Abstract
Objective
To assess the relationships between self-reported psychosocial stress and preterm birth, hypertensive disease of pregnancy, and small-for-gestational-age birth, and to assess the extent to which these relationships account for racial and ethnic disparities in these adverse outcomes.
Methods
Self-reported measures of psychosocial stress (perceived stress, depression, racism, anxiety, resilience, and social support) were collected during pregnancy among a racially and ethnically diverse cohort of women enrolled in a prospective observational study of nulliparous women with singleton pregnancies, from eight clinical sites across the United States, between October 2010 and May 2014. The associations of preterm birth, hypertensive disease of pregnancy, and small-for-gestational-age birth with the self-reported measures of psychosocial stress as well as with race and ethnicity were evaluated.
Results
The study included 9470 women (60.4% non-Hispanic white, 13.8% non-Hispanic black, 16.7% Hispanic, 4.0% Asian, and 5.0% other). Non-Hispanic black women were significantly more likely to experience any preterm birth, hypertensive disease of pregnancy, and small-for-gestational-age birth than were non-Hispanic white women (12.3 vs. 8.1%, 16.7% vs. 13.4%, and 17.2% vs. 8.6%, respectively; P < .05 for all). After adjusting for potentially confounding factors, including the six different psychosocial factors singly and in combination, non-Hispanic black women continued to be at greater risk for any preterm birth and small-for-gestational-age birth compared to non-Hispanic white women.
Conclusion
Among a large and geographically diverse cohort of nulliparous women with singleton gestations, non-Hispanic black women are most likely to experience preterm birth, hypertensive disease of pregnancy, and small-for-gestational-age birth. These disparities were not materially altered for preterm birth or small-for-gestational-age birth by adjustment for demographic differences, and did not appear to be explained by differences in self-reported psychosocial factors.
Introduction
Preterm birth remains a major public health problem, responsible for a large proportion of short- and long-term morbidity among newborns and for tens of billions of dollars a year in healthcare costs in the United States.1 Over decades, there has been little reduction in the frequency of preterm birth.2 Equally recalcitrant to reduction has been the racial disparity in preterm birth. Specifically, non-Hispanic black women have rates of preterm birth that are more than fifty percent higher than non-Hispanic white women.3
The reasons for this racial disparity remain uncertain, although social determinants of health have been proposed as one likely etiology.4 For example, women from households with lower incomes have a greater frequency of adverse pregnancy outcomes, including preterm birth.5 Such socio-demographic metrics, however, do not fully explain the observed difference in outcomes related to race; non-Hispanic black women remain at greater risk of preterm birth than their white counterparts even after accounting for income status.6 Similarly, attempts to adjust for other socio-demographic differences have not explained the observed racial disparity.
It is possible that measures such as income do not adequately capture differences in the environment that are experienced by women of different races and ethnicities. For example, black women are more likely to have more perceived stress, more depressive symptoms, and less social support than white women, regardless of income.7 Given the potential relationship between psychosocial stress and preterm birth, a disparity in the former may be at the root of the disparity in the latter.8 The objective of this analysis was to assess the relationships between self-reported psychosocial stress and preterm birth, and to assess to what extent this relationship accounts for racial and ethnic disparities in preterm birth, among a large cohort of prospectively evaluated nulliparous women.
Materials and Methods
The “Nulliparous Pregnancy Outcomes Study: monitoring mothers-to-be (nuMoM2b)” is a prospective cohort study in which 10,038 nulliparous women with singleton pregnancies were enrolled from geographically-diverse hospitals affiliated with 8 clinical centers. Full details of the study protocol have been published previously.9 In brief, women were eligible for enrollment if they had a viable singleton gestation, had no previous pregnancy that lasted more than 20 weeks of gestation, and were between 6 weeks 0 days’ gestation and 13 weeks 6 days’ gestation at recruitment. Exclusion criteria were: maternal age less than 13 years, history of 3 or more spontaneous abortions, current pregnancy complicated by a suspected fatal fetal malformation, known fetal aneuploidy, assisted reproduction with a donor oocyte, multifetal reduction, or plan to terminate the pregnancy. Patients also were excluded if they were already participating in an intervention study anticipated to influence pertinent maternal or fetal outcomes, were previously enrolled in the nuMoM2b study, or were unable to provide informed consent. A common protocol and manual of operations were used for all aspects of the study. Each site’s local governing Institutional Review Board approved the study and all women provided informed written consent prior to participation.
Participant data were collected by trained research personnel during three antepartum study visits. These visits were scheduled to occur between 6 weeks 0 days’ and 13 weeks 6 days’ gestation (Visit 1), 16 weeks 0 days’ and 21 weeks 6 days’ gestation (Visit 2), and 22 weeks 0 days’ and 29 weeks 6 days’ gestation (Visit 3). A woman’s self-identified race and ethnicity was categorized as non-Hispanic white, non-Hispanic black, Hispanic, Asian or “other”. Interviews at the visits included assessments of psychosocial factors, which were chosen to represent different domains of experience (e.g., perceived stress, social support, resilience). The assessments used in this analysis were as follows: Cohen’s 10-item Perceived Stress Scale (PSS)10 at visit 1; the trait subscale of the Spielberger State-Trait Anxiety Inventory (STAI-T)11 at visit 1; the Connor-Davidson Resilience Scale (CD-RISC)12 at visit 2; the Multi-Dimensional Scale of Perceived Social Support (MSS) at visit 113; the Krieger Racism Scale at visit 214; and the Edinburgh Postnatal Depression Scale (EPDS)15 at visit 1. These instruments are psychometrically valid for women of different race and ethnicity in this study population, and differences in the assessments according to race and ethnicity have been described previously.7,16 At least 30 days after delivery, trained and certified chart abstractors reviewed the medical records of all participants and recorded final birth outcomes.
The outcomes assessed in this analysis included preterm birth of a liveborn or stillborn infant for any cause between 20 weeks 0 days and 36 weeks 6 days of gestation, hypertensive disease of pregnancy and small-for-gestational age birth (<10th percentile birth per the Alexander curve17). Spontaneous preterm birth was defined as delivery that occurred subsequent to spontaneous onset of preterm labor or premature rupture of the membranes. Medically-indicated preterm birth was defined as preterm delivery after induction or cesarean delivery without labor. Hypertensive disease of pregnancy was considered to have occurred in the presence of antepartum gestational hypertension, or antepartum, intrapartum, or postpartum preeclampsia or eclampsia.
The analysis was performed using a series of multivariable logistic regression equations with each selected adverse pregnancy outcome as the dependent variable. For each outcome, in model 1, race-ethnicity was the only independent (predictor) variable, while in model 2, the covariates of maternal age, pre-pregnancy body mass index (BMI), smoking, and medical co-morbidities (an indicator variable for any of the following: diabetes mellitus, chronic hypertension, asthma and kidney disease) were added to the equation. Socio-economic indicators were not included in these models given the potential for collision bias with the main dependent (adverse pregnancy outcome) and exposure (stress) variables. In a final step, each model had a single psychosocial measure (e.g., PSS score) added to the covariates in model 2 in order to evaluate (1) whether there was a significant association between the scores of the particular psychosocial measure and the adverse pregnancy outcome and (2) whether addition of that measure substantially changed the magnitude of the odds ratios associated with race-ethnicity. Each psychosocial measure was entered as a dichotomous variable based on cutoffs chosen a priori. Most often, a quartile cut-point for the score was selected that reflected the quartile of those with the greatest psychosocial burden (e.g., the greatest perceived stress or the least social support).7 For the Edinburgh Depression survey, a participant was categorized according to whether her score was at least 10 or whether she admitted to suicidal ideation given that this threshold and response, respectively, indicate an increased risk of clinical depression. For the Krieger Racism instrument, because the upper 75th percentile for the population was a score of 0, a score of 3 or more (i.e., 6.6% of the population) was used to define those with the greatest perceived exposure to racism.7
Given the potential that consideration of all scores at once, rather than one at a time, would more adequately reflect a woman’s psychosocial milieu, we also used latent profile analysis to discern groups of women with similar patterns of responses to the set of psychosocial assessments. The group assignment variable resulting from the latent profile analysis was added to the model 2 covariates, as had been done with the individual scores. The latent profile analyses were conducted using Mplus software version 7.4.18 The most appropriate number of classes (profiles) was determined based on model fit indices, including the Akaike information criteria (AIC) and sample size-adjusted Bayesian information criteria (BIC), as well as the Vuong-Lo-Mendell-Rubin and bootstrapped likelihood ratio tests to assess improvement in fit with inclusion of an additional class.19–21
Logistic regression equations were used to estimate odds ratios and 95% confidence intervals. A p value < .05 was used to define statistical significance and all tests were two-tailed. No correction was made for multiple comparisons. Analyses were conducted using SAS/STAT software, version 9.3 or higher (SAS Institute Inc., Cary, NC, USA).
Results
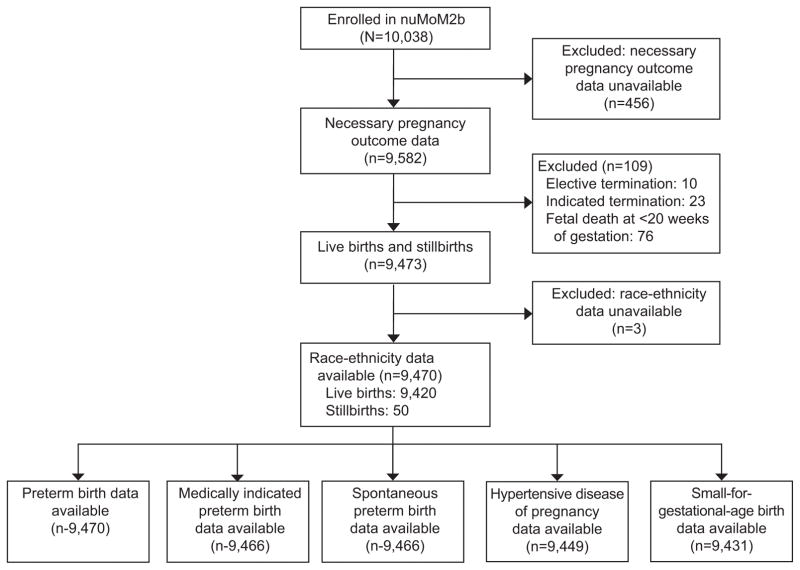
Of the 10,038 women enrolled in this prospective cohort, 9,470 were eligible for the present analysis (figure 1). Among eligible women, 5,721 (60.4%) were non-Hispanic white, 1,307 (13.8%) were non-Hispanic black, 1,586 (16.7%) were Hispanic, 379 (4.0%) were Asian, and 477 (5.0%) were of another race or ethnicity.
Figure 1.
Flow diagram for enrollment and inclusion in analysis
Frequencies of preterm birth (overall, medically-indicated, and spontaneous), hypertensive disease of pregnancy, and small-for-gestational-age birth are presented in table 1. All adverse pregnancy outcomes were most common among non-Hispanic black women, who were significantly more likely to experience these outcomes compared to non-Hispanic white women (Table 2, model 1). Hispanic women and Asian women were less likely to experience hypertensive disease of pregnancy than non-Hispanic white women, and all groups were more likely to have a small-for-gestational-age birth than non-Hispanic white women.
Table 1.
Frequencies of adverse pregnancy outcomes according to race-ethnicity
| Race-Ethnicity | Adverse Pregnancy Outcome | ||||
|---|---|---|---|---|---|
| Any PTB | iPTB | sPTB | HDP | SGA | |
| NHW | 464/5,721 (8.1) | 185/5,720 (3.2) | 274/5,720 (4.8) | 764/5,712 (13.4) | 490/5,702 (8.6) |
| NHB | 161/1,307 (12.3) | 76/1,306 (5.8) | 83/1,306 (6.4) | 218/1,304 (16.7) | 223/1,296 (17.2) |
| Hispanic | 128/1,586 (8.1) | 51/1,584 (3.2) | 75/1,584 (4.7) | 167/1,579 (10.6) | 185/1,580 (11.7) |
| Asian | 24/379 (6.3) | 8/379 (2.1) | 16/379 (4.2) | 32/378 (8.5) | 62/379 (16.4) |
| Other | 47/477 (9.9) | 18/477 (3.8) | 29/477 (6.1) | 63/476 (13.2) | 57/474 (12.0) |
Data presented as n/N (%); denominators may differ among columns due to missing data
PTB = preterm birth; iPTB = medically-indicated preterm birth; sPTB = spontaneous preterm birth; HDP = hypertensive disease of pregnancy; SGA = small-for-gestational-age birth; NHW = non-Hispanic white; NHB = non-Hispanic black
Table 2.
Association (odds ratio and 95% confidence interval) of race-ethnicity with adverse pregnancy outcomes in logistic regression models
| Race-Ethnicity | Adverse Pregnancy Outcome | ||||
|---|---|---|---|---|---|
| Any PTB | iPTB | sPTB | HDP | SGA | |
| MODEL 1 | |||||
| N = | 9,470 | 9,466 | 9,466 | 9,449 | 9,431 |
| NHB vs. NHW | 1.60 (1.32, 1.93) | 1.85 (1.41, 2.43) | 1.35 (1.05, 1.74) | 1.30 (1.10, 1.53) | 2.21 (1.86, 2.62) |
| Hispanic vs. NHW | 1.00 (0.82, 1.23) | 1.00 (0.73, 1.36) | 0.99 (0.76, 1.28) | 0.77 (0.64, 0.91) | 1.41 (1.18, 1.69) |
| Asian vs. NHW | 0.77 (0.51, 1.18) | 0.65 (0.32, 1.32) | 0.88 (0.52, 1.47) | 0.60 (0.41, 0.87) | 2.08 (1.56, 2.77) |
| Other vs. NHW | 1.25 (0.91, 1.71) | 1.17 (0.72, 1.92) | 1.29 (0.87, 1.91) | 0.99 (0.75, 1.30) | 1.45 (1.09, 1.95) |
| MODEL 2 | |||||
| N = | 9,233 | 9,231 | 9,231 | 9,231 | 9,199 |
| NHB vs. NHW | 1.31 (1.06, 1.63) | 1.28 (0.94, 1.74) | 1.30 (0.98, 1.72) | 0.95 (0.79, 1.14) | 2.08 (1.72, 2.52) |
| Hispanic vs. NHW | 0.94 (0.75, 1.17) | 0.84 (0.59, 1.18) | 0.99 (0.75, 1.31) | 0.69 (0.57, 0.83) | 1.44 (1.19, 1.75) |
| Asian vs. NHW | 0.87 (0.57, 1.34) | 0.84 (0.41, 1.73) | 0.89 (0.53, 1.50) | 0.78 (0.54, 1.14) | 2.07 (1.54, 2.79) |
| Other vs. NHW | 1.10 (0.80, 1.53) | 0.95 (0.57, 1.58) | 1.21 (0.81, 1.82) | 0.82 (0.61, 1.09) | 1.36 (1.01, 1.84) |
Model 1 – no covariates other than race and ethnicity (referent non-Hispanic white)
Model 2 – adjustment for maternal age, body mass index, smoking, and medical co-morbidities
PTB = preterm birth; iPTB = medically-indicated preterm birth; sPTB = spontaneous preterm birth; HDP=hypertensive disease of pregnancy; SGA = small-for-gestational-age birth; NHB = non-Hispanic black; NHW = non-Hispanic white
Denominators may differ among columns due to missing data; odds ratios significant at the p < .05 level presented in bold
After adjusting for potentially confounding factors (Table 2, model 2), some of the associations of race and ethnicity with adverse pregnancy outcomes were attenuated, with the greatest reduction in risk for medically-indicated preterm birth among non-Hispanic black women. However, non-Hispanic black women continued to be at greater risk for any category of preterm birth and women in all other race-ethnicity categories continued to be at greater risk of small-for-gestational-age birth compared to non-Hispanic white women.
When each psychosocial measure was added separately as a covariate to the model 2 covariates (Table 3), two notable findings were evident. First, in no case did the entry of a score from a psychosocial measure materially alter the observed association between race-ethnicity and adverse pregnancy outcome. Second, with the exception of perceived social support, there was no evidence that scores indicating greater psychosocial burden were independently associated with any of the adverse pregnancy outcomes. In the case of social support, women with scores indicating the least social support had statistically greater odds of any preterm birth, medically-indicated preterm birth, and small-for-gestational-age birth, although the magnitudes of association were small and the 95% confidence intervals on the odds ratios barely averted crossing 1.
Table 3.
Association (adjusted odds ratio and 95% confidence interval) of race-ethnicity and psychosocial measures with adverse pregnancy outcomes in multivariable models that include maternal age, body mass index, smoking, medical co-morbidities, race/ethnicity and the indicated psychosocial measure.
| Covariate | Adverse Pregnancy Outcome | ||||
|---|---|---|---|---|---|
| Any PTB | iPTB | sPTB | HDP | SGA | |
| Psychosocial measure = Edinburgh postnatal depression scale (EPDS) | |||||
| N = | 8,964 | 8,962 | 8,962 | 8,962 | 8,931 |
| NHB vs. NHW | 1.32 (1.06, 1.64) | 1.33 (0.97, 1.82) | 1.27 (0.95, 1.69) | 0.98 (0.81, 1.18) | 2.08 (1.71, 2.54) |
| Hispanic vs. NHW | 0.93 (0.74, 1.16) | 0.84 (0.60, 1.19) | 0.96 (0.72, 1.28) | 0.68 (0.56, 0.83) | 1.44 (1.19, 1.75) |
| Asian vs. NHW | 0.90 (0.58, 1.38) | 0.87 (0.42, 1.79) | 0.91 (0.54, 1.53) | 0.77 (0.53, 1.13) | 2.10 (1.56, 2.83) |
| Other vs. NHW | 1.12 (0.80, 1.55) | 0.99 (0.60, 1.64) | 1.20 (0.79, 1.82) | 0.84 (0.62, 1.12) | 1.31 (0.96, 1.78) |
| EPDS ≥ 10 or suicide ideation | 1.11 (0.92, 1.34) | 0.92 (0.69, 1.23) | 1.25 (0.99, 1.58) | 0.91 (0.77, 1.07) | 0.81 (0.67, 0.97) |
| Psychosocial measure = Krieger racism scale (Krieger) | |||||
| N = | 8,928 | 8,926 | 8,926 | 8,926 | 8,896 |
| NHB vs. NHW | 1.31 (1.04, 1.64) | 1.39 (1.00, 1.93) | 1.21 (0.90, 1.63) | 0.98 (0.81, 1.20) | 2.07 (1.69, 2.53) |
| Hispanic vs. NHW | 0.95 (0.76, 1.20) | 0.93 (0.65, 1.33) | 0.95 (0.71, 1.27) | 0.71 (0.58, 0.86) | 1.45 (1.19, 1.77) |
| Asian vs. NHW | 0.87 (0.56, 1.36) | 0.80 (0.37, 1.74) | 0.91 (0.54, 1.53) | 0.82 (0.56, 1.20) | 2.08 (1.54, 2.81) |
| Other vs. NHW | 1.14 (0.82, 1.59) | 1.00 (0.59, 1.68) | 1.23 (0.81, 1.85) | 0.85 (0.63, 1.14) | 1.42 (1.05, 1.93) |
| Krieger > 3 | 0.91 (0.67, 1.23) | 0.63 (0.38, 1.04) | 1.14 (0.78, 1.65) | 0.81 (0.62, 1.06) | 1.01 (0.78, 1.31) |
| Psychosocial measure = Perceived stress scale (PSS) | |||||
| N = | 9,191 | 9,189 | 9,189 | 9,189 | 9,157 |
| NHB vs. NHW | 1.31 (1.05, 1.62) | 1.27 (0.93, 1.73) | 1.30 (0.98, 1.72) | 0.95 (0.79, 1.14) | 2.08 (1.72, 2.53) |
| Hispanic vs. NHW | 0.94 (0.76, 1.17) | 0.84 (0.59, 1.18) | 1.00 (0.75, 1.32) | 0.69 (0.57, 0.83) | 1.44 (1.19, 1.75) |
| Asian vs. NHW | 0.86 (0.56, 1.33) | 0.83 (0.40, 1.72) | 0.88 (0.52, 1.49) | 0.79 (0.54, 1.15) | 2.08 (1.54, 2.79) |
| Other vs. NHW | 1.11 (0.80, 1.54) | 0.95 (0.57, 1.58) | 1.22 (0.81, 1.83) | 0.82 (0.62, 1.10) | 1.36 (1.01, 1.85) |
| PSS | 1.07 (0.91, 1.27) | 1.02 (0.80, 1.32) | 1.10 (0.88, 1.36) | 0.99 (0.86, 1.14) | 1.00 (0.86, 1.16) |
| Psychosocial measure = Spielberger State-Trait Anxiety inventory (STAI-T) | |||||
| N = | 8,178 | 8,177 | 8,177 | 8,177 | 8,150 |
| NHB vs. NHW | 1.39 (1.09, 1.76) | 1.36 (0.96, 1.92) | 1.36 (0.99, 1.86) | 1.01 (0.82, 1.24) | 2.12 (1.71, 2.63) |
| Hispanic vs. NHW | 0.91 (0.71, 1.16) | 0.78 (0.53, 1.15) | 0.99 (0.73, 1.34) | 0.65 (0.53, 0.79) | 1.51 (1.23, 1.85) |
| Asian vs. NHW | 0.65 (0.38, 1.10) | 0.64 (0.26, 1.57) | 0.66 (0.35, 1.27) | 0.74 (0.49, 1.11) | 2.02 (1.47, 2.78) |
| Other vs. NHW | 1.22 (0.86, 1.72) | 0.99 (0.57, 1.73) | 1.36 (0.89, 2.08) | 0.84 (0.62, 1.15) | 1.43 (1.04, 1.97) |
| STAI-T | 1.08 (0.90, 1.29) | 0.94 (0.71, 1.24) | 1.16 (0.93, 1.46) | 0.93 (0.80, 1.08) | 0.88 (0.74, 1.03) |
| Psychosocial measure = Multidimensional perceived social support scale (MSS) | |||||
| N = | 8,209 | 8,208 | 8,208 | 8,208 | 8,181 |
| NHB vs. NHW | 1.35 (1.06, 1.72) | 1.28 (0.90, 1.82) | 1.36 (0.99, 1.86) | 0.99 (0.80, 1.21) | 2.06 (1.67, 2.55) |
| Hispanic vs. NHW | 0.92 (0.72, 1.17) | 0.78 (0.53, 1.15) | 1.01 (0.75, 1.37) | 0.65 (0.53, 0.80) | 1.50 (1.22, 1.83) |
| Asian vs. NHW | 0.67 (0.40, 1.13) | 0.74 (0.32, 1.70) | 0.64 (0.34, 1.23) | 0.75 (0.50, 1.13) | 2.02 (1.48, 2.76) |
| Other vs. NHW | 1.18 (0.83, 1.67) | 0.97 (0.56, 1.69) | 1.31 (0.85, 2.02) | 0.84 (0.62, 1.15) | 1.43 (1.04, 1.96) |
| MSS | 1.21 (1.01, 1.44) | 1.37 (1.05, 1.78) | 1.08 (0.86, 1.36) | 1.15 (0.99, 1.33) | 1.20 (1.03, 1.40) |
| Psychosocial measure = Connor-Davidson resilience scale (CD-RISC) | |||||
| N = | 8,735 | 8,733 | 8,733 | 8,734 | 8,705 |
| NHB vs. NHW | 1.30 (1.04, 1.63) | 1.27 (0.92, 1.76) | 1.29 (0.96, 1.73) | 0.93 (0.77, 1.13) | 2.10 (1.72, 2.56) |
| Hispanic vs. NHW | 0.89 (0.70, 1.12) | 0.86 (0.60, 1.23) | 0.88 (0.65, 1.20) | 0.67 (0.55, 0.82) | 1.44 (1.18, 1.76) |
| Asian vs. NHW | 0.82 (0.53, 1.29) | 0.76 (0.35, 1.64) | 0.86 (0.50, 1.48) | 0.81 (0.55, 1.18) | 2.05 (1.51, 2.78) |
| Other vs. NHW | 1.15 (0.83, 1.60) | 0.95 (0.56, 1.60) | 1.30 (0.86, 1.95) | 0.82 (0.61, 1.10) | 1.43 (1.06, 1.95) |
| CD-RISC | 1.05 (0.89, 1.25) | 0.91 (0.70, 1.19) | 1.15 (0.92, 1.42) | 0.98 (0.85, 1.13) | 1.10 (0.94, 1.29) |
| Psychosocial measure = Groups derived from latent profile analysis | |||||
| N = | 9,233 | 9,231 | 9,231 | 9,231 | 9,199 |
| NHB vs. NHW | 1.31 (1.06, 1.63) | 1.35 (0.99, 1.85) | 1.25 (0.94, 1.67) | 0.98 (0.81, 1.19) | 2.07 (1.70, 2.51) |
| Hispanic vs. NHW | 0.94 (0.75, 1.17) | 0.87 (0.62, 1.23) | 0.97 (0.73, 1.28) | 0.70 (0.58, 0.85) | 1.43 (1.18, 1.74) |
| Asian vs. NHW | 0.87 (0.57, 1.34) | 0.88 (0.43, 1.82) | 0.86 (0.51, 1.45) | 0.81 (0.55, 1.18) | 2.05 (1.53, 2.77) |
| Other vs. NHW | 1.11 (0.80, 1.54) | 0.99 (0.59, 1.64) | 1.18 (0.78, 1.78) | 0.84 (0.62, 1.12) | 1.35 (1.00, 1.83) |
| Group 1 vs. 3 | 1.28 (0.87, 1.89) | 1.46 (0.86, 2.48) | 1.10 (0.65, 1.88) | 1.13 (0.81, 1.58) | 1.02 (0.70, 1.50) |
| Group 2 vs. 3 | 1.11 (0.93, 1.32) | 0.95 (0.73, 1.25) | 1.20 (0.96, 1.51) | 0.90 (0.77, 1.05) | 1.05 (0.90, 1.24) |
| Group 4 vs. 3 | 0.97 (0.71, 1.33) | 0.64 (0.38, 1.08) | 1.24 (0.85, 1.82) | 0.78 (0.59, 1.03) | 1.05 (0.81, 1.38) |
PTB = preterm birth; iPTB = medically-indicated preterm birth; sPTB = spontaneous preterm birth; HDP = hypertensive disease of pregnancy; SGA = small-for-gestational-age birth; NHB = non-Hispanic black; NHW = non-Hispanic white
All psychosocial instrument covariates represent women with a score in the quartile most associated with psychosocial burden (with referent = women with scores in the other three quartiles) unless otherwise indicated.
Denominators may differ among columns due to missing data; odds ratios significant at the p < .05 level presented in bold
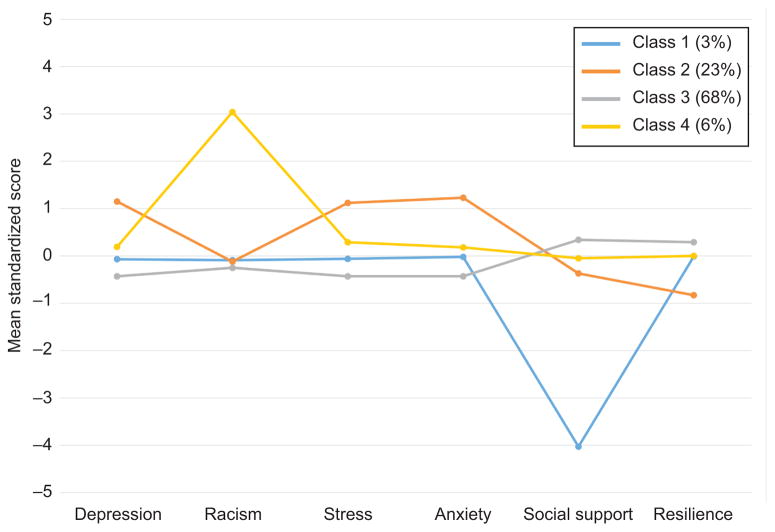
Lastly, a latent profile analysis was conducted to identify groups of women with similar patterns in scores across psychosocial measures. This analysis identified 4 groups of women (figure 2). Those in class 1 (3% of sample) had average scores on all measures except for very low scores on social support. Those in class 2 (23% of sample) had the highest levels of depression, stress, and anxiety and the lowest resilience. Those in class 3, who represented the majority (68%) of the sample, had slightly below average values for depressive symptoms, racism, stress, and anxiety, and slightly above average values for social support and resilience. Finally, those in class 4 (6% of sample) had average values on all measures except for very high values for the racism instrument. Addition of these classes into the multivariable equation (table 3), yielded no significant associations between class and any adverse pregnancy outcome.
Figure 2.
Patterns of response to psychosocial assessments using latent profile analysis
Discussion
Among a large and geographically diverse cohort of nulliparous women, we have found that non-Hispanic black women are most likely to experience adverse pregnancy outcomes such as preterm birth, hypertensive disease of pregnancy, and small-for-gestational-age birth. The evident disparity between non-Hispanic black and white women was not materially altered for all preterm birth or small-for-gestational-age birth by adjustment for demographic differences, such as maternal age and pre-pregnancy body mass index. Moreover, it did not appear to be explained by differences in self-reported psychosocial factors, such as those related to perceived stress, depression, racism, or social support. Also, the covariates representing these psychosocial factors largely were not significantly associated with higher odds of the adverse pregnancy outcomes. Perceived social support was the one exception, with the perception of low support being associated with all preterm birth, iatrogenic preterm birth, and small-for-gestational-age birth, although the magnitude of this association was very weak.
The etiology of the persistent racial and ethnic disparities in adverse pregnancy outcomes remains uncertain, although an origin related to social determinants of health has been considered to have biologic plausibility.8 There is some evidence that differences in social circumstances can translate into physiologic differences that could adversely affect pregnancy. For example, chronic exposure to stress has been related to derangements in the hypothalamic-pituitary axis and the immune system that can affect placental function and pregnancy maintenance.22–24
Yet, the specific exposure, or set of exposures, most related to – and potentially responsible for – adverse pregnancy outcomes has not been established. Because the racial and ethnic disparity in adverse pregnancy outcomes is not solely related to disparities in income, investigators have focused upon types of psychosocial burdens that transcend financial deprivation. For example, nulliparous non-Hispanic black women, regardless of income, were more likely to have a higher psychosocial burden score on all of the measures utilized in this study.7 Yet, studies have not demonstrated a consistent relationship between self-reported measures of these psychosocial burden and adverse pregnancy outcomes, or that these measures account for the observed racial-ethnic disparities.6,25
Several reasons for the inconsistency in outcomes have been postulated, including that different studies have used different instruments to quantify the exposure, that single scores may not adequately represent a woman’s psychosocial milieu, and that the sample sizes or the extent of data collection have not been adequate.25 In the present study, we attempted to overcome these limitations. In this study, we prospectively enrolled over 10,000 women and used trained research staff to collect both exposure and outcome data using a detailed and consistent protocol. Multiple instruments, representing a variety of domains related to psychosocial status, were evaluated singly and in combination in an effort to better represent the totality of the psychosocial environment.
Despite these approaches, we were largely unable to detect significant relationships or strong associations between measures of psychosocial status and more frequent adverse pregnancy outcomes, or demonstrate that these measures alter the association between race-ethnicity and adverse pregnancy outcomes. It cannot be known whether the investigation of other populations or the use of other self-reported measures might yield different results. Also, because individual subgroups were relatively small, the possibility of that actual differences exist but were undetected cannot be dismissed. And, our study results do not preclude a contribution of the social environment to health or pregnancy outcomes. These results do, however, suggest that the exact nature of that relationship and the most relevant exposures remain uncertain and require further elucidation. Mechanistic considerations aside, the results also demonstrate that it is unlikely that attempts at developing models for prediction of adverse pregnancy outcomes will benefit from inclusion of results from instruments such as those included in the present analysis.
Supplementary Material
Acknowledgments
Supported by grant funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) to Research Triangle Institute (U10 HD063036); CaseWestern Reserve University (U10 HD063072); Columbia University (U10 HD063047); Indiana University (U10 HD063037); Magee-Women’s Hospital (U10 HD063041); Northwestern University (U10 HD063020); University of California at Irvine (U10 HD063046); University of Pennsylvania (U10 HD063048); and University of Utah (U10 HD063053).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has indicated that he or she has met the journal’s requirements for authorship.
References
- 1.Spong CY. Prediction and prevention of recurrent spontaneous preterm birth. Obstet Gynecol. 2007;110:405–15. doi: 10.1097/01.AOG.0000275287.08520.4a. [DOI] [PubMed] [Google Scholar]
- 2.MacDorman MF, Declercq E, Zhang J. Obstetrical Intervention and the Singleton Preterm Birth Rate in the United States From 1991–2006. Am J Public Health. 2010;100:2241–7. doi: 10.2105/AJPH.2009.180570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.McKinnon B, Yang S, Kramer MS, et al. Comparison of black–white disparities in preterm birth between Canada and the United States. CMAJ. 2016;188:E19–26. doi: 10.1503/cmaj.150464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Warnecke RB, Oh A, Breen N, et al. Approaching health disparities from a population perspective: The National Institutes of Health Centers for Population Health and Health Disparities. Am J Public Health. 2008;98:1608–15. doi: 10.2105/AJPH.2006.102525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Vos AA, Posthumus AG, Bonsel GJ, Steegers EA, Denktaş S. Deprived neighborhoods and adverse perinatal outcome: A systematic review and meta-analysis. Acta Obstet Gynecol Scand. 2014;93:727–40. doi: 10.1111/aogs.12430. [DOI] [PubMed] [Google Scholar]
- 6.Bryant AS, Worjoloh A, Caughey AB, Washington AE. Racial and ethnic disparities in obstetric outcomes and care: Prevalence and determinants. Obstet Gynecol. 2010;202:335–43. doi: 10.1016/j.ajog.2009.10.864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grobman WA, Parker C, Wadhwa PD, et al. Racial and ethnic disparities in measures of self-reported psychosocial states and traits during pregnancy. Am J Perinatol. 2016;33:1426–32. doi: 10.1055/s-0036-1586510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wadhwa PD, Entringer S, Buss C, Lu MC. The contribution of maternal stress to preterm birth: issues and considerations. Clin Perinatol. 2011;38:351–84. doi: 10.1016/j.clp.2011.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Haas DM, Parker CB, Wing DA, et al. A description of the methods of the Nulliparous Pregnancy Outcomes Study: monitoring mothers-to-be (nuMoM2b) Am J Obstet Gynecol. 2015;212:539e1–e24. doi: 10.1016/j.ajog.2015.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 11.Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory for Adults. Palo Alto, CA: Mind Garden, Inc; 1983. [Google Scholar]
- 12.Connor KM, Davidson JR. Development of a new resilience scale: the Connor-Davidson Resilience Scale (CD-RISC) Depress Anxiety. 2003;18:76–82. doi: 10.1002/da.10113. [DOI] [PubMed] [Google Scholar]
- 13.Zimet GD, Dahlem NW, Zimet SG, Farley GK. The Multidimensional Scale of Perceived Social Support. J Personality Assess. 1988;52:30–41. [Google Scholar]
- 14.Krieger N, Smith K, Naishadham D, Hartman C, Barbeau EM. Experiences of discrimination: validity and reliability of a self-report measure for population health research on racism and health. Soc Sci Med. 2005;61:1576–96. doi: 10.1016/j.socscimed.2005.03.006. [DOI] [PubMed] [Google Scholar]
- 15.Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: Development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150:782–6. doi: 10.1192/bjp.150.6.782. [DOI] [PubMed] [Google Scholar]
- 16.Bann CM, Parker CB, Grobman WA, et al. Psychometric properties of stress and anxiety measures among nulliparous women. J Psychosom Obstet Gynaecol. 2017;38:53–62. doi: 10.1080/0167482X.2016.1252910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alexander GR, Himes JH, Kaufman RB, Mor J, Kogan M. A United States national reference for fetal growth. Obstet Gynecol. 1996;87:163–8. doi: 10.1016/0029-7844(95)00386-X. [DOI] [PubMed] [Google Scholar]
- 18.Muthén LK, Muthén BO. Mplus User’s Guide. 7. Los Angeles, CA: Muthén & Muthén; 2015. [Google Scholar]
- 19.McLachlan G, Peel D. Finite mixture models. New York: Wiley; 2000. [Google Scholar]
- 20.Lo Y, Mendell N, Rubin D. Testing the number of components in a normal mixture. Biometrika. 2001;88:767–78. [Google Scholar]
- 21.Vuong Q. Likelihood ratio tests for model selection and non-nested hypotheses. Econometrica. 1989;57:307–33. [Google Scholar]
- 22.Simon CD, Adam EK, Holl JL, Wolfe KA, Grobman WA, Borders AE. Prenatal Stress and the Cortisol Awakening Response in African-American and Caucasian Women in the Third Trimester of Pregnancy. Matern Child Health J. 2016;20:2142–9. doi: 10.1007/s10995-016-2060-7. [DOI] [PubMed] [Google Scholar]
- 23.Shapiro GD, Fraser WD, Frasch MG, Séguin JR. Psychosocial stress in pregnancy and preterm birth: associations and mechanisms J Perinat Med. J Perinat Med. 2013;41:631–45. doi: 10.1515/jpm-2012-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Olson DM, Severson EM, Verstraeten BS, Ng JW, McCreary JK, Metz GA. Allostatic Load and Preterm Birth. Int J Mol Sci. 2015;16:29856–74. doi: 10.3390/ijms161226209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chen MJ, Grobman WA, Gollan JK, Borders AEB. The use of psychosocial stress scales in preterm birth research. Am J Obstet Gynecol. 2011;205:402–34. doi: 10.1016/j.ajog.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.