Abstract
Gastrointestinal complaints without obvious organic causes confirmed by clinical laboratory analyses, endoscopy or radiology are often referred to functional entities. Irritable bowel syndrome (IBS) is the most common functional disorder in the gut. Careful examination of these patients may reveal other diagnoses of defined etiologies, e.g., enteric neuropathy, microscopic colitis, and primary Sjögre’s syndrome. The present case describes a young patient with incapacitating gastrointestinal symptoms presumed to be IBS, who underwent endoscopic full-thickness biopsy in sigmoid colon. Histopathological examination revealed degenerative enteric neuropathy, possibly secondary to chronic ischemia.
Keywords: endoscopic full-thickness biopsy, irritable bowel syndrome, gastrointestinal symptoms, degenerative enteric neuropathy
Gastrointestinal complaints without obvious organic causes confirmed by clinical laboratory analyses, endoscopy, or radiology are often referred to functional entities. Irritable bowel syndrome (IBS) is the most common functional disorder in the gut. Careful examination of these patients may reveal other diagnoses of defined etiologies, for example, enteric neuropathy, microscopic colitis, and primary Sjögren’s syndrome. The present case describes a young patient with incapacitating gastrointestinal symptoms presumed to be IBS, who underwent endoscopic full-thickness biopsy in the sigmoid colon. Histopathological examination revealed degenerative enteric neuropathy, possibly secondary to chronic ischemia.
Case presentation
This case report was approved by the Regional Ethics Review Board at Lund University (approval number 2015/786), and the patient gave written informed consent for participation and publication of this case report.
We present the case of a 13-year-old boy complaining of abdominal pain, which started after a traumatic incidence when falling from a tree. Over time, the pain turned chronic with increasing intensity. The pain was most prominent postprandial, with no relief related to bowel movements. As food intake provoked pain, nutrition became a problem and body weight varied significantly over time. He experienced no nausea or vomiting, but diarrhea was frequently present. A gastrointestinal work up was performed with normal esophagogastroduodenoscopy, colonoscopy, abdominal ultrasound, enterography, and laboratory analyses, which resulted in the diagnosis of IBS. Due to the complaints, the patient could not attend high school or work. Progressive depression and anxiety developed. Treatment with laxatives reduced diarrhea, which was suspected to be secondary to constipation. Analgesics used to reduce pain were of limited value. The patient consulted several healthcare institutions throughout the years, but the diagnosis of IBS persisted.
The patient was referred to our department of gastroenterology 17 years after symptom debut. Gastric-emptying scintigraphy (half-time 39 min), gastrointestinal transit time (1 day), and laboratory analyses were within normal reference values. Due to the aggravating symptoms inflicting on normal life, we decided to submit the patient to an endoscopic full-thickness biopsy (FTRD System, Ovesco Endoscopy AG, Tȕbingen, Germany).1 The sigmoid colon was chosen because of its easy access and the procedure was performed without any adverse events. Histopathological examination confirmed a full-thickness resection (20 × 16 mm) showing changes in the myenteric ganglia (Figure 1). The number of myenteric neurons was 57 neurons/10 mm (normal range: 53–167/10 mm2). Several neurons were hypertrophic/enlarged (50 µm), with or without vacuolated cytoplasm, whereas other neurons were shrunken with amphophilic cytoplasm and small hyperchromatic nuclei (Figure 2). Large lipofuscin granules accumulated in these neurons and a few lacunae after lysis of necrotized neurons were also observed (Figure 2), as well as enlarged nucleoli and chromatolysis in some neurons. Several neurons were negative or exhibited markedly reduced expression of B-cell lymphoma 2 (Bcl-2). There was hyperplasia and hypertrophy of the interstitial cells of Cajal (ICC) in both the intermyenteric plexus and within the circular muscle layer. The diagnosis was visceral degenerative vacuolar/hypertrophic neuropathy with hyperplasia/hypertrophy of the ICC. An angiography of the abdominal arteries revealed a decompressed celiac trunk and the diagnosis of median arcuate ligament syndrome (MALS) was suspected. The surgeons preferred no surgical intervention, since the stenosis was incomplete.
Figure 1.
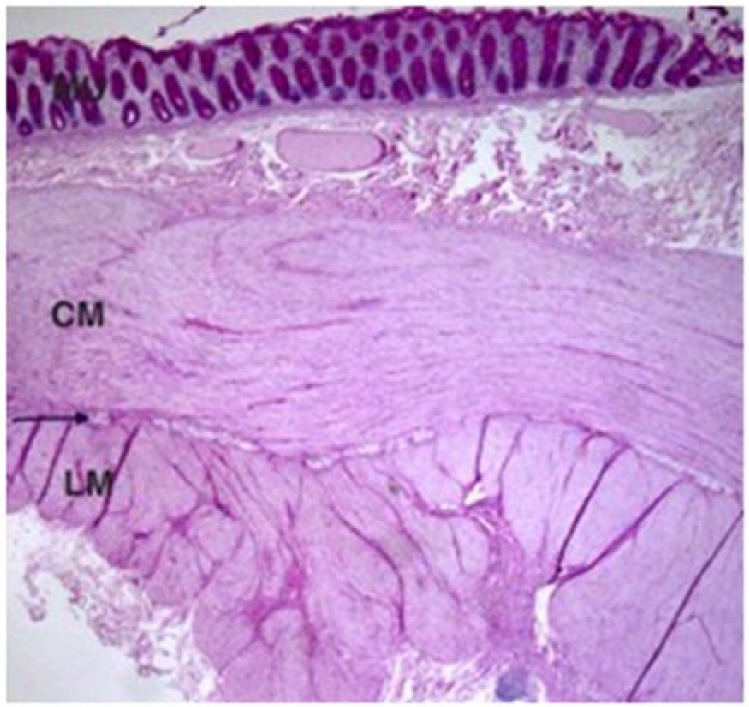
Endoscopic full-thickness biopsy showing the complete wall of the sigmoid colon (periodic acid-Schiff-diastase stain). Arrow points to the myenteric plexus. MU, mucosa; CM, circular muscle; LM, longitudinal muscle.
Figure 2.
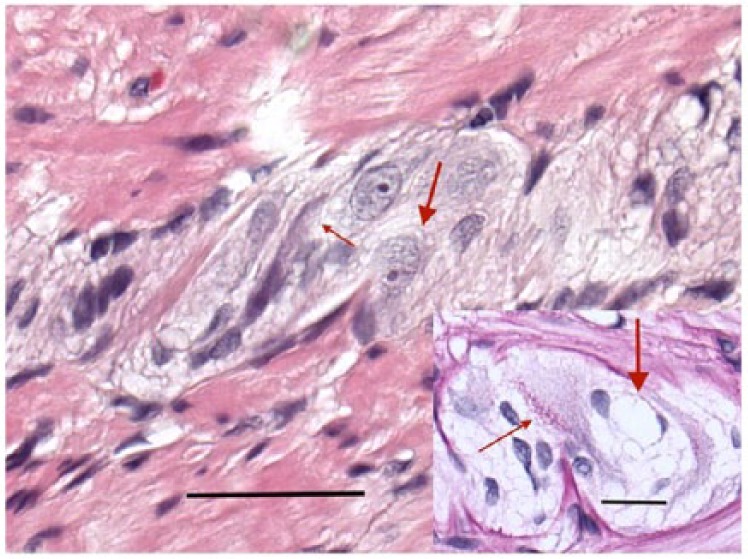
Myenteric ganglion with neurons showing vacuolated cytoplasm (thick arrow) and a shrunken, darker, amphophilic, pre-apoptotic neuron also with a few vacuoles (thin arrow) (hematoxylin and eosin stain) (bar: 50 µm). Insert: large accumulation of lipofuscin granules within a neuron (thin arrow). Thick arrow points to a lacuna after lysis of a necrotized neuron with the nuclei of two glial cells (periodic acid-Schiff-diastase stain) (bar: 20 µm).
Discussion
The present case report stresses the importance of a thorough anamnesis and clinical examination as a basis for making the diagnosis of IBS. One of the criteria for IBS is abdominal pain related to defecation.3 Furthermore, symptoms due to IBS seldom lead to weight changes and complete incapacity to study or work. Thus, variable body weight as well as severe and incapacitating abdominal pain should have led to the suspicion of alternative diagnoses than IBS.
MALS is an uncommon condition in young adults with chronic intermittent abdominal pain, nausea, and vomiting, followed by weight loss. The patients may be misdiagnosed due to overlap of physical and psychosocial symptoms with other gastrointestinal diseases, for example, IBS.4 The treatment of MALS is surgery to relieve the extrinsic compression. Nevertheless, a great number of patients undergoing surgery are not relieved of their symptoms.5
Suboptimal blood supply to the intestines may lead to chronic structural changes in the bowel wall.6 Convincing rat experiments have demonstrated that ischemia/reperfusion triggers nitric oxide release into the lumen, which in turn participates in the breakdown of the intestinal structures and loss of myenteric neurons.7,8 Experimental stroke models have described gastrointestinal dysmotility with altered levels of hormones and inflammatory cells.9 Focal ischemic stroke reduces the number of enteric neurons in parallel with central neural manifestations, mediated through systemic neuroimmune mechanisms involving galectin-3 and toll-like receptor 4.10 One hypothesis to the observed enteric neuropathy is therefore that intermittent ischemia may have caused ischemic/hypoxic neuropathy in the enteric nervous system (ENS). Another possibility to the neuropathy is idiopathic enteric neuropathy; decompression of the celiac trunk just being an incidental finding. The markedly reduced level of the anti-apoptotic protein Bcl-2 suggests an imbalanced apoptosis.11
From a scientific point of view, it seems extremely important to characterize etiology and pathology in cases with unclear abdominal complaints. Since the ENS has a huge reserve capacity, a great proportion of neurons may be lost before clinically apparent.12 The diagnosis of IBS must be set first after careful anamnesis and exclusion of alternative organic causes. At least a subgroup of IBS patients may suffer from unidentified enteric neuropathy. By clustering heterogenic cases, all named IBS, it will be impossible to find out etiologic agents and pathophysiological events, crucial for disease development. Methods to enable identification of enteric neuropathy by different etiologies must be developed to obtain clear patient groups suitable for optimal and directed treatment. Once enteric neuropathy is diagnosed, severe symptoms gain higher acceptability in society with improved access to healthcare and economic support.
This case represents one of our first patients undergoing endoscopic full-thickness resection and the FRTD System should be studied further in terms of specimen quality and patient safety. Reducing intraluminal gas extension, obtaining maximal grip with the FTRD-grasper, and avoiding suction are technical aspects that might improve tissue sampling. The FRTD System is not yet available in the USA, but the novel technique for gastric endoscopic muscle biopsy handles similar tissue specimen for histopathological examination.13
This brief case report shows that endoscopic full-thickness biopsy is feasible for obtaining a detailed morphological diagnosis of the ENS,1,2 and we conclude that this is a useful method in the work up of patients suffering from severe and complex gastrointestinal symptoms.
Acknowledgments
We want to thank the staff at the Department of Endoscopy and Cellular Pathology for technical support.
FS, HT, and ET designed the initial study with biopsy sampling. BO, RG, and BV designed the histopathological part of the study. HT performed the biopsy. BV performed the histopathological examination. BO wrote the initial draft of the paper. All authors contributed intellectually in the writing process and accepted the final version of the manuscript.
Footnotes
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Conflict of interest statement: The authors declare that there is no conflict of interest.
Contributor Information
Bodil Ohlsson, Department of Clinical Sciences, Lund University, Skåne University Hospital, Jan Waldenström Street 15, S-205 02 Malmö, Sweden.
Rita Gustafsson, Department of Gastroenterology, Skane University Hospital, Malmö, Sweden.
Fredrik Swahn, Department of Surgery, Lund University, Skane University Hospital, Lund, Sweden.
Ervin Toth, Department of Gastroenterology, Skane University Hospital, Malmö, Sweden.
Béla Veress, Department of Cellular Pathology, Unilabs AB, Skövde, Sweden.
Henrik Thorlacius, Department of Surgery, Lund University, Skane University Hospital, Malmö, Sweden.
References
- 1. Schmidt A, Meier B, Caca K. Endoscopic full-thickness resection: current status. World J Gastroenterol 2015; 21: 9273–9285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Amiot A, Lazals-Hatem D, Joly F, et al. The role of immunohistochemistry in chronic idiopathic intestinal pseudoobstruction (CIPO): a case-control study. Am J Surg Pathol 2009; 33: 749–758. [DOI] [PubMed] [Google Scholar]
- 3. Lacy BE, Mearin F, Chang L, et al. Bowel disorders. Gastroenterology 2016; 150: 1393–1407. [DOI] [PubMed] [Google Scholar]
- 4. Mak GZ, Lucchetti AR, Drossos T, et al. Pediatric chronic abdominal pain and median arcuate ligament syndrome: a review and psychosocial comparison. Pediatr Ann 2016; 45: e257–e264. [DOI] [PubMed] [Google Scholar]
- 5. Mak GZ, Speaker C, Anderson K, et al. Median arcuate ligament syndrome in the pediatric population. J Pediatr Surg 2013; 48: 2261–2270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Berritto D, Iacobellis F, Mazzei MA, et al. MDCT in ischaemic colitis: how to define the aetiology and acute, subacute and chronic phase of damage in the emergency setting. Br J Radiol 2016; 89: 20150821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Sand E, Themner-Persson A, Ekblad E. Infiltration of mast cells in rat colon is a consequence of ischemia/reperfusion. Dig Dis Sci 2008; 53: 3158–3169. [DOI] [PubMed] [Google Scholar]
- 8. Takada K, Yamashita K, Sakurai-Yamashita Y, et al. Participation of nitric oxide in the mucosal injury of rat intestine induced by ischemia-reperfusion. J Pharmacol Exp Ther 1998; 287: 403–407. [PubMed] [Google Scholar]
- 9. Xu X, Zhu Y, Chuai J. Changes in serum ghrelin and small intestinal motility in rats with ischemic stroke. Anat Rec (Hoboken) 2012; 295: 20–25. [DOI] [PubMed] [Google Scholar]
- 10. Cheng X, Boza-Serrano A, Turesson MF, et al. Galectin-3 causes enteric neuronal loss in mice after left sided permanent middle cerebral artery occlusion, a model of stroke. Sci Rep 2016; 6: 32893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Bowen JM, Gibson RJ, Cummins AG, et al. Intestinal mucositis: the role of the Bcl-2 family, p53 and caspases in chemotherapy-induced damage. Support Care Cancer 2006; 14: 713–731. [DOI] [PubMed] [Google Scholar]
- 12. Sand E, Roth B, Weström B, et al. Structural and functional consequences after buserelin-induced enteric neuropathy in rat. BMC Gastroenterol 2014; 14: 209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Rajan E, Gostout CJ, Wong Kee Song LM, et al. Innovative gastric endoscopic muscle biopsy to identify all cell types, including myenteric neurons and interstitial cells of Cajal in patients with idiopathic gastroparesis: a feasibility study (with video). Gastrointest Endosc 2016; 84: 512–517. [DOI] [PMC free article] [PubMed] [Google Scholar]


