Abstract
The efforts to control and eradicate polio as a global health burden have been successful to the point where currently only three countries now report endemic polio, and the number of cases of polio continues to decrease. The success of the polio programme has been dependant on a well-developed network of laboratories termed the global polio laboratory network (GPLN). Here we explore collaborative opportunities with the GPLN to target two of the 18 diseases listed as a neglected tropical diseases (NTD) namely soil transmitted helminthiasis (STH) and Schistosomiasis (SCH). These were chosen based on prevalence and the use of faecal materials to identify both polio, STH and SCH. Our study screened 448 faecal samples from the Ghana GPLN using three triplex TaqMan assays to identify Ascaris lumbricoides, Necator americanus, Ancylostoma spp, Trichuris trchiura, Strongyloides stercoralis and Schistosoma spp. Our results found a combined helminth prevalence of 22%. The most common helminth infection was A. lumbricoides with a prevalence of 15% followed by N. americanus (5%), Ancylostoma spp. (2.5%), Schistosoma spp. (1.6%) and S. stercoralis (1%). These results show that it is possible to identify alternative pathogens to polio in the samples collected by the GPLN platform and to introduce new diagnostic assays to their laboratories. The diagnostic methods employed were also able to identify S. stercoralis positive samples, which are difficult to identify using parasitological methods such as Kato-Katz. This study raises the possibility of collaboration with the GPLN for the surveillance of a wider range of diseases which would both benefit the efforts to control the NTDs and also increase the scope of the GPLN as a diagnostic platform.
Author summary
The successful campaign being waged against polio has eliminated the disease from most countries where it was once endemic. With this success, it is anticipated that the disease will be eradicated in the coming years with only 37 cases being reported in 2016. Although the efforts to control polio are successful there are a number of low-profile, but no less serious disease, that are still highly prevalent throughout the world. These diseases have been termed the neglected tropical diseases (NTD) and this study aims to test the suitability of the Global Polio Laboratory Network (GPLN) as a platform to screen for two of the NTDs, soil transmitted helminthiasis (STH) and schistosomiasis (SCH). To test the suitability of the samples collected by the GPLN and the suitability of the laboratories themselves 448 samples from the Ghanaian GPLN laboratory were screened with multiplex TaqMan assays for the following six helminth types: Ascaris lumbricoides, Necator americanus, Ancylostoma spp, Trichuris trchiura, Strongyloides stercoralis and Schistosoma spp. Using this method this study was able to identify a prevalence of 22% for the combined helminth infection. The most common infection was A. lumbricoides with a prevalence of 15% followed by N. americanus (5%), Ancylostoma spp. (2.5%), Schistosoma spp. (1.6%) and S. stercoralis (1%). The success of this study indicates that this may be a cost-effective method to passively screen a country for STH and SCH and its success in identifying S. stercoralis infections makes it especially useful as this parasite is hard to identify using traditional surveillance techniques.
Introduction
In 1988 the WHO set out to eradicate polio after the successful development of effective polio vaccines and since then the eradication campaign has reduced the number of countries reporting endemic polio from 125 to three in 2016. Control of polio has been a co-ordinated effort involving two main arms; the delivery of vaccination alongside establishing an effective laboratory network for monitoring and surveillance. This surveillance arm is comprised of 145 labs spread throughout the world which taken as a whole forms the Global Polio Laboratory Network (GPLN). The network receives samples from local health clinics where individuals have presented with clinical signs of the disease, typically acute flaccid paralysis (AFP), with the need to confirm or exclude an aetiology of polio. Thus, investigation of AFP initially involves collection of a faecal sample(s) which is then transferred from the regional clinic thence to the central laboratory to undergo a culture screen for polio virus and if found positive is then followed up with a real-time PCR analysis with diagnostic primers able to identify and discriminate if the sample is wild type, vaccine strain or a vaccine-derived virus. Across Africa there are 16 GPLN labs and these have received, in total, an average of 22,017 samples per year in the past 5 years with Ghana contributing, on average, 350 samples per year. These 16 laboratories are divided into three regional reference laboratories (RRLs) and 13 intratypic differentiation laboratories (ITD). The ITD laboratories are responsible for the isolation of poliovirus, molecular characterization of isolates and referral of critical samples to a sequencing laboratory [1]. Currently faecal samples collected by the GPLN are only screened for polio and non-polio enteroviruses; here we explore the potential of the GPLN to screen for other pathogens of public health importance allowing for co-investigation.
Across the world, but especially in Africa, the Neglected Tropical Diseases (NTDs) are an umbrella group of diseases that afflict the poor and retain a cycle of poverty. In total, approximately a billion people from the poorest communities across the globe are infected with at least one NTD [2]. There are currently 18 diseases listed as NTDs [3] with seven of these diseases caused by parasitic helminths. The intestinal nematodes, often referred to as soil transmitted helminths (STH) contribute the greatest number of infections and highest number of DALYs lost for any NTD [4] closely followed by schistosomiasis (SCH), a waterborne trematode infection [5]. Recently the importance of control of these diseases has been recognised by policy makers and steps have been taken to develop cost effective strategies in managing them [6]. Although there are WHO guidelines for classic parasitological surveillance, there is no equivalent for a molecular diagnostic platform of these infections. A key block in doing so is the cost of setting up a standard surveillance platform, de novo, it would therefore be sensible to expand and strengthen existing surveillance structures. The GPLN is a good example and is maintained with substantial annual investments [7]. Thus being able to augment or ‘piggyback’ appropriate NTD surveillance onto the GPLN could have the necessary ‘kick-starting’ effect to provide better access to diagnostic tools needed for control and elimination of STH and SCH [8–12].
Addressing the need for a molecular diagnostics platform for NTDs, in this investigation we explore and develop synergies and necessary steps with the GPLN, taking advantage of its accumulated experience and resources, to include pilot screening for STH (A. lumbricoides, N. americanus, Ancylostoma spp, T. trchiura, S. stercoralis) and SCH (S. mansoni and S. haematobium). The Ghanaian National Polio laboratory based at the Noguchi Memorial Institute for Medical Research was selected to carry out this assessment determining the suitability of the GPLN faecal collections with multiplex TaqMan diagnostic assays.
Methods
Ethics
Ethics applications were approved by LSTM (Research protocol 16-007) and Noguchi Scientific and Technical Committee (Study number 065/16-17) followed by the Institutional Review Board. To obtain approval, initial patient collection forms were amended to later facilitate expanded diagnostic testing with the results made available to the national NTD programme. All participants were anonymised for the final study.
Training workshop
Prior to the work being carried at the Ghanaian GPLN a workshop was carried out to train the staff in the methods used to extract DNA from faecal samples and the subsequent optimisation and running of the qPCR TaqMan assays. The workshop included both practical and theoretical training, this gave the staff of the GPLN a good background knowledge and practical experience in the methods they would use [13, 14].
Samples
The samples used in this study were faecal samples sent to the Ghanaian GPLN laboratory from individuals presenting with acute flaccid paralysis. The samples were sent via courier from local health clinics and were kept at 4°C until it reached the GPLN laboratory at which point they were stored at -20°C. The age of the patients that supplied the sample as well as the district from which it originated from were available to this study.
DNA extraction
Faecal samples were removed from the -20°C freezer and allowed to defrost at room temperature, once defrosted ~0.1g of faeces was removed and placed into a 2mL screw cap sample tube that was preloaded with 0.9g of 1.4mm ceramic beads. To this 250μL of a 2% PVPP/PBS suspension was added and the sample vortexed for 5-10 seconds. The faecal suspension was then frozen at -20°C overnight. The following day the samples underwent bead-beating at 3000rpm for 30 seconds using the MagnaLyser system. DNA extraction was carried out using the QIAamp DNA Mini kit per the manufacturer’s instructions with the following two modifications: i) an aliquot of phocine herpes virus-1 was added to the AL buffer to act as an internal positive control for the subsequent TaqMan assays, ii) the DNA was eluted in 200μL of nuclease free water. As well as introducing Phocine Herpes Virus (PhHV) into each sample to act as an internal positive control a DNA extraction negative control was introduced after every 47th sample, in total 448 samples were processed [15].
Multiplex qPCR
The six helminth types were screened using previously described primers and probes [8–10, 12, 16, 17] and these were used in three triplex reactions, each targeting two helminth types and the internal positive control. The first of these targeted S. stercoralis and N. americanus; the second targeted Ancylostoma spp. and a generic Schistosoma spp. (S. mansoni, S. haematobium, S. intercalatum); the third triplex reaction targeted A. lumbricoides and T. trichiura (Table 1). The primer concentrations were determined individually through primer limiting assays and then tested in the final triplex concentrations using mono, double and triple target DNA assays to ensure there was no internal competition within a reaction. The final volume for each triplex reaction was 20μL, consisting of 12.5μL of iQ supermix, 2μL of DNA template and a final helminth primer concentration of 200nM except for Ancylostoma spp. which ran at 300nM; the concentration of all probes and the PhHV primers was 100nM. All assays were processed using the same ABI 7500 qPCR thermocycler. Each qPCR run consisted of the following cycle, an initial holding step at 95°C for three minutes followed by 50 cycles of 95°C for 15s, 60°C for 30s, 72°C for 30s and a final extension step at 72°C for two minutes.
Table 1. Primer and probes used in this study.
| Multiplex | Probe/Primer | Target | Probe and Primer sequence (5'-3') | Described |
|---|---|---|---|---|
| 1 | Forward | S. stercoralis | GAA TTC CAA GTA AAC GTA AGT CAT TAG C | Verweij 2009 |
| Reverse | TGC CTC TGG ATA TTG CTC AGT TC | |||
| Probe | FAM-ACA CAC CGG CCG TCG CTG C-BHQ1 | |||
| Forward | N. americanus | CTG TTT GTC GAA CGG TAC TTG C | Verweij 2007 | |
| Reverse | ATA ACA GCG TGC ACA TGT TGC | |||
| Probe | TAMRA-CTG TAC GCA TTG TAT AC-BHQ2 | |||
| 2 | Forward | Ancylostoma spp. | GAA TGA CAG CAA ACT CGT TGT TG | Verweij 2007 |
| Reverse | ATA CTA GCC ACT GCC GAA ACG T | |||
| Probe | TAMRA-ATC GTT TAC CGA CTT TAG-BHQ2 | |||
| Forward | Schistosoma spp. | GGTCTAGATGACTTGATYGAGATGCT | Obeng 2008 | |
| Reverse | TCCCGAGCGYGTATAATGTCATTA | |||
| Probe | FAM-TGG GTT GTG CTC GAG TCG TGG C-BHQ1 | |||
| 3 | Forward | A. lumbricoides | GTA ATA GCA GTC GGC GGT TTC TT | Wiria 2010 |
| Reverse | GCC CAA CAT GCC ACC TAT TC | |||
| Probe | TAMRA-TTG GCG GAC AAT TGC ATG CGA T-BHQ2 | |||
| Forward | T. trichiura | TTGAAACGACTTGCTCATCAACTT | Liu 2013 | |
| Reverse | CTGATTCTCCGTTAACCGTTGTC | |||
| Probe | FAM-CGA TGG TAC GCT ACG TGC TTA CCA TGG-BHQ1 | |||
| 1,2,3 | Forward | Phocine herpes virus | GGG CGA ATC ACA GAT TGA ATC | Niesters 2002 |
| Reverse | GCG GTT CCA AAC GTA CCA A | |||
| Probe | VIC-TTT TTA TGT GTC CGC CAC CAT CTG GAT C-BHQ2 |
Results
Location
The 10 regions of Ghana were used to categories the origins of the samples collected by the Ghanaian GPLN. This was then used to determine how evenly across Ghana the origins of the samples were distributed. The region that contributed the most samples was Brong Ahafo, where 23% of the samples originated from following this was the Western region, supplying 15% of the samples. The Ashanti, Central, Greater Accra, Northern, Upper East and Volta regions all contributed a similar amount of between 7-10%. The regions that contributed the least number of samples were the Eastern and Upper West Regions. The distribution of the participants that supplied the samples can be shown to have come from across the country with most regions contributing a similar number of samples.
Age
Due to the anonymity of the samples the sex of the participants was unknown and could not be included as a risk factor, however their age was recorded. It was possible to observe the age range of samples as this would affect the suitability of samples for STH screening. Across the 10 regions the average age ranged from 5 to 6 years and an analysis using ANOVA resulted in a P = 0.16, indicating there was no significant difference in participants age across the six regions of Ghana. Breaking down the ages of participants into pre-school age (PSAC, 0-4 yrs), school age (SAC, 5-16yrs) and adults (17+) the following percentages were found for each group: 60%, 30% and 10% respectively.
Parasitology
The qPCR assay was successful in identifying positive samples for A. lumbricoides, N. americanus, A. duodenale, Schistosoma and S. stercoralis. A total of 102 out of 448 samples were found to be positive for one or more helminth types tested, giving an overall prevalence of 22.7% with 92 of these being single helminth infections and 10 being double infections (Table 2)
Table 2. Species contribution to single and mixed helminth infections.
| Single Infections | |||||||
| Ascaris | Necator | Ancylostoma | Trichuris | Schistosoma | Strongyloides | Total | |
| 59 | 15 | 10 | 0 | 5 | 3 | 92 | |
| Double Infections | |||||||
| Ascaris/Necator | Asccaris/Schistosoma | Ascaris/Strongyloides | Necator /Ancylostoma | Total | |||
| 5 | 2 | 2 | 1 | 10 | |||
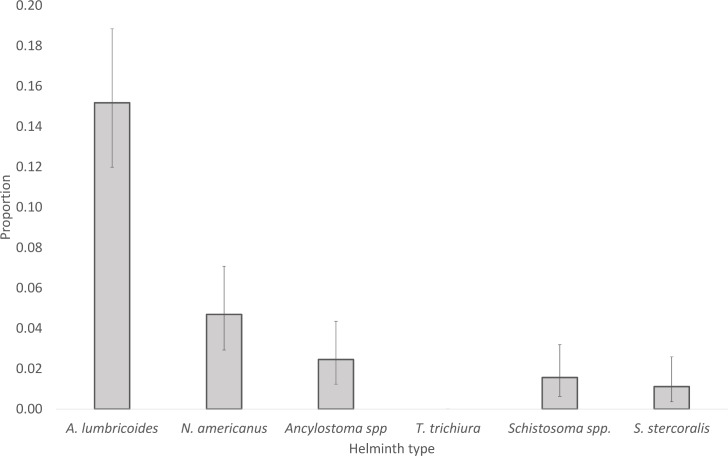
The proportion of samples positive for the different helminth types is shown in Fig 1, A. lumbricoides was found to be the most prevalent helminth, being found in 16% of all samples. The two-hookworm species followed with N. americanus found in 6% of samples and Ancylostoma spp. found in 3%. The prevalence of Schistosoma spp. and S. stercoralis was 2% and 1% respectively whilst no samples were found to be positive for T. trichiura.
Fig 1. Proportion of helminth types found.
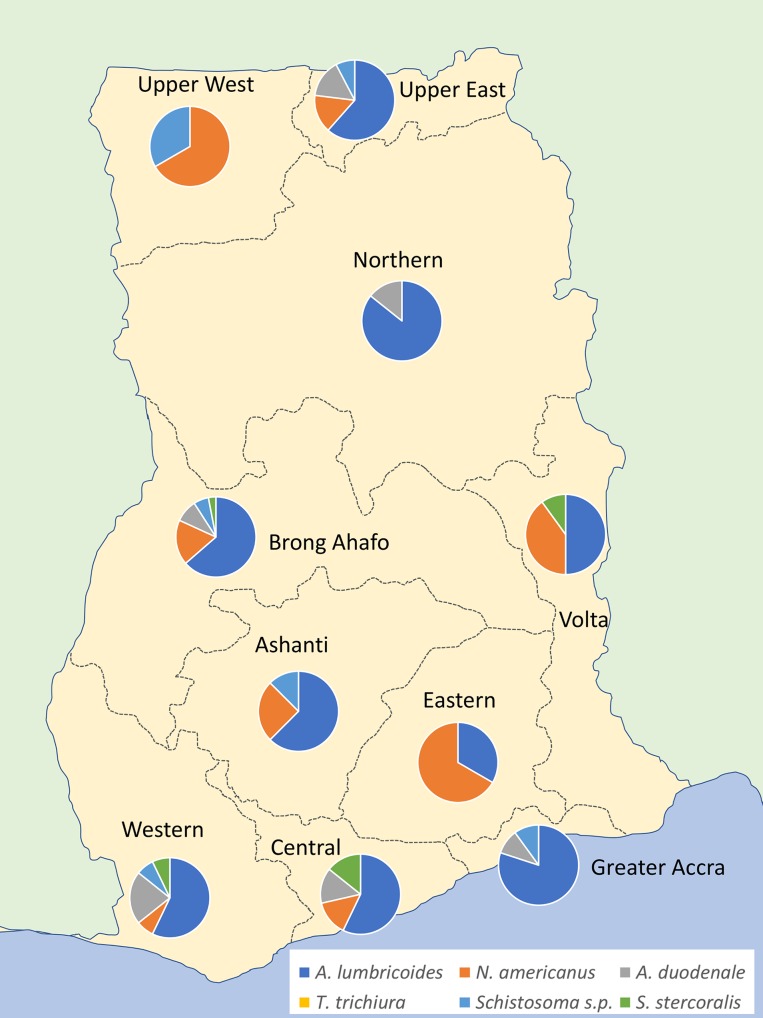
The distribution of helminth species across the different regions of Ghana varied with Brong Ahafo having the highest proportion of positive samples and the central region having the lowest proportion of positives. The distribution of helminth species across these regions was also not even with the Upper West, Northern and Eastern regions only being positive for two of the helminth types (Fig 2). Other regions contained samples positive for multiple species of helminth.
Fig 2. Geographical distribution of the different helminth positives from the GPLN samples screened in this study, Image created using GNU Image Manipulation Program [18].
Discussion
The purpose of this study is to demonstrate the suitability of adapting a GPLN laboratory for the detection of STH and SCH. It is not within the scope of this study to infer anything from the epidemiological data as the sample size is too small to be representative of the different administrative regions of Ghana. Similarly the samples collected by the GPLN will not be representative of the communities they originate from as they are from individuals that have presented with specific clinical symptoms, notably acute flaccid paralysis.
There were a total of 102 helminth positive samples detected out of a total of 448 samples screened, of which 92 were single infections comprising A. lumbricoides (59), N. americanus (15) and Ancylostoma spp. (10) respectively. Schistosoma spp. (5) was the next most common helminth although surprisingly no cases of Schistosoma spp. were detected in samples from the Volta. S. stercoralis is perhaps the least understood of the intestinal helminths [19] and is difficult to detect with traditional techniques, despite this our study was able to identify five cases of S. stercoralis, three single infections and two co-infections with A. lumbricoides. The total number of samples positive for co-infections was 10 of which half were a co-infection of A. lumbricoides and N. americanus.
The results show that the average age of participants falls between five to six years which means they fall within the SAC age group which is the usual target group for STH and SCH prevalence surveys. The sample contribution from each region varied from 23% to 3% however seven out of the 10 regions contributed a similar percentage of samples. Surprisingly no SCH positives were found in samples from the Volta. The reason for the lack of SCH positives from the Volta region is not yet clear and could be due to insufficient samples from this region, although this is unlikely as regions contributing fewer samples were still found to have SCH positives. An alternative explanation for the lack of Schistosoma s.l. positives is that the method described in this paper is more suited to the detection of S. mansoni than it is for S. haematobium, whose eggs are typically passed in stool samples, whereas S. haematobium predominantly pass their eggs in urine [20].
The scientific community has long acknowledged the likely high burden of disease and morbidity that is caused by S. stercoralis [21]. Current estimates of global infection range from 30 to 100 million [22, 23] although these estimates are based on imperfect sampling techniques and a more recent study has proposed a higher prevalence of 370 million people infected world-wide [24]. This wide range in prevalence estimates highlights the variable reliability of different screening methods. The most common method of screening for helminth infections, Kato-Katz, is poorly suited to the detection of S. stercoralis [25]. The success of the methodology used in this paper to detect S. stercoralis alongside the other STH species and Schistosoma spp. demonstrate the versatility of using qPCR to detect a wider range of helminth infections than more traditional methods. Currently there is no data regarding the distribution of S. stercoralis in Ghana however by screening the samples from the GPLN we were able to identify five samples positive for S. stercoralis.
The current design of the GPLN is not yet suited for its samples to be used to infer the distribution of STH and SCH as the samples are too few in number and are from a specific group within the population, those presenting with clinical signs of polio. The introduces confounding factors and does not provide a representative cross section of the communities at risk, notably adults and school age children were fewer in number than pre-school age children. To become an adequate surveillance platform the range of clinical symptoms for sample collection would need to be widened to include those presenting with STH and SCH symptoms. This would no doubt increase the number of samples being sent in for analysis and subsequently improve the surveillance capabilities of the system. However, this would no doubt incur a greater cost, a possible solution would be to incorporate other pathogens for screening to attract extra funding to cover these costs.
In conclusion, the findings of this study show that it is possible to identify STH and SCH positives in the faecal samples collected by the GPLN and that new diagnostic techniques can be introduced to compliment the work currently being carried out. The current narrow clinical symptoms required to qualify a sample to be sent to the GPLN limits their epidemiological use, a change in sample submission policy would be required to improve their epidemiological relevance. Despite this the study demonstrates a potential way forward in the monitoring and control of NTDs that could be included in the legacy plan of the GPLN.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
COUNTDOWN is a multi-disciplinary research consortium dedicated to investigating cost-effective, scaled-up and sustainable solutions, necessary to control and eliminate the seven most common NTDs by 2020. COUNTDOWN was formed in 2014 and is funded by UKAID part of the Department for International Development (DFID). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Gumede N, Coulibaly SO, Yahaya AA, Ndihokubwayo JB, Nsubuga P, Okeibunor J, et al. Polio Eradication Initiative (PEI) contribution in strengthening public health laboratories systems in the African region. Vaccine. 2016;34(43):5164–9. doi: 10.1016/j.vaccine.2016.05.055 PubMed PMID: WOS:000385597400007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Fenwick A. The global burden of neglected tropical diseases. Public Health. 2012;126(3):233–6. doi: 10.1016/j.puhe.2011.11.015 PubMed PMID: WOS:000301376000017. [DOI] [PubMed] [Google Scholar]
- 3.WHO. Neglected Tropical Diseases: Fact Sheets Relating to NTD [cited 2017]. Available from: http://www.who.int/neglected_diseases/mediacentre/factsheet/en/.
- 4.Pullan RL, Smith JL, Jasrasaria R, Brooker SJ. Global numbers of infection and disease burden of soil transmitted helminth infections in 2010. Parasites & Vectors. 2014;7 doi: 10.1186/1756-3305-7-37 PubMed PMID: WOS:000334641400001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van der Werf MJ, de Vlas SJ, Brooker S, Looman CWN, Nagelkerke NJD, Habbema JDF, et al. Quantification of clinical morbidity associated with schistosome infection in sub-Saharan Africa. Acta Tropica. 2003;86(2-3):125–39. doi: 10.1016/s0001-706x(03)00029-9 PubMed PMID: WOS:000183248200002. [DOI] [PubMed] [Google Scholar]
- 6.Molyneux DH, Hotez PJ, Fenwick A. "Rapid-impact interventions": How a policy of integrated control for Africa's neglected tropical diseases could benefit the poor. Plos Medicine. 2005;2(11):1064–70. doi: 10.1371/journal.pmed.0020336 PubMed PMID: WOS:000234303000012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.de Gourville E, Tebbens RJD, Sangrujee N, Pallansch MA, Thompson KM. Global surveillance and the value of information: The case of the global polio laboratory network. Risk Analysis. 2006;26(6):1557–69. doi: 10.1111/j.1539-6924.2006.00845.x PubMed PMID: WOS:000242867200014. [DOI] [PubMed] [Google Scholar]
- 8.Verweij JJ, Brienen EAT, Ziem J, Yelifari L, Polderman AM, Van Lieshout L. Simultaneous detection and quantification of Ancylostoma duodenale, Necator americanus, and Oesophagostomum bifurcum in fecal samples using multiplex real-time PCR. American Journal of Tropical Medicine and Hygiene. 2007;77(4):685–90. PubMed PMID: WOS:000250244800019. [PubMed] [Google Scholar]
- 9.Wiria AE, Prasetyani MA, Hamid F, Wammes LJ, Lell B, Ariawan I, et al. Does treatment of intestinal helminth infections influence malaria? Background and methodology of a longitudinal study of clinical, parasitological and immunological parameters in Nangapanda, Flores, Indonesia (ImmunoSPIN Study). Bmc Infectious Diseases. 2010;10 doi: 10.1186/1471-2334-10-77 PubMed PMID: WOS:000277054600001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Obeng BB, Aryeetey YA, de Dood CJ, Amoah AS, Larbi IA, Deelder AM, et al. Application of a circulating-cathodic-antigen (CCA) strip test and real-time PCR, in comparison with microscopy, for the detection of Schistosoma haematobium in urine samples from Ghana. Annals of Tropical Medicine and Parasitology. 2008;102(7):625–33. doi: 10.1179/136485908X337490 PubMed PMID: WOS:000260674900007. [DOI] [PubMed] [Google Scholar]
- 11.Verweij JJ, Stensvold CR. Molecular Testing for Clinical Diagnosis and Epidemiological Investigations of Intestinal Parasitic Infections. Clinical Microbiology Reviews. 2014;27(2):371–418. doi: 10.1128/CMR.00122-13 PubMed PMID: WOS:000334076500008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu J, Gratz J, Amour C, Kibiki G, Becker S, Janaki L, et al. A Laboratory-Developed TaqMan Array Card for Simultaneous Detection of 19 Enteropathogens. Journal of Clinical Microbiology. 2013;51(2):472–80. doi: 10.1128/JCM.02658-12 PubMed PMID: WOS:000314108000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stothard R, Verweij J, Cunningham L, Osei-Atweneboana M. Practical training in molecular DNA diagnostics 2016 [cited 2017]. Available from: https://countdownonntds.wordpress.com/2016/03/21/practical-training-in-molecular-dna-diagnostics/.
- 14.Cunningham L. Building links with polio surveillance in Ghana 2016 [cited 2017]. Available from: https://countdownonntds.wordpress.com/2016/04/25/building-links-with-polio-surveillance-in-ghana/.
- 15.Taniuchi M, Verweij JJ, Noor Z, Sobuz SU, van Lieshout L, Petri WA, et al. High Throughput Multiplex PCR and Probe-based Detection with Luminex Beads for Seven Intestinal Parasites. American Journal of Tropical Medicine and Hygiene. 2011;84(2):332–7. PubMed PMID: WOS:000287003900029. doi: 10.4269/ajtmh.2011.10-0461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verweij JJ, Canales M, Polman K, Ziem J, Brienen EAT, Polderman AM, et al. Molecular diagnosis of Strongyloides stercoralis in faecal samples using real-time PCR (vol 103, pg 342, 2009). Transactions of the Royal Society of Tropical Medicine and Hygiene. 2010;104(5):378–. doi: 10.1016/j.trstmh.2010.02.010. PubMed PMID: WOS:000277881200014. [DOI] [PubMed] [Google Scholar]
- 17.Niesters HGM. Clinical virology in real time. Journal of Clinical Virology. 2002;25:S3–S12. PubMed PMID: WOS:000179936400002. [DOI] [PubMed] [Google Scholar]
- 18.GIMP: GNU Image Manipulation Program [cited 2017]. Available from: https://www.gimp.org/.
- 19.Olsen A, van Lieshout L, Marti H, Polderman T, Polman K, Steinmann P, et al. Strongyloidiasis - the most neglected of the neglected tropical diseases? Transactions of the Royal Society of Tropical Medicine and Hygiene. 2009;103(10):967–72. doi: 10.1016/j.trstmh.2009.02.013 PubMed PMID: WOS:000273309300001. [DOI] [PubMed] [Google Scholar]
- 20.John D, Petri W. Markell and Voge's Medical Parasitology. 9th ed: Elsevier; 2006. [Google Scholar]
- 21.Thayer WS. On the Occurence of Strongyloides intestinalis in the United States. J Exp Med. 1901;6:75–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Genta RM. GLOBAL PREVALENCE OF STRONGYLOIDIASIS - CRITICAL-REVIEW WITH EPIDEMIOLOGIC INSIGHTS INTO THE PREVENTION OF DISSEMINATED DISEASE. Reviews of Infectious Diseases. 1989;11(5):755–67. PubMed PMID: WOS:A1989AU01000008. [DOI] [PubMed] [Google Scholar]
- 23.Jorgensen T, Montresor A, Savioli L. Effectively controlling strongyloidiasis. Parasitology Today. 1996;12(4):164–. doi: 10.1016/0169-4758(96)80806-4 PubMed PMID: WOS:A1996UB39600012. [DOI] [PubMed] [Google Scholar]
- 24.Bisoffi Z, Buonfrate D, Montresor A, Requena-Mendez A, Munoz J, Krolewiecki AJ, et al. Strongyloides stercoralis: A Plea for Action. Plos Neglected Tropical Diseases. 2013;7(5). doi: 10.1371/journal.pntd.0002214 PubMed PMID: WOS:000319994400019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Machicado JD, Marcos LA, Tello R, Canales M, Terashima A, Gotuzzo E. Diagnosis of soil-transmitted helminthiasis in an Amazonic community of Peru using multiple diagnostic techniques. Transactions of the Royal Society of Tropical Medicine and Hygiene. 2012;106(6):333–9. doi: 10.1016/j.trstmh.2012.03.004 PubMed PMID: WOS:000305854600002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.