Abstract
Objective
We examine the association between emergency physician characteristics and practice factors with the risk of being named in a malpractice claim.
Methods
We used malpractice claims along with provider, operational, and jurisdictional data from a national emergency medicine group (87 emergency departments (EDs) in 15 states from 1/1/2010 to 6/30/2014) to assess the relationship between individual physician and practice variables and being named in a malpractice claim. Individual and practice factors included: years in practice, emergency medicine Board Certification, visit admission rate, Relative Value Units/hour generated, total visits seen as attending physician of record, working at multiple facilities, working primarily overnight shifts, patient experience data percentile, and state malpractice environment. We assessed the relationship between emergency physician and practice variables and malpractice claims using logistic regression.
Results
In 9,477,150 ED visits seen by 1,029 emergency physicians, there were 98 malpractice claims against 90 physicians (9%). Increasing total number of years in practice (adjusted odds ratio 1.04, 95% CI 1.02–1.06) and higher visit volume (adjusted odds ratio 1.09 per 1000 visits, 95% CI 1.05–1.12) were associated with being named in a malpractice claim. No other factors were associated with malpractice claims.
Conclusion
In this sample of emergency physicians, one in 11 were named in a malpractice claim over 4.5 years. Total number of years in practice and visit volume were the only identified factors associated with being named, suggesting that exposure to higher patient volumes and longer practice experience are the primary contributors to malpractice risk.
Keywords: malpractice, litigation, acute care, emergency care, emergency department
Introduction
Background
Emergency medicine is a specialty with high malpractice risk due to the undifferentiated patient population and limited time and resources to manage acutely ill and injured individuals. Emergency physicians are likely to be involved in malpractice claims; over 75% of emergency physicians will be named in a malpractice claim at some point in their career.1 On average, physicians spend 50.7 months of their career involved in litigation.2 To help reduce risk, 9 in 10 physicians report overusing or over-ordering tests or procedures, termed defensive medicine, which costs an estimated $46 billion annually in the U.S.3,4
Importance
A malpractice claim can negatively impact a provider through anxiety, depression and even thoughts of suicide, referred to as medical malpractice stress syndrome.5 Identifying factors associated with greater malpractice risk could help improve physician well-being. While patient experience data, years in practice, and practice location have been studied in isolation or outside of emergency medicine with respect to malpractice claims, limited data exist on the effect of emergency physician and practice factors in combination on malpractice risk.6–8 Identification of such factors may inform how emergency physicians practice, the environments in which they choose to work, and how to approach reducing malpractice risk.
Goals of This Investigation
We evaluate the association of commonly measured emergency physician and practice factors with the risk of being named in a malpractice claim.
METHODS
Study Design and Setting
We performed a retrospective cross-sectional study using data from a national emergency physician group that managed 87 EDs (including 3 Level-1 Trauma centers and 12 with Emergency Medicine residents) in 15 states during the study period (January 1, 2010–June 30, 2014) (Appendix 1). As hospital contracts can change over time, the number of facilities varied between 51 and 65 for any given month. This physician group also maintained its own risk retention program that recorded all malpractice claims during the study period. Data on malpractice claims were downloaded on September 30, 2015 to ensure complete availability of the provider, operational and jurisdictional variables evaluated in the study. Visit characteristics, including Current Procedural Terminology Evaluation and Management and Procedure codes (CPT E/M codes) and relative value units (RVUs) generated, were abstracted by trained billing specialists. During this period, billing specialists were required to have or acquire relevant certification(s) between their second and third employment year with ongoing training, auditing, and external evaluation. The group also maintains a demographic and credentialing database of all physicians. Physicians’ clinical hours were tracked electronically (Tangier, Sparks, MD). Patient experience data (Press-Ganey Associates Inc., South Bend, IN) were linked to physicians monthly. The study was approved by the Carnegie Mellon University Institutional Review Board.
Selection of Participants
We included emergency physicians with at least four consecutive months of practice data working in a non-pediatric ED (mean patient age ≥18 years). To ensure that our results were not contaminated by idiosyncratic physician patterns and observe practice stability, we explored the monthly RVUs/hour for each physician. Starting with each physician’s first appearance in the dataset, we calculated the monthly RVUs/hour for each of the first 6 months of physician data. We compared RVUs/hour for each month with the previous month using the paired t-tests and Wilcoxon signed-rank tests when appropriate. As month-to-month changes in RVUs/hour did not differ after the third month, this suggested that four months of practice was sufficient to allow time for provider acclimatization to the practice environment and assessment of practice patterns related to malpractice risk. Pediatric EDs may have different malpractice risks than general, non-pediatric EDs; therefore, pediatric EDs and were excluded.
Methods and Measurements
We modeled variables theoretically related to malpractice risk based on prior work and through the authors’ consensus.1–7 These variables included provider and operational factors as well as assessment of the malpractice risk based on the state malpractice environment of the ED (described in detail below). Provider factors included: years in practice, defined as the number of years (days/365.25) between residency completion (not counting fellowship training) and the median study period date (March 31, 2012), Board Certification (American Board of Emergency Medicine (ABEM) or American Osteopathic Board of Emergency Medicine (AOBEM)), and majority night practice (>50% of clinical hours between 0000 and 0600 over the time period the physician was in the dataset).
Operational factors at the physician level included median monthly RVUs generated per hour (RVUs/patient x Patients/hour) which is a composite measure for patient acuity and volume, data on patient experience (median monthly physician Press-Ganey© percentile), median monthly physician admission rate (a risk tolerance and patient acuity marker),1,9 total visits seen as an attending physician of record, and working in multiple EDs (more than 20% of clinical hours at >1 site). The latter was included as less familiarity with local operating policies may occur when physicians work in multiple EDs. RVUs were those attributed to the attending physician of record. We did not include visits where RVUs were not attributed to an attending physician (e.g. those visits seen only by an advanced practice provider). Total visits were defined as the cumulative number of visits seen by the physician as the attending of record during the study period.
Data from the 2014 American College of Emergency Physicians (ACEP) report card on the emergency medicine malpractice practice environment were also included.10 This report evaluated US states on multiple factors including the malpractice environment and assigned a grading system, ‘A’ being the best score and ‘F’ being the worst. The malpractice environment assessment included consideration of standards for certifying and judging malpractice claims, limitations or lack thereof on monetary damages, and legislative or regulatory tort reform among other factors. We chose to evaluate whether perceived above average medical malpractice liability environment, compared to perceived average or below average environment, was associated with reduced odds of being named in a malpractice claim. We therefore collapsed medical liability environment categories (Grades A & B and Grades C, D, & F) based on the modal ED for each physician during the study period (Appendix 1).
Outcome Measure
The outcome measure was the physician being named in any (i.e., one or more) malpractice claim filed based on visits occurring during the study period (January 1, 2010–June 30, 2014) regardless of claim disposition, under the captive risk retention program of the national physician group. We included all claims filed during the study period regardless of disposition (i.e. whether it was settled, dismissed, or adjudicated in favor of the plaintiff or defendant).
Data Analysis
We used logistic regression to estimate the association between a physician being named in a malpractice claim and included factors. Multi-collinearity among variables was assessed using variance inflation factors (VIFs). We computed a VIF for each coefficient in the logistic regression equation, and multi-collinearity was not detected. We used the Hosmer-Lemeshow statistic to assess goodness of fit (Table 1). We estimated cluster robust standard errors, which correct for heteroscedasticity and correlation between physicians working in the same ED.
Table 1.
Characteristics of Emergency Physicians With and Without Malpractice Claims
| Variable | Physicians With No Malpractice Cases (N=939) | Physicians with One or More Malpractice Cases (N=90) | Odds Ratio (95% CI)* |
|---|---|---|---|
| Physician Characteristics | |||
| Total Years in Practice (SD) | 11.8 (9.4) | 15.7 (9.2) | 1.04 (1.02–1.06) |
| Board Certification in Emergency Medicine (N, % Yes) | 758 (80.72%) | 81 (90%) | 1.14 (0.49–2.69) |
| Predominantly Night Practice (N, % Yes) | 53 (5.6%) | 6 (6.7%) | 1.31 (0.50–3.44) |
| Operational Characteristics | |||
| Total number of visits (IQR) | 7572 (3471–13501) | 13787 (10282–17352) | 1.09 (1.05–1.12)** |
| Median Monthly Physician Press-Ganey© Percentile (IQR) | 60 (25–90) | 60 (30–90) | 1.00 (0.99–1.01) |
| Median Monthly RVUs/hr (IQR) | 9.6 (8.6–10.6) | 9.78 (8.8–10.7) | 1.00 (0.87–1.15) |
| Median Monthly Admission Percentage Rate (IQR) | 20% (13.6–26.5) | 18.6% (13.4–23.8) | 2.92 (0.32–26.9) |
| Work at Multiple Facilities (N, % Yes) | 217 (23.1%) | 26 (28.9%) | 1.34 (0.63–2.87) |
| Jurisdictional Characteristic – ACEP Report Card | |||
| Grades A & B | States - 2/15 (13.3%) Physicians – 188/939 (20%) |
States - 2/15 (13.3%) Physicians – 27/90 (30%) |
Reference |
| Grades C, D & F | States - 13/15 (86.7%) Physicians – 751/939 (80%) |
States – 13/15 (86.7%) Physicians – 63/90 (70%) |
0.65 (0.27–1.54) |
SD – Standard Deviation
RVUs/hr – Relative Value Units/hour
IQR – interquartile range
ACEP – American College of Emergency Physicians
Odds ratios represent the results of multivariable analysis for physician-level risks of being named in one or more malpractice claims over the study period
Odds Ratio per 1000 Visits
Hosmer-Lemeshow Statistic for Logistic Regression Model – 8.905
We also conducted several sensitivity analyses. Due to the low frequency of malpractice claims, we used Firth’s penalized likelihood logistic regression for comparison to reduce potential bias when analyzing rare events. We also evaluated potential interaction terms for the included factors. Varying definitions of years in practice were also tested (to end of the study period and to end of physician appearance in the data set).
A challenge with a cross-sectional study such as this is that physicians enter and exit the data set at different points in the study period. To address this, we also examined the variables of years in practice and number of visits seen to assess for length-biased sampling.11 This analysis showed no evidence of length-biased sampling for years in practice and inconclusive results for number of visits seen. However, using Visits/Year would control for the potential latter bias. By standardizing all physicians’ visits to a specific unit of time, we were able to control for the potential bias caused by being in the sample for a longer period of time than other physicians. Replacing Total Visits Seen with Visits/Year in the logistic regression model yielded equivalent results to those reported below, suggesting that length bias was not a problem in the data set.
Malpractice claims may also impact the rate at which providers exit the physician group as well as the database. There is a potential that physicians who were named early in practice may have dropped out of the specialty and been lost from the dataset, making it appear that longer practice led to more claims. To account for this, we also compared the rate of providers who dropped out of the dataset between those named and those not named in a claim. As it can take time from an index visit until a malpractice claim is filed, we ran a sensitivity analysis excluding providers with ≤2 years of experience. To address the extremes in number of visits seen by physicians depending on supervised personnel (e.g., physician assistants or residents) and time in practice, we also ran a sensitivity analysis excluding both high and low (top and bottom 1%) volume providers. All analyses were completed using R statistical software (Version 3.3.1) and Stata MP 14 (Stata Corp, College Station, TX).
Results
Characteristics of study subjects
There were 9,477,150 ED visits seen by 1,029 emergency physicians (711 male and 318 female) from 87 EDs who met inclusion criteria; 90 included emergency physicians were named in 98 malpractice claims during the study period. No physician was named in more than two malpractice claims during the study period. Overall, the mean duration (minimum, maximum) of providers within the dataset was 31 (5, 54) months, 29.8 (5, 54) for those not involved in a claim and 43.2 (7, 54) for those involved in a claim. Total visits seen and total number of years in practice were higher among those named in a claim (Table 1). While many providers were new to the practice of emergency medicine (Appendix 2), the mean (standard deviation) practice duration was 11.8 (9.4) years for those not named in a claim compared to 15.7 (9.2) for those named in a claim. Supplemental analyses which excluded those early in their career and the extremes of volumes of visits in practice showed that the results did not appreciably change (Appendices 3 and 4). Median monthly Press-Ganey© scores (inter-quartile range) were similar between those named (60 [30–90]) and not named in a claim (60 [25–90]). Of the included malpractice claims, 70 (71.4%) were dismissed, and most commonly involved neurologic cases (28 [28.6%]) (Table 2).
Table 2.
Characteristics of 98 Included Malpractice Claims
| Primary Body System/Disease Process for Malpractice Claim# | N (%) * |
|---|---|
|
| |
| Neurologic | 28 (28.6) |
| Gastrointestinal | 15 (15.3) |
| Cardiovascular | 9 (9.18) |
| Obstetrics and Gynecology | 9 (9.18) |
| Orthopedics | 8 (8.16) |
| Respiratory | 8 (8.16) |
| Other§ | 21 (21.4) |
|
| |
| Case Resolution | N (%)* |
|
| |
| Dismissed | 70 (71.4) |
| Settled | 21 (21.4) |
| Defense Verdict | 4 (4.08) |
| Plaintiff Verdict | 2 (2.04) |
| Still in litigation | 1 (1.02) |
Totals may not equal 100% due to rounding.
Based on the internal classification by the risk management department of this multistate emergency medicine group
‘Other’ includes claims involving integument/wounds (n=7), genitourinary (n=4), otolaryngology (n=2), endocrine (n=2), psychiatry (n=2), blood/lymphatic (n=1), and other malpractice claims not related to specific organ systems such as issues regarding patient confidentiality (n=3).
Main Results
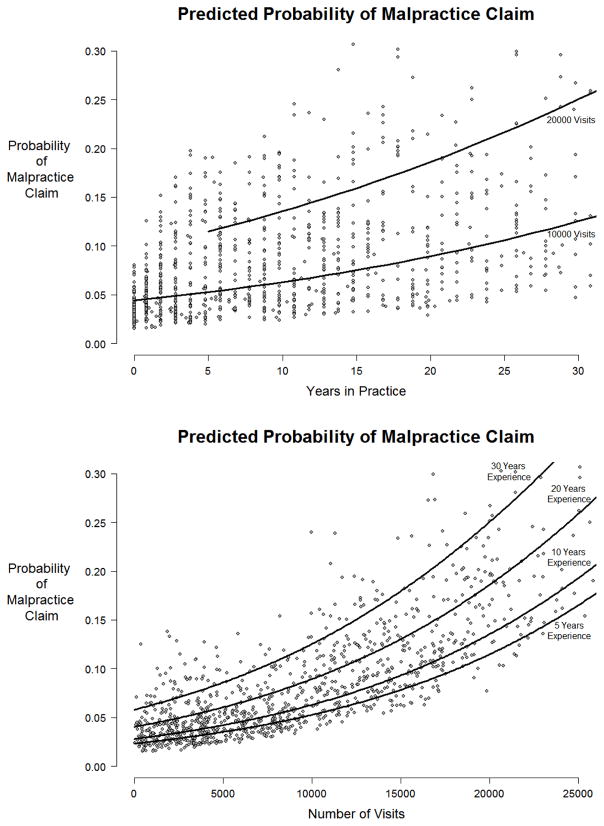
Of the nine independent variables, only increasing total number of years in practice (adjusted odds ratio 1.04,per year 95% CI 1.02–1.06) and total visits seen as the attending physician of record (adjusted odds ratio 1.09 per 1000 visits, 95% CI 1.05–1.12) were associated with being named in a malpractice claim (Table 1). When stratified by visit volume, there was a direct relationship between visit volume and malpractice risk that increased with rising years in practice (Figure). No interaction terms were significant, and the results were similar in all sensitivity analyses conducted with the various definitions of years in practice described above. Dropout rates from the dataset during the study period were similar between those named in a claim (34/90, 37.8%) and those not named in a claim (416/939, 44.3%). The results did not change with the sensitivity analyses of removing physicians with ≤2 years of experience or extremes of volume of visits seen in practice (Appendices 3 and 4).
Figure.
Predicted Probabilities of a Physician Being Named in a Malpractice Claim by Years in Practice and Total Number of Visits
Points represent the probability of being named in a malpractice claim as predicted by the logistic regression model for the 1029 physicians in this study. Lines represent the predicted probabilities holding other independent variables constant at average or most common value. Number of visits and years in practice (starting at <1 year, represented as 0) are reported as median values during the study time period.
Limitations
Our study findings were limited to assessing malpractice claims filed during the study period. Included physicians may have had malpractice claims prior or subsequent to the study period, which may have led to misclassification of the primary outcome. Despite examining over 9 million ED visits, the number of malpractice claims was small (a rate of ~1 claim/100,000 ED visits), and the percent of physicians involved in a claim per year (90 providers out of 1029 over 4.5 years or ~2%) is lower than other national estimates (7–8%).1 Therefore, small changes in the number of claims could alter these results. However we performed multiple sensitivity analyses to verify the validity of our results.
Given the lag between the relevant ED visit and the malpractice claim filing date, provider, operational, and jurisdictional factors used in the study may have changed. In addition, we did not include variables that may theoretically be related to risk of a malpractice claim, such as physician age, gender, race, or diagnostic test utilization. In our data, physician age, as expected, was highly correlated with years in practice, and total hours worked by a physician was correlated with total visits seen (correlation coefficient r=0.91, 95CI: 0.89–0.92) (Appendix 5). As we believe years in practice to be more telling of the risk of being named in a malpractice claim due to increased exposure, and in an effort to restrict the number of predictor variables, we elected to use years in practice instead of physician age. For a similar reason, we chose to use total visits seen rather than total hours worked by a physician. We also did not measure patient factors that could have increased the risk of a claim, such as patient age, insurance status, and race.6–8 There were a small number of providers (n=8) who were involved in more than one claim during the study period. Given this small number and that previous work has described characteristics of physicians involved in multiple claims, we did not further categorize this group.7 Further research examining larger pools of emergency physicians involved in multiple malpractice claims may help to better characterize this population.
Our results come from a single national emergency medicine group. However, this group does not staff hospitals in all states. Therefore, the malpractice risk may differ in areas not examined in our study. Also, this group strives to employ Board Certified (ABEM or AOBEM) with over 80% being certified in our dataset. Future work is needed to examine malpractice claims against non-Board Certified emergency physicians. However, in this sample, Board Certification or lack thereof was not associated with malpractice risk.
Due to the number of outcomes, we only included a limited number of predictors in the model. We, a priori, chose factors we believed to be conceptually related to malpractice claims and potentially modifiable by emergency physicians or emergency medicine groups. To include factors we felt were important, we dichotomized multiple variables, which may limit the predictive ability of these variables to account for non-linear relationships with malpractice risk. This is especially true for the state malpractice environment. Given the multiple factors that are included in a state’s emergency medicine malpractice environment, further work should evaluate the impact of specific legal environment factors on the incidence of malpractice claims in larger data sets where there is broader representation of state jurisdictions.
In addition, we did not have granular malpractice claim data to evaluate the role of supervision of either advanced practice providers or residents in the included malpractice claims. Appendices 6 and 7 provide a description of the supervisory status of the EDs from which claims originated in this study and their general operational characteristics. However, the important question of the role of supervision should be further explored in larger-scaled studies.
Finally, our analysis only evaluated the association of the included independent variables with malpractice claims as opposed to malpractice claim dispositions. Given the limited number of included physicians with claims, evaluating associations with claim dispositions separately was limited. However, we do present the results of this association in Appendices 8 and 9. Consistent with our primary analysis, higher visit volume continued to be an associated factor in both of these models and total years in practice in the dismissed/defense verdict model. However, the nature of the relatively small sample size of emergency physicians named in a malpractice claim will require further study of this issue in the future.
Discussion
Among more than 1,000 emergency physicians over a four-and-a-half year period, increasing years in practice and higher visit volume as attending physician of record were the only factors we found to be associated with increased risk of being named in a malpractice claim. Factors conceptually associated with malpractice risk, such as practice intensity, Board Certification, predominant night or multi-ED practice, higher admission rates, patient experience assessment, and practice environment were not found to be predictors.
Our findings have important implications for emergency physicians, their practice organizations, and advocacy efforts. Errors and poor outcomes can occur in medical care, and the ED is a high-risk environment due to the nature of the practice, high volumes, visit acuity, and lack of prior patient relationships. Yet only a small proportion of visits ever lead to a malpractice claim. Of those, only a subset are true adjudicated or acknowledged breaches in the standard of care. In many claims, outcomes may not be preventable errors or can be attributed more directly to other factors outside of the physicians’ control. In our sample, the vast majority of claims were dismissed (although we do not know at what stage), and less than one in 20 led to plaintiff verdicts. Therefore, being named in a malpractice claim may not be an indicator of practice quality.
However, rising total number of years in practice was associated with higher rates of malpractice claims, with the odds rising 4% per year in practice. This means that a physician in practice for 20 years is at considerably higher risk of a malpractice claim than a physician who has been out of residency only a few years. This finding did not disappear despite many adjustments, including practice volume, as can be seen in the Figure. We were unable to determine a reason for this finding other than increased exposure to patients over time. No other factors, including measures of practice style (i.e. admission rate and Press-Ganey© scores) or training (i.e. Board Certification), or methodologic adjustments explained the finding. Conceptually, several factors may theoretically underlie the association between total years in practice and increased odds of being named in a malpractice claim such as changes in emergency medicine training over time, how emergency physicians obtain continuing medical education after residency training is complete, or other factors. Further investigation is warranted to better understand this effect.
Practice volume also raised the marginal risk of a malpractice claim. This makes sense in that every additional patient represents an additional exposure to a clinical event that could trigger a malpractice claim. There were providers in the dataset who saw a greater number of visits over the four-and-a-half-year study period (>30,000 patients). If these providers work an average of 1800 hours/year, then some would be averaging treatment of nearly four patients/hour. While for an individual provider this may be challenging, it is possible to have this pace when seeing patients in conjunction with other providers including advanced practice providers or residents. Based on the dataset, we were unable to identify if these were seen primarily by the attending or in conjunction with residents or advanced practice providers. By contrast, there were some physicians who saw relatively few visits. To account for this, we reran the analysis after removing both the high and low volume physicians (top and bottom 1%) and, as noted above, found no change in our results.
The finding that patient experience data were not associated with being named in a malpractice claim is noteworthy since prior work has linked higher patient complaints about communication to malpractice; however, this has not been studied specifically in emergency physicians.6,8 The lack of an association may be due to poor reliability and validity of patient experience data itself which is driven by small numbers of responses and, more importantly, non-representative samples (i.e. poor response rates in ED experience surveys). Alternatively, better quality communication may not impact malpractice risk, possibly because of the limited relationship and relatively brief interaction with an emergency physician. Similarly, admission rates were also not associated with malpractice (i.e. risk averse providers may admit patients more frequently); therefore, lowering the admission threshold to reduce malpractice risk may not be an effective strategy. 1,12–13 In addition, other potential indicators of practice quality (i.e., Board Certification), practice pattern (i.e., high intensity [RVUs/hour]), or predominantly night or multi-facility practice, were similarly not important predictors of malpractice risk. However, further study and replication of our results should be considered.
We also found, within the limitations of the states from which we can draw data, no association between state malpractice environment, defined by the ACEP classification system that takes into account factors related to how malpractice claims are certified and the standard for their judgment in court, and the risk of a malpractice claim.10 While tort reform has been suggested as a means of reducing defensive medicine, it does not impact practice patterns of ED providers, including admission rates.9 Our results add to these data, suggesting that national efforts to help mitigate malpractice risk in emergency medicine may need to consider other approaches.
In conclusion, increasing years in practice and total visit volume seen as attending physician of record were associated with increased odds of being named in a malpractice claim. Other physician and practice factors previously believed to be associated with malpractice claims were not associated with increased risk.
Supplementary Material
Acknowledgments
Funding: Dr. Ward is supported by Award Number K23 HL127130from the National Heart, Lung, and Blood Institute (NHLBI)/NIH.
The authors would like to acknowledge the contribution of Susan Fix, JD of US Acute Care Solutions for her work on the regulatory aspects of this research collaboration, Paul Dietzen, Jesse Eterovich, Dianne Onesti, RN, LNCC, and the Legal Department of US Acute Care Solutions for their work in compiling the data used in this study, and thank Dominic Bagnoli, MD, Michael Osmundson, MD, James Augustine, MD, Amer Aldeen, MD, and the leadership of US Acute Care Solutions for their support of this research collaboration.
Footnotes
Conflicts of Interest: None
Authors Contribution Statement: JNC, JMP, CC, MJW and AV conceived the study. JNC, CC and AV supervised data collection. KMF and MZH performed the statistical analysis. JNC, JMP and AV drafted the manuscript, and all authors contributed substantially to its revision. AV takes responsibility for the manuscript as a whole.
References
- 1.Jena AB, Seabury S, Lakdawalla D, Chandra A. Malpractice risk according to physician specialty. N Engl J Med. 2011 Aug 18;365(7):629–636. doi: 10.1056/NEJMsa1012370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Seabury SA, Chandra A, Lakdawalla DN, Jena AB. On average, physicians spend nearly 11 percent of their 40-year careers with an open, unresolved malpractice claim. Health Aff (Millwood) 2013 Jan;32(1):111–119. doi: 10.1377/hlthaff.2012.0967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bishop TF, Federman AD, Keyhani S. Physicians’ views on defensive medicine: a national survey. Arch Intern Med. 2010 Jun 28;170(12):1081–1083. doi: 10.1001/archinternmed.2010.155. [DOI] [PubMed] [Google Scholar]
- 4.Mello MM, Chandra A, Gawande AA, Studdert DM. National costs of the medical liability system. Health Aff (Millwood) 2010 Sep;29(9):1569–1577. doi: 10.1377/hlthaff.2009.0807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sanbar SS, Firestone MH. [Accessed September 27, 2016];Medical Malpractice Stress Syndrome. http://www.acep.org/uploadedFiles/ACEP/Professional_Development/Faculty_Development/Medical Malpractice Stress Syndrome article for web.pdf.
- 6.Cydulka RK, Tamayo-Sarver J, Gage A, Bagnoli D. Association of patient satisfaction with complaints and risk management among emergency physicians. J Emerg Med. 2011 Oct;41(4):405–411. doi: 10.1016/j.jemermed.2010.10.021. [DOI] [PubMed] [Google Scholar]
- 7.Studdert DM, Bismark MM, Mello MM, Singh H, Spittal MJ. Prevalence and Characteristics of Physicians Prone to Malpractice Claims. N Engl J Med. 2016 Jan 28;374(4):354–362. doi: 10.1056/NEJMsa1506137. [DOI] [PubMed] [Google Scholar]
- 8.Hickson GB, Federspiel CF, Pichert JW, Miller CS, Gauld-Jaeger J, Bost P. Patient complaints and malpractice risk. JAMA. 2002 Jun 12;287(22):2951–2957. doi: 10.1001/jama.287.22.2951. [DOI] [PubMed] [Google Scholar]
- 9.Waxman DA, Greenberg MD, Ridgely MS, Kellermann AL, Heaton P. The effect of malpractice reform on emergency department care. N Engl J Med. 2014 Oct 16;371(16):1518–1525. doi: 10.1056/NEJMsa1313308. [DOI] [PubMed] [Google Scholar]
- 10.Report Card Task Force Members, ACEP Staff. America’s emergency care environment, a state-by-state Report Card: 2014 edition. Ann Emerg Med. 2014 Feb;63(2):97–242. doi: 10.1016/j.annemergmed.2013.11.024. [DOI] [PubMed] [Google Scholar]
- 11.Akman O, Gamage J, Jannot J, Juliano S, Thurman A, Whitman D. A simple test for detection of length-biased sampling. Journal of Biostatistics. 2007;1(2):189–195. [Google Scholar]
- 12.Pines JM, Isserman JA, Szyld D, Dean AJ, McCusker CM, Hollander JE. The effect of physician risk tolerance and the presence of an observation unit on decision making for ED patients with chest pain. Am J Emerg Med. 2010 Sep;28(7):771–779. doi: 10.1016/j.ajem.2009.03.019. [DOI] [PubMed] [Google Scholar]
- 13.Abualenain J, Frohna WJ, Shesser R, Ding R, Smith M, Pines JM. Emergency department physician-level and hospital-level variation in admission rates. Ann Emerg Med. 2013 Jun;61(6):638–643. doi: 10.1016/j.annemergmed.2013.01.016. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.