Abstract
Objectives
To assess the morbidity associated with continuing the second-stage duration of labor, weighing the probability of spontaneous vaginal birth without morbidity compared with birth with serious maternal or neonatal complications.
Methods
In a retrospective cohort, we analyzed singleton, vertex births ≥ 36 weeks of gestation without prior cesarean (n=43,810 nulliparous and 59,605 multiparous women). We calculated rates of spontaneous vaginal birth and composite serious maternal or neonatal complications. Results were stratified by parity (nulliparous or multiparous) and epidural status (yes or no). Competing risks models were created for: 1) spontaneous vaginal birth with no morbidity; 2) birth with maternal or neonatal morbidity; and 3) no spontaneous vaginal birth and no morbidity, and our main interest was in comparing number 1 above against number 2.
Results
Rates of spontaneous vaginal birth without morbidity were slightly higher after the first half hour (>0.5 to 1.0 hour) for nulliparous women, after which rates decreased with increasing second-stage duration. For multiparous women, rates of spontaneous vaginal birth without morbidity decreased with increasing second-stage duration. For illustration, for a nulliparous woman with an epidural at 3.0 hours of second stage who extended by another 1.0 hour, her likelihood of delivering by spontaneous vaginal birth was 31.4% compared to her likelihood of birth with any serious complication in the next hour of 7.6%. The percent of cesareans for nonreassuring fetal heart rate tracing were higher for women without compared to with an epidural.
Conclusion
Rates of spontaneous vaginal birth without serious morbidity steadily decreased for increasing second-stage duration except for the first half hour for nulliparous women. We did not observe an inflection point at a particular hour mark for either spontaneous vaginal delivery without morbidity or births with morbidity. Our findings will assist in the decision making for extending second-stage duration.
Introduction
Prolonged second stage of labor beyond historical definitions is associated with high rates of successful vaginal birth but increased risks of maternal and neonatal morbidity.(1) Specifically, prolonging the second stage of labor is associated with increased maternal morbidity including postpartum hemorrhage, maternal febrile morbidity, infection and perineal trauma. There is also increased neonatal morbidity including increased rates of 5 minute Apgar score < 4 (except nulliparous women without an epidural), neonatal intensive care unit (NICU) admission, neonatal asphyxia in nulliparous women, and perinatal mortality for deliveries without an epidural; however, the overall absolute rates for both of these latter outcomes are low (<0.5%).(1)
In a workshop including the Society for Maternal-Fetal Medicine and ACOG to prevent the first cesarean birth, it was recommended that second-stage arrest could be defined after an additional hour: four and three hours for nulliparous women with and without an epidural, respectively, and three and two hours for multiparous women with and without an epidural, respectively.(2) Clinical counseling and decision making requires weighing the likelihood of achieving vaginal birth with the risks of complications that can occur with increasing second-stage duration. Information on the risks of specific durations for second stage of labor is currently lacking.(3, 4) The aim of our study was to calculate the likelihood of vaginal birth without serious maternal or neonatal morbidity or mortality versus birth with morbidity or mortality to assist in clinical decision making.
Materials and Methods
This was a retrospective analysis utilizing the data from the Consortium on Safe Labor (CSL). The CSL was a retrospective study of electronic medical records from 12 U.S. sites, 2002–2008, with a main study aim of determining the optimal time for operative birth during the course of labor to minimize maternal and neonatal complications.(5) Data were abstracted from the electronic medical record including demographic, medical, prenatal, antenatal and labor and birth and neonatal information, and supplemented with maternal and newborn discharge summaries. Validation of four important variables was performed with manual chart review, including cesarean birth for nonreassuring fetal heart rate tracing, asphyxia, NICU admission for respiratory conditions and shoulder dystocia. The electronic medical records were demonstrated to be highly accurate with >91% concordance for all subgroups and >95% for most.(5, 6) Institutional Review Board approval was obtained by all participating institutions.
In the current study analysis, we included all women who delivered a singleton, vertex, non-anomalous fetus ≥ 36 weeks of gestation. Women who had an antepartum stillbirth, prior uterine incision, or failed to reach the second stage of labor were excluded, for a total of n=43,810 nulliparous and 59,605 multiparous women remaining for present analysis. Details on the analytic cohort were previously published.(1)
Duration of the second stage of labor was calculated as the difference between the date and time of birth from the date and time of 10cm cervical dilation as recorded in the maternal medical record. Spontaneous vaginal birth was chosen as the reference group since operative vaginal and cesarean births are associated with increased maternal and neonatal morbidity.
When considering what would be the optimal duration of the second stage of labor, we considered any serious maternal or neonatal outcome as an event to be avoided. Therefore, an event was considered to have occurred if any of the outcomes were present. Maternal and neonatal outcomes were abstracted from the medical record. Composite maternal serious maternal complications included postpartum hemorrhage, blood transfusion, cesarean hysterectomy, intensive care unit (ICU) admission, or death. Composite neonatal serious complications included shoulder dystocia with fetal injury (clavicular fracture, Erb palsy, Klumpke palsy or hypoxic ischemic encephalopathy), need for continuous positive airway pressure (CPAP) resuscitation or higher, NICU length of stay > 72 hours, sepsis, pneumonia, hypoxic-ischemic encephalopathy or periventricular leukomalacia, seizure, intracranial hemorrhage or periventricular hemorrhage, asphyxia, or neonatal death.
Indications for cesarean birth were as recorded in the electronic medical record and mapped into predefined categories as previously described. (3)
The duration of second stage and rates of mode of birth (spontaneous vaginal, operative vaginal and cesarean birth) as well as rates of composite maternal and composite neonatal outcomes for deliveries were calculated for each parity (nulliparous or multiparous) and epidural status (yes or no). Rates were plotted for each 0.5-hour interval duration of second stage on bar graphs. The denominator included deliveries occurring during each 0.5-hour interval.
For remaining analyses, we estimated a composite complication for maternal and neonatal complications combined. We first estimated for a given duration of second stage of labor the additional probability that a woman would achieve a vaginal birth and how often morbidity occurred during a subsequent time interval of 0.5 hours with additional duration of second stage beyond a certain time point.
For analysis, we treated duration of second stage of labor as competing risks type of data. Competing risks event are said to be present when a patient is at risk of more than one mutually exclusive event, such as death from different causes, and the occurrence of one of these events will prevent any other event from ever happening. We considered the following three exclusive outcomes during the second stage of labor: 1) spontaneous vaginal birth without maternal or neonatal serious morbidity or mortality; 2) birth by any mode with any maternal or neonatal serious morbidity or mortality; 3) non-spontaneous vaginal birth (i.e. operative vaginal or cesarean birth) without any maternal or neonatal serious morbidity or mortality. Note that in our analysis, our main interest was in comparing the 1) spontaneous vaginal birth with no morbidity against 2) deliveries with any morbidity, so we combined operative vaginal or cesarean birth with no morbidity as one cause. This technique does not change our probabilities for the main objectives. For example, if one were interested in risk of cancer deaths against not dying from cancer, other causes of death would be combined. We estimated the probabilities of delivering by spontaneous vaginal birth without serious morbidity or mortality and probabilities of delivering by any mode with any serious morbidity or mortality, during the next 0.5-hour interval given that the woman had not delivered by the current time point) based on a competing risks framework defined earlier. These probabilities are calculated as ratio of the probability of a birth of specific cause occurring in the interval of interest with that of probability of woman at risk of delivering at the start of the time interval. These probabilities are based on cumulative incidence functions and overall survival probability (i.e. probability of a woman still at risk for birth).(7) Rates for additional intervals were also calculated.
Indications for cesarean birth were calculated for extending the second stage of birth by one hour past historical definitions of second-stage duration for parity and epidural status.
All analyses were implemented using SAS (version 9.4, SAS Institute, Inc., Cary, North Carolina) or R (version 3.1.2, http://www.R-project.org).
Results
Nulliparous women incurred a serious maternal complication in 7.0% of cases with an epidural and 5.0% without an epidural, while multiparous women incurred a serious maternal complication in 6.4% of cases with an epidural and 4.3% of cases without. (Table 1) The neonatal composite serious outcome occurred in 4.3% and 3.2% of nulliparous and 2.7% and 2.2% of multiparous women with and without an epidural, respectively.
Table 1.
Duration of second stage of labor and outcomes by parity and epidural status.
| Nulliparous With Epidural 35657 (81.4%)* |
Nulliparous Without Epidural 8153 (18.6%)* |
Multiparous With Epidural 43436 (72.9%)* |
Multiparous Without Epidural 16169 (27.1%)* |
|
|---|---|---|---|---|
| Duration, hours - median (10th, 90th percentile) | 1.1 (0.3,3.0) | 0.7 (0.2,2.4) | 0.3 (0.1,1.1) | 0.2 (0.03,0.7) |
| Maternal Morbidity or Death | ||||
| Maternal Composite † | 2,481 (7%) | 410 (5%) | 2,765 (6.4%) | 691 (4.3%) |
| Postpartum hemorrhage | 1,410 (4%) | 329 (4%) | 1,030 (2.4%) | 459 (2.8%) |
| Blood transfusion | 1,102 (3.1%) | 85 (1%) | 1,715 (3.9%) | 231 (1.4%) |
| Cesarean hysterectomy | 8 (0.02%) | 2 (0.02%) | 11 (0.03%) | 3 (0.02%) |
| ICU admission | 119 (0.3%) | 11 (0.1%) | 117 (0.3%) | 37 (0.2%) |
| Maternal death | 2 (0.006%) | 0 | 2 (0.005%) | 0 |
| Neonatal Morbidity or Death | ||||
| Neonatal Composite ‡ | 1,523 (4.3%) | 262 (3.2%) | 1155 (2.7%) | 353 (2.2%) |
| Shoulder dystocia with | 30 (0.1%) | 7 (0.1%) | 29 (0.1%) | 8 (0.05%) |
| fetal injury § | ||||
| Need for CPAP | 366 (1%) | 39 (0.5%) | 264 (0.6%) | 67 (0.4%) |
| resuscitation or higher | ||||
| NICU length of stay > 72 hours | 864 (2.4%) | 130 (1.6%) | 705 (1.6%) | 199 (1.2%) |
| Sepsis | 487 (1.4%) | 96 (1.2%) | 287 (0.7%) | 120 (0.7%) |
| Pneumonia | 255 (0.7%) | 39 (0.5%) | 198 (0.5%) | 51 (0.3%) |
| Hypoxic-ischemic encephalopathy or periventricular leukomalacia | 5 (0.01%) | 2 (0.02%) | 1 (0.002%) | 0 |
| Seizure | 39 (0.1%) | 4 (0.05%) | 17 (0.04%) | 8 (0.05%) |
| Intracranial hemorrhage or periventricular hemorrhage | 56 (0.2%) | 7 (0.1%) | 34 (0.1%) | 4 (0.02%) |
| Asphyxia | 58 (0.2%) | 12 (0.1%) | 41 (0.1%) | 11 (0.1%) |
| Neonatal death | 9 (0.03%) | 4 (0.05%) | 10 (0.02%) | 6 (0.04%) |
| Route of Delivery | ||||
| Spontaneous vaginal birth | 29529 (82.8%) | 7349 (90.1%) | 41421 (95.4%) | 15855 (98.1%) |
| Operative vaginal birth | 4748 (13.3%) | 613 (7.5%) | 1742 (4.0%) | 261 (1.6%) |
| Cesarean birth | 1380 (3.9%) | 191 (2.3%) | 273 (0.6%) | 53 (0.3%) |
Abbreviations: ICU, intensive care unit; CPAP, Continuous positive airway pressure; NICU, neonatal intensive care unit
Data are n (%) except where noted.
Maternal composite includes all individual maternal outcomes listed below.
Neonatal composite includes all individual neonatal outcomes listed below.
Fetal injury included clavicular fracture, Erb’s palsy, Klumpke’s palsy or hypoxic-ischemic encephalopathy
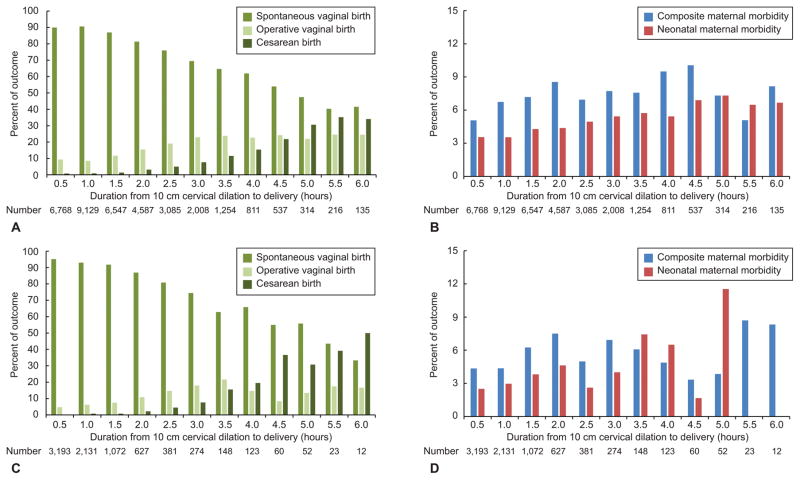
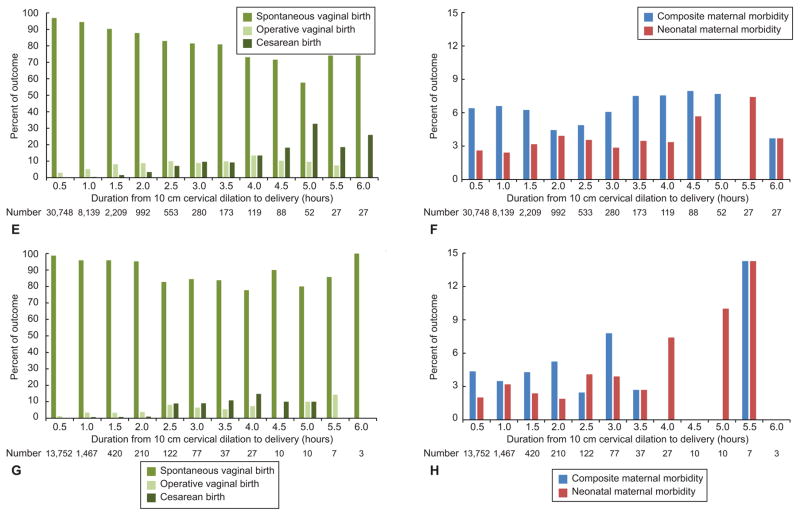
The empirical rates for mode of birth and maternal or neonatal morbidity or mortality for deliveries that occurred during each 0.5-hour interval of the second-stage duration are presented in Figure 1. Vaginal delivery rates were overall high, although decreased with increasing second-stage duration, a trend that was more variable for multiparous women. Neonatal morbidity or mortality rates increased and then levelled off for deliveries at > 4.0 to 4.5 hours for nulliparous women with an epidural. Each of the individual morbidity rates also tended to increase with increasing second-stage duration for nulliparous women without an epidural, indicating that the composite morbidity was not driven by any individual morbidity in particular (data not shown).
Figure 1.
Empirical rates of birth mode and morbidity or mortality. Nulliparous women with epidural (A–B), nulliparous women without epidural (C–D), multiparous women with epidural (E–F), and multiparous women without epidural (G–H). Rates per 0.5 hour interval for mode of birth (spontaneous vaginal birth, operative vaginal birth, or cesarean birth); composite serious maternal morbidity or mortality including postpartum hemorrhage, blood transfusion, cesarean hysterectomy, intensive care unit admission, or death; and composite serious neonatal morbidity or mortality including shoulder dystocia with fetal injury (clavicular fracture, Erb palsy, Klumpke palsy or hypoxic-ischemic encephalopathy), need for continuous positive airway pressure resuscitation or higher, neonatal intensive care unit length of stay >72 hours, sepsis, pneumonia, hypoxic-ischemic encephalopathy or periventricular leukomalacia, seizure, intracranial hemorrhage or periventricular hemorrhage, asphyxia, or neonatal death.
Neonatal morbidity or mortality rates varied with increasing duration for nulliparous women without an epidural and for multiparous women.
We considered three exclusive outcomes during the second stage of labor. The percentages of women delivering by spontaneous vaginal birth without serious morbidity or mortality versus the percentages of women delivering by any mode with any serious morbidity or mortality in the next 0.5-hour interval among all the women that have not delivered at a given time point are presented in Table 2. Rates of spontaneous vaginal birth without morbidity were slightly higher after the first half hour (>0.5 to 1.0 hour) for nulliparous women, after which rates decreased with increasing second-stage duration. For multiparous women, rates of spontaneous vaginal birth without morbidity decreased with increasing second-stage duration. The rates of births with a composite maternal or neonatal morbidity or mortality were variable with increasing second-stage duration, but not inconsequential ranging up to 5.6% for birth after >4.0 to 4.5 hours of second stage duration for nulliparous women with an epidural, and 5.3% for birth after >4.5 to 5.0 hours for nulliparous women without an epidural. For example, for nulliparous women with an epidural, given that a woman had not delivered in 3 hours, her likelihood of delivering with any serious morbidity or mortality in the next half hour was 4.4% compared to her likelihood of delivering by spontaneous vaginal birth without serious morbidity or mortality was 19.5%. For multiparous women, the percentages of births with morbidity were more varied, with the highest percentages in the first half hour of second stage (0 to 0.5 hours), and peaking again at 4.8% for birth after >4.0 to 4.5 hours of second stage duration for multiparous women with an epidural, and 5.0% for birth after >5.5 to 6.0 hours for multiparous women without an epidural.
Table 2.
Percentage of women delivering by spontaneous vaginal birth without serious morbidity or mortality vs. percentage of women delivering with any serious morbidity or mortality by half hour intervals, among women that have not delivered by the beginning of the interval, stratified by parity and epidural status.*
| Nulliparous With Epidural | Nulliparous Without Epidural | Multiparous With Epidural | Multiparous Without Epidural | |||||
|---|---|---|---|---|---|---|---|---|
| Duration of 2nd Stage (hours) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) |
| 0 to 0.5 | 15.6 | 1.6 | 34.1 | 2.6 | 60.1 | 6.0 | 73.4 | 5.0 |
| >0.5 to 1.0 | 25.2 | 3.1 | 36.0 | 2.9 | 50.9 | 5.2 | 50.4 | 3.6 |
| >1.0 to 1.5 | 25.0 | 3.6 | 30.3 | 3.6 | 38.1 | 4.2 | 37.4 | 2.8 |
| >1.5 to 2.0 | 24.3 | 4.2 | 26.7 | 4.0 | 33.3 | 3.3 | 33.7 | 2.7 |
| >2.0 to 2.5 | 23.5 | 4.0 | 25.0 | 2.4 | 29.6 | 3.1 | 29.8 | 2.4 |
| >2.5 to 3.0 | 21.7 | 4.5 | 23.9 | 3.9 | 25.1 | 2.9 | 28.8 | 3.9 |
| >3.0 to 3.5 | 19.5 | 4.4 | 17.2 | 4.1 | 23.1 | 3.4 | 24.8 | 1.6 |
| >3.5 to 4.0 | 18.6 | 5.0 | 22.4 | 4.2 | 21.6 | 3.2 | 22.4 | 2.2 |
| >4.0 to 4.5 | 16.3 | 5.6 | 15.2 | 1.4 | 22.8 | 4.8 | 15.4 | 0 |
| >4.5 to 5.0 | 13.4 | 4.5 | 16.7 | 5.3 | 18.0 | 2.5 | 14.5 | 2.1 |
| >5.0 to 5.5 | 12.3 | 3.8 | 9.5 | 2.1 | 18.0 | 1.9 | 15.6 | 2.6 |
| >5.5 to 6.0 | 12.5 | 4.6 | 5.5 | 1.4 | 22.6 | 2.5 | 73.4 | 5.0 |
For example, for nulliparous women with epidural, given that a woman had not delivered in 3 hours, her likelihood of delivering with any serious morbidity or mortality in the next half hour was 4.4% compared to her likelihood of delivering by spontaneous vaginal birth without serious morbidity or mortality was 19.5%.
Delivery by any mode; composite maternal morbidity or mortality included postpartum hemorrhage, blood transfusion, cesarean hysterectomy, endometritis, intensive care unit admission or death. Composite neonatal morbidity or mortality included shoulder dystocia with fetal injury (clavicular fracture, Erb’s palsy, Klumpke’s palsy or hypoxic-ischemic encephalopathy), 5-minute Apgar < 4, need for continuous positive airway pressure resuscitation or higher, NICU admission, sepsis, pneumonia, hypoxic-ischemic encephalopathy or periventricular leukomalacia, seizure, intracranial hemorrhage or periventricular hemorrhage, asphyxia, or neonatal death.
Ranges of intervals are also provided in Table 3. For example, for nulliparous women with an epidural, given that a woman had not delivered in 3 hours, her likelihood of delivering with any serious morbidity or mortality in one hour beyond historical definitions of second-stage duration (>3.0 to 4.0 hours) was 7.6% compared to her likelihood of delivering by spontaneous vaginal birth without serious morbidity or mortality of 31.4%. The rates for the previous hour (>2.0 to 3.0 hours) were 6.9% and 37.5%, respectively.
Table 3.
Percentage of women delivering by spontaneous vaginal birth without serious morbidity or mortality vs. percentage of women delivering with any serious morbidity or mortality by range intervals, among women that have not delivered by the beginning of the interval, stratified by parity and epidural status. *
| Nulliparous With Epidural | Nulliparous Without Epidural | Multiparous With Epidural | Multiparous Without Epidural | |||||
|---|---|---|---|---|---|---|---|---|
| Duration of 2nd Stage (hours) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) | Spontaneous Vaginal Birth without Morbidity (%) | Birth with Composite Maternal or Neonatal Morbidity or mortality† (%) |
| >1.0 to 2.0 | 41.2 | 6.4 | 46.9 | 6.1 | 55.1 | 5.9 | 55.9 | 4.3 |
| >2.0 to 3.0 | 37.5 | 6.9 | 40.9 | 5.0 | 44.8 | 4.8 | 47.6 | 4.8 |
| >3.0 to 4.0 | 31.4 | 7.6 | 32.6 | 7.0 | 37.5 | 5.6 | 40.7 | 3.2 |
| >3.0 to 5.0 | 41.7 | 11.1 | 44.2 | 9.2 | 52.9 | 8.5 | 53.5 | 4.0 |
| >3.0 to 6.0 | 45.3 | 12.3 | 46.8 | 9.8 | 59.5 | 9.2 | 60.6 | 4.8 |
| >4.0 to 5.0 | 24.8 | 8.4 | 27.0 | 5.2 | 34.4 | 6.4 | 27.4 | 1.7 |
| >4.0 to 6.0 | 33.3 | 11.3 | 33.2 | 6.6 | 49.1 | 8.0 | 42.5 | 3.4 |
| >5.0 to 6.0 | 20.5 | 6.8 | 13.7 | 3.1 | 34.9 | 3.8 | 23.2 | 2.6 |
For example, for nulliparous women with epidural, given that a woman had not delivered in 3 hours, her likelihood of delivering with any serious morbidity or mortality in the next hour was 7.6% compared to her likelihood of delivering by spontaneous vaginal birth without serious morbidity or mortality was 31.4%.
Delivery by any mode; composite maternal morbidity or mortality included postpartum hemorrhage, blood transfusion, cesarean hysterectomy, endometritis, intensive care unit admission or death. Composite neonatal morbidity or mortality included shoulder dystocia with fetal injury (clavicular fracture, Erb’s palsy, Klumpke’s palsy or hypoxic-ischemic encephalopathy), 5-minute Apgar < 4, need for continuous positive airway pressure resuscitation or higher, NICU admission, sepsis, pneumonia, hypoxic-ischemic encephalopathy or periventricular leukomalacia, seizure, intracranial hemorrhage or periventricular hemorrhage, asphyxia, or neonatal death.
Indications for cesarean birth were calculated for extending the second stage of labor by one hour past historical definitions of second-stage duration for parity and epidural status. (Table 4) The percent of cesarean births for non-reassuring fetal heart rate tracing for women without versus with an epidural were higher.
Table 4.
Indications for cesarean birth in one hour beyond historical definitions of second-stage duration by parity and epidural status*
| Nulliparous With Epidural >3.0 to 4.0 hours (n=270) | Nulliparous Without Epidural >2.0 to 3.0 hours (n=38) | Multiparous With Epidural >2.0 to 3.0 hours (n=65) | Multiparous Without Epidural >1.0 to 2.0 hours (n=5) | |
|---|---|---|---|---|
| Failure to progress or CPD b | 227 (84.1%) | 29 (76.3%) | 46 (70.8%) | 1 (20.0%) |
| Non-reassuring fetal heart rate tracing c | 24 (8.9%) | 8 (21.1%) | 9 (13.8%) | 4 (80.0%) |
| Other | 31 (11.5%) | 6 (15.8%) | 13 (20.0%) | 2 (40.0%) |
Abbreviations: CPD, cephalopelvic disproportion
Since more than one indication could have been listed, indications add up to > 100%.
Discussion
Spontaneous vaginal birth without morbidity was slightly higher after the first half hour (>0.5 to 1.0 hour) for nulliparous women, after which rates decreased with increasing second-stage duration, while rates steadily declined for multiparous women.. To assist in weighing the likelihood of vaginal birth against the risk of serious maternal or neonatal morbidity or mortality, we provide data on both the risks and likelihood of spontaneous vaginal birth without serious morbidity or mortality versus the percentages of women delivering by any mode with any serious morbidity or mortality for increasing the duration of second stage.
Our findings are somewhat difficult to put into the context of the literature since modeling the outcomes of delivery and morbidity or mortality jointly in a competing risks framework in the same model is novel. In addition, many prior studies were limited in their ability to study rare serious morbidity and mortality given fewer numbers. The recommendations for point at which to stop a second stage has changed over the recent years. Historically, maternal and neonatal risks have been considered to increase with a second stage beyond two hours and have been described with increasing duration in other studies.(3, 4, 8–16) Operative vaginal birth historically was considered as an option in cases with lack of continuing progress for two hours without regional anesthesia in nulliparous women and one hour in multiparous women, with allowance for an additional hour with regional anesthesia, in an older ACOG practice bulletin on operative vaginal birth from 2000 which since has been replaced in 2015 without mention of specific duration.(17) ACOG and SMFM have published an obstetric care consensus document acknowledging that while an absolute maximum duration of second stage is unknown, the diagnosis of second stage arrest should not be made until as at least three hours of pushing in nulliparous women and two hours of pushing in multiparous women, and allowing consideration of longer durations in women making progress to be determined on an individual basis.(18) These recommendations note the importance of progress with pushing which is distinct from whether active versus passive second stage may be associated with differences in maternal and neonatal outcomes and requires future study. In our study, we did not observe an inflection at a particular hour mark. The percentage of women having a spontaneous vaginal birth without serious maternal or neonatal morbidity steadily decreased regardless of parity or epidural status for increasing second-stage duration (except for the first half hour for nulliparous women), while the percentage of deliveries by any mode with a serious morbidity were variable but not inconsequential. Ultimately the willingness to accept a certain percent risk of morbidity to achieve vaginal birth is up to the woman and clinician.
The major strength of our study is the large numbers and multiple centers allowing investigation of rare serious morbidity and mortality. However, our study is limited by the retrospective nature of the data. The decision making for women who were allowed to have longer second-stage durations likely was complex and may have included a number of factors such as progression, maternal and neonatal status, clinician experience and the clinician-patient relationship. It is unclear how the interplay of these factors could have influenced the success of vaginal birth and rate of adverse outcomes. In addition, we did not have information on active versus delayed pushing. The generalizability of our findings might be slightly less given the increasing obesity in the United States since the original data collection. Data on long term maternal morbidity including incontinence and child neurological outcomes are also lacking.
Data to assist in decision making for extending the second stage of labor beyond the historical definitions of second-stage duration is limited. Additional factors such as progress in descent, station achieved, position of the head, estimated fetal weight, maternal fatigue, the presence of chorioamnionitis or meconium, and fetal heart tracing, are important to take into account when deciding on the length of the second stage for any individual patient. While we cannot make a recommendation for the optimal second-stage duration, our findings will assist clinicians and patients in the decision for weighing the likelihood of spontaneous vaginal birth with the risk of serious maternal and neonatal morbidity or mortality when considering continuing the duration of second stage.
Supplementary Material
Acknowledgments
Supported by the Intramural Research Program of the National Institutes of Health, Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). The Consortium on Safe Labor was funded by the Intramural Research Program of the NICHD, through Contract No. HHSN267200603425C.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal’s requirements for authorship.
For a list of institutions involved in the Consortium, see Appendix 1 online at http://links.lww.com/xxx.
Presented at the Annual Society for Maternal-Fetal Medicine Meeting, San Diego, CA, February 5, 2015 and the Annual Meeting of the Society for Pediatric and Perinatal Epidemiologic Research, Denver, CO, June 16, 2015.
References
- 1.Laughon SK, Berghella V, Reddy UM, Sundaram R, Lu Z, Hoffman MK. Neonatal and maternal outcomes with prolonged second stage of labor. Obstet Gynecol. 2014 Jul;124(1):57–67. doi: 10.1097/AOG.0000000000000278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Spong CY, Berghella V, Wenstrom KD, Mercer BM, Saade GR. Preventing the first cesarean delivery: summary of a joint Eunice Kennedy Shriver National Institute of Child Health and Human Development, Society for Maternal-Fetal Medicine, and American College of Obstetricians and Gynecologists Workshop. Obstet Gynecol. 2012 Nov;120(5):1181–93. doi: 10.1097/aog.0b013e3182704880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hamilton G. On mortality from the use of forceps. British and Foreign Med Chir Rev. 1853;11:511. [PMC free article] [PubMed] [Google Scholar]
- 4.Rouse DJ, Weiner SJ, Bloom SL, Varner MW, Spong CY, Ramin SM, et al. Second-stage labor duration in nulliparous women: relationship to maternal and perinatal outcomes. Am J Obstet Gynecol. 2009 Oct;201(4):357, e1–7. doi: 10.1016/j.ajog.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhang J, Troendle J, Reddy UM, Laughon SK, Branch DW, Burkman R, et al. Contemporary cesarean delivery practice in the United States. Am J Obstet Gynecol. 2010 Oct;203(4):326, e1–e10. doi: 10.1016/j.ajog.2010.06.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Graseck AS, Odibo AO, Tuuli M, Roehl KA, Macones GA, Cahill AG. Normal first stage of labor in women undergoing trial of labor after cesarean delivery. Obstet Gynecol. 2012 Apr;119(4):732–6. doi: 10.1097/AOG.0b013e31824c096c. [DOI] [PubMed] [Google Scholar]
- 7.Scrucca L, Santucci A, Aversa F. Competing risk analysis using R: an easy guide for clinicians. Bone marrow transplantation. 2007 Aug;40(4):381–7. doi: 10.1038/sj.bmt.1705727. [DOI] [PubMed] [Google Scholar]
- 8.Hellman LM, Prystowsky H. The duration of the second stage of labor. Am J Obstet Gynecol. 1952 Jun;63(6):1223–33. doi: 10.1016/s0002-9378(16)38916-5. [DOI] [PubMed] [Google Scholar]
- 9.Hamilton G. On the proper management of tedious labors. British and Foreign Med Chir Rev. 1871;48:449. [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen WR. Influence of the duration of second stage labor on perinatal outcome and puerperal morbidity. Obstet Gynecol. 1977 Mar;49(3):266–9. [PubMed] [Google Scholar]
- 11.Moon JM, Smith CV, Rayburn WF. Perinatal outcome after a prolonged second stage of labor. J Reprod Med. 1990 Mar;35(3):229–31. [PubMed] [Google Scholar]
- 12.Saunders NS, Paterson CM, Wadsworth J. Neonatal and maternal morbidity in relation to the length of the second stage of labour. Br J Obstet Gynaecol. 1992 May;99(5):381–5. doi: 10.1111/j.1471-0528.1992.tb13753.x. [DOI] [PubMed] [Google Scholar]
- 13.Menticoglou SM, Manning F, Harman C, Morrison I. Perinatal outcome in relation to second-stage duration. Am J Obstet Gynecol. 1995 Sep;173(3 Pt 1):906–12. doi: 10.1016/0002-9378(95)90364-x. [DOI] [PubMed] [Google Scholar]
- 14.Myles TD, Santolaya J. Maternal and neonatal outcomes in patients with a prolonged second stage of labor. Obstet Gynecol. 2003 Jul;102(1):52–8. doi: 10.1016/s0029-7844(03)00400-9. [DOI] [PubMed] [Google Scholar]
- 15.Cheng YW, Hopkins LM, Caughey AB. How long is too long: Does a prolonged second stage of labor in nulliparous women affect maternal and neonatal outcomes? Am J Obstet Gynecol. 2004 Sep;191(3):933–8. doi: 10.1016/j.ajog.2004.05.044. [DOI] [PubMed] [Google Scholar]
- 16.Allen VM, Baskett TF, O’Connell CM, McKeen D, Allen AC. Maternal and perinatal outcomes with increasing duration of the second stage of labor. Obstet Gynecol. 2009 Jun;113(6):1248–58. doi: 10.1097/AOG.0b013e3181a722d6. [DOI] [PubMed] [Google Scholar]
- 17.Operative vaginal delivery. American College of Obstetricians and Gynecoloists. Practice Bulletin No. 154. Obstet Gynecol. 2015;126:e56–65. doi: 10.1097/AOG.0000000000001147. [DOI] [PubMed] [Google Scholar]
- 18.National Institutes of Health Consensus Development conference statement: vaginal birth after cesarean: new insights March 8–10, 2010. Obstet Gynecol. 2010 Jun;115(6):1279–95. doi: 10.1097/AOG.0b013e3181e459e5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.