Abstract
Background
The objective of this study is to evaluate the safety and quality of computed tomographic angiography of the thoracic aorta (CTA-TA) exams performed using intraosseous needle intravenous access (ION-IVA) for contrast media injection (CMI).
Methods
All CTA-TA exams at the study institution performed between 1/1/2013 and 8/14/2015 were reviewed retrospectively to identify those exams which had been performed using ION-IVA (ION-exams). ION-exams were then analyzed to determine aortic attenuation and contrast-to-noise ratio (CNR). Linear regression was used to determine how injection rate and other variables affected image quality for ION-exams. Patient electronic medical records were reviewed to identify any adverse events related to CTA-TA or ION-IVA.
Results
17 (~0.2%) of 7401 exams were ION-exams. ION-exam CMI rates varied between 2.5 and 4 ml/s. Mean attenuation was 312 HU (SD 88 HU) and mean CNR was 25 (SD 9.9). A strong positive linear association between attenuation and injection rate was found. No immediate or delayed complications related to the ION-exams, or intraosseous needle use in general, occurred.
Conclusion
For CTA-TA, ION-IVA appears to be a safe and effective route for CMI at rates up to 4 ml/s.
Keywords: Intraosseous needle, Computed tomography, Angiography, Thoracic aorta, Traumatic aortic injury, Emergency radiology, Injection, Contrast media
1. Introduction
The majority of victims of major trauma require computed tomographic angiography of the thoracic aorta (CTA-TA) as part of their imaging evaluation.1 CTA-TA requires intravenous access (IVA) for contrast media injection (CMI) at high flow rates.2 Peripheral IVA is favored for this purpose, but is not always achievable.2 In such circumstances, central lines can be used for CMI.2 In instances when central line placement is inexpedient or impossible, an alternative exists: intraosseous needle intravenous access (ION-IVA) (see Figs 1 and 2). ION-IVA placement is safer and faster than central line placement, with a failure rate of less than 1%.3
Fig. 1.
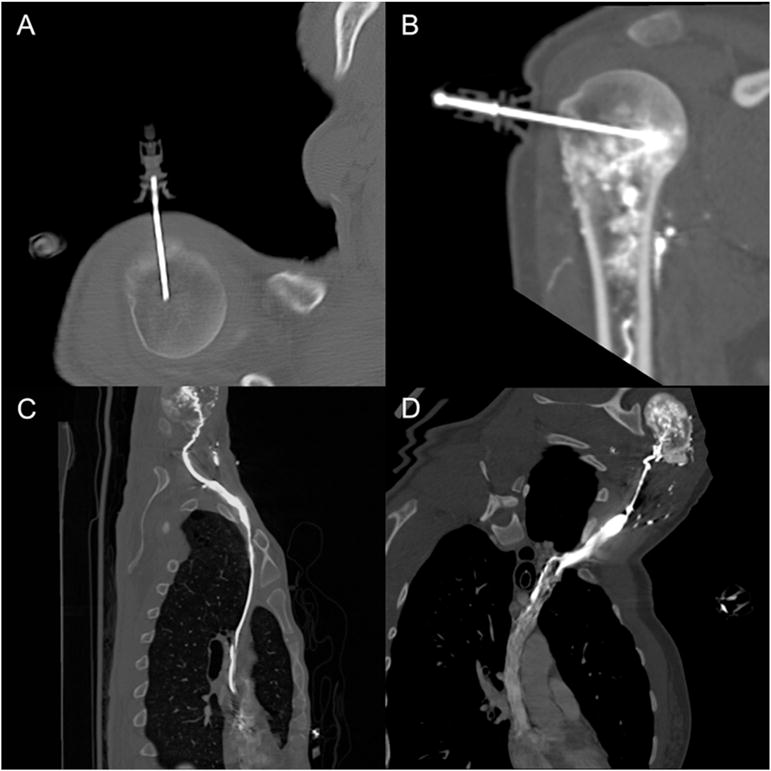
A) MPR image derived from a preliminary scan performed to check intraosseous needle position. B) Thin MIP image derived from a scan showing an intraosseous needle and contrast media within the intramedullary space. C) CPR image showing path of contrast media from right humerus to the right atrium. D) Path of contrast from the left humerus.
Fig. 2.
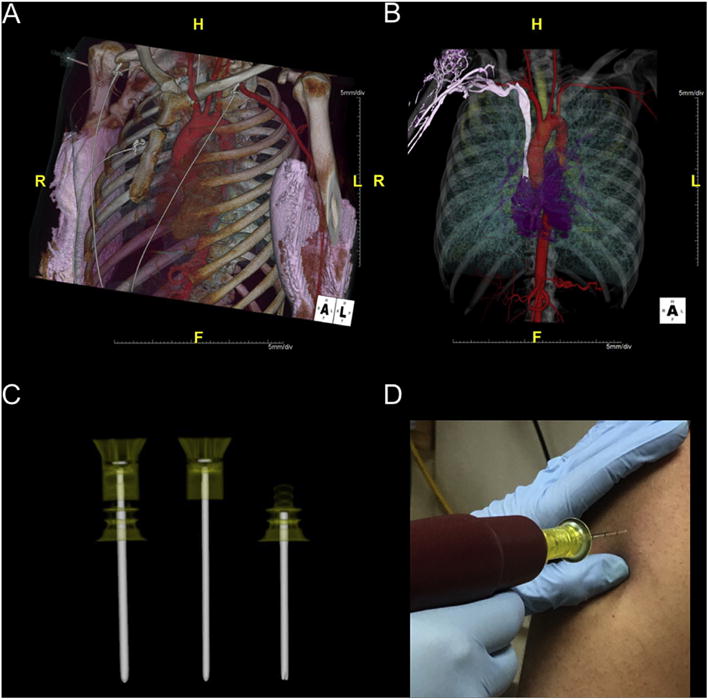
A) VR image of data from an ION-exam. Note that there is bilateral extravasation from two injection attempts via antecubital IVA. In this case, ION-IVA was used to salvage the study. B) VR image of data from a different ION-exam. Note that in this case the post contrast media saline flush was not adequate and there is residual contrast within the venous system. The image demonstrates the relationship of the intramedullary space to the veins of the upper extremity. C) Volume Rendering of data from a scan of two intraosseous needle sets, one with the trocar in place and the other with the trocar beside the needle. D) Intraosseous needle loaded on a needle driver and ready for insertion.
A recent clinical review by Baadh et al. calls for imaging physicians to familiarize themselves with the technique of using ION-IVA for CMI.4 There is a substantial body of mid twentieth century literature, predating the advent of computed tomography, reporting the safe use of ION-IVA for CMI during fluoroscopic venography studies.5 Fairly recent data on the safe use of ION-IVA for CMI from animal models has also been published.6,7 However, modern literature reporting the clinical use of ION-IVA for CTA-TA is sparse.4,8–10 The objective of this study was to retrospectively survey the safety of ION-IVA CMI performed during CTA-TA and to assess the quality of the resultant exams.
2. Materials and methods
7401 CTA-TA exams, performed between January 1, 2013 and August 14, 2015, were reviewed to create a CTA-TA database. Written informed consent was waived by the Institutional Review Board due to the retrospective nature of the project and because of the large number of exams included in the database. CTA-TA quality measurements were performed from survey series of 3.0 mm thick images. Attenuation and noise were measured within the ascending aorta and nearby adipose tissue using circular region-of-interests of approximately 100 mm.2 Contrast-to-noise ratio (CNR) for the aorta was derived using the method of Feuchtner et al.11 Other CTA-TA data collected included technical factors such as site of IVA, CMI rate, CMI dose, scanner type, and reconstruction method. Patient data, such as age, sex, weight, height, and chest width, was collected. The institutional adverse event reporting system was queried for all events related to CTA-TA. Complete chart review was performed for all patients who received CTA-TA exams utilizing ION-IVA.
Statistical analyses were performed using open source “R” statistical software version 3.1.1. Scatterplots and correlation coefficients were used to examine adequacy of a linear association between CNR and covariates of interest. The potential of multicollinearity was assessed with the Pearson correlation coefficient. Multiple linear regression models were fitted with two-way interactions. Backward elimination procedure, F-statistic, and adjusted R squared were used to select parsimonious models. Constant variance, normality, and independence were examined.
3. Results
17 (~0.2%) of 7401 of the exams performed during the study period utilized ION-IVA. All ION-exams were performed with EZ-IO needles (Teleflex Medical, Limerick, Pennsylvania, U.S.A.). CMI rates for ION-exams varied between 2.5 and 4.0 ml/s (mean of 3.4 ml/s). CMI dose varied between 80 and 100 ml (mean of 91 ml) of Iohexol 350. Mean attenuation for the ION-exams was 312 HU (SD 88 HU) and mean CNR was 25 (SD 9.9). Assessment of attenuation versus other covariates revealed a strong positive linear association between attenuation and CMI rate (R = 0.58, p-value = 0.014) and a strong negative association between attenuation and chest width (R = −0.53, p-value = 0.028). CNR also exhibited a strong negative linear association with chest width (R = −0.77, p-value<0.001). ION-exam and patient data is summarized in Table 1. Representative images from exemplary ION-exams are presented in Fig. 2 (and GIFs 1 and 2 online).
Table 1.
Data related to CTA-TA exams performed with ION-IVA.
| Case Number |
Injection Rate (cm/s) |
Contrast Media Dose (mL) |
ION site |
kVp | mAs | CTDIvol (mGy) |
DLP (mGy*cm) |
Scanner Model |
A AA (HU) |
N AA (HU) |
A F (HU) |
CNR AA | History | Age | Sex | Body Mass Index |
Chest Width (cm) |
Disposition |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2.5 | 100 | RH | 120 | 253 | 17 | 446 | S40 | 136 | 18 | −52 | 10 | assault | 23 | M | 26 | 42 | expired |
| 2 | 2.7 | 100 | RH | 120 | 279 | 23 | 492 | S40 | 233 | 16 | −112 | 22 | fall | 88 | F | 33 | 46 | rehab |
| 3 | 3 | 100 | RH | 120 | 202 | 17 | 461 | S40 | 250 | 21 | −113 | 17 | MVC | 48 | F | 29 | 42 | home |
| 4 | 3 | 100 | LT | 120 | 200 | 16 | 341 | S40 | 239 | 18 | −109 | 19 | MVC | 51 | F | 30 | 42 | expired |
| 5 | 3 | 100 | RH | 120 | 185 | 15 | 331 | S40 | 308 | 13 | −95 | 31 | assault | 23 | M | 18 | 33 | rehab |
| 6 | 3.5 | 80 | RH | 120 | 154 | 13 | 371 | S40 | 434 | 11 | −91 | 48 | EXP | 32 | M | 17 | 32 | rehab |
| 7 | 3.2 | 100 | LT | 100 | 130 | 5 | 145 | Edge | 254 | 12 | −83 | 28 | MVC | 27 | M | 20 | 32 | home |
| 8a | 3.5 | 100 | LH | 120 | 192 | 16 | 377 | S40 | 396 | 20 | −88 | 24 | GSW | 21 | M | 35 | expired | |
| 9 | 3.5 | 80 | LH | 120 | 206 | 17 | 292 | S40 | 299 | 21 | −103 | 19 | fall | 40 | F | 28 | 45 | home |
| 10 | 3.5 | 100 | LH | 120 | 149 | 12 | 345 | S40 | 407 | 14 | −100 | 36 | MVC | 26 | F | 23 | 29 | home |
| 11 | 3.5 | 80 | LH | 100 | 140 | 6 | 118 | Edge | 367 | 18 | −117 | 27 | fall | 47 | M | 23 | 31 | home |
| 12 | 3.5 | 80 | RH | 120 | 235 | 15 | 370 | Edge | 260 | 10 | −127 | 39 | MVC | 24 | M | 28 | 35 | home |
| 13 | 3.5 | 80 | RH | 120 | 197 | 16 | 357 | S40 | 235 | 37 | −107 | 9 | MVC | 34 | M | 27 | 47 | home |
| 14 | 4 | 80 | RH | 120 | 200 | 16 | 336 | S40 | 374 | 23 | −96 | 20 | MVC | 23 | F | 35 | 45 | home |
| 15 | 4 | 90 | LH | 120 | 192 | 16 | 396 | S40 | 456 | 18 | −91 | 30 | MVC | 27 | F | 26 | 37 | expired |
| 16 | 4 | 100 | RH | 120 | 204 | 17 | 395 | S40 | 272 | 20 | −108 | 19 | GSW | 62 | F | 29 | 46 | home |
| 17 | 4 | 80 | RH | 100 | 227 | 9 | 201 | Edge | 381 | 19 | −120 | 26 | GSW | 28 | M | 23 | 35 | home |
| mean | 3.41 | 91 | 116 | 197 | 14 | 339 | 311 | 18 | −101 | 25 | 37 | 26 | 38 | |||||
| SD | 0.46 | 9.9 | 7.9 | 39 | 4.4 | 102 | 88 | 6 | 17 | 10 | 18 | 5 | 6 |
Abbreviations: ION = intraosseous needle, CTDIvol = volume computed tomography dose index, DLP = dose length product, HU = Hounsfield units, S40 = Siemens Sensation 40 ERCT, Edge = Siemens Somatom Definition Edge, A = attenuation, AA = ascending aorta, N = noise, F = fat, RH = right humerus, LH = left humerus, LT = left tibia, MVC = motor vehicle collision, EXP = explosion, GSW = gunshot wound, M = male, F = female, CNR = contrast to noise ratio, rehab = rehabilitation facility, SD = standard deviation.
Height and weight data was not recorded for this patient. In all cases the contrast media, Iohexol 350, was injected at room temperature.
No extravasation events related to CMI via ION-IVA occurred. However, it is interesting to note that two patients received ION-IVA CMI after extravasations related to antecubital IVA (for example see Fig. 1a, GIF 2). A complete review of ION-exam patient records failed to reveal any evidence of ION-IVA related complication. Specifically, there were no reports of ION-IVA placement failure, functional failure, bone marrow aspiration difficulty, damage to the ION-IVA, aborted CTA-TA exam, extravasation, patient discomfort, fracture, infection, fat embolism, bone infarction, or manifestation of compartment syndrome.
4. Discussion
The use of ION-IVA for CTA-TA during the study period was rare, occurring in only 17 (0.2%) of the 7401 exams performed. (central lines, in contrast, were utilized in 125). This rarity may reflect trepidation of imaging personnel who were confused by or unfamiliar with ION-IVA. However, the study institution has developed a useful algorithm (Fig. 3) for using ION-IVA for CMI. As this and other algorithms4 are promulgated via the medical literature, training in the use ION-IVA for CTA-TA may become routine. Furthermore, it is promising that in this series no untoward event related to CMI via ION-IVA was observed. As this and similar evidence4,8–10 related to the safety of ION-IVA for CMI mounts, personnel may be less reluctant to use ION-IVA for this indication.
Fig. 3.
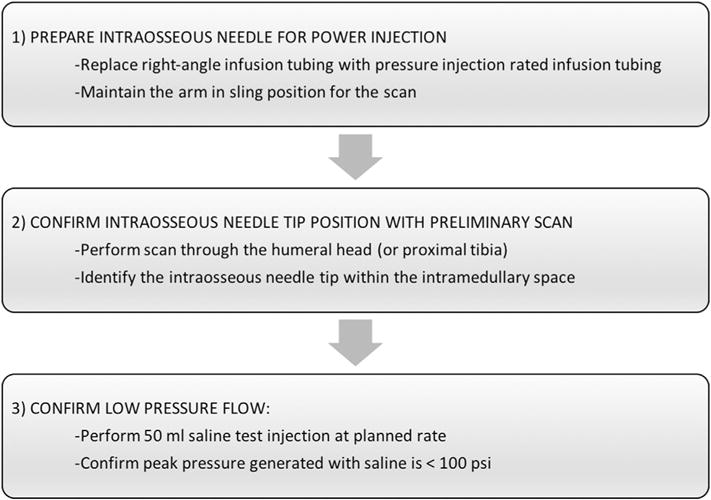
Algorithm to confirm suitability of ION-IVA for CM injection.
The mean aortic attenuation observed in the ION-exams was 312 HU, exceeding the mean attenuation of exams in the database performed with antecubital access, which was 271 HU. Due to the small sample size of ION-exams, this result should not be considered significant. The ION-exam data demonstrated statistically significant positive linear associations between aortic attenuation and CMI rate. The implication of this association is that, although the vascular anatomy of bone differs from that of superficial soft tissue, these differences do not limit flow, at least for rates less than 4.0 ml/s. Further study will be necessary to determine if this holds true for higher injection rates (e.g. the 5.0–6.0 ml/s rates recommended for cardiac CT).
Intramedullary bone is rich in pain receptors, and there is both the potential for, and anticipation of, pain during prolonged ION-IVA infusions.3,12 While it is interesting that during this review no reports of ION-IVA related pain were found, it is important to note that all of the patients studied were either experiencing pain associated this their traumatic injuries, the recipients of IV analgesia, or obtunded at the time of CTA-TA acquisition. Consequentially, pain from their ION-IVA infusions may have been masked or simply not recorded. Prophylactic analgesia is recommended when ION-IVA is used for large volume infusions.3
4.1. Limitations and bias
This study has notable limitations. It is a single institution observational study that yielded a very small sample size (N = 17). Patients with difficult AC-IVA often suffer from cardiovascular insufficiency, which may have introduced susceptibility bias. Technologist unfamiliarity with ION likely lead to selection bias and may explain the small sample size of this study.
5. Conclusion
The data presented herein suggests ION-IVA may be an acceptable alternative route for CMI for CTA-TA when peripheral IVA is unavailable or inexpedient. Prospective studies should be performed to validate this finding.
6. Summary
This study investigated the safety and quality of intraosseous needle intravenous access for contrast injection for Computed Tomographic Angiography of the Thoracic Aorta. A retrospective search of a quality and safety database found 17 studies performed in this manner. A control group, comprised of the studies in the database performed with antecubital intravenous access, was used for comparison. The quality metrics of the two groups were similar, with the intraosseous needle group being slightly better. A review of patient and complication records found no evidence of complications related to intraosseous needle use.
Supplementary Material
Acknowledgments
Role of funding sources
The work was supported by a grant from Teleflex Incorporated and by NIH grant 8UL1TR000117. Teleflex received a draft of the manuscript prior to submission but had no role in the study or editorial privilege.
Abbreviations
- CTA-TA
computed tomographic angiography of the thoracic aorta
- IVA
intravenous access
- CMI
contrast media injection
- P-IVA
peripheral intravenous access
- ION-IVA
intraosseous needle intravenous access
- ION-exams
examinations performed using ION-IVA
- CNR
contrast-to-noise ratio
Appendix A. Supplementary data
Supplementary data related to this article can be found at http://dx.doi.org/10.1016/j.jcct.2017.03.001.
Footnotes
Conflict of interest statement
We wish to confirm that there are no known conflicts of interest associated with this publication and there has been no significant financial support for this work that could have influenced its outcome.
References
- 1.Fox N, Schwartz D, Salazar JH, et al. Evaluation and management of blunt traumatic aortic injury: a practice management guideline from the eastern association for the surgery of trauma. J Trauma Acute Care Surg. 2015 Jan;78:136–146. doi: 10.1097/TA.0000000000000470. http://dx.doi.org/10.1097/TA.0000000000000470. [DOI] [PubMed] [Google Scholar]
- 2.Bae KT. Intravenous contrast medium administration and scan timing at CT: considerations and approaches. Radiology. 2010 Jul;256:32–61. doi: 10.1148/radiol.10090908. http://dx.doi.org/10.1148/radiol.10090908. [DOI] [PubMed] [Google Scholar]
- 3.Petitpas F, Guenezan J, Vendeuvre T, Scepi M, Oriot D, Mimoz O. Use of intra-osseous access in adults: a systematic review. Crit Care. 2016 Apr 14;20:102. doi: 10.1186/s13054-016-1277-6. http://dx.doi.org/10.1186/s13054-016-1277-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baadh AS, Singh A, Choi A, Baadh PK, Katz DS, Harcke HT. Intraosseous vascular access in radiology: review of clinical status. AJR Am J Roentgenol. 2016 May;10:W1–W7. doi: 10.2214/AJR.15.15784. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 5.Schobinger RA. Intra-osseous Venography. New York: Grune & Stratton; 1960. [Google Scholar]
- 6.Günal I, Köse N, Gürer D. Compartment syndrome after intraosseous infusion: an experimental study in dogs. J Pediatr Surg. 1996 Nov;31:1491–1493. doi: 10.1016/s0022-3468(96)90162-1. [DOI] [PubMed] [Google Scholar]
- 7.Cohen J, Duncan L, Triner W, Rea J, Siskin G, King C. Comparison of computed tomography image quality using intravenous vs. Intraosseous contrast administration in swine. J Emerg Med. 2015 Nov;49:771–777. doi: 10.1016/j.jemermed.2014.06.036. http://dx.doi.org/10.1016/j.jemermed.2014.06.036. [DOI] [PubMed] [Google Scholar]
- 8.Knuth TE, Paxton JH, Myers D. Intraosseous injection of iodinated computed tomography contrast agent in an adult blunt trauma patient. Ann Emerg Med. 2011 Apr;57:382–386. doi: 10.1016/j.annemergmed.2010.09.025. http://dx.doi.org/10.1016/j.annemergmed.2010.09.025. [DOI] [PubMed] [Google Scholar]
- 9.Ahrens KL, Reeder SB, Keevil JG, Tupesis JP. Successful computed tomography angiogram through tibial intraosseous access: a case report. J Emerg Med. 2013 Aug;45:182–185. doi: 10.1016/j.jemermed.2012.11.091. http://dx.doi.org/10.1016/j.jemermed.2012.11.091. [DOI] [PubMed] [Google Scholar]
- 10.Budach NM, Niehues SM. CT angiography of the chest and abdomen in an emergency patient via humeral intraosseous access. Emerg Radiol. 2016:1–4. doi: 10.1007/s10140-016-1438-6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 11.Feuchtner GM, Jodocy D, Klauser H, et al. Radiation dose reduction by using 100-kV tube voltage in cardiac 64-slice computed tomography: a comparative study. Eur J Radiol. 2010 Jul;75:e51–56. doi: 10.1016/j.ejrad.2009.07.012. http://dx.doi.org/10.1016/j.ejrad.2009.07.012. [DOI] [PubMed] [Google Scholar]
- 12.Mach DB, Rogers SD, Sabino MC, et al. Origins of skeletal pain: sensory and sympathetic innervation of the mouse femur. Neuroscience. 2002;113:155–166. doi: 10.1016/s0306-4522(02)00165-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


