Abstract
Background
Men who have sex with men (MSM) are at increased risk for HIV infection in India, particularly those who engage in transactional sex with other men (i.e., male sex workers; MSW). Despite the need, HIV prevention efforts for Indian MSW are lacking. As in other settings, MSW in India increasingly rely on the use of mobile phones for sex work solicitation. Integrating mobile phone technology into an HIV prevention intervention for Indian MSW may mitigate some of the challenges associated with face-to face approaches, such as implementation, lack of anonymity, and time consumption, while at the same time proving to be both feasible and useful.
Methods
This is a pilot randomized controlled trial to examine participant acceptability, feasibility of study procedures, and preliminary efficacy for reducing sexual risk for HIV. MSW (N = 100) were equally randomized to: (1) a behavioral HIV prevention intervention integrating in-person and mobile phone delivered HIV risk reduction counseling, and daily, personalized text or voice messages as motivating “cognitive restructuring” cues for reducing condomless anal sex (CAS); or (2) a standard of care (SOC) comparison condition. Both groups received HIV counseling and testing at baseline and 6-months, and completed ACASI-based, behavioral and psychosocial assessments at baseline, 3, and 6 months. Mixed-effects regression procedures specifying a Poisson distribution and log link with a random intercept and slope for month of follow-up was estimated to assess the intervention effect on the primary outcomes: 1) CAS acts with male clients who paid them for sex, and 2) non-paying sexual partners – both outcomes assessed over the past month.
Results
The intervention was both feasible (98% retention at 6-months) and acceptable (>96% of all interventions sessions attended); all intervention participants rated the intervention as “acceptable” or “very acceptable.” A reduction in the reported number of CAS acts with male clients who paid them for sex in the past month was seen in both study conditions. MSW in the intervention condition reported a faster rate of decline in the number of CAS acts with male clients in the past month from the baseline to both the 3-month (B=−1.20; 95% CI=−1.68, −0.73; p<0·0001) and 6-month (B=−2.44; 95% CI=−3.35, −1.53; p<0·00001) assessment visits compared to the SOC condition. Post-hoc contrasts indicated that, at 3 months, participants in the intervention condition reported 1.43 (SD=0.29) CAS acts with male clients in the past month compared to 4.85 (SD=0.87) in the control condition (p=0.0003). Furthermore, at 6 months, the intervention condition participants reported 0.24 (SD=0.09) CAS acts with male clients in the past month compared to 2.79 (SD=0.79) in the control condition (p<0·0001).
Conclusions
Findings are encouraging and provide evidence of feasibility and acceptability, and demonstrate initial efficacy (for reducing sexual risk for HIV) of a behavioral HIV prevention intervention for Indian MSW that combines daily, personalized text or voice messages with mobile phone-delivered sexual risk reduction counseling and skills building. Future testing of the intervention in a fully powered randomized controlled efficacy trial is warranted.
Keywords: HIV, Male Sex Workers (MSW), India, HIV Prevention, Behavioral Intervention
Introduction
Men who have sex with men (MSM) are at increased risk for HIV in India, with a prevalence rate over 18 times higher than in the general population.1 Moreover, a large but hidden population of MSM engage in transactional sex (i.e., male sex workers; MSWs), putting them at further risk for HIV.2 While no population-level HIV prevalence data has been published about Indian MSW, convenience samples in large metropolitan cities have reported two-fold higher rates of HIV in MSW compared to MSM who do not engage in sex work.3,4,5 Similarly, surveys have found higher rates of sexual risk behaviors and inconsistent condom use with both transactional and non-transactional sex partners among MSW compared to MSM who do not engage in transactional sex.3,4,6
MSW in India, where the illegality of same-sex intercourse has been upheld by the Supreme Court, face multilevel and complex risk factors for HIV including social stigma, discrimination and criminalization – by defying norms of both sexual behavior and employment.7 This stigma, discrimination and potential for criminalization further marginalize Indian MSW, and, as a result, reduce their access to HIV treatment and prevention services and increase HIV transmission and acquisition risks.7 HIV prevention efforts in India have focused on traditional risk groups including MSM who don’t engage in sex work, female sex workers and their clients, and injection drug users; however, specific interventions for Indian MSW are lacking and much needed.8
Advances in mobile phone technologies in India has made sex work increasingly dispersed.9, 10 Moreover, given that traditional in-person interventions may present important challenges to Indian MSW, including transportation costs, scheduling difficulties and lack of anonymity, using mobile phones as part of an HIV prevention strategy may prove effective for general prevention efforts, but may be most useful for Indian MSW in particular. As evidenced by the effectiveness of mobile phone interventions in other contexts such as in promoting medication adherence, mobile phone counseling as a psychosocial intervention or sending tailored text messages to mobile phones may prove effective in reducing risk behaviors (e.g., condomless anal sex) and increasing protective behaviors (e g., HIV/STI testing) and by acting as reminders of intervention content.11
The current study is part of a program of research to fully develop and test a culturally relevant, theory-based HIV risk reduction intervention using mobile phone technology for MSW in Chennai, India. The intervention was informed by in-depth qualitative feedback from MSW and key informants (KI) from the MSM community in Chennai. Guided by empowerment theory and using motivational interviewing techniques, the intervention was designed to facilitate personal strategies and problem solving skills for sexual risk reduction.12,13 We conducted an open pilot trial of the intervention to determine the feasibility of study procedures and participant acceptability. A major goal of this study was to further assess feasibility and acceptability and to assess preliminary efficacy for reducing condomless anal sex (CAS) acts among MSW in this setting. We hypothesized that MSW who were assigned to the intervention condition would reduce HIV risk behavior in greater magnitude compared to MSW assigned to standard of care (SOC) alone. The current paper describes the outcome data from an initial pilot randomized controlled trial. The study’s premise was that if the intervention shows promise, future testing in a fully powered efficacy trial over a longer follow-up period to fully assess sustained effects, as well as a trial examining the cost-effectiveness of the integrated in-person counseling and mobile phone delivered intervention compared to face-to-face or a time-matched control group would be justified.
Methods
Participants and Procedures
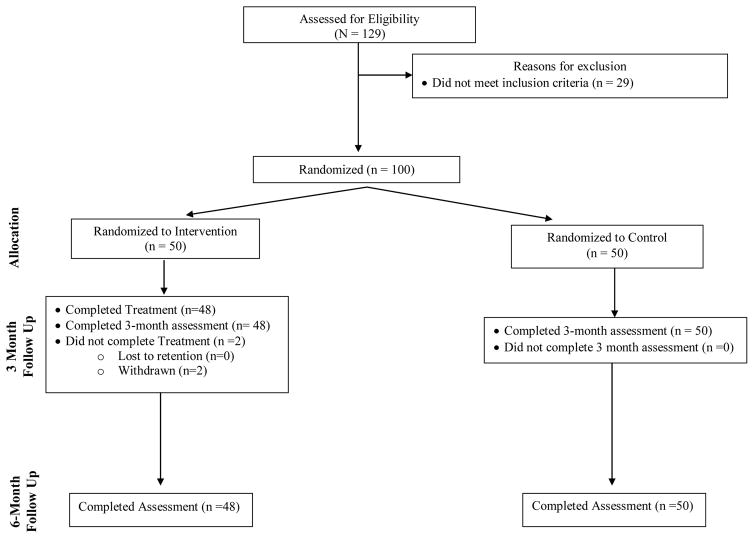
This was a two-arm, pilot randomized controlled trial with 1:1 allocation ratio. A total of 129 individuals were screened for study eligibility; 29 of these men were not eligible because they did not meet inclusion criteria. The remaining 100 were eligible based on inclusion criteria and all consented to enroll; they were randomly assigned to the experimental condition (n=50) or to the SOC comparison condition (n=50) (both described below) using a computerized randomization program. The study interviewer was blinded to the assigned study condition for all participants.
Figure 1 depicts participant flow throughout the study from screening to follow-up. Inclusion criteria included being 18 years or older, identifying as male, and having engaged in anal sex (insertive or receptive) with another man in exchange (i.e., someone gave them) for money, goods, favors or gifts, as a way to generate income in the 3 months prior to screening. Individuals were excluded if they were unwilling to complete the written informed consent procedures, had participated in an HIV prevention intervention in the past year or identified as a hijra/transgender. Transgender individuals were not included in the current study, as it was determined in prior formative work that different intervention topics would be necessary for varied gender minority populations. All study visits were conducted at the National Institute for Research on Tuberculosis (NIRT) in Chennai, India. All study procedures were approved by the Institutional Review Boards and Ethics Committees at NIRT/Indian Council for Medical Research (ICMR), Chennai, India and The Fenway Institute, Fenway Health, Boston, MA.
Figure 1.
CONSORT Diagram
HIV Counseling and Testing (Standard of Care Condition)
Participants in both study conditions received HIV testing and counseling at baseline and at the 6-month follow-up study visit. HIV testing was conducted using Retroquic HIV Rapid card tests (Qualpro diagnostics, Goa, India). All reactive samples were tested by HIV Tri dot kit (J. Mitra & Co. New Delhi, India) for confirmation.
Experimental Intervention
The content, format, and structure of the intervention was informed by formative qualitative research.13 Data collected during this formative phase included individual in-depth interviews with MSW and key informants from the MSM and MSW communities in Chennai as well as feedback from a peer community advisory board on the usability of the proposed technology components, which were reported as easy to use. After the intervention manual was developed, it was tested in an open pilot trial with eight MSW. The experience of implementation, along with feedback garnered through exit interviews conducted with the participants, provided an opportunity for further refinement of the content, structure, and format of the intervention, which was now ready to be.
In addition to HIV counseling and testing as described above, the intervention integrated two in-person and four mobile phone sessions with a trained, Masters-level (e.g., social work, psychology) counselor. The two in-person sessions took place in weeks one and three, and were between 30 to 60 minutes each in duration. Two of the four mobile phone sessions occurred in weeks two and four and lasted ~15 to 20 minutes each. Two (~15 to 20 minutes each) “booster” mobile phone sessions were added in weeks 8 and 12 in order to reinforce and “check in” on the participants’ integration of risk reduction skills learned during their initial sessions. The in-person sessions were designed to cover new material and facilitate in-depth discussions while the mobile phone sessions were shorter and emphasized review of participants’ action plan for reducing sexual risk that was developed during their in-person session during the prior week.
The intervention also included a mobile messaging component. During the first in-person session, each participant randomized to the intervention arm was asked to choose seven brief text or voice messages from a list of sixteen, intended to remind them about their personal goals for sexual safety and dispute maladaptive thoughts as potential barriers to HIV risk reduction. For a 12-week period (post-randomization), daily messages were sent through an automated system to participants’ mobile phones during a time they previously reported as a “period of possible higher risk” with male sex work clients. Participants had the option of receiving Tamil-script text messages or pre-recorded voice messages in Tamil.
Throughout the first in-person session, the counselor and participant discussed how to use condoms and lubricants, problems with condoms, alternative sexual activities and communicating with clients about condoms and sexual limits. Additionally, during this session they practiced how to negotiate condom use with their clients, even in the event should additional money be offered. At the end of this session, the participant developed an action plan, which detailed the steps that they would take to improve communication and condom negotiation with their sex work clients. During the second in-person session, the counselor and participant discussed reasons for and experiences with sex work and a review of HIV and STD transmission behaviors and ways to mitigate risk. Also discussed was the concept of “triggers” of CAS—including the environment/setting where sex work is done, type of clients, alcohol use, depressed mood, both sexual minority and sex work stigma, and self-esteem—and practiced strategies for managing these triggers. At the end of this session, the participant developed an action plan for managing their potential triggers for risky sex.
In the week following each in-person session, the mobile phone sessions were conducted and used to review the action plans, discuss challenges that participants had implementing their plans, put a back-up plan in place, and role-play potential scenarios and solutions.
Study Assessments
Participants completed three study assessment visits: 1) baseline (pre-randomization), 2) post-intervention which was when the final components of the intervention were complete for those who were assigned to the experimental condition (approximately 3 months after randomization for both study conditions), and 3) 6-month follow-up. Questions regarding sexual behavior with paying and non-paying partners, including our primary outcome of CAS acts with clients in the past month, were assessed using audio-computer assisted self-interview (A-CASI) in order to reduce social desirability bias from interviewer administered assessments.14, 15 Demographic and psychosocial characteristics were interviewer-administered.
Demographic and Psychosocial Characteristics
During their baseline visit, participants’ age, education attainment, sexual orientation, relationship status, religion, alcohol use, and HIV status was assessed.
Primary Outcome
CAS Acts, a surrogate endpoint for HIV acquisition and transmission. Participants were asked about the number of times that they had anal sex without a condom with male clients and, separately, with non-paying male partners, in the past month. Consideration was given to assessing sex with men of a different HIV status, but our prior formative work and evidence in the literature suggests that sex workers rarely know the status of their clients, and therefore are unlikely to be able to report it accurately. Because this was a pilot trial, it was not powered to examine incident HIV and STIs as an outcome. The ultimate efficacy trial will be powered to examine difference in incident HIV/STIs between the study conditions.
Measures of Feasibility and Acceptability
Feasibility of study procedures and participant acceptability of the intervention were assessed by examining attrition for the follow-up study assessments visits, and, among those who were assigned to the intervention condition, attendance at the individual and mobile phone sessions were examined. Intervention participants were also asked to rate their level of acceptability of the intervention on a 4-point scale (not acceptable, less acceptable, acceptable, and very acceptable).
Sample Size Calculation
As this was a pilot randomized controlled trial, the primary reason for conducting the study is to assess participant acceptability and feasibility of all study procedures; we were also interested in examining preliminary efficacy. The primary outcome for this study was number of CAS acts across the two study conditions. Analyses were conducted to assess the potential impact of the intervention by comparing the average number of CAS acts in the previous 3 months. A sample size was determined using the data from a study of MSW in India, in which more than half (53%) used condoms only “sometimes or never”, with a mean number of 21 (SD=24) transactional male sex partners in the past 3 months in which condoms were “never” used. Assuming a 30% or greater decline in the experimental condition, with 80 participant completers (50 enrolled per study condition to account for attrition), there would be an 80% chance of detecting a significant difference at a two-sided, .05 alpha level.
Statistical Methods
All analyses conducted were determined a priori. Means for continuous variables and frequencies for categorical variables were calculated to describe sociodemographic characteristics of the participants at baseline for the overall sample and stratified by randomization condition. T and chi-square tests were used to examine differences by study condition and assess balance of randomization on key variables.
Intent-to-Treat Analyses
We assessed the impact of the intervention on changes in number of distinct CAS acts with male clients and with non-paying male partners in the past month over the course of the 6-month follow-up period. Because number of CAS acts is count data and was not normally distributed, we estimated mean counts to examine differences by intervention condition using mixed-effects models, specifying a Poisson distribution and log link with a random intercept and slope for month of follow up (baseline, 3 or 6 months). Additionally, in post-hoc analyses, we used contrasts to examine differences in the change in mean CAS acts with male clients and male non-paying partners at each time point (baseline, 3 months and 6 months) separately. All analyses were conducted in SAS (version 9.4) and were intent to treat.
Results
Baseline Characteristics
One hundred men who have sex with men in exchange (i.e., being given) for money, goods or other items of value were enrolled and randomized. Socio-demographic characteristics of the sample are summarized in Table I. The mean age was 27.7 years (SD=9·1). The majority (77.0%) identified as kothi (an effeminate man who takes on a female gender role in same sex relationships, often with a desire to be the penetrated member in sexual intercourse), and 42% were single and 38% had a primary boyfriend/male partner. Eight-five percent were Hindu. While most (50%) completed secondary education or less, a large minority (31%) completed undergraduate college. Most participants (59%) had another source of personal income outside of sex work. Almost half (49%) reported alcohol use in the context of sex work. Only 3 participants were HIV-infected at baseline. These socio-demographic characteristics did not differ by the two study conditions, suggesting a balance due to randomization.
Table I.
Baseline characteristics and psychosocial factors of participants (N=100)
| Overall | Intervention | Control | p-value | |
|---|---|---|---|---|
| Mean (SD) | ||||
|
|
||||
| Age | 27.7 (9.1) | 27.1 (7.3) | 28.2 (10.6) | 0.577 |
| Number of CAS acts, past month | 12.2 (17.7) | 10.7 (10.5) | 13.7 (22.7) | 0.406 |
| N (%) | ||||
|
|
||||
| Sexual Orientation | 0.564 | |||
| Panthi | 2 (2.0) | 1 (2.0) | 1 (2.0) | |
| Kothi | 77 (77.0) | 41 (82.0) | 36 (72.0) | |
| Double-decker | 21 (21.0) | 8 (16.0) | 13 (26.0) | |
| Relationship Status | 0.741 | |||
| Wife/Female partner/girlfriend | 4 (4.0) | 3 (6.0) | 1 (2.0) | |
| Male partner/boyfriend (not married) | 38 (38.0) | 19 (38.0) | 19 (38.0) | |
| Other | 16 (16.0) | 7 (14.0) | 9 (18.0) | |
| Single | 42 (42.0) | 21 (42.0) | 21 (42.0) | |
| Religion | 0.511 | |||
| Hindu | 85 (85.0) | 40 (80.0) | 45 (90.0) | |
| Muslim | 5 (5.0) | 3 (6.0) | 2 (4.0) | |
| Christian | 9 (9.0) | 6 (12.0) | 3 (6.0) | |
| Other | 1 (1.0) | 1 (2.0) | 0 (0.0) | |
| Education Completed | 0.555 | |||
| Secondary or less | 50 (50.0) | 27 (54.0) | 23 (46.0) | |
| Higher secondary | 19 (19.0) | 10 (20.0) | 9 (18.0) | |
| Undergraduate college or more | 31 (31.0) | 13 (26.0) | 18 (36.0) | |
| Other Source of Personal Income (besides sex work) | 0.309 | |||
| Yes | 59 (59.0) | 27 (54.0) | 32 (64.0) | |
| No | 41 (41.0) | 23 (46.0) | 18 (36.0) | |
| Alcohol use, last 3 months | 0.345 | |||
| Never | 51 (51.0) | 26 (52.0) | 25 (50.0) | |
| Monthly or less | 15 (15.0) | 10 (20.0) | 5 (10.0) | |
| 2 to 4 times a month | 22 (22.0) | 8 (16.0) | 14 (28.0) | |
| More than weekly | 12 (12.0) | 6 (12.0) | 6 (12.0) | |
| HIV infected | 0.560 | |||
| Yes | 3 (3.0) | 2 (4.0) | 1 (2.0) | |
| No | 97 (97.0) | 48 (96.0) | 49 (98.0) | |
Feasibility and Acceptability
As depicted in Table II, of the 100 individuals who were enrolled and provided informed consent to participate, 98 completed 3-month and 6-month follow up assessments, and 98 completed HIV testing and counseling at their 6-month follow-up visit. One participant moved out of the area and one participant was in a serious non-study related accident that changed his availability to participate. Of the 50 participants randomized to the intervention condition, 50 completed their in-person session 1 visit, and 48 (96%) completed all of the remaining in-person visits and four mobile phone delivered counseling sessions. Lastly, all participants who were assigned to the experimental intervention found it to be “acceptable” or “highly acceptable.”
Table 2.
Retention of Participants for Assessments (N=100) and for Intervention Sessions (N=50)
| Behavioral Assessment | HIV testing | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Total | Intervention | Control | Total | Intervention | Control | |
| Baseline | 100 | 50 | 50 | 100 | 50 | 50 |
| 3-Month Follow Up | 98 | 48 | 50 | -- | ||
| 6-Month Follow Up | 98 | 48 | 50 | 98 | 48 | 50 |
|
| ||||||
| In Person Session | Mobile Phone Session | |||||
|
| ||||||
| Session 1 | 50 | 48 | ||||
| Session 2 | 48 | 48 | ||||
| Session 3 (Booster) | -- | 48 | ||||
| Session 4 (Booster) | -- | 48 | ||||
Primary Outcomes
Change in Condomless Anal Sex (CAS) With Male Clients
A reduction in reported number of CAS acts with male clients who paid them for sex in the past month was seen in both study conditions. As evidenced by the significant condition by time interactions in Table III, MSW in the intervention condition reported a faster rate of decline in the number of CAS acts with male clients in the past month from the baseline to both the 3-month (B=−1.20; 95% CI=−1.68, −0.73; p<0·0001) and 6-month (B=−2.44; 95% CI=−3.35, −1.53; p<0·00001) assessment visits compared to the SOC condition.
Table III.
Effect of intervention on number of condomless anal sex acts with male clients and non-paying male partners, past month, mixed effects Poisson regression (N=100)
| CAS with male clients | CAS with non-paying male partners | |||||
|---|---|---|---|---|---|---|
| Estimate* | 95% CI | p-value | Estimate* | 95% CI | p-value | |
|
| ||||||
| Intercept | 2.05 | 1.76, 2.35 | <0.0001 | 0.82 | 0.44, 1.21 | <0.0001 |
| Condition | ||||||
| Intervention | −0.02 | −0.43, 0.40 | 0.939 | −0.29 | −0.85, 0.26 | 0.304 |
| Control | 0 | -- | -- | 0 | -- | -- |
| Time | ||||||
| Baseline | 0 | -- | -- | 0 | -- | -- |
| 3 month | −0.47 | −0.78, −0.17 | 0.003 | −0.76 | −1, −0.52 | <0.0001 |
| 6 month | −1.03 | −1.59, −0.46 | 0.0006 | −1.58 | −1.9, −1.25 | <0.0001 |
| Condition * Time | ||||||
| Intervention* Baseline | 0 | -- | -- | 0 | -- | -- |
| Intervention*3 month | −1.20 | −1.68, −0.73 | <0.0001 | −0.35 | −0.75, 0.05 | 0.092 |
| Intervention*6 month | −2.44 | −3.35, −1.53 | <0.0001 | −0.96 | −1.63, −0.29 | 0.006 |
| Control* Baseline | 0 | -- | -- | 0 | -- | -- |
| Control*3 month | 0 | -- | -- | 0 | -- | -- |
| Control*6 month | 0 | -- | -- | 0 | -- | -- |
Estimate=log(IRR)
At baseline, the number of CAS acts with male clients in the past month did not differ by study condition (7.7 vs. 7.8 for the intervention vs. control conditions, respectively; p=1.0), which provides evidence that randomization was successful at balancing the two study conditions. Notably, at 3 months, participants in the intervention condition reported 1.43 (SD=0.29) CAS acts with male clients in the past month compared to 4.85 (SD=0.87) in the control condition (p=0·0003). At 6 months, the intervention condition participants reported 0.24 (SD=0.09) CAS acts with male clients in the past month compared to 2.79 (SD=0.79) in the control condition (p<0·0001) (Table IV).
Table IV.
Adjusted Mean (SE) Baseline and Follow-up Number of Condomless Anal Sex Acts with Male Clients and Non-Paying Male Partners, Past Month* by Study Condition.
| CAS with Male Clients | CAS with Non-Paying Male Partners | |||||
|---|---|---|---|---|---|---|
| Baseline | Month 3 | Month 6 | Baseline | Month 3 | Month 6 | |
|
| ||||||
| Intervention | 7.67 (1.15) | 1.43 (0.29) | 0.24 (0.09) | 1.70 (0.35) | 0.56 (0.13) | 0.13 (0.05) |
| Control | 7.79 (1.17) | 4.85 (0.87) | 2.79 (0.79) | 2.27 (0.45) | 1.06 (0.22) | 0.47 (0.11) |
| p-value | 1.000 | 0.0003 | <0.0001 | 0.304 | 0.045 | 0.003 |
Number of CAS acts (and standard errors) are estimated through Poisson regression and adjusted through the use of mixed effects analyses.
Change in Condomless Anal Sex (CAS) with Male Non-Paying Partners
Similarly, a reduction in reported the number of CAS acts with male non-paying partners in the past month was seen in both the intervention and control groups. Notably however, participants in the intervention condition reported a faster rate of decline in the number of CAS acts with male non-paying partners in the past month from baseline to 3-month (B=−0.35; 95% CI=−0.75, 0.05; p=0·092) and from baseline to 6-month (B=−0.96; 95% CI=−1.63, −0.29; p=0.006) follow-up assessments (Table III).
Specifically, at baseline, the number of CAS acts with male non-paying partners in the past month did not differ by condition (1·70 (SD=0.35) vs. 2·27 (SD=0.45) for the intervention condition vs. the control condition, respectively; p=0·304). By 3-months, participants in the intervention condition reported 0·56 (SD=0.13) CAS acts with male non-paying partners in the past month compared to 1·06 (SD=0.22) in the control condition (p=0·045). At 6 months, participants in the intervention condition reported 0·13 (SD=0.05) CAS acts with male non-paying partners in the past month compared to 0·47 (SD=0.11) in the control condition (p=0·003) (Table IV).
Discussion
The findings from this study provide preliminary evidence that a culturally-tailored, integrated in-person and mobile phone delivered counseling intervention has the ability to reach the desired population and can more effectively reduce HIV risk behaviors than SOC efforts (i.e., in-person HIV testing and counseling) alone. While HIV prevention programs in India exist, among MSM they are generally limited to condom distribution and educational outreach and are not contextually tailored to meet the specific needs of each subpopulation. This study was limited to being an initial pilot randomized controlled trial of a culturally-tailored intervention to reduce HIV and STI risk in MSW in India, with the goal of promoting sexual health in this population. However, these findings provide a background for a larger randomized controlled efficacy trial with longer follow-up to examine sustained intervention effects, which will have wider implications.
Furthermore, this paper documents the feasibility of delivery and participant acceptability of a behavioral HIV prevention intervention integrating in-person and mobile phone delivered HIV risk reduction counseling, and daily, personalized text or voice messages as motivating “cognitive restructuring” cues for reducing CAS acts among MSW in India. Given the vulnerable nature of MSW in India as an invisible and underserved population and the fact that our formative work revealed that MSWs are connected via their mobile phones13, HIV prevention efforts must use innovative methods to access even the most difficult-to-reach groups.
The importance of reducing sexual risk among MSW is further emphasized as a result of the multiple roles of MSM in India. The constitutional illegality of same-sex intercourse, coupled with social stigma and discrimination, increases the pressure for MSM in India to marry women and have children. These men, at elevated risk for HIV infection, may serve as a bridge between heterosexual and homosexual populations or sex work clients and non-paying sexual partners in India. In prior studies from our group and others evaluating more than 3,000 men attending STI clinics in Mumbai, we found that 25% reported prior sex with other men and all also had sex with women, and HIV prevalence among MSM married to women was comparably high as unmarried MSM.5 Other studies in Chennai have found that 2% to 15% of non-gay identified men reported male-male sexual behaviors.16–19 Further research is warranted to understand the importance and multiple roles of MSM who engage in sex work as a potential “bridge population” in which tailored HIV prevention efforts are indicated.
This intervention was developed to be responsive to the changing profile of sex work in India, capitalizing on the widespread use of mobile phones by sex workers in this setting. Sex work has changed in light of expanded mobile phone capabilities, becoming more dispersed and spatially mobile in many developing countries, as opposed to being predominantly clustered in neighborhoods, streets, or brothels.10 The strength of this intervention program is heightened by using a community based approach where the MSW were an integral part of developing the intervention curriculum. This included the format with regard to the type of interventions (e.g., SMS texts, voicemail recording), the structure (formative data revealed a strong desire to have a mix of both in-person and mobile phone delivered counseling sessions), the language used for the text and voice messages which were MSW friendly and in “tanglish” (a combination of Tamil and English) and the content of the messages, for example, “Don’t forget to use chocolate” (colloquially “chocolate” means condoms). This helped maintain confidentiality in the messages received as it was a language only they understood.
This study is the first we are aware of that utilizes mobile phone technologies in the context of sexual health and HIV prevention among this risk group. The intervention was designed to be tested as an “intervention package,” examining the combined impact of the in-person and mobile phone delivered counseling on reductions in CAS. Even though the risk reduction skills learned, the individualized topics discussed, the plan for risk reduction finalized, et cetera, during the 2 in-person counseling sessions were woven back into the mobile phone delivered counseling sessions, there is the possibility that either one of these approaches alone could derive the same benefits yielded from the combination of the two tested in this study. Notably, the sexual risk analysis that included all three time points showed significant differences with respect to the intervention versus the control group in changes in the reported number of CAS acts with paying male clients in the past month. We provide further evidence that our intervention is feasible to deliver, highly acceptable to participants, and promisingly effective with respect to reducing HIV and STI transmission and acquisition among this population. Because pilot trials are notorious for producing unreliable effect size estimates20–27, a larger, fully powered study testing intervention efficacy over a longer follow-up period to fully assess sustained effects is justified. Our approach to intervention development and testing was sequential, with the intention to tailor this intervention to the experiences and context of sex work among MSM in Chennai. Because of this, the intervention, if expanded for use with other populations at high risk for HIV and STIs, should be adapted to the specific needs of the population being reached.
Conclusions
The results from this study provide initial evidence that this intervention is effective in reducing sexual risk when compared to a standard of care comparison condition. Efficacy testing of this intervention in the context of a longer follow-up period is needed to have a more accurate estimate of the intervention effect overtime. From there, if successful, the potential expansion of this intervention as an alternative to standard of care HIV counseling and testing alone for high risk populations like Indian MSW would be recommended. The population of MSW in India face social and economic marginalization, and engage in sexual behaviors that may exacerbate HIV acquisition and transmission. Despite this, HIV prevention efforts for Indian MSW are lacking. Innovative and culturally and contextually informed approaches to addressing sexual risk among this group are urgently needed to curb HIV spread in India.
Acknowledgments
Funding: The current project was supported by the Indo-U.S. Joint Working Group on Prevention of Sexually Transmitted Diseases and HIV/AIDS through U.S. National Institute of Drug Abuse grant #R21DA033720 (Matthew Mimiaga, PI) and Indian Council of Medical Research grant #Indo-U.S/72/9/2010-ECDII (Beena Thomas, PI).
Footnotes
Compliance with Ethical Standards
Conflict of Interest: Authors MJM, BT, KB, BEJ, SS, PN, SB, AD, EFC, SM, CO, KHM, and SAS each declares that he/she has no conflict of interest.
Ethical approval: All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional review boards of The Fenway Institute, Boston, MA and the National Institute for Research in Tuberculosis, Chennai, India, and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent: Informed consent was obtained from all individual participants included in the study.
References
- 1.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for HIV infection among men who have sex with men in low-and middle-income countries 2000–2006: A systematic review. PLoS Med. 2007;4(12):339. doi: 10.1371/journal.pmed.0040339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Department of AIDS Control - Ministry of Health & Family Welfare. Annual Report 2012–2013. India: Department of AIDS Control - National AIDS Control Organization; 2012. [Google Scholar]
- 3.Mimiaga MJ. Differential HIV transmission risk behaviors among MSM subgroups engaging in transactional sex in Chennai, India. Presentation presented at; 2010; International AIDS Society Meeting; Vienna, Austria. [Google Scholar]
- 4.Shinde S, Setia MS, Row-Kavi A, Anand V, Jerajani H. Male sex workers: Are we ignoring a risk group in Mumbai, India? Indian Journal of Dermatology, Venereology, and Leprology. 2009;75(1):41–6. doi: 10.4103/0378-6323.45219. [DOI] [PubMed] [Google Scholar]
- 5.Kumta S, Lurie M, Weitzen S, et al. Bisexuality, sexual risk taking, and HIV prevalence among men who have sex with men accessing voluntary counseling and testing services in Mumbai, India. Journal of Acquired Immune Deficiency Syndromes (1999) 2010;53(2):227–33. doi: 10.1097/QAI.0b013e3181c354d8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Newman PA, Chakrapani V, Cook C, Shunmugam M, Kakinami L. Correlates of paid sex among men who have sex with men in Chennai, India. Sexually Transmitted Infections. 2008;84(6):434–8. doi: 10.1136/sti.2008.031484. [DOI] [PubMed] [Google Scholar]
- 7.Bharat S, Aggleton P, Tyrer P. India: HIV and AIDS-related discrimination stigmatization and denial. UNAIDS; Geneva, Switzerland: 2001. [Google Scholar]
- 8.Avahan: India AIDS Initiative: The Business of HIV Prevention at Scale. New Delhi, India: Bill & Melinda Gates Foundation; 2008. [Google Scholar]
- 9.Aral SO, St Lawrence J, Uusküla A. Sex work in Tallinn, Estonia: The sociospatial penetration of sex work into society. Sexually Transmitted Infections. 2006;82(5):348–53. doi: 10.1136/sti.2006.020677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahapatra B, Saggurti N, Halli SS, Jain AK. HIV risk behaviors among female sex workers using cell phone for client solicitation in India. Journal of AIDS & Clinical Research. 2012;1:176. [Google Scholar]
- 11.Fjeldsoe BS, Marshall AL, Miller YD. Behavior change interventions delivered by mobile telephone short-message service. American journal of Preventive Medicine. 2009;36(2):165–73. doi: 10.1016/j.amepre.2008.09.040. [DOI] [PubMed] [Google Scholar]
- 12.Biello KB, Thomas BE, Johnson BE, et al. Transactional sex and the challenges to safer sexual behaviors: A study among male sex workers in Chennai, India. AIDS care. 2016;9:1–8. doi: 10.1080/09540121.2016.1204421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thomas B, Closson EF, Biello K, et al. Development and open pilot trial of an HIV-prevention intervention integrating mobile-phone technology for male sex workers in Chennai, India. Archives of Sexual Behavior. 2015;29:1–2. doi: 10.1007/s10508-015-0665-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tourangeau R, Smith TW. Computer Assisted Survey Information Collection. John Wiley & Sons, Inc; 1998. Collecting sensitive information with different modes of data collection; pp. 431–454. [Google Scholar]
- 15.Moum T. Mode of administration and interviewer effects in self-reported symptoms of anxiety and depression. Social Indicators Research. 1998;45(1–3):279–318. [Google Scholar]
- 16.Hernandez AL, et al. The Prevalence of Sexual Behaviors with Other Men Among Men who Attend Sexually Transmitted Infection Clinics in Mumbai, India. Presentation presented at; 2006; NACO National Conference on Research in HIV and AIDS; Delhi, India. [Google Scholar]
- 17.Hernandez AL, Lindan CP, Mathur M, et al. Sexual behavior among men who have sex with women, men, and Hijras in Mumbai, India—multiple sexual risks. AIDS and Behavior. 2006;10(1):5–16. doi: 10.1007/s10461-006-9129-z. [DOI] [PubMed] [Google Scholar]
- 18.Hernandez AL, et al. Men in India have sex with women as well as other men and Hijras-multiple sexual risks. Presentation presented at; 2004; 15th International AIDS Conference; Bangkok, Thailand. [Google Scholar]
- 19.Kumta S, et al. Men who have sex with men (MSM) and male-to-female transgender (TG) in Mumbai: A critical emerging risk group for HIV and sexually transmitted infections (STI) in India. Presentation presented at; 2002; 14th International AIDS Conference; Barcelona, Spain. [Google Scholar]
- 20.Cocks K, Torgerson DJ. Sample size calculations for pilot randomized trials: a confidence interval approach. J Clin Epidemiol. 2013;66(2):197–201. doi: 10.1016/j.jclinepi.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 21.Feeley N, Cossette S, Cote J, et al. The importance of piloting an RCT intervention. Can J Nurs Res. 2009;41(2):85–99. [PubMed] [Google Scholar]
- 22.Kraemer HC, Mintz J, Noda A, Tinklenberg J, Yesavage JA. Caution regarding the use of pilot studies to guide power calculations for study proposals. Arch Gen Psychiatry. 2006;63(5):484–489. doi: 10.1001/archpsyc.63.5.484. [DOI] [PubMed] [Google Scholar]
- 23.Lancaster GA, Dodd S, Williamson PR. Design and analysis of pilot studies: recommendations for good practice. J Eval Clin Pract. 2004;10(2):307–312. doi: 10.1111/j..2002.384.doc.x. [DOI] [PubMed] [Google Scholar]
- 24.Shanyinde M, Pickering RM, Weatherall M. Questions asked and answered in pilot and feasibility randomized controlled trials. BMC Med Res Methodol. 2011;11:117. doi: 10.1186/1471-2288-11-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sim J, Lewis M. The size of a pilot study for a clinical trial should be calculated in relation to considerations of precision and efficiency. J Clin Epidemiol. 2012;65(3):301–308. doi: 10.1016/j.jclinepi.2011.07.011. [DOI] [PubMed] [Google Scholar]
- 26.Thabane L, Ma J, Chu R, et al. A tutorial on pilot studies: the what, why and how. BMC Med Res Methodol. 2010;10:1. doi: 10.1186/1471-2288-10-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vickers AJ. Underpowering in randomized trials reporting a sample size calculation. J Clin Epidemiol. 2003;56(8):717–720. doi: 10.1016/s0895-4356(03)00141-0. [DOI] [PubMed] [Google Scholar]