Abstract
Introduction:
Health kiosks have been increasingly adopted to provide health-care services to those with limited access. Kiosks have the potential to reach people who may have undiagnosed health conditions or those who are not under regular physician care. Thus far, there is limited research assessing the usefulness of health kiosks in the community. This study aimed to explore the acceptability, usability, usefulness, and overall satisfaction of health kiosks in African American majority community settings.
Methods:
Two health kiosks were placed in predominantly African American low-income areas in an urban city in Western Pennsylvania. After the kiosk interaction, participants 18 years and older were recruited to complete a survey on their overall kiosk use experience. The technology acceptance model was adapted to develop the survey. Survey responses were analyzed using descriptive statistics. Qualitative survey responses were analyzed using content analysis.
Results:
Seventy-seven percent of the 31 survey respondents were female and 37.8% were ages 60 to 69 years old. Overall, 90% of participants were satisfied with their kiosk experience and 97% found the kiosk useful for health self-management, with 94% stating that they would use the kiosk again.
Conclusion:
This study showed that health kiosks are accepted among African Americans in community settings such as churches and community centers. Participants found the kiosks easy to use and an overall useful tool to help manage their health. Future studies are needed to provide a better understanding of health kiosk acceptance among minority populations and in community settings.
Keywords: health kiosks, community health, health-care services, technology
Introduction
The growth of kiosk use is constantly evolving with the primary role of providing members of the community who do not have direct access to health care a more accessible way to take control of their health and health information.1-4 Access to health services is particularly important for underserved communities due to the barriers they experience with accessing health information.5 Most kiosks are portable, interactive, and deliver information through the use of a touch screen computer.4 They are usually placed in clinical or community settings that are accessible to the public.4 According to a systematic review by Yvonne Chan et al,6 many studies found that kiosks have been shown to be effective educational tools regardless of the education level, age, or sex of the population.6 One study concluded that 90% of kiosk users learned something new about their overall health.7 Health kiosks can help to disseminate knowledge such as users’ vital signs, health information, or references to outside services like free clinics or rehabilitation centers.6-8
According to a systematic review conducted by Joshi and Trout,4 most research studies on health kiosks have been conducted in urban, clinical settings, with few examining their acceptability in community settings.4 Findings showed that previous studies have used many different theoretical frameworks to develop interventions using health kiosks (ie, health belief model, cultural tailoring, behavioral, cognitive, and humanistic theories); however, none have used the technology acceptance model (TAM), which guided data collection and analysis for this study.4 The majority of past kiosk studies in the United States targeted all races and ethnicities; consequently, there is limited research on the acceptability of health kiosks in African American communities.4 African Americans in particular have a higher burden of hypertension than any other racial group.9 Additionally, high-stress environments such as low socioeconomic status have been shown to increase blood pressure (BP) among African Americans.9 Consequently, this study aims to examine the acceptability, ease of use, and usefulness of a health screening kiosk that measures BP, weight, body mass index (BMI), and heart rate in low-income African American community settings.
Methods
Conceptual Framework
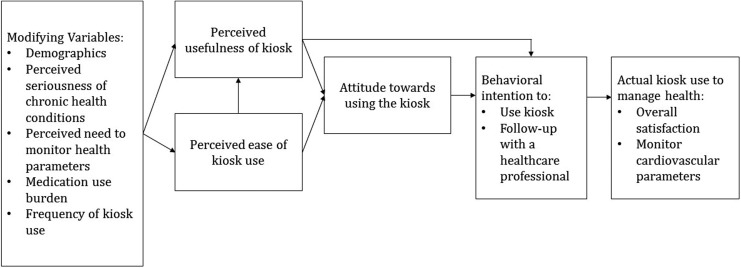
The TAM was adapted and used as a guiding framework for this study to develop the survey that examined kiosk acceptance, perceived usefulness (PU), and perceived ease of use (PEOU; Figure 1). The TAM is an adequate, reliable, and one of the most common information technology models that assesses the acceptance of technology and use by consumers.10-14 The TAM proposes that the actual use of a system can be predicted or explained by motivation, which is a result of external variables.15
Figure 1.
Conceptual framework for assessing kiosk use: adaption of the technology acceptance model (TAM).10,11
Setting
Two health kiosks (Figure 2) were implemented for 1 year in 2 locations in Western Pennsylvania. Both kiosks were located in low-income areas of an urban city where one was placed in a minority community center and the other at an African American church. Both kiosks were placed in low income areas of an urban city where one was located in a community center and the other at a predominantly African American church.16 The church is located in a predominantly African American low-income neighborhood. In each setting, the kiosk was placed in an area that was easily accessible.
Figure 2.
An example of the kiosk that was used in this stydy.
Data Collection
Health kiosk flyers were distributed to people at each setting and those aged 18 years and older were recruited to participate in the use of the health kiosk and an accompanied postuse survey. Written consent was obtained from all participants before kiosk use and survey completion. The survey was distributed to any returning users 6 months after the initial implementation of the kiosks. Survey questions addressed the following categories: frequency of kiosk use, kiosk satisfaction, reason for kiosk use, kiosk usefulness, kiosk ease of use, kiosk service improvement, medication use, post-kiosk follow-up with a health-care provider, and demographics. Data were collected from a total of 31 survey participants from November 2016 to February 2017. No compensation was provided to the participants. This study was approved by the institutional review board of University of Pittsburgh.
Data Analysis
Survey data were analyzed using descriptive statistics. Microsoft Excel was used for content thematic analysis of text survey data.
Results
The sample was predominantly female with a 4:1 female to male ratio. Educational attainment ranged from 29% obtaining some college, 26% obtaining a high school diploma/General Educational Development (GED), and 23% obtaining a graduate or professional degree as their highest level of education. Most (42%) earned an annual household income between US$25 000 and US$74 999, followed by 32.3% earning less than US$25 000 per year. The age ranged from 26 to 71, with 37.8% aged 60 to 69 years old (Table 1).
Table 1.
Demographics of Participants.a
| Sample Characteristics | Frequency, n (%) |
|---|---|
| Gender | |
| Male | 6 (19.4) |
| Female | 24 (77.4) |
| No response | 1 (3.2) |
| Age range | |
| 20-29 | 1 (3.2) |
| 30-39 | 1 (3.2) |
| 40-49 | 6 (19.4) |
| 50-59 | 8 (25.8) |
| 60-69 | 12 (38.7) |
| 70-79 | 1 (3.2) |
| No response | 1 (3.2) |
| Ethnicity | |
| Not Hispanic or Latino | 26 (83.9) |
| Hispanic or Latino | 1 (3.2) |
| No response | 4 (12.9) |
| Race | |
| Black or African American | 25 (80.6) |
| White | 2 (6.5) |
| Other | 2 (6.5) |
| 2 or more races | 2 (6.5) |
| Highest level of education | |
| High school diploma/GED | 8 (25.8) |
| Some college | 9 (29.0) |
| 4-year college degree | 6 (19.4) |
| Graduate or professional degree | 7 (22.6) |
| No response | 1 (3.2) |
| Annual household income | |
| Less than US$25 000 | 10 (32.3) |
| US$25 000-US$74 999 | 13 (41.9) |
| US$75 000-US$124 999 | 4 (12.9) |
| US$125 000 or more | 1 (3.2) |
| No response | 3 (9.7) |
aN = 31.
Among the 31 participants, 29 (94%) claimed they would use the health kiosk again if given the opportunity. Thirty (97%) of the participants found the kiosk easy to use and 29 (94%) stated they would recommend using the kiosk to a friend or family member. Of the 31 participants, 25 (81%) noted that based on their current technological/computer skills, they could operate the kiosk without any difficulty and 100% of participants claimed they were physically able to use the kiosk comfortably. A large portion (29/31, 94%) stated that learning how to operate the kiosk software was easy and 27 (87%) participants found it easy to navigate the kiosk. Overall, almost 90% of participants responded “satisfied” or “very satisfied” to the question “Overall, how satisfied were you with using the kiosk?”
Respondent input was also gathered on the topic of health kiosk improvement. One recurring recommendation from participants was to add a voice recording of their results and be provided with attached headphones. Participants also listed many other different locations they would like the kiosks to be placed. Common examples were easily accessible locations including grocery stores or supermarkets, pharmacies, schools, and health clinics. When asked about which health measurement was the most helpful, the majority of people answered BP and weight. However, most people recommended that additional health screenings such as blood sugar testing should be implemented to make the kiosk more useful.
The remaining survey questions revealed that 14 (45%) participants expressed interest in following up with a health-care professional after using the kiosk. The health-care professionals that participants felt the most comfortable following up with included a physician (n = 26, 84%), nurse (n = 8, 26%), pharmacist (n = 7, 23%), and a physician’s assistant (n = 7, 23%). A question asked if participants would be interested in talking with a pharmacist about their medications and most people (n = 26, 84%) indicated that they were not interested in following up with a pharmacist after using the kiosk.
Discussion
Health kiosks are a low-cost way for people with limited access to health-care services to monitor their health.4-6 The main purpose of this study was to examine the acceptability, PU, and PEOU of the kiosk in predominantly African American community settings. Study findings indicate that, in general, users were accepting of the health kiosk. Findings suggest that 94% of users found the kiosk easy to use and 97% of users found the feature and functions of the kiosk useful. Overall, the 90% satisfaction kiosk user rating confirms what similar studies have conducted in that most people are accepting of health kiosks.8,17 Another study finding that is consistent with previous research is that more women used the kiosk than men.5
Another relevant study revealed that beyond their success in increasing user knowledge, health kiosks have become potential facilitators in bridging the patient–provider engagement gap. In the study, 2 of the 37 questions asked whether users would be interested in following up with a health-care professional. Results indicate that the majority of users (n = 14, 45%) showed an interest in following up with a health-care professional. Most users have an interest in following up with physicians and some are also interested in following up with providers such as nurse practitioners, pharmacists, and physician assistants. This discovery is particularly noteworthy because like other studies, this study has shown that almost half of the kiosk users were more inclined to talk to physicians about various health-related topics after use.18 Therefore, these parallel conclusions support the notion that interactive health kiosks not only provide access to physical health parameters but also serve as conversation starters between physicians and patients.4,17,19-21
As of today, most kiosks focus on general health parameters such as BMI, BP, and weight. Research has shown that one route health kiosks could take is to make the services they provide more selective.22 Targeted kiosks could specialize in particular screenings, honing in on certain areas such as cardiovascular health or smoking cessation.18,22,23 Consequently, there are multiple opportunities for the future development of health kiosks.
Conclusion
This study indicates that overall, health kiosks are accepted by the majority of participants, perceived as easy to use, and beneficial for obtaining health-related information. Although findings from this study showed mostly positive kiosk feedback, they may not be generalizable to the African American population due to the small sample size. Future research on a larger scale is needed to examine kiosk acceptability among African Americans in urban, low-income community settings.
Acknowledgments
The authors thank Dr Jia Pu for assisting with data analysis.
Author Biographies
Olufunmilola Abraham, PhD, MS, BPharm, is an assistant professor at the Department of Pharmacy and Therapeutics, University of Pittsburgh School of Pharmacy.
Megha Patel, PharmD Candidate, is a second-year pharmacy student at the University of Pittsburgh School of Pharmacy.
Alison Feathers, BS, is a research assistant at the Department of Pharmacy and Therapeutics, University of Pittsburgh School of Pharmacy and a graduate student at the University of Pittsburgh Graduate School of Public Health.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential competing interests with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This publication was made possible by Grant Number 5 UL1 TR0000005 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCATS or NIH. Information on NCATS is available at http://www.ncats.nih.gov/.
References
- 1. Jones R. Making health information accessible to patients. Aslib Proc. 2003;55:334–338. [Google Scholar]
- 2. Nicholas D, Huntington P, Williams P, Chahal P. Determinants of health kiosk use and usefulness: case study of a kiosk which serves a multi-cultural population. Libri. 2001;51:102–113. [Google Scholar]
- 3. Lasky T, Kogut S, Campbell S, Risica PM. Computer kiosks to deliver medication information in the pharmacy. J Consum Health Internet. 2011;15(4):347–360. [Google Scholar]
- 4. Joshi A, Trout K. The role of health information kiosks in diverse settings: a systematic review. Health Info Libr J. 2014;31:254–273. [DOI] [PubMed] [Google Scholar]
- 5. Dulchavsky SA, Ruffin WJ, Johnson DA, Cogan C, Joseph CLM. Use of an interactive, faith-based kiosk by congregants of four predominantly, African-American churches in a metropolitan area. Front Public Health. 2014;2:106 doi:10.3389/fpubh.2014.00106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yvonne Chan YF, Nagurka R, Bentley S, Ordonez E, Sproule W. Medical utilization of kiosks in the delivery of patient education: a systematic review. Health Promot Perspect. 2014;4(1):1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Rosas LG, Trujillo C, Camacho J, Madrigal D, Bradman A, Eskenazi B. Acceptability of health information technology aimed at environmental health education in a prenatal clinic. Patient Educ Couns. 2014;97:244–247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Radvan D, Wigger J, Hazell T. HEALTH C.H.I.P.s: opportunistic community use of computerized health information programs. Health Educ Res. 2004;19(5):581–590. [DOI] [PubMed] [Google Scholar]
- 9. Musemwa N, Gadegbeku CA. Hypertension in African Americans. Curr Cardiol Rep. 2017;19:129. [DOI] [PubMed] [Google Scholar]
- 10. Or CKL, Karsh BT, Severtson DJ, Burke LJ, Brown RL, Brennan PF. Factors affecting home care patients’ acceptance of a web-based interactive self-management technology. J Am Med Inform Assoc. 2011;18(1):51–59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Venkatesh V, Morris MG, Davis GB, Davis FD. User acceptance of information technology: toward a unified view. MIS Q. 2003;27(3):425–478. [Google Scholar]
- 12. Davis F. Perceived usefulness, perceived ease of use, and user acceptance of information technology. MIS Q. 1989;13(3):319–340. [Google Scholar]
- 13. Wilson EV, Lankton NK. Modeling patients’ acceptance of provider-delivered E-health. J Am Med Inform Assoc. 2004;11(4):241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Keselman A, Logan R, Smith CA, Leroy G, Zeng-Treitler Q. Developing informatics tools and strategies for consumer-centered health communication. J Am Med Inform Assoc. 2008;15(4):473–483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. King WR, He J. A meta-analysis of the technology acceptance model. Information & Management. 2006;43(6):740–755. [Google Scholar]
- 16. The American City Coalition. http://tamcc.org/engagement/oakhill-pittsburgh-pa. Accessed September 22, 2017.
- 17. Thompson D, Lozano P, Christakis D. Parent use of touchscreen computer kiosks for child health promotion in community settings. Pediatrics. 2007;119(3):427–434. [DOI] [PubMed] [Google Scholar]
- 18. Hariri S, Goodyer L, Anderson C, Meyer J. CardioPharm: interactive multimedia health promotion software for community pharmacy. Nutr Food Sci. 1997;2:71–75. [Google Scholar]
- 19. Tan SSL, Goonawardene N. Internet health information seeking and the patient-physician relationship: a systematic review. J Med Internet Res. 2017;19(1):e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Nicholas D, Huntington P, Williams P. The impact of location on the use of information systems. J Doc. 2002;58:284–301. [Google Scholar]
- 21. Goldschmidt L, Goodrich GL. Development and evaluation of a point-of-care interactive patient education kiosk. J Telemed Telecare. 2004;10(1):30–32. [DOI] [PubMed] [Google Scholar]
- 22. Cupertino AP, Richter K, Cox LS, et al. Feasibility of a Spanish/English computerized decision aid to facilitate smoking cessation efforts in underserved communities. J Health Care Poor Underserved. 2010;21:504–517. [DOI] [PubMed] [Google Scholar]
- 23. Houle SKD, Chuck AW, Tsuyuki RT. Blood pressure kiosks for medication therapy management programs: business opportunity for pharmacists. J Am Pharm Assoc. 2012;52(2):188–194. [DOI] [PubMed] [Google Scholar]