriding concern.
Table.
Generations of Representative Dental Zirconias and Glass–Ceramics.
| Generation: Material | Manufacturer | Composition a | E, GPa | T, MPa·m1/2 | S, GPa |
|---|---|---|---|---|---|
| Zirconia | |||||
| 1 | |||||
| Lava Frame | 3M ESPE | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.2 to 1.5 |
| Prettau Zirconia | Zirconzhan | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.2 to 1.4 |
| KaVo Everest ZH | KaVo Dental | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.2 to 1.4 |
| Vita YZ T | Vita Zahnfabrik | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.1 to 1.3 |
| Zenostar MO | Wieland Dental | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.0 to 1.3 |
| 2 | |||||
| Lava Plus | 3M ESPE | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.1 to 1.3 |
| Cercon ht | Dentsply Sirona | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.1 to 1.3 |
| Vita YZ HT | Vita Zahnfabrik | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.0 to 1.2 |
| Bruxir Full-Strength | Glidewell | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 1.0 to 1.2 |
| Zpex | Tosoh | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 0.9 to 1.1 |
| Zenostar T | Wieland Dental | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 0.9 to 1.1 |
| Luxisse Dental | Heany | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 0.9 to 1.1 |
| Katana HT/ML | Kuraray Noritake | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 0.9 to 1.1 |
| inCoris TZI | Dentsply Sirona | 3Y-TZP (<15% c) | 200 to 210 | 3.5 to 4.5 | 0.9 to 1.1 |
| 3 | |||||
| Zpex 4 | Tosoh | 4Y-PSZ (>25% c) | 200 to 210 | 2.5 to 3.5 | 0.8 to 1.0 |
| IPS e.max ZirXAD MT | Ivoclar Vivadent | 4Y-PSZ (>25% c) | 200 to 210 | 2.5 to 3.5 | 0.8 to 0.9 |
| Zenostar MT | Wieland Dental | 4Y-PSZ (>25% c) | 200 to 210 | 2.5 to 3.5 | 0.6 to 0.8 |
| Katana ST/STML | Kuraray Noritake | 4Y-PSZ (>25% c) | 200 to 210 | 2.5 to 3.5 | 0.6 to 0.8 |
| Lava Esthetic | 3M ESPE | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.7 to 0.9 |
| Cercon xt | Dentsply Sirona | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.7 to 0.8 |
| DD cube X2 | Dental Direkt Materials | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.5 to 0.8 |
| BruxZir Anterior | Glidewell | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.6 to 0.7 |
| Prettau Zirconia | Zirconzhan | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.6 to 0.7 |
| Katana UT/UTML | Kuraray Noritake | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.5 to 0.6 |
| Zpex Smile | Tosoh | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.4 to 0.5 |
| Luxisse + | Heany | 5Y-PSZ (>50% c) | 200 to 210 | 2.2 to 2.7 | 0.4 to 0.5 |
| Lithia-silicate glass-ceramic | |||||
| 1 | |||||
| IPS e.max CAD | Ivoclar Vivadent | LS2 (4 wt% ZrO2) | 100 to 110 | 2.0 to 2.5 | 0.45 to 0.5 |
| IPS e.max Press | Ivoclar Vivadent | LS2 (4 wt% ZrO2) | 100 to 110 | 2.0 to 2.5 | 0.42 to 0.46 |
| 2 | |||||
| Obsidian | Glidewell | LS (4 to 6 wt% ZrO2) | 100 to 110 | 2.0 to 2.5 | 0.3 to 0.4 |
| 3 | |||||
| Celtra Duo | Dentsply DeTrey | LMS/LS2 (10 wt% ZrO2) | 106 to 110 | 2.0 to 2.5 | 0.35 to 0.4 |
| Celtra CAD | Dentsply DeTrey | LMS/LS2 (10 wt% ZrO2) | 100 to 106 | 2.0 to 2.5 | 0.35 to 0.4 |
| Suprinity | Vita Zahnfabrik | LMS/LS2 (10 wt% ZrO2) | 100 to 106 | 2.0 to 2.5 | 0.35 to 0.4 |
Data compiled from manufacturers and literature sources, with broad value ranges encompassing variability in reported values.
3Y-TZP, 3 mol% yttria partially stabilized tetragonal zirconia polycrystal; 4Y-PSZ, 4 mol% yttria partially stabilized zirconia; 5Y-PSZ, 5 mol% yttria partially stabilized zirconia; E, modulus; LMS, lithium metasilicate; LS, lithium silicate; LS2, lithium disilicate; S, flexural strength; T, fracture toughness; ZrO2, zirconia.
Cubic (c) phases in zirconia; ZrO2 content in glass-ceramic.
In an attempt to improve monolithic ceramics with acceptable translucency, processing of the next generation of 3Y-TZPs was refined largely by drastically reducing the concentration of alumina additive and eliminating porosity by sintering at a higher temperature. This led to modest improvement in translucency (Tong et al. 2016). While suitable for monolithic posterior restorations, these second-generation zirconias were still insufficiently aesthetic for use as monoliths in the anterior zone but at least paved the way to further improvements.
The next stage in monolithic zirconia development came with a move to include some transparent phase in the final product to reduce opacity. This was achieved by using a higher yttria content to produce partially stabilized zirconias, 4 mol% (4Y-PSZ) or 5 mol% (5Y-PSZ), with increased amounts of nonbirefringent c phase (Table). This markedly improved translucency, but strength and toughness were diminished because cubic zirconia does not undergo stress-induced transformation (Zhang et al. 2016). The most translucent 5Y-PSZ materials were indicated for broad usage as anterior crowns and FDPs. However, a recent study revealed a failure rate >2% over 5 y in the anterior zone (Sulaiman et al. 2016). Applications in minimally invasive restorations, such as veneers, inlays, and onlays, remain to be evaluated. Accordingly, appropriate caution needs to be exercised in placement of this class of zirconia restorative ceramic (Christensen 2016).
Mechanical properties for these variants of Y-TZP are included in the Table. For the most part, values were measured via standard laboratory test methods as reported by the manufacturers. Of particular note is the significant reduction in strength and toughness in successive, more translucent generations, forewarning the necessity for greater caution in clinical implementation. Typical first- and second-generation grain sizes lie in the range ~0.5 to 1 µm, encompassing the wavelength spectrum of visible light and thus accounting (along with t phase birefringence) for the characteristic opacity. A larger grain size (~1.5 µm), with greater content of c phase, accounts for the improved translucency in third-generation materials.
Zirconias versus Silica-Based Ceramics
Zirconia has a competitor in the dental ceramic market—namely, silica-based feldspathic porcelains and glass-ceramics. These latter materials are favored over the zirconias because of their superior translucency, attributable to their high glass content, with aesthetics to match that of natural enamel. An advantage of silicate ceramics is their capacity to be acid etched and silanized, promoting adhesion and reinforcement in resin bonding (Blatz et al. 2003). The most successful materials of this class are the lithia-based silicates (Table). The downside to the superior aesthetics is a comparatively lower strength and toughness, at least relative to first- and second-generation zirconias. However, glass-ceramics also have lower elastic modulus, which provides a better match to the underlying tooth support. The original versions consisted of lithium disilicate (LS2) crystallites embedded in a Li2O·2SiO2 glass matrix. The base glass composition contained up to 4 wt% ZrO2, with additives for color and opalescence. Another lithia-based glass-ceramic contained a thermodynamically stable lithium silicate (LS) crystalline phase, with little change in mechanical properties. A recent variant contained more lithium metasilicate than LS2 crystallites. In this generation, the base glass included 10 wt% ZrO2, ostensibly as a reinforcing agent. However, since the zirconia phase is not present in the form of dispersion-strengthening particles but rather subsumed into the glassy matrix, the lithium metasilicate/LS2 biphasic material again presents no significant gain in toughness.
Long-term clinical data support the use of LS2 glass-ceramics as single restorations in the anterior and posterior regions of the mouth (Kern et al. 2012; Gehrt et al. 2013), although multiple-unit restorations are not advised in the latter region.
Fracture and Fatigue
The quest for an optimal dental ceramic necessitates awareness of the various ways that a prosthesis may fail. There are 2 basic classes of fracture mode in crowns and FDPs (Fig. 1): one from concentrated near-field tensile stresses at the occlusal contact surface, the other from far-field tensile stresses in flexural loading. A detailed geometric description of these modes is given elsewhere (Zhang et al. 2013). The first class includes cone and median cracks emanating from a stationary or sliding contact (Hertzian) zone. The second class includes radial cracks originating from the intaglio cementation surface or connectors and interfacial delamination cracks. The first class of fractures is more likely to dominate in thicker restorations with lower elastic modulus mismatch relative to an underlying tooth substrate; the second, in thinner restorations with higher elastic mismatch (Lawn et al. 2002).
The quantities strength S and toughness T are inextricably involved in the failure of dental prostheses: S is the tensile stress to initiate fracture from microstructural or contact-induced flaws of the type shown schematically in Figure 2a and 2b; T is the capacity of the microstructure to inhibit subsequent crack propagation. Interestingly, a coarser microstructure generally diminishes S but enhances T (Green et al. 1989; Lawn 1993; Kelly and Denry 2008). Elastic modulus E is also a factor—a greater value for the restorative ceramic relative to the substrate dentin means that the stiffer prosthesis supports a greater proportion of stress, thereby increasing the risk of failure (Lawn et al. 2002).
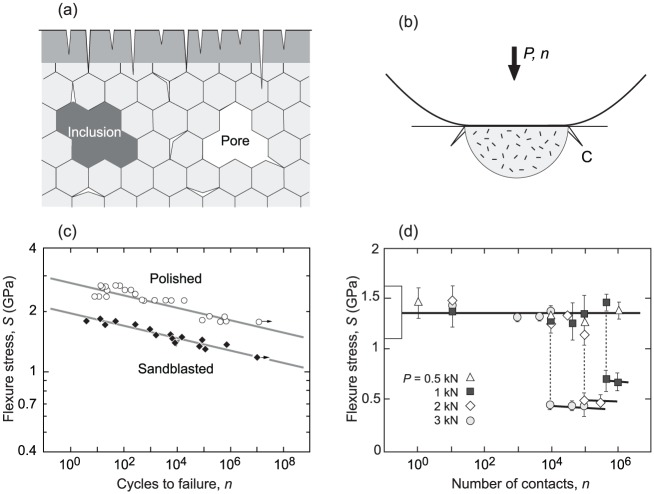
Figure 2.
Factors affecting durability of zirconia ceramics. (a) Schematic diagram showing flaws in ceramic structure: microcracks at internal grain boundaries and surface damage zone (shaded) from machining/sandblasting; pores and inclusions from sintering. (b) Schematic diagram of degradation from damage at surface from occlusal contact at load P (arrow) and number of cycles n, showing generation of quasiplastic zone with initiation of macroscopic cone-like crack (C) from microcrack coalescence. (c) Flexural stress versus number of cycles (S-n curve) for an ultrastrong 3Y-TZP in as-polished and heavily sandblasted states. Data from Zhang et al. (2004). (d) Static strength for a 3Y-TZP after repeat surface contact with a metal sphere (radius, 3.18 mm). Box at left axis designates laboratory strengths (unindented specimens, SD bounds). Data from Jung et al. (2000). Pronounced fatigue is apparent in both data sets. 3Y-TZP, 3 mol% yttria stabilized tetragonal zirconia polycrystal.
But durability is more than quoting static material properties from standardized laboratory tests. Properties can undergo progressive degradation from crack growth under cyclic loading, sometimes quite abruptly. In the mouth, a prosthesis must sustain repeat loading over years in a hostile environment. Two sets of cyclic test data on flat 3Y-TZP specimens in aqueous solutions demonstrate the potential extent of such degradation. In Figure 2c, the flexural stress S for an ultrastrong polished 3Y-TZP ceramic is plotted as a function of number of cycles n to spontaneous failure (Zhang et al. 2004). This degradation is attributable to slow crack growth from intrusion of water molecules into surface flaws (Wiederhorn 1972). As a rule of thumb, strength diminishes by a factor of 2 to 3 over a lifetime for ceramics (Zhang et al. 2004). In Figure 2d, single-cycle strength of a dental 3Y-TZP is measured after first loading prospective tensile surfaces with a hard spherical indenter for n cycles at applied load P (Jung et al. 2000). After a critical number of cycles, the strength drops by a factor of 2 to 3 again, depending on the contact load in the indentation experiment. In this case, the degradation is due to the coalescence of microcracks within the Hertzian contact zone to form a macroscopic cone-like crack (Lawn 1998), augmented in severe cases by hydraulic pumping into the microfissures (Zhang et al. 2013). If it were to be argued that loading with a hard metal ball represents an extreme case, the data in Figure 2d would suggest that Y-TZP restorations should be able to survive continual bite forces in excess of 500 N for several years. However, sliding contacts and ensuing wear facets from microcontacts with sharp intervening particulates (Zhang et al. 2013) can exacerbate the degradation process.
There is some evidence that later-generation zirconias with higher c content may be even more susceptible to contact-related damage, including damage from grit blasting and grinding (McLaren et al. 2017). This is attributable to diminished t → m transformation content, thus negating degradation from microcrack production by introduction of compressive (“work-hardening”) surface stresses. However, the addition of small amounts of oxide colorants and sintering additives does not appear to have a significant effect on fracture and fatigue properties (Spyropoulou et al. 2016).
Chemical Aging and Wear
3Y-TZP ceramics have also been shown to be susceptible to progressive chemical aging. Chemical aging, so-called low-temperature degradation (LTD), can occur in the presence of water at room temperature (Chevalier 2006). The aging process involves penetration of water into surface microcracks, inducing a reversion of metastable t phase zirconia back to its more stable m phase (Keuper et al. 2014). These reversions cause local mismatch strains, further driving the microcracks and transferring internal stresses deeper into the subsurface grain by grain. Ultimately, the microcracks coalesce and lead to grain detachment, with consequent degradation in strength. LTD can be mitigated by maintaining a smaller grain size with homogeneous yttria distribution and by judicious incorporation of small amounts (<0.5 wt%) oxide sintering additives (e.g., Al2O3, TiO2) and colorants (e.g., Fe2O3, Er2O3) (Lawson 1995; Nakamura et al. 2016). However, these additives do not form solid solutions with ZO2, and excessive amounts can cause internal stresses at the grain boundaries (Masaki 1986; Zhang et al. 2015). Zirconias with higher c content are less susceptible to aging, since that phase does not undergo transformation (Zhang et al. 2016).
Wear of zirconia prostheses and antagonistic enamel has been the subject of review (Passos et al. 2014). Notwithstanding a wide range of wear-based testing methods, zirconia materials, applied forces, loading cycles, and intermedium fluids, it was concluded that the wear rates of enamel were minimized when set against a highly polished zirconia surface. High surface polishes are a feature of all yttria zirconias because of their fine-grain sizes. Relative to other restorative materials, the wear rate of enamel from contact with polished zirconia was comparable to that of a resin-based composite but much less than that of a pressable lithium disilicate glass-ceramic (Sripetchdanond and Leevailoj 2014). Abrasiveness increased (in order) from polished, polished then glazed and stained, adjusted and glazed, and, finally, porcelain veneered (Lawson et al. 2014). Short-term clinical studies revealed that monolithic zirconia crowns caused more enamel wear than natural teeth but less than porcelain-veneered prostheses (Stober et al. 2014; Mundhe et al. 2015).
Novel Zirconias on the Horizon
Challenges for Next-Generation Zirconias
Challenges for future development of all-ceramic restorations were outlined in an earlier article, but principally they revolve around the use of tough ceramics as core materials for an overlying porcelain veneer (Rekow et al. 2011). As indicated, the focus has since shifted to monolithic zirconias, to circumvent issues with mismatch residual stresses and ensuing veneer chipping and delamination, as well as to alleviate material thickness requirements. Efforts are underway to improve the aesthetics of monolithic zirconia by using different dopants in the starting powders. For instance, incorporation of 0.2 mol% La2O3 into 3Y-TZP enhances translucency and aging resistance but with diminished mechanical properties (Zhang et al. 2016). Also, the translucency enhancement is not as high as 5Y-PSZ. Zirconia-toughened aluminas have achieved enhanced strengths and aging resistance (Ban et al. 2008) but with opacities still precluding use as anterior dental restorations.
Further experimentation with different dopants and associated sintering protocols to produce more translucent phases would appear to be a profitable line of research, with due attention to the pervasive trade-off between strength and aesthetics.
Graded Zirconia
One approach to achieving a more aesthetic zirconia without compromising mechanical properties involves infiltrating the outer surface with a feldspathic glass, to produce a cross section with a graded composition (Zhang and Kim 2009). Appropriate glass infiltration reduces the elastic modulus at cameo and intaglio restoration surfaces, closer to values for dental porcelains and glass-ceramics, with consequent diminishment of tensile stresses at cementation interfaces where flexurally induced radial cracking initiates.
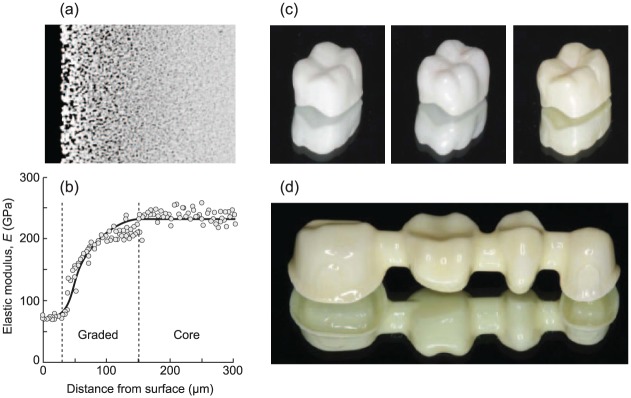
A cross-section view of such a glass-infiltrated 3Y-TZP ceramic is illustrated in Figure 3a, with a plot in Figure 3b showing the corresponding gradation in elastic modulus. Modulus values increase continuously from those for feldspathic glass at the outer surface toward those for bulk zirconia at ~150-µm depth in the interior. The graded zone is in some ways analogous to a glass-ceramic veneer but with continuous rather than abrupt change in elastic properties through the cross section, thereby eliminating the threat of delamination at a weak internal interface (Chai et al. 2014).
Figure 3.
Graded zirconia. (a) Cross section of 3Y-TZP (3 mol% yttria stabilized tetragonal zirconia polycrystal) after surface infiltration with glass. Dark region at left is residual glass layer. Note change in microstructure near the surface to a net depth of ~150 µm (skin depth: 30 µm + penetration: depth 120 µm). (b) Profile of elastic modulus. Vertical dashed lines delineate glass-layer, graded, and core regions. (c) Fabricated anatomically correct crowns (left to right—ungraded white, graded white, graded tinted) and (d) fixed dental prosthesis framework (graded tinted). After Ren et al. (2011).
Examples of anatomically correct crowns and an FDP framework based on infiltration technology are included in Figure 3c and 3d. Fracture tests on infiltrated flexure specimens relative to unfiltrated controls indicate significant increases in load-bearing capacity. Interestingly, toughness appears to be little affected. Similar improvements in single- and multicycle fracture resistance have been reported for graded FDPs (Villefort et al. 2017).
Efforts to optimize the infiltration protocol with alternative glasses and heat treatments are ongoing. Care needs to be exercised in selecting the right glass composition to achieve wetting and to avoid generating residual stresses within the material. Important side benefits of glass infiltration include a substantial increase in bond strength at the cementation interface (Chai et al. 2015) and the capacity to build in shade matching at the cameo surface, thereby diminishing the need for subsequent veneering (Ren et al. 2011).
Nanostructured Zirconia
We have indicated the limitation to translucency in zirconias owing to birefringent t and m phases. Light scattering from grain boundaries and other microstructural defects results in a largely opaque structure. Incorporation of c phase zirconia leads to some improvement in light transmittance but with concurrent diminution in mechanical properties. An alternative way to increase transmittance of Y-TZP is to reduce grain size well below the wavelength of visible light. Consideration of classical light-scattering models indicates that a grain size <100 nm is necessary to produce acceptable transmittance in Y-TZP ceramics (Zhang 2014). Production of zirconias with nanoscale grain sizes is technologically challenging, beginning with well-dispersed homogeneous starting nanopowders containing controlled concentrations of stabilizing additive. Such zirconia nanopowders are now becoming commercially available. Innovative processing routes then have to be devised to avoid porosity and excessive grain growth during sintering. These processing routes are currently being developed.
An example of a fully sintered nanoscale 3Y-TZP is shown in Figure 4. The microstructure image (Fig. 4a) shows a uniform distribution of t grains with a mean diameter of ~100 nm and a bulk density of 99.8%. Translucency of this microstructure is markedly improved relative to second-generation 3Y-TZP (Fig. 4b). A plot of measured transmittance for these 2 materials (Fig. 4c) demonstrates improvement over the entire visible light spectrum. Early mechanical testing on nanostructured 3Y-TZPs reveals improvements in strength, consistent with smaller intrinsic flaw sizes. The small grain size is also likely to inhibit reversion t → m transformations (Green et al. 1989), thereby cutting back on toughness but also reducing susceptibility to fatigue and chemical degradation. Again, the enhanced translucency diminishes the need for veneering.
Figure 4.
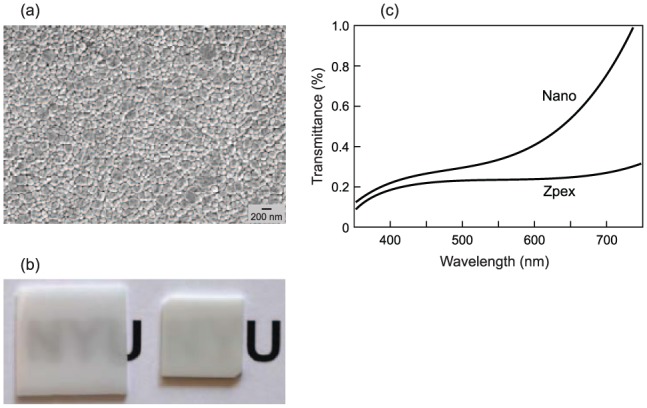
Nanoscale 3Y-TZP (3 mol% yttria stabilized tetragonal zirconia polycrystal), showing (a) small-grain microstructure, (b) improved transmittance of nanostructure slab (left) relative to second-generation Zpex (right), and (c) measured transmittance in visible spectrum for slabs of 1-mm thickness.
This area of research is in its infancy, but the early studies are confirming feasibility. They are demonstrating substantial improvements in translucency while preserving, even enhancing, strength properties. Attention to specific details in powder selection and preparation, yttria and other dopant content, green compact homogeneity, sintering temperatures, and postsintering coloration treatments are yet to be optimized.
Discussion
Prosthetic dentistry is witnessing a trend toward monolithic ceramic restorations. This trend is being accompanied by the development of chairside digital scanning and automated machining protocols for fabricating crowns and FDPs from ceramic blocks or pucks. The drive has been tempered by a fundamental trade-off: ceramics with the highest durability tend to be those with poorest translucency. Zirconia, specifically Y-TZP, has emerged as the most durable of the dental ceramics, with a combination of relatively high toughness (t → m transformation) and strength (small grain size). Zirconias have not yet achieved the opalescent qualities of more aesthetic (but weaker) lithia-based glass-ceramics, which remain the preferred material for anterior prostheses. However, the refinement continues, and novel aesthetic Y-TZP zirconias suitable for anterior prostheses (graded and nanoscale microstructures) are emerging.
It is crucial to view material development in the context of clinical practice. Zirconia ceramics are strong but not the easiest materials to work with. They are hard to adjust, repair, or replace, especially when they are adhesively bonded to tooth structure. Some recommend bonding full-coverage zirconia restorations with reduced adhesion resin-modified glass-ionomer cements (Hill and Lott 2011; Ramsey 2014). Because they are stronger, zirconia prostheses do not have to be so thick, necessitating less removal of supporting tooth tissue. However, for minimally invasive inlays, onlays, and veneers, good bonding is essential. Untreated zirconia surfaces require prior surface preparation—for example, by surface roughening by grit blasting to produce mechanical purchase (Kosmac et al. 1999) and chemical surface functionalization (Blatz et al. 2007; Blatz et al. 2018)—before any resin luting agents can be applied. The infiltration technique used to produce graded structures in Figure 3 affords a natural glass-rich surface for conventional etch-silane treatments.
In the pursuit of aesthetic zirconias, it is well to remain cognizant of degradable mechanical properties. Very little attention has been paid to distinctions among various failure modes in the clinical lifetime literature. Standardized static laboratory characterization of dental materials, characterized by data of the kind listed in the Table, offers only a cautionary glimpse into prospective performance. Flexural strengths >0.8 GPa to prevent crack initiation and toughnesses >5 MPa·m1/2 to provide damage tolerance once cracks do form have been viewed as desirable goals for monolithic 4 or more units prostheses (ISO 6872 2015), but quality control is also crucial to ensure reliability. However, introduction of extrinsic flaws from machining, grinding, sandblasting, and polishing during finishing and from contact damage and ensuing wear facets during repeat loading can degrade strengths by more than half. Toughness can be similarly degraded. This latter degradation is most pronounced for the toughest zirconias, as cyclic loading and chemical (LTD) interactions with water induce premature t → m reversions. A key to all kinds of progressive degradation modes in Y-TZP, hydrothermal aging, as well as mechanical fatigue is to avoid premature t → m transformation. A corollary is that the highest toughness is not a guarantee of best performance—the very mechanisms that provide toughening in the first place can be progressively reversed in long-term exposure to cyclic loading and chemical interaction. Accordingly, measured sacrifice in mechanical properties to promote enhanced translucency could afford long-term durability as well as aesthetic benefits. Failure modes can be many and complex (Fig. 1), and because of an inherent stability in crack growth in some cases, any one mode may be overtaken by another en route to failure. This makes it difficult to predetermine the fracture evolution from basic fracture parameters alone. In addition, there are other important factors that have an impact on performance over a lifetime. Ceramics are much more immune to biological attack than are their metal counterparts, an especially important consideration in implants. Wear is another—despite the high hardness of zirconia, antagonistic abrasion of opposing tooth enamel can be kept to a minimum by producing highly smoothed surfaces (Mundhe et al. 2015). In all these cases, in vivo degradation may be minimized by fabricating zirconias with homogeneous, fine-grain structures or by appropriate glass-infiltration treatments.
The future of zirconia or any other restorative ceramic rests with fundamental innovations in the materials science community, subsequent development by entrepreneurial dental manufacturers, and implementation by skilled clinical artisans. The challenge is to improve aesthetics while maintaining the high intrinsic strength of fine-grain microstructures. As always, it is a game of incremental improvements and compromises.
Author Contributions
Y. Zhang, contributed to conception, design, data acquisition, analysis, and interpretation, drafted and critically revised the manuscript; B.R. Lawn, contributed to conception, design, data analysis, and interpretation, drafted and critically revised the manuscript. Both authors gave final approval and agree to be accountable for all aspects of the work.
Footnotes
Funding was provided by the U.S. National Institutes of Health: National Institute of Dental and Craniofacial Research (grants R01DE017925, R01DE026279, and R01DE026772) and National Science Foundation (grant CMMI-0758530). The inclusion of commercial materials identified in this article is not to imply recommendation or endorsement by the National Institute of Standards and Technology.
The authors declare no potential conflicts of interest with respect to the authorship and/or publication of this article.
References
- Almazdi AA, Khajah KM, Monaco EA, Kim H. 2012. Applying microwave technology to sintering dental zirconia. J Prosthet Dent. 108(5):304–309. [DOI] [PubMed] [Google Scholar]
- Ban S, Sato H, Suchiro Y, Nakanishi H, Nawa M. 2008. Biaxial flexure strength and low temperature degradation of Ce-TZP/Al2O3 nanocomposite and Y-TZP as dental restoratives. J Biomed Mater Res B Appl Biomater. 87(2):492–498. [DOI] [PubMed] [Google Scholar]
- Blatz MB, Chiche G, Holst S, Sadan A. 2007. Influence of surface treatment and simulated aging on bond strengths of luting agents to zirconia. Quintessence Int. 38(9):745–753. [PubMed] [Google Scholar]
- Blatz MB, Sadan A, Kern M. 2003. Resin-ceramic bonding: a review of the literature. J Prosthet Dent. 89(3):268–274. [DOI] [PubMed] [Google Scholar]
- Blatz MB, Vonderheide M, Conejo J. 2018. The effect of resin bonding on long-term success of high-strength ceramics. J Dent Res. 97(2):132-139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai H, Kaizer M, Chughtai A, Tong H, Tanaka C, Zhang Y. 2015. On the interfacial fracture resistance of resin-bonded zirconia and glass-infiltrated graded zirconia. Dent Mater. 31(11):1304–1311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chai H, Lee JJ, Mieleszko AJ, Chu SJ, Zhang Y. 2014. On the interfacial fracture of porcelain/zirconia and graded zirconia dental structures. Acta Biomater. 10(8):3756–3761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chevalier J. 2006. What future for zirconia as a biomaterial? Biomaterials. 27(4):535–543. [DOI] [PubMed] [Google Scholar]
- Christensen GJ. 2009. Porcelain-fused-to-metal versus zirconia-based ceramic restorations. J Amer Dent Assoc. 140(8):1036–1039. [DOI] [PubMed] [Google Scholar]
- Christensen GJ. 2016. Translucent zirconias: tooth reduction and chairside adjustment issues; to refer or not to refer, that is the question. Clin Rep. 9(7):1–3. [Google Scholar]
- Cionca N, Hashim D, Mombelli A. 2017. Zirconia dental implants: where are we now, and where are we heading? Periodontology. 73(1):241–258. [DOI] [PubMed] [Google Scholar]
- Denry I, Kelly JR. 2008. State of the art of zirconia for dental applications. Dent Mater. 24(3):299–307. [DOI] [PubMed] [Google Scholar]
- Garvie RC, Hannink RH, Pascoe RT. 1975. Ceramic steel? Nature. 258(5537):703–704. [Google Scholar]
- Gehrt M, Wolfart S, Rafal N, Reich S, Edelhoff D. 2013. Clinical results of lithium-disilicate crowns after up to 9 years of service. Clin Oral Investig. 17(1):275–284. [DOI] [PubMed] [Google Scholar]
- Green DJ, Hannink RHJ, Swain MV. 1989. Transformation toughening of ceramics. Boca Raton (FL): CRC Press. [Google Scholar]
- Hannink RHJ, Kelly PM, Muddle BC. 2000. Transformation toughening in zirconia-containing ceramics. J Amer Ceram Soc. 83(3):461–487. [Google Scholar]
- Hill EE, Lott J. 2011. A clinically focused discussion of luting materials. Aust Dent J. 56 Suppl 1:67–76. [DOI] [PubMed] [Google Scholar]
- ISO 6872. 2015. Dentistry - Ceramic materials, 4th ed Geneva (Switzerland): International Organization of Standardization (ISO). [Google Scholar]
- Jung Y-G, Peterson IM, Kim DK, Lawn BR. 2000. Lifetime-limiting strength degradation from contact fatigue in dental ceramics. J Dent Res. 79(2):722–731. [DOI] [PubMed] [Google Scholar]
- Kaizer MR, Guess PC, Dos Santos MB, Cava SS, Zhang Y. 2017. Speed sintering translucent zirconia for chairside one-visit dental restorations: optical, mechanical, and wear characteristics. Ceram Int. 43(14):10999–11005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kelly JR, Benetti P. 2011. Ceramic materials in dentistry: historical evolution and current practice. Aust Dental J. 56 Suppl 1:84–96. [DOI] [PubMed] [Google Scholar]
- Kelly JR, Denry I. 2008. Stabilized zirconia as a structural ceramic: an overview. Dent Mater. 24(3):289–298. [DOI] [PubMed] [Google Scholar]
- Kern M, Sasse M, Wolfart S. 2012. Ten-year outcome of three-unit fixed dental prostheses made from monolithic lithium disilicate ceramic. J Amer Dent Assoc. 143(3):234–240. [DOI] [PubMed] [Google Scholar]
- Keuper M, Berthold C, Nickel KG. 2014. Long-time aging in 3 mol% yttria-stablized tetragonal zirconia polycrystals at human body temperature. Acta Biomater. 10(2):951–959. [DOI] [PubMed] [Google Scholar]
- Kosmac T, Oblak C, Jevnikar P, Funduk N, Marion L. 1999. The effect of surface grinding and sandblasting on flexural strength and reliability of Y-TZP zirconia ceramic. Dent Mater. 15(6):426–433. [DOI] [PubMed] [Google Scholar]
- Larsson C, Vult von Steyern P. 2013. Implant-supported full-arch zirconia-based mandibular fixed dental prostheses: eight-year results from a clinical pilot study. Acta Odontol Scand. 71(5):1118–1122. [DOI] [PubMed] [Google Scholar]
- Lawn BR. 1993. Fracture of brittle solids. Cambridge (UK): Cambridge University Press. [Google Scholar]
- Lawn BR. 1998. Indentation of ceramics with spheres: a century after Hertz. J Amer Ceram Soc. 81(8):1977–1994. [Google Scholar]
- Lawn BR, Deng Y, Miranda P, Pajares A, Chai H, Kim DK. 2002. Overview: damage in brittle layer structures from concentrated loads. J Mater Res. 17(12):3019–3036. [Google Scholar]
- Lawson NC, Janyavula S, Skylawer S, McLaren EA, Burgess JO. 2014. Wear of enamel opposing zirconia and lithium disilicate after adjustment, polishing and glazing. J Dent. 42(12):1586–1591. [DOI] [PubMed] [Google Scholar]
- Lawson S. 1995. Environmental degradation of zirconia ceramics. J Europ Ceram Soc. 15(6):485–502. [Google Scholar]
- Masaki T. 1986. Mechanical properties of Y-PSZ after aging at low temperature. Int J High Tech Ceram. 2(2):85–98. [Google Scholar]
- McLaren EA, Lawson N, Choi J, Kang J, Trujillo C. 2017. New high-translucent cubic-phase-containing zirconia: clinical and laboratory considerations and the effect of air abrasion on strength. Compend Cont Educat Dentistry. 38(6):e13–e16. [PubMed] [Google Scholar]
- Mundhe K, Jain V, Pruthi G, Shah N. 2015. Clinical study to evaluate the wear of natural enamel antagonist to zirconia and metal ceramic crowns. J Prosthet Dent. 114(3):358–363. [DOI] [PubMed] [Google Scholar]
- Nakamura K, Harada A, Ono M, Shibasaki H, Kanno T, Niwano Y, Adolfsson E, Milleding P, Ortengren U. 2016. Effect of low-temperature degradation on the mechanical and microstructural properties of tooth-colored 3Y-TZP ceramics. J Mech Behav Biomed Mater. 53:301–311. [DOI] [PubMed] [Google Scholar]
- Pang Z, Chughtai A, Sailer I, Zhang Y. 2015. A fractographic study of clinically retrieved zirconia-ceramic and metal-ceramic fixed dental prostheses. Dent Mater. 31(10):1198–1206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passos SP, Torrealba Y, Major P, Linke B, Flores-Mir C, Nychka A. 2014. In vitro wear behavior of zirconia opposing enamel: a systematic review. J Prosthodont. 23(8):593–601. [DOI] [PubMed] [Google Scholar]
- Pieger S, Salman A, Bidra AS. 2014. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: a systematic review. J Prosthet Dent. 112(1):22–30. [DOI] [PubMed] [Google Scholar]
- Pieralli S, Kohal RJ, Jung RE, Vach K, Spies BC. 2017. Clinical outcomes of zirconia dental implants: a systematic review. J Dent Res. 96(1):38–46. [DOI] [PubMed] [Google Scholar]
- Ramsey C. 2014. Predictable cementation for monolithic zirconia crowns. Dent Today. 33(2):114–116. [PubMed] [Google Scholar]
- Rekow ED, Silva NRFA, Coehlo PG, Zhang Y, Guess P, Thompson VP. 2011. Performance of dental ceramics: challenges for improvements. J Dent Res. 90(8):937–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ren L, Janal MN, Zhang Y. 2011. Sliding contact fatigue of graded zirconia with external esthetic glass. J Dent Res. 90(9):1116–1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sax C, Hämmerle CH, Sailer I. 2011. 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent. 14(3):183–201. [PubMed] [Google Scholar]
- Spyropoulou PE, Kamposiora P, Eliades G, Papavasiliou G, Razzoog MW, Thompson JY, Smith RL, Bayne SC. 2016. Composition, phase analysis, biaxial flexural strength, and fatigue of unshaded versus shaded procera zirconia ceramic. J Prosthet Dent. 116(2):269–276. [DOI] [PubMed] [Google Scholar]
- Sripetchdanond J, Leevailoj C. 2014. Wear of human enamel opposing monolithic zirconia, glass ceramic, and composite resin: an in vitro study. J Prosthet Dent. 112(5):1141–1150. [DOI] [PubMed] [Google Scholar]
- Stober T, Bermejo JL, Rammelsberg P, Schmitter M. 2014. Enamel wear caused by monolithic zirconia crowns after 6 months of clinical use. J Oral Rehab. 41(4):314–322. [DOI] [PubMed] [Google Scholar]
- Sulaiman TA, Abdulmajeed AA, Donavan TR, Cooper LF, Walter R. 2016. Fracture rate of monolithic zirconia restorations up to 5 years: a dental laboratory study. J Prosthet Dent. 116(3):436–439. [DOI] [PubMed] [Google Scholar]
- Sulaiman TA, Abdulmajeed AA, Shahramian K, Lassila L. 2017. Effect of different treatments on the flexural strength of fully versus partially stabilized monolithic zirconia. J Prosthet Dent. 118(2):216–220. [DOI] [PubMed] [Google Scholar]
- Tong H, Tanaka CB, Kaiser MR, Zhang Y. 2016. Characterization of three commercial Y-TZP ceramics produced for their high translucency. Ceram Int. 42(1 Pt B):1077–1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Villefort RF, Amaral M, Pereria GK, Campos TM, Zhang Y, Bottino MG, Valandro LF, deMelo RM. 2017. Effects of two grading techniques of zirconia material on the fatigue limit of full-contour 3-unit fixed dental prostheses. Dent Mater. 33(4):e155–e164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiederhorn SM. 1972. A chemical interpretation of static fatigue. J Amer Ceram Soc. 55(2):81–85. [Google Scholar]
- Wiedhahn K, Fritzsche G, Wiedhahn C, Schenk O. 2016. Zirconia crowns—the new standard for single-visit dentistry? Int J Comput Dent. 19(1):9–26. [PubMed] [Google Scholar]
- Zhang F, Inokoshi M, Batuk M, Hadermann J, Naert I, VanMeerbeek B, Vleugels J. 2016. Strength, toughness and aging stability of highly-translucent Y-TZP ceramics for dental restorations. Dent Mater. 32:e327–e337. [DOI] [PubMed] [Google Scholar]
- Zhang F, Vanmeensel K, Inokoshi M, Batuk M, Haderman L, VanMeerbeek B, Naert I, Vleugels J. 2015. Critical influence of alumina content on the low temperature degradation of 2-3 mol% yttria-stabilized TZP for dental restorations. J Europ Ceram Soc. 35(2):741–750. [Google Scholar]
- Zhang Y. 2014. Making yttria-stablized tetragonal zirconia translucent. Dent Mater. 30(10):1195–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Kim JW. 2009. Graded structures for damage resistant and aesthetic all-ceramic restorations. Dent Mater. 25(6):781–790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang Y, Lawn BR, Rekow ED, Thompson VP. 2004. Effect of sandblasting on the long-term strength of dental ceramics. J Biomed Mater Res B Appl Biomater. 71(2):381–386. [DOI] [PubMed] [Google Scholar]
- Zhang Y, Sailer I, Lawn BR. 2013. Fatigue of dental ceramics. J Dent. 41(12):1135–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]