Abstract
Male sex workers (MSW) are a significant but invisible population in India who are at risk for HIV/STI. Few studies from India have documented HIV risk factors and motivations for sex work in this population. Between 2013 and 2014, a community-based convenience sample of 100 MSW in Chennai (south India) completed a baseline risk assessment as part of a behavioral intervention. Participants were ≥18 years, and reported current sex work. We report medians and proportions, and Wilcoxon-Mann-Whitney and chi-square tests are used to examine differences between sex work and sexual behavior measures by income source. Participants were engaged in sex work for 5.0 years (IQR=2.3-10.0), and earned 3,000 (IQR=2000-8000) Rupees (<50 USD) per month from sex work. Sixty-four percent reported ever testing for HIV and 20.2% for any STI. The most common reasons for starting sex work were money (83.0) and pleasure (56.0%). Participants reported 8.0 (IQR=3.0-15.0) male clients and 7 (IQR=4.0-15.0) condomless anal sex acts with male clients in the past month. Compared to participants with an additional source of income, those whose only source of income was sex work reported more male clients in the past month (10.0 vs. 6.0, p=0.017), as well as more condomless anal sex acts with male clients (8.0 vs. 5.0, p=0.008). Nearly 70.0% were offered more money not to use a condom during sex with a client, and 74.2% reported accepting more money not to use a condom. Three-quarters reported having experienced difficulty using condoms with clients. MSW in India engage in high levels of sexual risk for HIV/STIs. Money appears to be a driving factor for engaging in sex work and condomless sex with clients. HIV prevention interventions with MSW should focus on facilitating skills that will support their ability to negotiate sexual safety in the context of monetary disincentives.
Keywords: men who have sex with men, HIV prevention, male sex workers, India, sexual risk
Introduction
The HIV epidemic in India is fueled by sexual transmission, primarily between men who have sex with men (MSM) (National AIDS Control Organization, 2015; UNAIDS, 2013). Estimates of the prevalence of HIV among MSM in India generally range from 7.0 to 16.5% (Joint United Nations Programme on HIV/AIDS, 2010; Thomas et al., 2009), significantly higher than the India National AIDS Control Unit 2015 estimate of the overall HIV prevalence in India of 0.36% (National AIDS Control Organization, 2015). An invisible and often ignored population due to stigma and societal expectations, male sex workers (MSW) who have sex with men are at elevated risk for HIV and other STIs compared to the broader MSM population. Contextual factors related to sex work, including stigma, increased financial incentives for riskier behaviors, and lack of access to prevention services make it likely that the prevalence of HIV and STIs among MSW exceeds that of the broader MSM population in India (Biello, Colby, Closson, & Mimiaga, 2014; Chakrapani, Shunmugam, Newman, Kershaw, & Dubrow, 2015; Closson et al., 2015; Oldenburg, Biello, et al., 2014; Oldenburg et al., 2015; Shinde, Setia, Row-Kavi, Anand, & Jerajani, 2009). Few studies have sought to estimate the prevalence of HIV among MSW specifically, with some estimates as high as 33.0% among a population of MSW living in Maharashtra (Shinde et al., 2009). Despite their increased risk and significant contribution to the HIV epidemic in India (National AIDS Control Organization, 2015; UNAIDS, 2013), MSW remain understudied when compared to female sex workers and the broader population of MSM in India.
Previous studies that have sought to characterize the MSW population in India have been limited in scope, and geographically concentrated in Mumbai and Hyderabad, two of the largest cities in India (Narayanan et al., 2013; Shinde et al., 2009). Shinde et al. identified an HIV prevalence of 17.0% and a syphilis prevalence of 28% among MSW in Mumbai, 13.0% of which report never having used a condom (Shinde et al., 2009). Using data from a study of MSM attending STI clinics in Mumbai and Hyderabad, Narayanan et al. reported an HIV prevalence of 43.6% among MSM who engage in sex work (Narayanan et al., 2013). In Chennai – the biggest industrial and commercial center of South India – the prevalence of HIV and risk factors for HIV acquisition among the broader MSM community have been characterized (Chakrapani, Newman, & Shunmugam, 2008; Go et al., 2004; Mimiaga et al., 2011; Thomas et al., 2009). Thomas et al. identified not having previously engaged in an HIV prevention program, having symptoms of clinical depression and lower self-efficacy as predictors for MSM engaging in unprotected anal intercourse, a key risk factor for testing positive for HIV (Thomas et al., 2009). Despite this, limited research has examined behavioral factors and sexual risk specifically among MSW in India.
While numerous studies have examined HIV risk behavior among MSW in other parts of Southeast Asia (Biello et al., 2014; Chemnasiri et al., 2010; Colby et al., 2012; Guadamuz et al., 2010; Toledo et al., 2010), these studies have focused on Thailand and Vietnam. To the best of our knowledge, no studies have explored risk factors and motivations for engaging in sex work among MSW in India (Shinde et al., 2009). Using baseline data from a pilot intervention study to reduce HIV risk, we describe sociodemographic risk factors, motivations for sex work, sexual behaviors, and sex work characteristics among a sample of 100 MSW in Chennai, India.
Methods
Participants and Procedures
Between July 2013 and June 2014 one hundred MSW from Chennai, India completed a baseline behavioral assessment battery as part of their involvement in a pilot of an HIV prevention intervention for MSW. Participants were 18 years or older, born biologically male at birth, identified as male, and reported having anal sex (insertive or receptive) with another man in exchange for money, goods, favors or gifts, in the 3 months prior to enrollment. MSW were recruited by trained employees of Sahodaran, a non-governmental organization that provides HIV-related prevention and care services, and other support services to MSM in Chennai. Sahodaran staff provided MSM information about the study during normal street-based outreach activities, and those interested were then able to reach out to study staff. MSM were informed that their participation, refusal to participate, or withdrawal from the study in no way would affect their services at Sahodaran. Hijra (transgender women) were not included in the current study, as previous studies have shown that hijra have a distinct set of needs and specific interventions should be designed to target gender minority populations (Altaf, Zahidie, & Agha, 2012; Phillips et al., 2013; Sahastrabuddhe et al., 2012). The assessment battery was administered in Tamil by a trained research assistant in a private room at the National Institute for Research on Tuberculosis in Chennai. However, the section on sexual transmission risk behaviors was assessed using an audio-computer assisted self-interview (A-CASI) device in order to reduce social desirability bias (Kurth et al., 2004). Additionally, participants received HIV counseling and testing by trained counselors. Three percent of the sample had a reactive test at baseline.
All participants completed a written informed consent process before data collection commenced. Procedures were approved by the Institutional Review Boards at Fenway Health as well as the Ethics Committees at National Institute for Research on Tuberculosis and the Indian Council for Medical Research.
Measures
Personal Characteristics
The assessment included questions on age, education, relationship status, religion, alcohol use, and HIV status. We also assessed sexual identity using categories appropriate for India: Panthi (i.e., MSM who display more masculine characteristics and are exclusively insertive), Kothi (i.e., MSM who typically display more effeminate characteristics and are likely to take the receptive role in sex) or Double-Decker (i.e., MSM who do not necessarily display effeminate characteristics and may have sex with either men or women, and may be either insertive and/or receptive during anal sex) (Asthana & Oostvogels, 2001).
Sex work
Participants reported the number of years that they had been engaged in sex work, their typical monthly income from sex work, and whether sex work was their only source of income. Participants were asked to report reasons for starting and continuing sex work, separately. They could choose as many as they endorsed from the following response options (which were informed by formative work in an earlier phase of this study): money, money for family, pay for drugs, place to sleep, excitement, pleasure, educational expenses, coerced/forced, feel better about myself. Additionally, participants were asked if they had any desire to stop doing sex work, and how often they felt good about engaging in sex work. Participants were also asked whether they had experienced any of the following forms of violence while engaging in sex work: (i) verbal abuse; (ii) physical abuse; (iii) forced to not use a condom; (iv) forced anal sex; and (v) forced alcohol use.
Sexual behaviors
Participants reported the number of male clients and non-paying male sex partners they had in past month and how many times they had condomless anal sex with these partners and clients. To assess condom use self-efficacy, participants were asked if they had ever been offered more money not to use a condom with a client, if they ever accepted more money not to use a condom with a client, and if they ever had difficulty using condoms with male clients and non-paying sex partners. Finally, the assessment had a series of questions on sexual activity with participants' most recent clients, including the amount paid, what sexual acts occurred, knowledge of client's HIV status and frequency of condom use.
Statistical Methods
Medians (with interquartile ranges) for continuous variables and frequencies for categorical variables were calculated to describe characteristics of the participants, overall and stratified by whether or not sex work was the only source of income. Wilcoxon-Mann-Whitney tests and chi-square tests were used to test differences by income source across personal characteristics, sex work related measures, and sexual behaviors. Multivariable logistic regressions were used to assess the association between income source and the sexual behavior and sex work related variables, controlling for age, sexual orientation, education and religion. All analyses were conducted in SAS statistical analysis software (version 9.4).
Results
Personal characteristics are described in Table 1. In brief, the median age of the participants was 25 years (IQR=21.0-31.75). Kothi was the predominant (77.0%) sexual identity of the sample. Half of participants had completed secondary education or less, and 86.0% identified as Hindu. Nearly two-thirds (63.6%) reported having ever been tested for HIV (outside of the current study) and one-fifth (20.2%) for any STIs.
Table 1. Personal Characteristics among male sex workers, Chennai, India (N=100).
| Overall (n=100) |
Income from sex work only (n=41) |
Other source of income (n=59) |
Chi-Square test statistic | p | |
|---|---|---|---|---|---|
| Median (IQR) | |||||
| Age | 25.0 (21.0-31.75) |
23 (21-30) |
26 (22-34) |
2.55 | .110 |
| % (N) | |||||
| Sexual Orientation | 0.15 | .928 | |||
| Panthi | 2.00 (2) | 2.44 (1) | 1.69 (1) | ||
| Kothi | 77.00 (77) | 78.05 (32) | 76.27 (45) | ||
| Double Decker | 21.00 (21) | 19.51 (8) | 22.03 (13) | ||
| Education | 5.27 | .072 | |||
| Secondary or less | 50.0 (50) | 36.59 (15) | 59.32 (35) | ||
| Higher Secondary | 19.0 (19) | 21.95 (9) | 16.95 (10) | ||
| College or more | 31.0 (31) | 41.46 (17) | 23.73 (14) | ||
| Religion | 2.44 | .118 | |||
| Hindu | 85.86 (85) | 92.5 (37) | 81.36 (48) | ||
| Other | 14.14 (14) | 7.50 (3) | 18.64 (11) | ||
| Ever tested for HIV | 63.64 (63) | 65.00 (26) | 62.71 (37) | 0.05 | .816 |
| Ever tested for STD | 20.20 (20) | 15.00 (6) | 23.73 (14) | 1.13 | .289 |
| Ever any STD symptoms | 14.0 (14) | 19.51 (8) | 10.17 (6) | 1.75 | .185 |
| HIV infected (via rapid testing) | 3.0 (3) | 2.44 (1) | 3.39 (2) | 0.08 | .784 |
| No alcohol use during sex in past 3 months | 51.00 (51) | 51.22 (21) | 50.85 (30) | 0.001 | .971 |
Forty-one percent reported that their only source of income came from sex work. There were no significant differences in personal characteristics by source of income. The most common reasons for starting and for continuing sex work were money (83.0% and 93.0%, respectively) and pleasure (56.0% and 50.0%, respectively). The least common reasons were to pay for drugs (0.0% and 1.0%, respectively) and or because they were coerced (1.0% and 0.0%, respectively). These reasons did not differ significantly by income source (all p>0.05). While 37.0% reported having a desire to stop doing sex work at some time, nearly three-quarters (72.0%) reported usually or always feeling good about engaging in sex work.
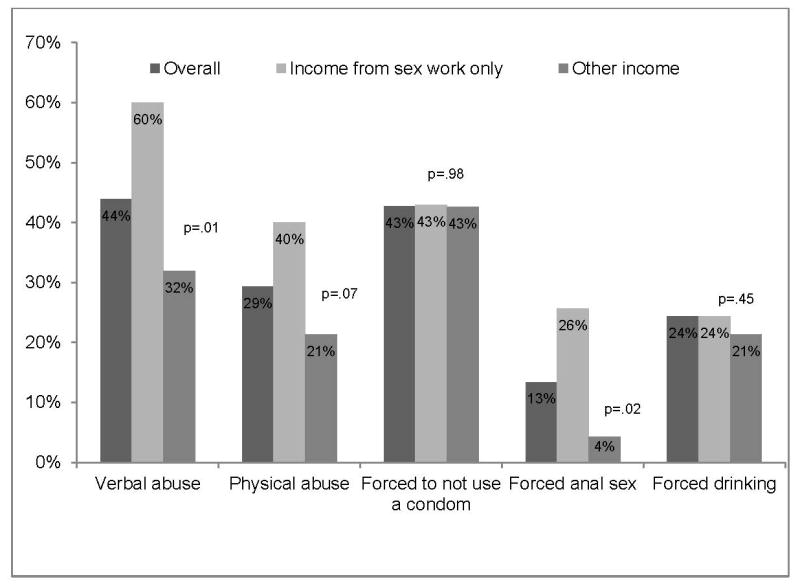
Experiences of violence while engaging in sex work are summarized in Figure 1. In multivariable models, adjusting for age, sexual orientation, education and religion, participants whose only source of income was from sex work were nearly six times as likely to report verbal abuse (aOR= 5.73, 95% CI 1.47-22.25; p=0.012) compared to those who had an additional source of income. While less common overall (13.0%), participants whose only source of income was from sex work were also five times as likely to report forced anal sex compared to those who had an additional source of income; however, this was no longer statistically significant in multivariable models (aOR= 5.24, 95% CI 0.78-29.0; p=0.089). Being forced to not use a condom for anal sex (43.0%), physical abuse (29.3%), and forced alcohol use (24.0%) were common, but did not significantly differ by income source (all p>0.10).
Figure 1. Experiences of violence while engaging in sex work among male sex workers, Chennai, India (N=100).
Sexual behaviors are reported in Table 2. The median number of years doing sex work was 5 (IQR=2.3-10.0), with a typical monthly income from sex work reported as 8,000 Rupees (approximately 123 USD) for participants whose income was from sex work only and 2,000 Rupees (approximately 31 USD) for participants who had other income (p<0.001). Compared to those who had other income, participants whose only income came from sex work reported significantly more male clients (median=10.0 vs. 6.0, p=0.017) and more condomless anal sex acts with male clients (median=8.0 vs. 5.0, p=0.008) in the past month. However, in multivariable models adjusting for age, sexual orientation, education and religion, only the association between monthly income from sex work (in thousands of Rupees) and source of income remained statistically significant (aOR=1.44, 95% CI 1.15-1.80; p<.001). Over two-thirds of participants (70.0%) reported being offered more money to not use a condom with a client, of which 74.2% report accepting the money to not use a condom. Two-thirds reported difficulty using condoms with clients. These did not differ significantly by income source in bivariate or multivariable models.
Table 2. Sexual behaviors and sex work-related measures among male sex workers, Chennai, India (N=100).
| Overall (n=100) |
Income from sex work only (n=41) |
Other income (n=59) |
Chi-Square test statistic | p | |
|---|---|---|---|---|---|
| Median (IQR) | |||||
| Years doing sex work | 5.0 (2.3-10.0) |
4 (2-8) |
7 (2.6-10) |
2.48 | .116 |
| Typical monthly income from sex work, in thousands of Rupees |
3 (2-8) |
8 (5-15) |
2 (1.5-3) |
29.97 | <.001 |
| No. of non-paying male partners, past month | 2 (0-6) |
2 (0-7) |
2 (0-5) |
0.17 | .681 |
| No. of times condomless anal sex with non-paying male partners, past month | 1 (0-4) |
2 (0-5) |
1 (0-4) |
0.52 | .470 |
| No. of paying male clients, past month |
8 (3-15) |
10 (6-20) |
6 (3-10) |
5.73 | .017 |
| No. of times condomless sex with paying male clients, past month |
7 (4-15) |
8 (6-20) |
5 (3-10) |
7.09 | .008 |
| % | |||||
| Ever been offered more money to NOT use condom | 69.4 | 77.5 | 63.8 | 2.09 | .148 |
| Difficulty using condoms with non-paying partners | 0.61 | .739 | |||
| Yes | 55.0 | 58.5 | 52.5 | ||
| No | 26.0 | 21.9 | 28.8 | ||
| Don't Know | 19.0 | 19.5 | 18.6 | ||
| Difficulty using condoms with clients | 0.41 | .816 | |||
| Yes | 66.7 | 70.0 | 64.4 | ||
| No | 21.2 | 20.0 | 22.0 | ||
| Don't Know | 12.1 | 10.0 | 13.6 | ||
| Sex with Most Recent Client | |||||
| Median (IQR) | |||||
| Rupees paid for most recent sex act | 350 (150-600) |
400 (200-800) |
300 (100-500) |
0.78 | 0.376 |
| % | |||||
| During this sexual act, which of the following occurred? | |||||
| Receptive oral sex | 64.0 | 68.3 | 61.0 | 0.56 | 0.456 |
| Insertive oral sex | 9.0 | 17.1 | 3.4 | 5.53 | 0.019 |
| Receptive anal sex | 70.0 | 73.2 | 67.8 | 0.33 | 0.564 |
| Insertive anal sex | 6.0 | 9.8 | 3.4 | 0.088 | |
| Knowledge of client HIV status during most recent sex act | 0.78 | 0.677 | |||
| Client did NOT have HIV | 51.0 | 46.3 | 54.2 | ||
| Client did have HIV | 3.0 | 2.4 | 3.4 | ||
| Did NOT KNOW HIV status of client | 46.0 | 51.2 | 42.4 | ||
| Used a condom during most recent sex act with client | 14.0 | 12.2 | 15.3 | 0.665 | |
When asked about sex with their most recent client (Table 2), participants reported being paid 350 Rupees (IQR=150.0-600.0) (approximately 5 USD) for the most recent transaction. Most participants reported that this sexual act included receptive anal sex (70.0%) and/or receptive oral sex (64.0%). A small minority reported insertive anal sex (6.0%) or insertive oral sex (9.0%) at last transaction, which differed significantly by income source in bivariate analysis (17.1% vs. 3.4%, p=0.019) but not in multivariable analyses (aOR=4.69, 95% CI 0.76, 28.76; p=0.09). Approximately half of participants reported that they did not know the HIV status of their most recent client, and 86.0% did not use a condom during the most recent sex act with a client.
Discussion
Findings from the present study describe high levels of sexual risk for HIV/STIs among MSW in Chennai, India. In the past month, MSW reported having 8 paying male clients and anal intercourse without a condom with male clients 7 times. Moreover, nearly half of participants did not know the HIV status of their most recent client, and 86.0% did not use a condom during the most recent sex with a client, considerably higher than reported in studies among MSW in other countries, including in Asian, Latin America and Europe (Ballester-Arnal, Gil-Llario, Salmeron-Sanchez, & Gimenez-Garcia, 2014). Both behaviors are demonstrated risk factors for HIV/ STI infection among MSM (S. Baral et al., 2009; Fan et al., 2012; Koblin et al., 2006; Trapence et al., 2012). In a study of 500 MSW living in Beijing, China, for example, Fan et al. found that not knowing the HIV status of the most recent male partner was associated with HIV infection (Fan et al., 2012).
Experiences of violence while engaging in sex work are common in this sample with high rates of verbal abuse and being forced to have anal sex without a condom. Instances of sexual violence among MSW have been commonly reported previously in other Asian countries. Biello et al. reported sexual violence prevalence at 19.8% among a population of 300 MSW in Ho Chi Minh City, Vietnam (Biello et al., 2014). Among sex workers in low- and middle-income countries, including those who identify as male, female, and transgender, experiencing violence is associated with an increase in HIV risk (S. Baral et al., 2012; S. Baral et al., 2014; S. D. Baral et al., 2015; Dunkle et al., 2013; Oldenburg et al., 2015; Oldenburg, Perez-Brumer, et al., 2014; Ulibarri et al., 2015). Previous studies have posited that violence can reduce a sex worker's ability to negotiate or control an encounter with a client, and their ability to use a condom with a client (Oldenburg, Perez-Brumer, et al., 2014; Ulibarri et al., 2015). Further, if a sex worker insists on using a condom, a client may turn violent and force the sex worker to have sex without a condom (Harcourt & Donovan, 2005).
Economic concerns appear to be a driving factor for engaging in sex work and higher risk sex with clients in this sample. A large majority of participants indicated that a reason for starting and engaging in sex work was money. Moreover, over two-thirds of participants reported being offered more money to not use a condom with a client. Previous studies have documented sex workers accepting additional financial incentives in exchange for unprotected sex, leading to an increased risk for HIV acquisition (Ballester-Arnal et al., 2014; Ballester, Salmeron, Gil, & Gomez, 2012; Muldoon et al., 2015; Nemoto et al., 2012; Patterson et al., 2012). A study of female sex workers in India conducted by Erausquin et al. between 2006 and 2010 identified accepting additional financial incentives for unprotected sex as a risk factor for HIV and STIs (Erausquin, Reed, & Blankenship, 2014). Moreover, those whose only source of income comes from sex work reported higher rates of violence in the context of sex work and more condomless anal sex with clients. Notably, most participants reported that sex work also provides pleasure and that they usually or always feel good about engaging in sex work. Together, these results suggest that a harm reduction approach to HIV/STI risk reduction may be appropriate, rather than focusing on abstaining from sex work all together.
These findings should be understood in the context of the study's limitations. The sample was not randomly selected and may not be representative of MSW in Chennai, India, and may not generalize to MSW in other cities and countries with distinct cultural norms and policies. Moreover, as with all self-report data, responses may be subject to social desirability or recall bias. However, importantly, the most sensitive sexual behavior questions were collected using ACASI in order to reduce self-report bias. Additionally, given that the survey used close-ended questions, the results may not represent the entire wide range of sex work experiences. Notably, in an earlier phase of this study, formative work was conducted and data was used to inform this study.
Notwithstanding these limitations, this study is, to the best of our knowledge, the first to characterize risk factors and motivations for engaging in sex work among MSW in Chennai, India. While exploratory in nature, these results suggest that HIV prevention interventions for MSW should explore supporting safe sexual practices, including facilitating sexual safety negotiation skills and strategies, in the face of monetary disincentives to do so, particularly given that many MSW may not want to stop sex work (Reed, Gupta, Biradavolu, & Blankenship, 2012).
Acknowledgments
This work was supported by the Indo-U.S. Joint Working Group on Prevention of Sexually Transmitted Diseases and HIV/AIDS through U.S. National Institute on Drug Abuse grant #R21DA033720 (Matthew Mimiaga, PI) and Indian Council of Medical Research grant #Indo-U.S/72/9/2010-ECDII (Beena Thomas, PI).
References
- Altaf A, Zahidie A, Agha A. Comparing risk factors of HIV among hijra sex workers in Larkana and other cities of Pakistan: an analytical cross sectional study. BMC public health. 2012;12(1):279. doi: 10.1186/1471-2458-12-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asthana S, Oostvogels R. The social construction of male ‘homosexuality’ in India: implications for HIV transmission and prevention. Soc Sci Med. 2001;52(5):707–721. doi: 10.1016/s0277-9536(00)00167-2. [DOI] [PubMed] [Google Scholar]
- Ballester-Arnal R, Gil-Llario MD, Salmeron-Sanchez P, Gimenez-Garcia C. HIV prevention interventions for young male commercial sex workers. Curr HIV/AIDS Rep. 2014;11(1):72–80. doi: 10.1007/s11904-013-0195-3. [DOI] [PubMed] [Google Scholar]
- Ballester R, Salmeron P, Gil MD, Gomez S. Sexual risk behaviors for HIV infection in Spanish male sex workers: differences according to educational level, country of origin and sexual orientation. AIDS Behav. 2012;16(4):960–968. doi: 10.1007/s10461-011-9964-4. [DOI] [PubMed] [Google Scholar]
- Baral S, Beyrer C, Muessig K, Poteat T, Wirtz AL, Decker MR, Kerrigan D. Burden of HIV among female sex workers in low-income and middle-income countries: a systematic review and meta-analysis. The Lancet infectious diseases. 2012;12(7):538–549. doi: 10.1016/S1473-3099(12)70066-X. [DOI] [PubMed] [Google Scholar]
- Baral S, Holland CE, Shannon K, Logie C, Semugoma P, Sithole B, Beyrer C. Enhancing Benefits or increasing harms: community responses for HIV among men who have sex with men, transgender women, female sex workers, and people who inject drugs. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2014;66:S319–S328. doi: 10.1097/QAI.0000000000000233. [DOI] [PubMed] [Google Scholar]
- Baral S, Trapence G, Motimedi F, Umar E, Iipinge S, Dausab F, Beyrer C. HIV prevalence, risks for HIV infection, and human rights among men who have sex with men (MSM) in Malawi, Namibia, and Botswana. PloS one. 2009;4(3):e4997. doi: 10.1371/journal.pone.0004997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baral SD, Friedman MR, Geibel S, Rebe K, Bozhinov B, Diouf D, Cáceres CF. Male sex workers: practices, contexts, and vulnerabilities for HIV acquisition and transmission. The Lancet. 2015;385(9964):260–273. doi: 10.1016/S0140-6736(14)60801-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biello KB, Colby D, Closson E, Mimiaga MJ. The syndemic condition of psychosocial problems and HIV risk among male sex workers in Ho Chi Minh City, Vietnam. AIDS and Behavior. 2014;18(7):1264–1271. doi: 10.1007/s10461-013-0632-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chakrapani V, Newman PA, Shunmugam M. Secondary HIV prevention among Kothi-identified MSM in Chennai, India. Culture, Health & Sexuality. 2008;10(4):313–327. doi: 10.1080/13691050701816714. [DOI] [PubMed] [Google Scholar]
- Chakrapani V, Shunmugam M, Newman PA, Kershaw T, Dubrow R. HIV Status Disclosure and Condom Use Among HIV-Positive Men Who Have Sex With Men and Hijras (Male-to-Female Transgender People) in India: Implications for Prevention. Journal of HIV/AIDS & Social Services. 2015;14(1):26–44. [Google Scholar]
- Chemnasiri T, Netwong T, Visarutratana S, Varangrat A, Li A, Phanuphak P, van Griensven F. Inconsistent condom use among young men who have sex with men, male sex workers, and transgenders in Thailand. AIDS Education & Prevention. 2010;22(2):100–109. doi: 10.1521/aeap.2010.22.2.100. [DOI] [PubMed] [Google Scholar]
- Closson EF, Colby DJ, Nguyen T, Cohen SS, Biello K, Mimiaga MJ. The balancing act: Exploring stigma, economic need and disclosure among male sex workers in Ho Chi Minh City, Vietnam. Global public health. 2015;10(4):520–531. doi: 10.1080/17441692.2014.992452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Colby D, Trang N, Lan H, Nguyen T, Thien D, Mai T, Mimiaga M. Prevalence of sexually transmitted diseases, HIV, and hepatitis among male sex workers in Ho Chi Minh City, Vietnam. International Journal of Infectious Diseases. 2012;16:e332. [Google Scholar]
- Dunkle KL, Wong FY, Nehl EJ, Lin L, He N, Huang J, Zheng T. Male-on-male intimate partner violence and sexual risk behaviors among money boys and other men who have sex with men in shanghai, china. Sexually transmitted diseases. 2013;40(5):362–365. doi: 10.1097/OLQ.0b013e318283d2af. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Erausquin JT, Reed E, Blankenship KM. Change over time in police interactions and HIV risk behavior among female sex workers in Andhra Pradesh, India. AIDS and Behavior. 2014:1–8. doi: 10.1007/s10461-014-0926-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fan S, Lu H, Ma X, Sun Y, He X, Li C, Ma W. Behavioral and serologic survey of men who have sex with men in Beijing, China: implication for HIV intervention. AIDS patient care and STDs. 2012;26(3):148–155. doi: 10.1089/apc.2011.0277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Go VF, Srikrishnan AK, Sivaram S, Murugavel GK, Galai N, Johnson SC, Celentano DD. High HIV prevalence and risk behaviors in men who have sex with men in Chennai, India. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2004;35(3):314–319. doi: 10.1097/00126334-200403010-00014. [DOI] [PubMed] [Google Scholar]
- Guadamuz TE, Kunawararak P, Beyrer C, Pumpaisanchai J, Wei C, Celentano DD. HIV prevalence, sexual and behavioral correlates among Shan, Hill tribe, and Thai male sex workers in Northern Thailand. AIDS care. 2010;22(5):597–605. doi: 10.1080/09540120903280935. [DOI] [PubMed] [Google Scholar]
- Harcourt C, Donovan B. The many faces of sex work. Sexually transmitted infections. 2005;81(3):201–206. doi: 10.1136/sti.2004.012468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Joint United Nations Programme on HIV/AIDS. Country Progress Report UNGASS India, 2010 2010 [Google Scholar]
- Koblin BA, Husnik MJ, Colfax G, Huang Y, Madison M, Mayer K, Buchbinder S. Risk factors for HIV infection among men who have sex with men. Aids. 2006;20(5):731–739. doi: 10.1097/01.aids.0000216374.61442.55. [DOI] [PubMed] [Google Scholar]
- Kurth AE, Martin DP, Golden MR, Weiss NS, Heagerty PJ, Spielberg F, Holmes KK. A comparison between audio computer-assisted self-interviews and clinician interviews for obtaining the sexual history. Sexually transmitted diseases. 2004;31(12):719–726. doi: 10.1097/01.olq.0000145855.36181.13. [DOI] [PubMed] [Google Scholar]
- Mimiaga M, Thomas B, Mayer K, Reisner S, Menon S, Swaminathan S, Safren S. Alcohol use and HIV sexual risk among MSM in Chennai, India. International journal of STD & AIDS. 2011;22(3):121–125. doi: 10.1258/ijsa.2009.009059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muldoon KA, Akello M, Muzaaya G, Simo A, Shoveller J, Shannon K. Policing the epidemic: High burden of workplace violence among female sex workers in conflict-affected northern Uganda. Global public health. 2015:1–14. doi: 10.1080/17441692.2015.1091489. [DOI] [PubMed] [Google Scholar]
- Narayanan P, Das A, Morineau G, Prabhakar P, Deshpande GR, Gangakhedkar R, Risbud A. An exploration of elevated HIV and STI risk among male sex workers from India. BMC public health. 2013;13(1):1059. doi: 10.1186/1471-2458-13-1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National AIDS Control Organization. Narrative Country Progress Report of India: Global AIDS Response Progress Reporting 2015. 2015 Retrieved from. [Google Scholar]
- Nemoto T, Iwamoto M, Perngparn U, Areesantichai C, Kamitani E, Sakata M. HIV-related risk behaviors among kathoey (male-to-female transgender) sex workers in Bangkok, Thailand. AIDS care. 2012;24(2):210–219. doi: 10.1080/09540121.2011.597709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Biello KB, Colby D, Closson EF, Mai T, Nguyen T, Mimiaga MJ. Stigma related to sex work among men who engage in transactional sex with men in Ho Chi Minh City, Vietnam. International journal of public health. 2014;59(5):833–840. doi: 10.1007/s00038-014-0562-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Perez-Brumer AG, Biello KB, Landers SJ, Rosenberger JG, Novak DS, Mimiaga MJ. Transactional Sex Among Men Who Have Sex With Men in Latin America: Economic, Sociodemographic, and Psychosocial Factors. American journal of public health. 2015;105(5):e95–e102. doi: 10.2105/AJPH.2014.302402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Perez-Brumer AG, Reisner SL, Mattie J, Bärnighausen T, Mayer KH, Mimiaga MJ. Global burden of HIV among men who engage in transactional sex: a systematic review and meta-analysis. 2014 doi: 10.1371/journal.pone.0103549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patterson TL, Volkmann T, Gallardo M, Goldenberg S, Lozada R, Semple SJ, Strathdee SA. Identifying the HIV transmission bridge: which men are having unsafe sex with female sex workers and with their own wives or steady partners? Journal of acquired immune deficiency syndromes (1999) 2012;60(4):414. doi: 10.1097/QAI.0b013e31825693f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips AE, Molitor J, Boily MC, Lowndes CM, Gurav K, Blanchard J, Alary M. Informal confidential voting interviewing in a sexual risk assessment of men who have sex with men (MSM) and transgenders (hijra) in Bangalore, India. Sexually transmitted infections. 2013;89(3):245–250. doi: 10.1136/sextrans-2011-050373. [DOI] [PubMed] [Google Scholar]
- Reed E, Gupta J, Biradavolu M, Blankenship K. Migration/mobility and risk factors for HIV among female sex workers in Andhra Pradesh, India: implications for HIV prevention. International journal of STD & AIDS. 2012;23(4):e7–e13. doi: 10.1258/ijsa.2009.009421. [DOI] [PubMed] [Google Scholar]
- Sahastrabuddhe S, Gupta A, Stuart E, Godbole S, Ghate M, Sahay S, Bollinger R. Sexually transmitted infections and risk behaviors among transgender persons (Hijras) of Pune, India. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2012;59(1):72–78. doi: 10.1097/QAI.0b013e318236bd6f. [DOI] [PubMed] [Google Scholar]
- Shinde S, Setia MS, Row-Kavi A, Anand V, Jerajani H. Male sex workers: are we ignoring a risk group in Mumbai, India? Indian Journal of Dermatology, Venereology, and Leprology. 2009;75(1):41. doi: 10.4103/0378-6323.45219. [DOI] [PubMed] [Google Scholar]
- Thomas B, Mimiaga MJ, Menon S, Chandrasekaran V, Murugesan P, Swaminathan S, Safren SA. Unseen and unheard: predictors of sexual risk behavior and HIV infection among men who have sex with men in Chennai, India. AIDS Educ Prev. 2009;21(4):372–383. doi: 10.1521/aeap.2009.21.4.372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Toledo CA, Varangrat A, Wimolsate W, Chemnasiri T, Phanuphak P, Kalayil EJ, van Griensven F. Examining HIV infection among male sex workers in Bangkok, Thailand: a comparison of participants recruited at entertainment and street venues. AIDS Education and Prevention. 2010;22(4):299–311. doi: 10.1521/aeap.2010.22.4.299. [DOI] [PubMed] [Google Scholar]
- Trapence G, Collins C, Avrett S, Carr R, Sanchez H, Ayala G, Baral SD. From personal survival to public health: community leadership by men who have sex with men in the response to HIV. Lancet. 2012;380(9839):400–410. doi: 10.1016/S0140-6736(12)60834-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ulibarri MD, Roesch S, Rangel MG, Staines H, Amaro H, Strathdee SA. “Amar te duele”(“Love hurts”): sexual relationship power, intimate partner violence, depression symptoms and HIV risk among female sex workers who use drugs and their non-commercial, steady partners in Mexico. AIDS and Behavior. 2015;19(1):9–18. doi: 10.1007/s10461-014-0772-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- UNAIDS. AIDS epidemic update: November 2009 2013 [Google Scholar]


