Abstract
Purpose
Cancer patients are at high risk of malnutrition and tumor cachexia further increasing morbidity and mortality. Reasons for cachexia are not clear yet, but inflammatory processes as well as the occurrence of taste disorders reducing nutrient uptake are discussed to play key roles. The purpose of this study was to gain insight into causative factors of taste disturbance in cancer patients. Does the cancer itself, inflammatory processes or cancer therapy influence taste disorders?
Methods
To capture an underlying taste disorder patients with cancer (n = 42), acutely hospitalized inflammatory disease patients (n = 57) and healthy controls (n = 39) were examined. To assess the influence of chemotherapy, patients with and without chemotherapy were compared. Taste tests were performed according to DIN ISO 3972:2011. Inflammation was recorded using laboratory parameters. Statistical evaluation was conducted using the Software R.
Results
Cancer patients showed significantly increased taste thresholds for sweet, salty, and umami compared to healthy controls. There were no significant differences in taste detection and recognition between patients with former, current, or without chemotherapeutical treatment. Patients with an acute inflammatory disease showed an increased taste threshold for umami compared to healthy controls.
Conclusions
It could be shown that cancer patients suffer from taste disorders irrespective of an existing chemotherapeutical treatment. Cancer-related inflammation appears to have a greater impact on taste perception than an acute inflammatory process. Therefore, an adapted dietary adjustment should be carried out at an early stage for cancer patients in order to avoid nutritional disorders caused by a taste disorder.
Keywords: Cancer, Taste disturbance, Inflammatory disease, Cachexia, Malnutrition
Introduction
In the course of malignant and acute inflammatory diseases, a broad range of physical functions is affected, frequently leading to reduced food intake and to significant weight loss [1, 2]. The resulting unintended reduction of fat and muscle mass can adversely influence prognosis, morbidity, and mortality of the patients [3]. Impaired nutrient intake is caused by multiple factors; one of them is altered taste perception [4–6].
Many different factors can trigger taste disorder. For instance, benign acute diseases like gastrointestinal or inflammatory processes can lead to an impaired sense of taste [7]. This link has already been described by Zopf et al. in patients with inflammatory bowel disease who had a significantly inferior sense of taste than healthy controls [8].
Due to the underlying disease and the tumor-specific therapy, cancer patients often suffer from anorexia. The resulting malnutrition contributes to the progression of cancer cachexia and to a reduced quality of life of the patients [9–11]. Systemic inflammation, enhanced catabolic processes [2, 12], and treatment with cytostatics or radiation therapy are discussed to influence taste sensation [13–15]. Mucosal damage due to the anti-cancer therapy is supposed to be one reason for the loss of taste, since healing of the mucosal inflammation has been described to improve taste perception [16, 17]. It is not yet clear, however, whether the underlying tumor disease or the specific therapy is mainly responsible for the taste disorder. Due to a high variability in the methods used for taste detection, the results from investigations with patients on impaired taste sense are hard to compare [18]. There is a particular lack of studies analyzing the taste detection of cancer patients versus patients with acute benign inflammatory disorders. Also missing are studies comparing cancer patients with or without chemotherapy. Of special interest is the evaluation of the impact of influence of a systemic inflammation on taste perceptions versus the impact of an acute mucosal damage due to tumor-specific therapy.
The aim of the presented study was to gain insight into how cancer disease and acute benign inflammatory disorders affect taste perception. Moreover, we aimed to achieve further information on a potential impact of chemotherapeutic treatment on gustatory sensation, in order to improve future therapy recommendations.
Material and methods
Selection of patients
In order to detect taste perceptions and assess causal factors, the following three groups were compared: tumor patients, acutely hospitalized patients with non-malignant inflammatory diseases, and healthy control study participants. The acquisition of patients took place in the in- and outpatient care of the Department of Medicine 1 of the University Hospital Erlangen. Healthy control participants were recruited from clinical staff and their circle of acquaintances.
Excluded were persons < 18 years of age, pregnant women, patients suffering from COPD (chronic obstructive pulmonary disease), taking anti-cholinergic medication or taking medication with a known strong influence on taste perception, as well as patients on parenteral nutrition. Also excluded were persons with a known taste or olfactory disorder.
Patient data
The collected data comprise demographic data (age and gender), anamnesis data (underlying diseases, drug intake, known taste or olfactory disorders, and nicotine or alcohol consumption), inflammation parameters (C-reactive protein (CRP), pathological > 5 mg/l, and leukocytes, pathological < 4.0 or > 10.0 × 103/μl) and albumin (pathological < 35 g/l). All patients’ assessments were performed within 2 days to guarantee coherence of taste test results with inflammation status.
Taste sensation test
The study participants were asked to refrain from eating, smoking, or drinking prior to testing. The taste sense was tested with a “whole mouth method” using a pump-action spray [19] with associated pharyngeal adapters. Using this approach, we determined the detection and recognition thresholds of the five basic taste-producing substances-herein designated as “tastants” -sweet, sour, salty, bitter, and umami [20, 21].
Preparation of solutions
The tastant solutions were prepared in the Aroma Research Group at the University of Erlangen-Nuremberg. The tastants were solubilized in water, and sorbic acid was added as a preservative. Sorbic acid is anti-microbial, has no influence on the organoleptic impact, and is soluble in water [22]. The solutions analyzed in the taste tests contained 0.1% sorbic acid. Additionally, the stock solution was boiled twice to minimize microbial contamination. The solutions were also tested regarding their stability in the Institute for Clinical Microbiology of the University Hospital Erlangen. The same concentrations of the tastant solutions were tested throughout the study. The solutions were kept at 2 to 10 °C in the refrigerator. Prior to each test, all participants received a new set of pharyngeal adapters for hygienic reasons. The solutions were based on the standard “Sensory analysis to determine taste sensitivity” (DIN ISO 3972:2011), which had been developed to monitor the taste sensation of study participants [23]. While keeping the concentration steps as described below, the test solutions were adapted to the elder and hospitalized study collective by increasing the starting concentration. The tastants sweet, salty, and umami were tested in six concentration steps. The tastants bitter and sour were tested in seven because pre-tests had shown that six steps were not sufficient. The highest concentrations contained 1.45 g/l citric acid, 0.65 g/l caffeine, 5.83 g/l sodium chloride, 55.56 g/l saccharose, and 2.92 g/l monosodium glutamate monohydrate. Sodium chloride-, caffeine- and citric acid solutions were stable for more than a week. Nevertheless, all solutions were prepared freshly every 5 days.
Performance of taste tests
When conducting the taste tests, the tastant solutions were presented in a standardized sequence. The study participants received water with the same frequency as the tastant solutions. The tastant solutions were offered in increasing concentrations. Umami was presented at the end in order to avoid a possibly intensified taste of subsequent flavors [24]. Before the exact tastant can be recognized (recognition threshold), a taste is detected (detection threshold) [25]. The concentrations were raised until a tastant could be determined correctly twice in a row (ascending method of limits) [26]. The quality of the tastants were established by a forced-choice procedure, the seven options being sweet, sour, salty, bitter, umami, or neutral and “other than water,” or “no neutral” tastant.
One puff of the pump spray equated to 75 μl of solution. Generally, two to three puffs were given per tastant solution in order to apply sufficient amounts of the respective tastant.
The following comparisons were performed to achieve further insights into taste perception of cancer patients:
Patients who received chemotherapeutics during the study course were compared to patients, who were currently not treated with chemotherapeutics.
Patients who were treated with chemotherapeutics in the past (current included) were compared to patients who were chemotherapy-naïve.
Olfactory test
With every participant, an olfactory analysis using Burghart Sniffin’ Sticks was performed to test for hyposmia.
Statistical evaluation
The Software R was used for statistical evaluation [27]. For patient characteristics, the One-way ANOVA according to Welch and the Fisher’s exact test were deployed. The data of taste detection were described as ordinal. Groups were therefore compared using the Kruskal-Wallis test (One-way ANOVA on ranks). In addition, the Wilcoxon-Mann Whitney was applied as post hoc test to compare the groups by pairs. When applying the post hoc tests, an adjustment of p values according to Holm-Bonferroni was performed in order to avoid type I errors. A p value or adjusted p value < 0.05 was defined as significant.
Results
Patient characteristics
In total, 138 patients participated in the investigation with a mean age of 65.2 years. The first group consisted of 42 tumor patients (14 female, 28 male), who were hospitalized due to the cancer disease (n = 22) or were summoned for tumor-specific chemotherapy (n = 20). Thirty-one of the tumor patients had chemotherapy already in the past; 26 had current chemotherapy. The second group included 57 patients (25 females, 32 males) who were hospitalized due to an acute inflammatory disease without malignant underlying diseases. The third group comprised 39 healthy study participants (21 females, 18 males). Mean age and gender did not differ significantly between groups.
Four patients dropped out of the olfactory and taste tests on their own request. One of the acutely hospitalized patients had food intolerance for glutamate and was therefore excluded from the umami testing.
The tumor entities were mostly gastrointestinal tumors (85.3%), with colorectal (33.3%), cholangiocellular (11.9%), pancreatic (11.9%), esophageal (11.9%), stomach (7.1%), or hepatocellular carcinoma (7.1%). 16.7% of the tumor patients suffered from other cancer types (mamma (4.8%), prostate (4.8%), lung (2.4%), neuroendocrine carcinoma (2.4%), and malignant insulinoma (2.4%). The patients with acute inflammatory diseases were hospitalized due to gastrointestinal (66.7%), cardiopulmonary (14%), nephrological (7%), or unspecified inflammatory processes (10.5%).
The tumor patients underwent different chemotherapeutical treatments (Table 1).
Table 1.
Chemotherapeutic treatment characteristics
| Current chemotherapeutic drug regimen | Number of patients (n = 26) |
|---|---|
| FOLFIRI ((FOLinic acid, Fluoruracil (5-FU), IRInotecan) | 10 |
| FLOT (Fluoruracil, Leucovorin, Oxaliplatin, doxeTaxel) /Cisplatin | 4 |
| FOLFOX (FOLinic acid, Fluoruracil (5-FU), OXaliplatin | 2 |
| Cisplatin, Trastuzumab | 2 |
| Gemcitabine, Cis-/oxaliplatin | 2 |
| Oxaliplatin | 1 |
| Cisplatin, Etoposide | 1 |
| Oxaliplatin, 5-FU, Leucovorin, Irinotecan | 1 |
| Gemcitabine, 5-FU, Leukovoril | 1 |
| Capecitabine, Lapatinib | 1 |
| Others | 1 |
| Monoclonal antibodies (Bevacizumab, Panitumumab, Trastuzumab, Lapatinib) | 11 |
Taste tests
The three study groups were tested and compared regarding their detection and recognition thresholds for the five basic tastants.
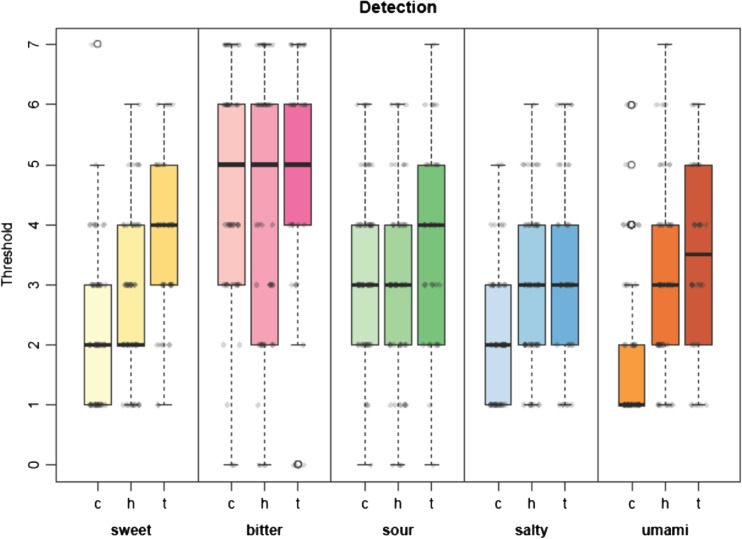
Analyzing the complete collectives, a significantly higher detection threshold of the tastants sweet (p value (adj.) = 0.004), salty (p value (adj.) = 0.021), and umami (p value (adj.) < 0.001) could be detected in the tumor group versus the healthy control group.
When comparing cancer patients with hospitalized patients suffering from benign inflammatory disease, a significantly increased detection threshold could be shown only in the tumor group for the tastants sweet (p value (adj.) = 0.004) and sour (p value (adj.) = 0.039). On the other hand, the hospitalized patients with inflammatory disease exhibited a higher detection threshold for umami (p value (adj.) = 0.002) compared to the control group (Fig. 1).
Fig. 1.
Detection threshold—comparison of the three groups. c control group, h hospitalized group, t tumor group. p values (Kruskal-Wallis rank sum test): p kw. p values (adjusted by Holm-Bonferroni): p ch = control group vs. hospitalized group, p ct = control group vs. tumor group, p ht = hospitalized group vs. tumor group. 1. Sweet: p kw = 0.00151. c vs. h, c vs. t, h vs. t. p values: p ch = 0.985, p ct = 0.004, p ht = 0.004. Numbers of subjects taken into account / n value: n c = 63, n h = 57, n t = 38. 2. Bitter: p kw = 0.492. c vs. h, c vs. t, h vs. t. p values: p ch = 0.846, p ct = 0.846, p ht = 0.846. Numbers of subjects taken into account / n value: n c = 63, n h = 57, n t = 38. 3. Sour: p kw = 0.0249. c vs. h, c vs. t, h vs. t. p values: p ch = 0.103, p ct = 0.507, p ht = 0.039. Numbers of subjects taken into account / n value: n c = 63, n h = 57, n t = 38. 4. Salty: p kw = 0.02. c vs. h, c vs. t, h vs. t. p values: p ch = 0.098, p ct = 0.021, p ht = 0.243. Numbers of subjects taken into account / n value: n c = 63, n h = 57, n t = 38. 5. Umami: p kw = 0.000216. c vs. h, c vs. t, h vs. t. p values: p ch = 0.002, p ct < 0.001, p ht = 0.150. Numbers of subjects taken into account / n value: n c = 63, n h = 56, n t = 38
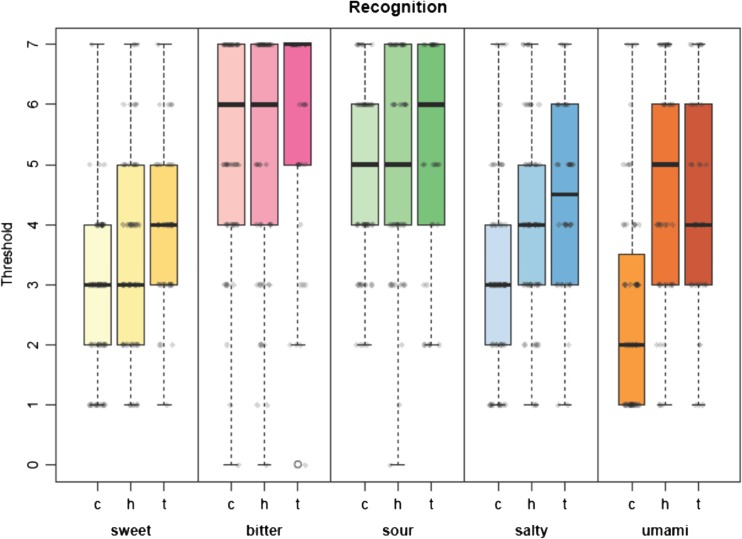
The recognition threshold (Fig. 2) was significantly elevated in the tumor group in comparison to the healthy control group for the tastants sweet (p value (adj.) = 0.024), salty (p value (adj.) = 0.031), and umami (p value (adj.) = 0.007).
Fig. 2.
Recognition threshold—comparison of the three groups. c control group, h hospitalized group, t tumor group. p values (Kruskal-Wallis rank sum test): p kw. p values (adjusted by Holm-Bonferroni): p ch = control group vs. hospitalized group, p ct = control group vs. tumor group, p ht = hospitalized group vs. tumor group. 1. Sweet: p kw = 0.0505. c vs. h, c vs. t, h vs. t. p values: p ch = 0.384, p ct = 0.024, p ht = 0.384. Numbers of subjects taken into account / n value: n c = 39, n h = 57, n t = 38. 2. Bitter: pkw = 0.594. c vs. h, c vs. t, h vs. t. p values: p ch = 1.0, p ct = 1.0, p ht = 1.0. Numbers of subjects taken into account / n value: n c = 39, n h = 57, n t = 38. 3. Sour: p kw = 0.754. c vs. h, c vs. t, h vs. t. p values: p ch = 1.0, p ct = 1.0, p ht = 1.0. Numbers of subjects taken into account / n value: n c = 39, n h = 57, n t = 38. 4. Salty: p kw = 0.0432. c vs. h, c vs. t, h vs. t. p values: p ch = 0.243, p ct = 0.031, p ht = 0.278. Numbers of subjects taken into account / n value: n c = 39, n h = 57, n t = 38. 5. Umami: p kw = 0.000148. c vs. h, c vs. t, h vs. t. p values: p ch < 0.001, p ct = 0.007, p ht = 0.272. Numbers of subjects taken into account / n value: n c = 39, n h = 56, n t = 38
The acutely hospitalized group differed significantly from the control group only in the recognition of umami (p value (adj.) < 0.001).
Comparative analysis of the recognition of the other tastants between the three groups showed differences below significance or no difference.
Furthermore, we could not see any significant difference between cancer patients who were currently receiving chemotherapy, who had been treated with chemotherapeutic agents in the past, or who were chemotherapy-naïve (Figs. 3 and 4).
Fig. 3.
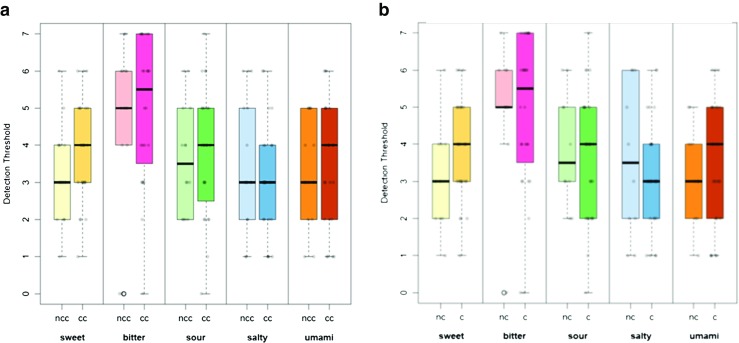
Detection thresholds. (a) Influence of current chemotherapeutical treatment. Detection thresholds of patients receiving current chemotherapy vs. patients currently not receiving chemotherapy. cc current chemotherapy, ncc no current chemotherapy. n value: n cc = 24, n ncc = 14. Wilcoxon-Mann-Whitney test: Significance levels: 1. Sweet: p cc/ncc = 0.238, W = 129. 2. Bitter: p cc/ncc = 0.814, W = 160. 3. Sour: p cc/ncc = 0.643, W = 152.5. 4. Salty: p cc/ncc = 0.454, W = 193. 5. Umami: p cc/ncc = 0.701, W = 155. (b) Influence of chemotherapeutical treatment. Detection threshold of chemotherapeutically treated patients vs. chemotherapy-naïve patients. c chemotherapy, nc no chemotherapy (chemotherapy-naïve). n value: n c = 28, n nc = 10. Wilcoxon-Mann-Whitney test: Significance levels: 1. Sweet: p c/nc = 0,151, W = 97. Bitter: p c/nc = 0.941, W = 137.5. Sour: p c/nc = 0.81, W = 147.5. Salty: p c/nc = 0.602, W = 156. Umami: p c/nc = 0.581, W = 123
Fig. 4.
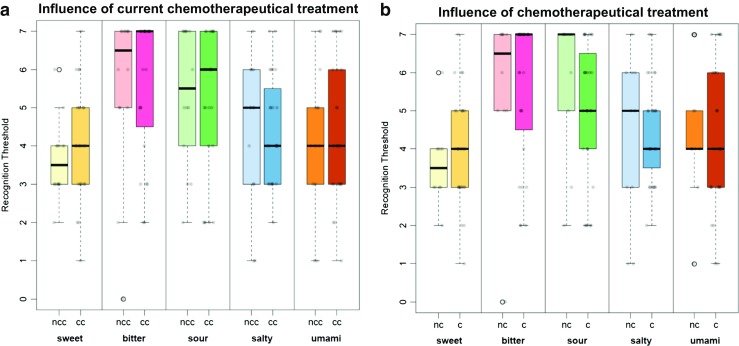
Recognition thresholds. (a) Influence of current chemotherapeutical treatment. Recognition threshold of patients receiving current chemotherapy vs. patients currently not receiving chemotherapy. cc current chemotherapy, ncc no current chemotherapy. n value: n cc = 24, n ncc = 14. Wilcoxon-Mann-Whitney test: Significance levels: 1. Sweet: p cc/ncc = 0.266, W = 131,5. 2. Bitter: p cc/ncc = 0.958, W = 166. 3. Sour: p cc/ncc = 0.661, W = 182.5. 4. Salty: p cc/ncc = 0.687, W = 181.5. 5. Umami: p cc/ncc = 0.922, W = 164.5. (b) Influence of chemotherapeutical treatment. Recognition threshold of chemotherpeutically treated patients vs. chemotherapy-naïve patients. c chemotherapy, nc no chemotherapy (chemotherapy-naïve). n value: n c = 28, n nc = 10. Wilcoxon-Mann-Whitney test: Significance levels: 1. Sweet: p c/nc = 0.31, W = 109.5. 2. Bitter: p c/nc = 1, W = 139.5. 3. Sour: p c/nc = 0.126, W = 185. 4. Salty: p c/nc = 0.895, W = 144. 5. Umami: p c/nc = 0.786, W = 148.5
If the line number of chemotherapeutic interventions the patients had previously received was taken into account, no significant differences between a first-line therapy and additional therapy lines were determined in the detection thresholds (pchemotherapy line (pcli) = 0.561, bitter: pcli = 0.117, sour: pcli = 0.848, salty: pcli = 0.87, umami: pcli = 0.611). Moreover, there was no difference in the detection thresholds caused by the number of performed chemotherapy cycles.
Regarding the inflammatory parameters CRP and leukocytes, we did not observe an effect on the taste perception of the tumor patients.
Lower albumin values, however, significantly increased the detection threshold for salty (p value = 0.002115). The median detection threshold ± [interquartile range] was 4 [2] (low albumin, < 35 [g/l], (n = 9)) and 3 [1] (normal albumin, > 35 [g/l], (n = 17)).
Regarding the other tastants, there were no differences in detection or recognition thresholds.
Olfactory test
The study participants did not show relevant olfactory or smell disturbance effects.
Discussion
The objective of this study was to examine the influence of cancer and inflammatory disease on the taste perception of patients. Primarily, we demonstrated that the incidence of taste disturbance is elevated in cancer patients. Hence, we were interested to identify triggering factors for this taste disturbance. Is the tumor therapy the sole reason for taste perception impairment or is the underlying disease partly involved? Therefore, we compared the taste sense of cancer patients undergoing chemotherapeutical treatment with the taste sense of patients without chemotherapy.
For the first time, we could demonstrate that the taste disturbance in cancer patients might not only be dependent on chemotherapeutical treatment. We determined no significant differences between patients with or without chemotherapeutical treatment. In addition, the number of performed treatment lines and cycles of chemotherapy did not significantly influence taste perception.
However, cancer patients and hospitalized patients with inflammatory disease showed a disturbed taste perception compared to healthy controls. Comparing acutely hospitalized and tumor patients with healthy controls, umami was significantly less perceived in both patient groups (detection and recognition thresholds). Cancer patients also had higher detection and recognition thresholds for sweet and salty than healthy controls. Regarding the tastants sweet and sour, the taste disturbances in cancer patients compared to hospitalized patients were also significantly more pronounced. Similar correlations have not been described before, since a comparative analysis of tumor patients and acutely hospitalized patients with inflammatory diseases has never been performed.
Interestingly, the inflammatory status as recorded with CRP values and the leukocyte count had no influence on taste disturbance (Table 2). Instead, tumor patients with reduced albumin values exhibited a diminished detection for salty.
Table 2.
Inflammatory parameters (means ± standard deviation, Mann-Whitney U test)
| Parameter | Hospitalized patients (n) | Tumor patients (n) | Significance p value |
|---|---|---|---|
| CRP [mg/l] | 36.93 ± 75.47 (52) | 23.01 ± 30.04 (30) | 0.363 |
| Leukocytes [10^3/μl] | 7.38 ± 2.65 (56) | 6.45 ± 2.62 (38) | 0.155 |
| Albumin [g/l] | – | 37.13 ± 5.77 (29) | – |
n number of patients
The reason why the detection and recognition of sour and bitter did not differ significantly between cancer patients and healthy controls can in part be explained by our finding that the thresholds for these two tastants are generally high in all groups. For future studies, it is recommended to examine even higher maximal concentrations for these two tastants. In contrast to our findings, there is evidence in the literature for disturbed detection of bitter in cancer patients [14]. Some studies indicate that bitter taste could potentially be regulated via tumor necrosis factor (TNF) signaling pathways. Thus, a higher concentration of TNF due to inflammatory processes and tumor disease could lead to reduced thresholds for bitter [7].
The fact that there is a taste disturbance in both, cancer patients and patients with inflammatory disorders, suggests that the deterioration of taste perception is due to systemic inflammation. Since cancer-induced inflammatory processes are more complex and more pronounced than the inflammation process in acute benign inflammatory disease, taste deterioration is possibly more severe in cancer patients.
It is known that inflammation-related changes in the interferon and the toll-like receptor pathway negatively affect the renewal of taste bud cells [28]. Further, lipopolysaccharide (LPS)-induced inflammation leads to a reduced proliferation of taste progenitor cells and shortens the lifespan of taste bud cells [29]. Since CRP values and leukocyte count had no impact on taste detection, other inflammatory mechanisms are likely to cause taste disturbances. Since the abovementioned toll-like receptor pathway is known to affect the course of a tumor disease [30], it might also affect taste sensation. However, in the course of a tumor disease, many pro-inflammatory cytokines are released inducing inflammation processes that might contribute to taste disturbances by disrupting various phases of taste cell differentiation or degradation.
The influence of chemotherapeutics on taste sensation is often blamed for the reduced dietary intake of cancer patients. Attributed to chemotherapeutics are increased detection thresholds for sweet, sour, salty, or bitter [18], as well as a constant perception of a metallic taste [31, 32]. An impairment of the taste buds by cytotoxic substances and a disturbance of the renewal processes of taste bud cells are discussed as possible consequences of chemotherapeutic agents leading to taste disturbances [33, 34].
A remarkable finding of our study is that the taste perception of patients with current or former chemotherapeutical treatment did not significantly differ from that of chemotherapy-naïve tumor patients (Figs. 3 and 4).
This means that chemotherapy seems not to have the anticipated clinically significant effect on taste, or at least not as strong as the effect of the tumorous process itself. We conclude from these data that the massive release of inflammatory factors in a cancer disease has probably a more relevant influence on taste perception than drug therapy with chemotherapeutics. This underlines the need for a systematic assessment of anorexia and weight loss in all cancer patients, regardless of the underlying therapy and tumor stage.
We could demonstrate that lower albumin values in tumor patients increased the detection threshold for salty. These results are supported by data from Lynch et al. showing an association between low serum albumin levels, low intake of sodium and protein, and increase of individual taste alterations [35]. Lowered albumin values originate from decreased synthesis in the liver, loss of protein, and malnutrition [36]. Thus, treating malnutrition by replenishing protein and albumin reservoirs could potentially improve taste disturbances [37]. However, this should be examined in detail in future studies.
The observed increased detection and recognition thresholds for umami in the acutely hospitalized as well as the tumor patients compared to healthy controls are remarkable since umami is considered as the signal for nutritious meals or protein-rich food [38]. The tastant umami develops when vegetables and meat are cooked or roasted because these processes release glutamate in food [39]. Foods such as Parmesan, smoked ham, or sundried tomatoes also contain large amounts of monosodium glutamate. As a predictor for the protein intake of a patient, the testing of glutamate could play an important role, since for humans umami indicates a nutritious protein source [40]. There might even be a correlation between a decreased umami perception and the reduced meat consumption of tumor patients. Since patients suffering from acute inflammatory diseases or cancer, perceive umami to a lesser extent as important taste modality of roasted or cooked meat, their desire for meat might be reduced as a consequence. Such a correlation has never been verified in a study. However, it is known that glutamate has a stimulating effect on appetite and saliva production [41]. When glutamate is elevated in a meal, the craving for salt and sugar is reduced. Thus, the addition of glutamate to a dish can not only increase its savory perception but may also contribute to a more healthy nutrition of elderly, ill, and tumor patients [39].
In order to collect data on taste alterations adequately, validated testing is inevitable. Established methods to determine taste senses can be divided into regional and “whole mouth methods” [42, 43]. Regional methods are applied when taste disturbances are already established. They allow conclusions about the nature of triggers on the neural level [33]. For tests of everyday taste perception, as intended in our study, more general, so called “whole-mouth methods” are suitable. One of the well-established “whole mouth methods” is the three-drop forced-choice method from Henkin et al. [42, 44]. Another method to detect taste perception in a more general manner and easier to apply than regional methods is a method using a device to spread tastant solutions around the entire tongue [25].
The DIN ISO 3972:2011 is well suited to standardize the preparation of tastant test solutions and has been used in other studies [9]. We observed that the concentrations for caffeine solutions could be even higher, since the tumor patients and the acutely hospitalized patients with inflammatory disease, frequently did not reach the detection thresholds of healthy subjects for bitter (Fig. 2). The application of pump sprays enables a relatively even distribution of tastant solutions around the entire tongue thereby avoiding the frequently strenuous sticking out of the tongue. Sprays have been used already in former screenings and are easy to apply [19].
Prospects
Since taste disturbances appear to have negative effects on appetite, nutrition intake, underlying disease, and on quality of life, early detection and treatment is of great importance. A potential approach is the treatment of protein malnutrition.
Food enhancement is much needed to treat taste disturbances before additional problems and complications arise, primarily malnutrition and major weight loss [5, 45]. This applies to tumor patients, acutely ill persons, and patients being malnourished due to other reasons. Besides glutamate, various other flavoring substances could be used to make meals more palatable to patients. This might increase the perception of a meal also through other sensory modalities.
Summary
This study could demonstrate that the capacity of tasting can deteriorate significantly during a tumor disease. This seems to be due not only to chemotherapeutic treatment but multiple other factors of the disease interacting with each other. These factors include inflammatory reactions, protein metabolism disturbances, and catabolic processes, which in part also occur in other acute diseases. In conjunction with taste disturbances, these factors can promote the development and maintenance of malnutrition leading to an impaired prognosis.
Acknowledgements
We thank Sarah Vogel for her support in taste test realization and Yvonne Sauermann for preparation of the tastant solutions.
Compliance with ethical standards
Ethical approval
All participants obtained a detailed description of the test systems and were enrolled in the study after signing a consent form. The study was approved by the ethics committee of the University of Erlangen and is in accordance with the 1964 Helsinki declaration and its later amendments.
References
- 1.Laviano A, Koverech A, Mari A. Cachexia: clinical features when inflammation drives malnutrition. Proc Nutr Soc. 2015;74(4):348–354. doi: 10.1017/S0029665115000117. [DOI] [PubMed] [Google Scholar]
- 2.Delano MJ, Moldawer LL. The origins of cachexia in acute and chronic inflammatory diseases. Nutr Clin Pract. 2006;21(1):68–81. doi: 10.1177/011542650602100168. [DOI] [PubMed] [Google Scholar]
- 3.Pressoir M, et al. Prevalence, risk factors and clinical implications of malnutrition in French comprehensive cancer centres. Br J Cancer. 2010;102(6):966–971. doi: 10.1038/sj.bjc.6605578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Maheswaran T, et al. Gustatory dysfunction. J Pharm Bioallied Sci. 2014;6(Suppl 1):S30–S33. doi: 10.4103/0975-7406.137257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Toffanello ED, et al. Taste loss in hospitalized multimorbid elderly subjects. Clin Interv Aging. 2013;8:167–174. doi: 10.2147/CIA.S37477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Holmes S. Food avoidance in patients undergoing cancer chemotherapy. Support Care Cancer. 1993;1(6):326–330. doi: 10.1007/BF00364971. [DOI] [PubMed] [Google Scholar]
- 7.Feng P, et al. Regulation of bitter taste responses by tumor necrosis factor. Brain Behav Immun. 2015;49:32–42. doi: 10.1016/j.bbi.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zopf Y, et al. Alterations of taste perception in Crohn’s disease and their dependency on disease activity and nutritional behavior. J Clin Gastroenterol. 2009;43(7):617–621. doi: 10.1097/MCG.0b013e31818acf91. [DOI] [PubMed] [Google Scholar]
- 9.Boltong A, et al. A prospective cohort study of the effects of adjuvant breast cancer chemotherapy on taste function, food liking, appetite and associated nutritional outcomes. PLoS One. 2014;9(7):e103512. doi: 10.1371/journal.pone.0103512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaughan VC, Martin P, Lewandowski PA. Cancer cachexia: impact, mechanisms and emerging treatments. J Cachexia Sarcopenia Muscle. 2013;4(2):95–109. doi: 10.1007/s13539-012-0087-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Zabernigg A, et al. Taste alterations in cancer patients receiving chemotherapy: a neglected side effect? Oncologist. 2010;15(8):913–920. doi: 10.1634/theoncologist.2009-0333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zopf Y, Herrmann HJ. Principles of cachexia in tumor patients. Onkologe. 2016;22(4):8. doi: 10.1007/s00761-016-0013-9. [DOI] [Google Scholar]
- 13.Berteretche MV, et al. Decreased taste sensitivity in cancer patients under chemotherapy. Support Care Cancer. 2004;12(8):571–576. doi: 10.1007/s00520-004-0589-2. [DOI] [PubMed] [Google Scholar]
- 14.Steinbach S, et al. Qualitative and quantitative assessment of taste and smell changes in patients undergoing chemotherapy for breast cancer or gynecologic malignancies. J Clin Oncol. 2009;27(11):1899–1905. doi: 10.1200/JCO.2008.19.2690. [DOI] [PubMed] [Google Scholar]
- 15.Sandow PL, Hejrat-Yazdi M, Heft MW. Taste loss and recovery following radiation therapy. J Dent Res. 2006;85(7):608–611. doi: 10.1177/154405910608500705. [DOI] [PubMed] [Google Scholar]
- 16.Jensen SB, et al. Oral mucosal lesions, microbial changes, and taste disturbances induced by adjuvant chemotherapy in breast cancer patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;106(2):217–226. doi: 10.1016/j.tripleo.2008.04.003. [DOI] [PubMed] [Google Scholar]
- 17.Squier CA, Kremer MJ. Biology of oral mucosa and esophagus. J Natl Cancer Inst Monogr. 2001;29:7–15. doi: 10.1093/oxfordjournals.jncimonographs.a003443. [DOI] [PubMed] [Google Scholar]
- 18.Boltong A, Keast R. The influence of chemotherapy on taste perception and food hedonics: a systematic review. Cancer Treat Rev. 2012;38(2):152–163. doi: 10.1016/j.ctrv.2011.04.008. [DOI] [PubMed] [Google Scholar]
- 19.Welge L et al (2004) Schmeckstörungen—Ursachen. Diagnostik und Therapie Therapeutische Umschau 61(5):302–307 [DOI] [PubMed]
- 20.Boltong A, Keast RS, Aranda SK. A matter of taste: making the distinction between taste and flavor is essential for improving management of dysgeusia. Support Care Cancer. 2011;19(4):441–442. doi: 10.1007/s00520-011-1085-0. [DOI] [PubMed] [Google Scholar]
- 21.Mojet J, Christ-Hazelhof E, Heidema J. Taste perception with age: generic or specific losses in threshold sensitivity to the five basic tastes? Chem Senses. 2001;26(7):845–860. doi: 10.1093/chemse/26.7.845. [DOI] [PubMed] [Google Scholar]
- 22.Thomas, L.V. and J. Delves-Broughton, PRESERVATIVES | Permitted Preservatives—Sorbic Acid, in Encyclopedia of Food Microbiology (Second Edition), C.A.B.L. Tortorello, Editor. 2014, Academic Press: Oxford p 102-107
- 23.DIN Deutsches Institut für Normung e. V., DIN ISO 3972:2012–07. 2012
- 24.Mojet J, Köster EP, Prinz JF. Do tastants have a smell? Chem Senses. 2005;30(1):9–21. doi: 10.1093/chemse/bjh251. [DOI] [PubMed] [Google Scholar]
- 25.Yamauchi, Y., et al., A new whole-mouth gustatory test procedure. 1. Thresholds and principal components analysis in healthy men and women. Acta Otolaryngol Suppl, 2002(546): p. 39–48 [DOI] [PubMed]
- 26.Epstein JB, Smutzer G, Doty RL. Understanding the impact of taste changes in oncology care. Support Care Cancer. 2016;24(4):1917–1931. doi: 10.1007/s00520-016-3083-8. [DOI] [PubMed] [Google Scholar]
- 27.R CoreTeam (2017) R: a language and environment for statistical computing. R Foundation for Statistical Computing, Vienna
- 28.Wang H, et al. Inflammation and taste disorders: mechanisms in taste buds. Ann N Y Acad Sci. 2009;1170:596–603. doi: 10.1111/j.1749-6632.2009.04480.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Cohn ZJ, et al. Lipopolysaccharide-induced inflammation attenuates taste progenitor cell proliferation and shortens the life span of taste bud cells. BMC Neurosci. 2010;11:72. doi: 10.1186/1471-2202-11-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yeh DW, et al. Interplay between inflammation and stemness in cancer cells: the role of toll-like receptor signaling. J Immunol Res. 2016;2016:4368101. doi: 10.1155/2016/4368101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jpma I I et al., Metallic taste in cancer patients treated with chemotherapy. Cancer Treat Rev, 2015. 41(2): p. 179–86 [DOI] [PubMed]
- 32.Gamper EM, et al. Coming to your senses: detecting taste and smell alterations in chemotherapy patients. A systematic review. J Pain Symptom Manag. 2012;44(6):880–895. doi: 10.1016/j.jpainsymman.2011.11.011. [DOI] [PubMed] [Google Scholar]
- 33.Barlow LA. Progress and renewal in gustation: new insights into taste bud development. Development. 2015;142(21):3620–3629. doi: 10.1242/dev.120394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Feng P, Huang L, Wang H. Taste bud homeostasis in health, disease, and aging. Chem Senses. 2014;39(1):3–16. doi: 10.1093/chemse/bjt059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lynch, K.E., et al., Altered taste perception and nutritional status among hemodialysis patients. J Ren Nutr, 2013. 23(4): p. 288–295.e1 [DOI] [PMC free article] [PubMed]
- 36.Tanriverdi O. A discussion of serum albumin level in advanced-stage hepatocellular carcinoma: a medical oncologist’s perspective. Med Oncol. 2014;31(11):282. doi: 10.1007/s12032-014-0282-3. [DOI] [PubMed] [Google Scholar]
- 37.Tsutsumi R, et al. Albumin-normalized serum zinc: a clinically useful parameter for detecting taste impairment in patients undergoing dialysis. Nutr Res. 2014;34(1):11–16. doi: 10.1016/j.nutres.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 38.de Araujo IE, et al. Representation of umami taste in the human brain. J Neurophysiol. 2003;90(1):313–319. doi: 10.1152/jn.00669.2002. [DOI] [PubMed] [Google Scholar]
- 39.Mouritsen OG. Umami flavour as a means of regulating food intake and improving nutrition and health. Nutr Health. 2012;21(1):56–75. doi: 10.1177/0260106012445537. [DOI] [PubMed] [Google Scholar]
- 40.Masic U, Yeomans MR. Monosodium glutamate delivered in a protein-rich soup improves subsequent energy compensation. J Nutr Sci. 2014;3:e15. doi: 10.1017/jns.2014.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Uneyama H, et al. Contribution of umami taste substances in human salivation during meal. J Med Investig. 2009;56(Suppl):197–204. doi: 10.2152/jmi.56.197. [DOI] [PubMed] [Google Scholar]
- 42.Ahne G, et al. Assessment of gustatory function by means of tasting tablets. Laryngoscope. 2000;110(8):1396–1401. doi: 10.1097/00005537-200008000-00033. [DOI] [PubMed] [Google Scholar]
- 43.Hummel, T., B.N. Landis, and K.B. Huttenbrink, Smell and taste disorders. GMS Curr Top Otorhinolaryngol Head Neck Surg, 2011. 10: p. Doc04 [DOI] [PMC free article] [PubMed]
- 44.Henkin RI, Gill JR, Jr, Bartter FC. Studies on taste thresholds in normal man and in patients with adrenal cortical insufficiency: the role of adrenal cortical steroids and of serum sodium concentration. J Clin Invest. 1963;42(5):727–735. doi: 10.1172/JCI104765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schiffman SS, et al. Combination of flavor enhancement and chemosensory education improves nutritional status in older cancer patients. J Nutr Health Aging. 2007;11(5):439–454. [PubMed] [Google Scholar]