Abstract
Background:
We investigated the role of prostaglandin receptors (e.g. prostaglandin E2 receptor 2 (EP2), EP4) and the efficacy of celecoxib in urothelial tumourigenesis and cancer progression.
Methods:
We performed immunohistochemistry in bladder cancer (BC) tissue microarrays, in vitro transformation assay in a normal urothelial SVHUC line, and western blot/reverse transcription–polymerase chain reaction/cell growth assays in BC lines.
Results:
EP2/EP4 expression was elevated in BCs compared with non-neoplastic urothelial tissues and in BCs from those who were resistant to cisplatin-based neoadjuvant chemotherapy. Strong positivity of EP2/EP4 in non-muscle-invasive tumours or positivity of EP2/EP4 in muscle-invasive tumours strongly correlated with disease progression or disease-specific mortality, respectively. In SVHUC cells, exposure to a chemical carcinogen 3-methylcholanthrene considerably increased and decreased the expression of EP2/EP4 and phosphatase and tensin homologue (PTEN), respectively. Treatment with selective EP2/EP4 antagonist or celecoxib also resulted in prevention in 3-methylcholanthrene-induced neoplastic transformation of SVHUC cells. In BC lines, EP2/EP4 antagonists and celecoxib effectively inhibited cell viability and migration, as well as augmented PTEN expression. Furthermore, these drugs enhanced the cytotoxic activity of cisplatin in BC cells. EP2/EP4 and PTEN were also elevated and reduced, respectively, in cisplatin-resistant BC sublines.
Conclusions:
EP2/EP4 activation correlates with induction of urothelial cancer initiation and outgrowth, as well as chemoresistance, presumably via downregulating PTEN expression.
Keywords: chemoresistance, EP2, EP4, immunohistochemistry, PTEN, tumour progression, neoplastic transformation, urothelial cancer
Urinary bladder cancer (BC), mostly urothelial carcinoma, is one of the most frequently diagnosed neoplasms (Siegel et al, 2017). There are two distinct forms of BCs: non-muscle- and muscle-invasive diseases. Patients with the former carry a life-long risk of disease recurrence following transurethral tumour resection and currently available intravesical pharmacotherapy, whereas those with the latter are at a high risk of developing disease progression and metastasis even following more aggressive treatment including radical cystectomy with or without cisplatin (cis-diamminedichloroplatinum(II); CDDP)-based neoadjuvant/adjuvant systemic chemotherapy. Accordingly, identification of key molecules or pathways responsible for the development and/or progression of BC, as well as drug resistance, may offer targeted therapy to improve patient outcomes.
Prolonged inflammation is known to associate with the development of various malignancies including BC (Coussens and Werb, 2002). It has been documented that the expression of cyclooxygenase-2 (COX-2), an inducible enzyme that converts arachidonic acid into prostaglandins, specifically prostaglandin E2 (PGE2), is elevated in urothelial carcinomas of the bladder (Mohammed et al, 1999) and upper urinary tract (Jeon et al, 2010). Prostaglandin E2 has indeed been shown to play a central role in not only inflammation but also cell proliferation as an antiapoptotic molecule (Lin et al, 2001). Therefore, inhibition of PGE2 is considered a possible anticancer strategy.
Prostaglandin E2 exerts its effects via G-protein-coupled receptors (GPCRs), including PGE2 receptor 2 (EP2), EP3, and EP4. EP2 and EP4 are coupled with G protein and increase the intracellular cyclic adenosine monophosphate, whereas EP3 is coupled with an inhibitory G protein and decreases it (Dorsam and Gutkind, 2007). EP2 and EP4 are also known to be activated by other prostaglandins, such as PGE1, PGF2α, PGI2, and PGD2 (Narumiya et al, 1999). Meanwhile, non-steroidal anti-inflammatory drugs (NSAIDs) inhibit COXs, which is the primary mechanism of antitumour activity, although their COX-independent effects are documented (Gurpinar et al, 2014). For instance, in prostate cancer lines, NSAIDs, including COX-2-selective celecoxib, have been shown to inhibit cell growth via modulation of EP2 or EP3 signals (Kashiwagi et al, 2013, 2014). Nonetheless, it remains to be resolved whether and how GPCR signalling is involved in BC initiation and outgrowth. In the present study, we aimed to investigate the functional role of prostaglandin receptors, as well as the efficacy of celecoxib, in urothelial tumourigenesis and cancer progression.
Materials and methods
Chemicals
AH6809 (EP2 antagonist), butaprost (EP2 agonist), and CAY10598 (EP4 agonist) were purchased from Cayman Chemical (Ann Arbor, MI, USA). Celecoxib and ONO-AE3-208 (EP4 antagonist) were purchased from ChemScene (Monmouth Junction, NJ, USA) and BioVision (Milpitas, CA, USA), respectively. CDDP was obtained from Sigma-Aldrich (St Louis, MO, USA).
Cell lines
An immortalised human normal urothelial cell line (SVHUC) and human urothelial carcinoma cell lines (5637, UMUC3) were originally obtained from the American Type Culture Collection (Manassas, VA, USA). Another human urothelial carcinoma cell line (647V) was used in our previous studies (Zheng et al, 2011; Li et al, 2014; Kashiwagi et al, 2016). All these lines were recently authenticated, using GenePrint 10 System (Promega, Madison, WI, USA). SVHUC and 5637/UMUC3/647V were maintained in Kaighn’s modification of Ham’s F-12K (Mediatech, Manassas, VA, USA) and Dulbecco’s modified Eagle’s medium (Mediatech), respectively, supplemented with 10% foetal bovine serum (FBS) at 37 °C in a humidified atmosphere of 5% CO2.
In vitro transformation
We used a method for neoplastic transformation in SVHUC with exposure to a carcinogen 3-methylcholanthrene (MCA), as described in a previous study (Reznikoff et al, 1988), with minor modifications. Briefly, cells (2 × 106/10-cm culture dish incubated for 24 h) were cultured in serum-free F-12K containing 5 μg ml−1 MCA (Sigma-Aldrich). After the first 24 h of MCA exposure, FBS (1%) was added to the medium. After additional 24 h, the cells were cultured in medium containing 5% FBS without MCA until near confluence. Subcultured cells (1/3 split) were again cultured in the presence of MCA for a 48- h exposure period, using the above protocol. MCA exposure was repeated one more time. These cells were then subcultured for 6 weeks in the presence or absence of AH6809, ONO-AE3-208, or celecoxib, and thereafter used for further assays.
Tumour formation in vivo
The animal protocol in accordance with National Institutes of Health Guidelines for the Care and Use of Experimental Animals was approved by the Institutional Animal Care and Use Committee. SVHUC cells (1 × 106) exposed to MCA and subcultured with celecoxib, as described above, were suspended, mixed with 100 μl Matrigel (BD Biosciences, San Jose, CA, USA), and subcutaneously injected into the flank of 6-week-old male NOD-SCID mice (Johns Hopkins University Research Animal Resources), as described previously (Kawahara et al, 2016). Tumour formation was then monitored every day.
Western blot
Equal amounts of proteins (30 μg) obtained from cell extracts were subjected to sodium dodecyl sulphate–polyacrylamide gel electrophoresis, transferred to polyvinylidene difluoride membrane electronically, blocked, and incubated with a specific primary antibody (i.e. COX-2 (no. 160107; Cayman Chemical), EP2 (no. 101750; Cayman Chemical), EP3 (no. 101760; Cayman Chemical), EP4 (no. 101775; Cayman Chemical), GAPDH (6c5; Santa Cruz Biotechnology, Dallas, TX, USA), NF-κB (sc-109; Santa Cruz Biotechnology), p-NF-κB (Ser536; Cell Signalling Technology, Danvers, MA, USA), phosphatase and tensin homologue (PTEN) (D4.3; Cell Signalling Technology), Y-box binding protein-1 (YB-1) (EP2708Y; Epitomics, Burlingame, CA, USA), phospho-YB-1 (Ser102, Epitomics)). The membrane was then incubated with a secondary antibody, and specific signals were detected, using a LI-COR Imaging System (LI-COR, Lincoln, NE, USA).
MTT assay
Cells (2–6 × 103) seeded in 96-well plates were cultured for 72 h and then incubated with 0.5 mg ml−1 of MTT (Sigma-Aldrich) in 100 μl of medium for 3 h at 37 °C. MTT was dissolved by DMSO, and the absorbance was measured at a wavelength of 570 nm with background subtraction at 630 nm.
Plate colony formation assay
Cells (5 × 102) seeded in 12-well plates were allowed to grow until colonies in the control well were easily distinguishable. The cells were then fixed with methanol, stained with 0.1% crystal violet, and photographed. The numbers of colonies were quantitated using the ImageJ software (National Institutes of Health, Bethesda, MD, USA).
Scratch wound-healing assay
Cells at a density of 90–100% confluence in 12-well plates were scratched manually with a sterile 200 μl plastic pipette tip, cultured for 24 h, fixed with methanol, and stained with 0.1% crystal violet. The width of the wound area was quantitated, using the ImageJ.
Reverse transcription and real-time polymerase chain reaction
Total RNA isolated from cultured cells by TRIzol (Invitrogen, Carlsbad, CA, USA) was reverse transcribed, using 1 μmol l−1 oligo (dT) primers and four units of Ominiscript reverse transcriptase (Qiagen, Valencia, CA, USA). Real-time polymerase chain reaction (PCR) was then performed, using RT2 SYBR Green FAST Mastermix (Qiagen). The primer sequences are: 5′-GACTAATGCGTTCAGTCCTCTG-3′ (forward) and 5′-GGTCAGCCTGTTTACTGGCA-3′ (reverse) for EP2; 5′-CATCATCTGCGCCATGAGTGT-3′ (forward) and 5′-GCTTGTCCACGTAGTGGCT-3′ (reverse) for EP4; 5′-GTTTACCGGCAGCATCAAAT-3′ (forward) and 5′-CCCCCACTTTAGTGCACAGT-3′ (reverse) for PTEN; and 5′-TGTGGGCATCAATGGATTTGG-3′ (forward) and 5′-ACACCATGTATTCCGGGTCAAT-3′ (reverse) for GAPDH.
Small interfering RNAs
EP2 was silenced, using specific small interfering RNA (siRNAs), as described previously (Kashiwagi et al, 2014). Each siRNA (EP2-siRNA no. 1, 5′-UUCCUUUCGGGAAGAGGUUUCAUUC-3′ EP2-siRNA no. 2, 5′-AAUCCGACAACAGAGGACUGAACGC-3′ or negative control siRNA) purchased from Invitrogen was transfected into 647V and 5637 cells at various amounts, using Lipofectamine 2000 (Invitrogen), according to the manufacturer’s protocol.
Tissue microarray and immunohistochemistry
Two sets of tissue microarrays (TMAs) consisting of retrieved bladder tissue specimens obtained by transurethral resection performed at the Johns Hopkins Hospital were constructed previously upon appropriate approval from the institutional review board (Miyamoto et al, 2012). The first set consisted of 129 cases of urothelial neoplasm from 98 men and 31 women with a mean/median age of 65.7/69 years (range: 26–89), including 11 papillary urothelial neoplasms of low malignant potential, 40 non-invasive (pTa) low-grade urothelial carcinomas, 27 non-muscle-invasive (pTa/pT1) high-grade urothelial carcinomas, and 51 muscle-invasive (⩾pT2) high-grade urothelial carcinomas. All 51 patients with muscle-invasive tumour ultimately underwent radical cystectomy. Follow-up typically included repeat cystoscopy and urine cytology in those with non-muscle-invasive tumour, as well as imaging studies in those with muscle-invasive tumour after radical cystectomy, at standard intervals. A subset of patients underwent intravesical pharmacotherapy and/or neoadjuvant/adjuvant chemotherapy. The second set consisted of 37 cases of high-grade muscle-invasive urothelial carcinoma that received CDDP-based neoadjuvant chemotherapy (three cycles without dose deduction or ≥4 cycles) before cystectomy, including 16 responders and 21 non-responders to the neoadjuvant therapy, as defined previously (Miyamoto et al, 2012; Baras et al, 2015). None of the patients had received therapy with radiation or anticancer drugs before the collection of the tissues included in the TMAs.
Immunohistochemistry was performed on the sections (5 μm thick) from the bladder TMAs, using a primary antibody to EP2 (dilution 1 : 200), EP3 (dilution 1 : 200), or EP4 (dilution 1 : 200), and a broad-spectrum secondary antibody (Invitrogen), as described previously (Miyamoto et al, 2012; Kashiwagi et al, 2016). All stains were manually quantified by a single pathologist (H.M.) blinded to sample identify. The German immunoreactive scores calculated by multiplying the percentage of immunoreactive cells (0%=0; 1–10%=1; 11–50%=2; 51–80%=3; 81–100%=4) by staining intensity (negative=0; weak=1; moderate=2; strong=3) were considered negative (0; 0–1), weakly positive (1+ 2–4), moderately positive (2+ 6–8), and strongly positive (3+ 9–12).
Statistical analysis
Student’s t-test was used to analyse differences in variables with a continuous distribution. The Fisher’s exact test or χ2 test was used to evaluate the associations between categorised variables. Correlations between variables were determined by the Spearman’s correlation coefficient (CC). Survival rates in patients with non-muscle-invasive tumour with a mean (range) follow-up of 42.3 (4–173) months or those with muscle-invasive tumour with a mean (range) follow-up of 53.2 (3–268) months were calculated by the Kaplan–Meier method and comparison was made by log-rank test. In addition, the COX proportional hazards model (stepwise regression) was used to assess the prognostic indicators. P-values <0.05 were considered statistically significant.
Results
Expression of prostaglandin receptors in BC specimens
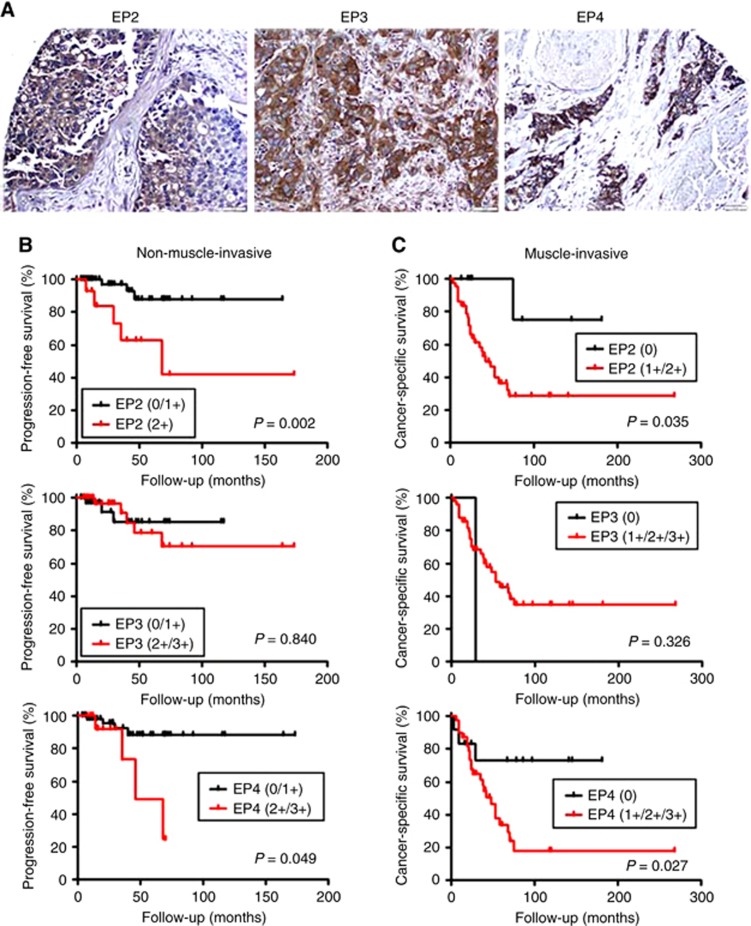
We first stained immunohistochemically for EP2, EP3, and EP4 in the bladder TMAs, consisting of 129 urothelial neoplasms and corresponding 87 non-neoplastic bladder tissues. Positive signals of respective receptors were detected predominantly in the cytoplasm of benign/malignant urothelial cells (Figure 1A).
Figure 1.
Immunohistochemistry of EP2, EP3, and EP4 in BC specimens. (A) Expression of EP2, EP3, and EP4 in BC (original magnification: × 200). Kaplan–Meier analyses for (B) progression-free survival in 78 patients with non-muscle-invasive tumour and (C) cancer-specific survival in 51 patients with muscle-invasive tumour, according to the levels of EP2/EP3/EP4 expression.
Table 1 summarises the status of receptor expression in non-neoplastic urothelium vs urothelial tumour tissues. Overall, the positive rates of EP2, EP3, and EP4 expression and their levels were significantly elevated in tumours, compared with benign urothelial tissues. In tumours, there were significant associations in the expression of EP2 vs EP4 (CC=0.209, P=0.017) and EP3 vs EP4 (CC=0.488, P<0.001), but not that of EP2 vs EP3 (CC=0.097, P=0.273). We next analysed the correlations of EP2/EP3/EP4 expression with the histopathological profile available for our patient cohort (Table 2). The positive rate of EP2 expression was significantly higher in high-grade (70.5%) or muscle-invasive (70.6%) tumours than in lower grade (31.4%) or non-muscle-invasive (44.9%) tumours, respectively. The positive rate of EP3 expression was also significantly elevated in muscle-invasive tumours (98.0%), compared with non-muscle-invasive tumours (79.5%). There were no significant correlations between EP4 expression and tumour grade or pT stage as well as between each receptor expression and the status of lymph node involvement.
Table 1. Expression of EP2, EP3, and EP4 in bladder tissue microarrays.
|
Expression levels |
P-value |
|||||||
|---|---|---|---|---|---|---|---|---|
| Negative |
Positive |
|||||||
| n | 0 | 1+ | 2+ | 3+ | 0 vs 1+/2+/3+ | 0/1+ vs 2+/3+ | 0/1+/2+ vs 3+ | |
|
EP2 | ||||||||
| Non-neoplastic urothelium | 87 | 76 (87.4%) | 11 (12.6%) | 0 (0%) | 0 (0%) | <0.001 | <0.001 | NA |
| Urothelial neoplasm | 129 | 58 (45.0%) | 57 (44.2%) | 14 (10.9%) | 0 (0%) | |||
|
EP3 | ||||||||
| Non-neoplastic urothelium | 87 | 26 (29.9%) | 23 (26.4%) | 22 (25.3%) | 16 (18.4%) | 0.003 | 0.039 | 0.401 |
| Urothelial neoplasm | 129 | 17 (13.2%) | 37 (28.7%) | 44 (34.1%) | 31 (24.0%) | |||
|
EP4 | ||||||||
| Non-neoplastic urothelium | 87 | 49 (56.3%) | 31 (35.6%) | 7 (8.0%) | 0 (0%) | <0.001 | <0.001 | 0.043 |
| Urothelial neoplasm | 129 | 34 (26.4%) | 59 (45.7%) | 29 (22.5%) | 7 (5.4%) | |||
Abbreviation: EP2=prostaglandin E2 receptor 2.
Table 2. Correlations between EP2/EP3/EP4 and histopathologic profile of the patients.
| EP2 expression | EP3 expression | EP4 expression | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Negative | Positive | Negative | Positive | Negative | Positive | |||||
| n | 0 | 1+/2+ | P-value | 0 | 1+/2+/3+ | P-value | 0 | 1+/2+/3+ | P-value | |
| Tumour grade | <0.001a | 0.289a | 0.840a | |||||||
| PUNLMP | 11 | 10 (90.9%) | 1 (9.1%) | 2 (18.2%) | 9 (81.8%) | 5 (45.5%) | 6 (54.5%) | |||
| Low-grade carcinoma | 40 | 25 (62.5%) | 15 (37.5%) | 7 (17.5%) | 33 (82.5%) | 9 (22.5%) | 31 (77.5%) | |||
| PUNLMP+Low-grade | 51 | 35 (68.6%) | 16 (31.4%) | 9 (17.6%) | 42 (82.4%) | 14 (27.5%) | 37 (72.5%) | |||
| High-grade carcinoma | 78 | 23 (29.5%) | 55 (70.5%) | 8 (10.3%) | 70 (89.7%) | 20 (25.6%) | 58 (74.4%) | |||
| Pathologic stage | 0.006b | 0.002b | 0.683b | |||||||
| pTa | 75 | 43 (57.3%) | 32 (42.7%) | 16 (21.3%) | 59 (78.7%) | 22 (29.3%) | 53 (70.7%) | |||
| pT1 | 3 | 0 (0%) | 3 (100%) | 0 (0%) | 3 (100%) | 0 (0%) | 3 (100%) | |||
| Non-muscle-invasive | 78 | 43 (55.1%) | 35 (44.9%) | 16 (20.5%) | 62 (79.5%) | 22 (28.2%) | 56 (71.8%) | |||
| pT2 | 19 | 5 (26.3%) | 14 (73.7%) | 0 (0%) | 19 (100%) | 5 (26.3%) | 14 (73.7%) | |||
| pT3 | 24 | 9 (37.5%) | 15 (62.5%) | 0 (0%) | 24 (100%) | 6 (25.0%) | 18 (75.0%) | |||
| pT4 | 8 | 1 (12.5%) | 7 (87.5%) | 1 (12.5%) | 7 (87.5%) | 1 (12.5%) | 7 (87.5%) | |||
| Muscle-invasive | 51 | 15 (29.4%) | 36 (70.6%) | 1 (2.0%) | 50 (98.0%) | 12 (23.5%) | 39 (76.5%) | |||
| LN involvement | 0.728 | 1.000 | 0.702 | |||||||
| pN0 | 35 | 11 (31.4%) | 24 (68.6%) | 1 (2.9%) | 34 (97.1%) | 9 (25.7%) | 26 (74.3%) | |||
| pN+ | 13 | 3 (23.1%) | 10 (76.9%) | 0 (0%) | 13 (100%) | 2 (15.4%) | 11 (84.6%) | |||
Abbreviations: EP2=prostaglandin E2 receptor 2; LN=lymph node; PUNLMP=papillary urothelial neoplasm of low malignant potential.
PUNLMP+low- grade vs high-grade.
Non-muscle-invasive vs muscle-invasive.
We then performed Kaplan–Meier analysis coupled with the log-rank test to assess possible associations between each receptor expression and patient outcomes. There were no significant differences in recurrence- or progression-free survival rate between EP2/EP3/EP4-positve vs EP2/EP3/EP4-negative non-muscle-invasive tumours. However, patients with EP2(2+) (P=0.002) or EP4(2+/3+) (P=0.049) non-muscle-invasive tumour had significantly higher risks of disease progression (Figure 1B). In patients with muscle-invasive tumour, there were significant associations between positivity of EP2 (P=0.035) or EP4 (P=0.027) and lower cancer-specific survival rates (Figure 1C). To determine whether EP2 or EP4 expression was an independent prognosticator, multivariate analysis was performed with Cox model (Supplementary Table S1). In non-muscle-invasive tumours, strong (2+/3+) EP2 or EP4 expression was not significantly (P>0.1) associated with disease progression. In muscle-invasive tumours, however, EP2 positivity (hazard ration (HR)=6.452, P=0.069) and EP4 positivity (HR=5.604, P=0.022) showed a trend towards significance and statistical significance, respectively, for cancer-specific mortality. These findings in our immunohistochemistry, including significant differences in their expression levels between non-neoplastic urothelium and urothelial neoplasm, suggested that activation of at least EP2 and EP4 might involve bladder tumourigenesis and cancer progression.
Effects of prostaglandin receptor inhibitors on neoplastic transformation of urothelial cells
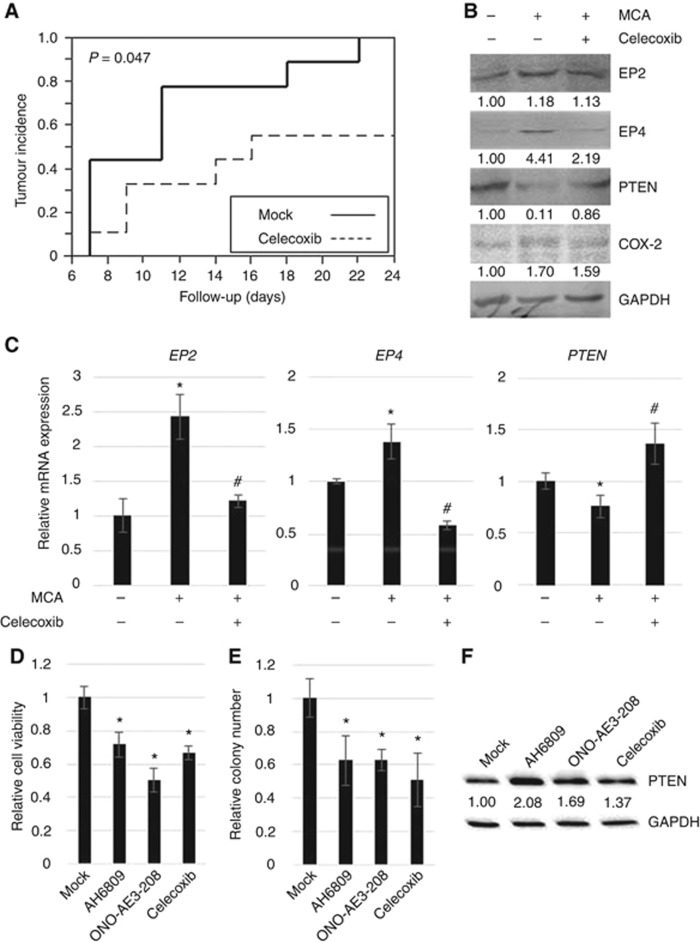
To assess the effects of celecoxib on urothelial tumourigenesis as well as the expression of prostaglandin receptors in urothelial cells, we used an in vitro transformation model in which non-neoplastic SHVUC cells could undergo stepwise transformation upon exposure to a chemical carcinogen MCA (Reznikoff et al, 1988). MCA-exposed SVHUC cells were treated with 1 μM celecoxib only during the process of neoplastic transformation (for 6 weeks). This dose of celecoxib did not affect the growth of SVHUC cells (Supplementary Figure S1). Tumourigenicity was then assessed, using a mouse xenograft model. SVHUC cells with MCA exposure and subsequent mock/celecoxib treatment were inoculated subcutaneously into immunocompromised mice, and tumour formation was monitored without further drug treatment. As expected, celecoxib treatment strikingly delayed or prevented the formation of xenograft tumours compared with mock treatment (Figure 2A).
Figure 2.
Effects of EP2/EP4 antagonists and celecoxib on neoplastic transformation of urothelial cells. (A) SVHUC cells exposed to MCA, subsequently cultured for 6 weeks with ethanol (mock) or celecoxib (1 μM), suspended, and mixed with Matrigel (1 × 106 cells/100 μl) were subcutaneously implanted into the flank of 6-week-old male NOD-SCID mice (n=11 in each group). The end point for this study was tumour formation without further drug treatment (exceeding 10 mm3 in its estimated volume (by the following formula: (short diameter)2 × (longest diameter) × 0.5) or 4 mm in greatest dimension). (B) Western blotting of EP2, EP4, COX-2, and PTEN using proteins extracted from SVHUC cells without MCA exposure and MCA-exposed SVHUC cells subsequently cultured for 6 weeks with ethanol or celecoxib (1 μM). Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) served as a loading control. Densitometry values for specific bands standardised by GAPDH that are relative to the value of mock treatment are included below the lanes. (C) Quantitative RT–PCR of EP2, EP4, and PTEN in SVHUC cells without MCA exposure and MCA-exposed SVHUC cells subsequently cultured for 6 weeks with ethanol or celecoxib (1 μM) were subjected to RNA extraction and subsequent real-time RT–PCR. Expression of EP2, EP4, or PTEN gene was normalised to that of GAPDH. Transcription amount is presented relative to that of control cells without MCA. SVHUC cells exposed to MCA and subsequently treated with ethanol (mock), AH6809 (1 μM), ONO-AE3-208 (1 μM), or celecoxib (1 μM) for 6 weeks were seeded for MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay (D; cultured for 72 h) or colony formation assay (E; cultured for 2 weeks). During these assays, AH6809, ONO-AE3-208, or celecoxib was not treated. Cell viability or the number of the colonies (⩾20 cells) is presented relative to that in mock-treated cells. Each value represents the mean (±s.d.) from at least three independent determinations. *P<0.05 (vs control without MCA). #P<0.05 (vs control with MCA). (F) Western blotting of PTEN using proteins extracted from MCA-exposed SVHUC cells subsequently cultured for 6 weeks with ethanol (mock) or celecoxib (1 μM). GAPDH served as a loading control. Densitometry values for PTEN standardised by GAPDH that are relative to the value of mock treatment are included below the lanes.
After 6 weeks of celecoxib treatment in SVHUC cells with the carcinogen challenge, we also compared the protein levels of EP2, EP4, and COX-2, as well as a tumour suppressor PTEN known to function as a central regulator of BC outgrowth (Abbosh et al, 2015) (Figure 2B). MCA exposure resulted in considerable increases in the expression of EP2, EP4, and COX-2. In addition, compared with mock treatment in MCA-SVHUC cells, celecoxib reduced their expression. Moreover, PTEN expression was downregulated by MCA-induced neoplastic transformation, which was reversed by celecoxib treatment. Correspondingly, using a quantitative reverse transcription (RT)–PCR analysis, increases in EP2/EP4 expression and a decrease in PTEN expression by MCA, as well as decreases in EP2/EP4 expression and an increase in PTEN expression by celecoxib, were confirmed at their mRNA levels (Figure 2C). Thus, celecoxib inhibited neoplastic transformation of urothelial cells as well as decreased and increased the expression levels of EP2/EP4 and PTEN, respectively, in these cells.
We also assessed the effects of selective EP2/EP4 antagonists on neoplastic transformation of urothelial cells, using the in vitro transformation model. MCA-exposed SVHUC cells were cultured in the presence of each antagonist for 6 weeks, and oncogenic activity was monitored by cell viability (MTT assay; Figure 2D) and colony formation (clonogenic assay; Figure 2E) without further drug treatment that could directly affect cell proliferation or colony formation. Thus, we compared the degree of neoplastic transformation in urothelial cells exposed to a carcinogen and subsequently cultured with EP2/EP4 antagonist or celecoxib, but did not intend to simply assess their effects on the growth of transformed cells. Both EP2 and EP4 antagonists, as well as celecoxib, could strongly inhibit neoplastic transformation of urothelial cells. In addition, western blotting in SVHUC cells undergoing neoplastic transformation showed increases in PTEN expression by EP2/EP4 antagonists (Figure 2F).
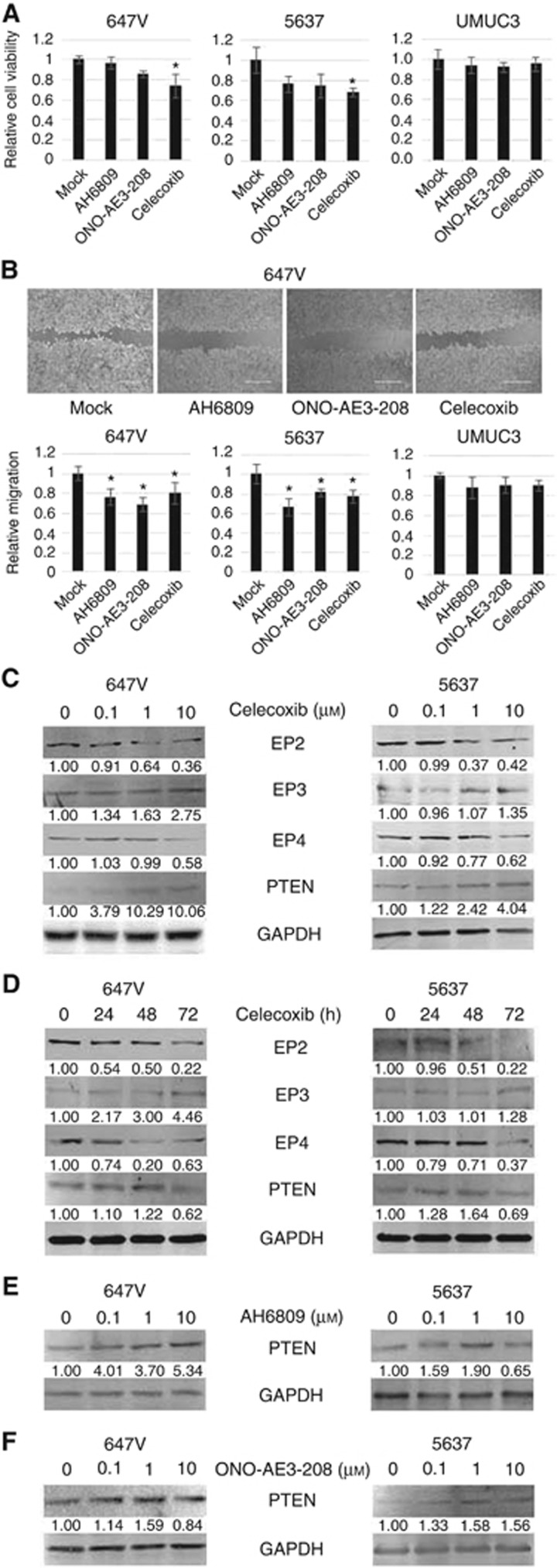
Effects of prostaglandin receptor inhibitors on BC cell proliferation and migration
To investigate whether celecoxib and EP2/EP4 antagonists have an antitumour activity in BC lines, we next compared cell viability in those cultured with each compound. After 72-h treatment, 10 μM celecoxib significantly inhibited the growth of 647V (27% decrease) and 5637 (32% decrease) cells, compared with mock treatment, whereas AH6809 (4–24% decrease at 10 μM) or ONO-AE3-208 (15–26% decrease at 10 μM) only marginally inhibited it (Figure 3A). We also performed a scratch would healing assay to assess the effects of celecoxib and EP2/EP4 antagonists on cell migration. AH6809 (24–34% decrease), ONO-AE3-208 (19–31% decrease), and celecoxib (20–23% decrease) significantly inhibited wound closure of 647V and 5637 cells 24 h after wound generation (Figure 3B). By contrast, celecoxib and EP2/EP4 antagonists did not show significant inhibitory effects on the viability and migration of PTEN-negative UMUC3 cells.
Figure 3.
Effects of EP2/EP4 antagonists and celecoxib on BC cell viability and migration. (A) MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay in 647V, 5637, and UMUC3 cells cultured with ethanol (mock), AH6809 (10 μM), ONO-AE3-208 (10 μM), or celecoxib (10 μM) for 72 h. Cell viability is presented relative to that of mock treatment in each line. (B) Wound healing assay in 647V, 5637, and UMUC3 cells. The cells grown to confluence were gently scratched and the wound area was measured after 24-h culture with ethanol (mock), AH6809 (10 μM), ONO-AE3-208 (10 μM), or celecoxib (10 μM). The migration determined by the rate of cells filling the wound area is presented relative to that of mock treatment in each line. Each value represents the mean (±s.d.) from at least three independent determinations. *P<0.05 (vs mock treatment). Western blotting of EP2, EP3, EP4, and PTEN using proteins extracted from 647V and 5637 cells cultured with (C) 0–10 μM of celecoxib for 48 h, (D) 1 μM of celecoxib for 0–72 h, (E) 0–10 μM of AH6809 for 48 h, or (F) 0–10 μM of ONO-AE3-208, as indicated. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH) served as a loading control. Densitometry values for specific bands standardised by GAPDH that are relative to those of mock treatment are included below the lanes.
We explored underlying mechanisms of the antitumour activity of celecoxib as well as EP2/EP4 antagonists in BC cells. Using western blotting, celecoxib was found to downregulate and upregulate the expression of EP2/EP4 and EP3, respectively, in dose- (Figure 3C) and time- (Figure 3D) dependent manners. In addition, celecoxib treatment resulted in increases in PTEN expression (peak at 48 h) in 647V and 5637 cells. Similarly, EP2 (Figure 3E) and EP4 (Figure 3F) antagonists at 1 or 10 μM induced PTEN expression in these cells.
Effects of EP2 modulation on BC cell migration and PTEN expression
To further study the functional role of prostaglandin receptors in the growth of BC, EP2-siRNAs were expressed in 647V and 5637 cells. As expected, the levels of EP2 expression were substantially lower in EP2-siRNA-expressing lines than in a control line (Supplementary Figure S2A). Moreover, transfection of each EP2-siRNA resulted in the upregulation of PTEN expression. In the wound healing assay, the migration of EP2-siRNA cells was significantly inhibited, compared with control cells (Supplementary Figure S2B). On the other hand, treatment with a selective EP2 agonist dose-dependently reduced PTEN expression in 5637 cells (Supplementary Figure S2C).
Role of prostaglandin receptors in chemosensitivity in BC cells
In our previous study (Kashiwagi et al, 2016), we used a CDDP-resistant 647V subline (647V-CR). Similarly, we established the 5637-CR subline by long-term (i.e. >12 weeks) culture with low/increasing doses of CDDP. Using these sublines, we investigated the expression of EP2/EP3/EP4 as well as YB-1 whose activation has been implicated in acquisition of CDDP resistance in BC cells (Shiota et al, 2011). Compared with respective control sublines, the expression levels of EP2, EP4, YB-1, and its phosphorylated form (p-YB-1) were elevated in 647V-CR and 5637-CR (Supplementary Figure S3). On the other hand, EP3 (only in 5637-CR) and PTEN expression were reduced in CDDP-resistant cells. These findings suggested that EP2 and EP4 signals were involved in chemosensitivity in BC cells.
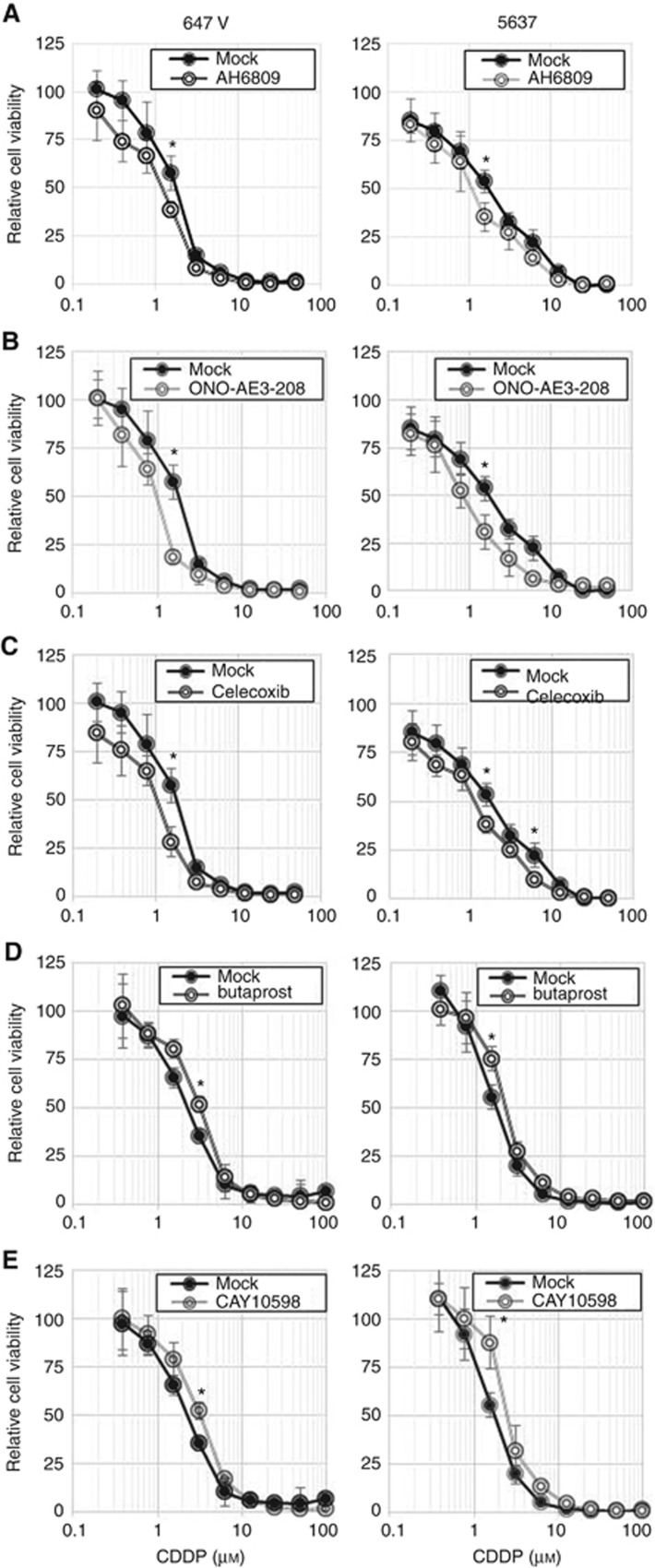
MTT assay was then performed to assess the effects of EP2/EP4 antagonists and agonists on the cytotoxic activity of CDDP in BC cells. Treatment with EP2 antagonist (Figure 4A), EP4 antagonist (Figure 4B), or celecoxib (Figure 4C) each at 1 μM resulted in considerable increases in CDDP sensitivity. By contrast, EP2 (Figure 4D) or EP4 (Figure 4E) agonist-treated cells were resistant to CDDP. In these experiments, the effects of the drugs on cell viability, irrespective of CDDP, was excluded by comparing with respective controls without CDDP treatment. Western blotting further showed that EP2 antagonist (Supplementary Figure S4A), EP4 antagonist (Supplementary Figure S4B), and/or celecoxib (Supplementary Figure S4C) could reduce the expression of YB-1 and p-YB-1 as well as NF-κB and p-NF-κB that were known to play a critical role in chemoresistance in BC cells (Ito et al, 2015; Kashiwagi et al, 2016).
Figure 4.
Effects of EP2/EP4 antagonists/agonists and celecoxib on the cytotoxicity of CDDP in BC cells. MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide) assay in 647V and 5637 cells cultured with ethanol (mock) vs AH6809 (1 μM; A), ONO-AE3-208 (1 μM; B), celecoxib (1 μM; C), butaprost (1 μM; D), or CAY10598 (1 μM; E), and different concentrations (0–50 μM) of CDDP for 72 h. Cell viability is presented relative to that of each line/treatment without CDDP. Each value represents the mean (±s.d.) from at least three independent determinations. *P<0.05 (vs mock treatment).
Correlations of EP2/EP4 expression with chemoresistance in BC patients
Finally, we immunohistochemically stained again for EP2 and EP4 in our TMA consisting of muscle-invasive BC specimens from patients who subsequently received CDDP-based neoadjuvant chemotherapy. We then compared their expression levels between responders vs non-responders to chemotherapy (Supplementary Table S2). Overall, EP2 was positive in 31 (83.8%) of 37 cases, including 11 (68.8%) of 16 responders vs 20 (95.2%) of 21 non-responders. Similarly, EP4 was positive in 30 (81.1%) of 37 cases, including 11 (68.8%) of 16 responders vs 19 (90.5%) of 21 non-responders. Thus, positivity of EP2 (P=0.030) or EP4 (P=0.095) was significantly or marginally, respectively, associated with chemoresistance.
Discussion
The relationship between inflammation and cancer has been extensively explored, and it is now well known that persistent inflammation can induce tumourigenesis in various organs, including the bladder (Coussens and Werb, 2002). Celecoxib has also been found to downregulate antiapoptotic proteins (Jendrossek, 2013), such as survivin and Bcl-2, and inhibit cell cycle progression by upregulating p21 and p27 (Liu et al, 2009). Correspondingly, in animal models, celecoxib has been shown to prevent gastric (Hu et al, 2004) and pancreatic (Arjona-Sánchez et al, 2010) carcinogenesis. In a prospective study involving 6729 men undergoing prostate biopsy, the use of aspirin and/or NSAIDs was also associated with significantly lower risks of cancer detection (Vidal et al, 2015). Meanwhile, knockdown of EP2 in mice resulted in significant decreases in lung (Keith et al, 2006) or colon (Ma et al, 2015) tumour formation, whereas treatment with selective EP2 (Ma et al, 2015) or EP4 (Mutoh et al, 2002) inhibitor prevented colon tumourigenesis. We here found that chemical carcinogen exposure to non-neoplastic urothelial cells induced EP2/EP4 expression and that celecoxib as well as EP2/EP4 inhibitors similarly prevented their neoplastic transformation via monitoring cell viability, colony formation, and tumour formation in mice (celecoxib only). Again, we did not assess the effects of these drugs on the growth of MCA-exposed cells, which rather represented the degree of neoplastic transformation. These observations suggest that EP2 and EP4 contribute to induction of urothelial cancer initiation. Indeed, in a murine model, a chemical carcinogen, N-butyl-N-(4-hydroxybutyl)-nitrosamine, induced EP2/EP4 gene expression in the bladder before the development of invasive cancer (Taylor et al, 2009). Moreover, a pilot study in 124 patients with non-muscle-invasive BC showed marginally better effects of oral celecoxib on tumour recurrence, compared with intravesical mitomycin C therapy (median disease-free interval: 67 vs 41 months; P=0.25) currently used as a chemopreventive option (Pagliarulo et al, 2015). Further studies are still required to determine how EP2/EP4 signals regulate urothelial carcinogenesis.
EP2 and EP4 signals have also been implicated in cell proliferation/migration and metastasis in several types of malignancies (Castellone et al, 2005; Ma et al, 2006; Kim et al, 2010; Kashiwagi et al, 2014). Specifically, in non-urothelial cancer cells, EP2 and EP4 could modulate E-cadherin (Brouxhon et al, 2007)/hypoxia-inducible factor-1α (Fernández-Martínez and Lucio-Cazaña, 2015), and PI3K-AKT/NF-κB (Majumder et al, 2015), respectively, up- or downregulation of whose expression in urothelial cancer has indeed been linked to the prognosis of the patients (Fromont et al, 2005; Nakanishi et al, 2005; Yeh et al, 2010; Zheng et al, 2011). In BC cell lines including UMUC3, celecoxib also exhibited antitumour effects (Dhawan et al, 2008). A pilot study in 26 patients with muscle-invasive BC further showed that short-term neoadjuvant celecoxib therapy contributed to the achievement of pT0 status in radical cystectomy specimens (3 of 13 cases vs 0 of 13 controls) as well as significant induction/reduction in apoptosis/vascular endothelial growth factor expression, respectively, in residual tumours, compared with the control cohort (Dhawan et al, 2010). In the current study, we found that celecoxib considerably reduced EP2/EP4 expression in BC cells in dose- and time-dependent manners. We further demonstrated that celecoxib and EP2/EP4 inhibitors similarly suppressed cell migration of PTEN-positive BC lines, while EP2 silencing resulted in its significant reduction. These results suggest that EP2 and EP4 promote urothelial cancer progression.
Celecoxib has been assessed in clinical trials whether it increases sensitivity to chemotherapy (Altorki et al, 2003). Using preclinical models for gastric cancer, celecoxib has also been shown to enhance the cytotoxic effects of CDDP by modulating P-glycoprotein expression (Xu et al, 2016). Similarly, celecoxib treatment in BC cell line and mouse models has been suggested to contribute to overcoming resistance to CDDP-based chemotherapy (Kurtova et al, 2015). We then found increases in the expression levels of EP2 and EP4, along with those of YB-1/p-YB-1 and NF-κB/p-NF-κB that were known to involve chemoresistance in BC cells (Shiota et al, 2011; Ito et al, 2015; Kashiwagi et al, 2016), in CDDP-resistant sublines, compared with respective control sublines. EP2/EP4 inhibitors and agonists were additionally found to significantly increase and decrease, respectively, the cytotoxic activity of CDDP at its pharmacological concentrations (e.g. 1.3–8.4 μM; Kashiwagi et al, 2016)). Thus, EP2/EP4 inhibitors may function as sensitisers of CDDP treatment in BC cells.
PTEN is a tumour suppressor and its mutations are often seen in various types of malignancies, including BC (Aveyard et al, 1999). Interestingly, loss of its function has been shown to correlate with induction of not only urothelial tumourigenesis but also the growth and chemoresistance in BC cells (Tanaka et al, 2000; Puzio-Kuter et al, 2009). In particular, PTEN inactivation resulted in activation of the mTOR/AKT pathways in BC cells. We demonstrated that celecoxib and EP2/EP4 inhibitors augmented PTEN expression in urothelial cells undergoing neoplastic transformation as well as in BC cells. An EP2 agonist also reduced PTEN expression in BC cells. In addition, PTEN expression was downregulated in CDDP-resistant sublines, compared with respective control sublines. These observations imply that PTEN has a central role in celecoxib- and selective EP2/EP4 inhibitor-mediated prevention of urothelial carcinogenesis, BC cell growth, and chemoresistance in BC cells. Remarkably, in contrast to the previous findings with celecoxib (Dhawan et al, 2008), celecoxib as well as EP2/EP4 inhibitors failed to significantly inhibit cell proliferation and migration of PTEN-null UMUC3, further suggesting the necessity of PTEN in EP2/EP4-mediated cell growth. In lung and thyroid cancer cells, PTEN expression has been shown to be downregulated by NF-κB (Vasudevan et al, 2004). A positive feedback loop consisting of COX-2-PGE2-EP2-NF-κB is also documented (Aoki et al, 2011). Thus, EP2 and EP4 may downregulate PTEN expression via the NF-κB pathway. It will still need to be determined how EP2/EP4 modulate PTEN signalling in non-neoplastic and neoplastic urothelial cells.
The levels of EP2/EP4 expression have been shown to be elevated in several types of malignancies, such as colorectal (Gustafsson et al, 2007) and endometrial (Jabbour et al, 2001) carcinomas, compared with corresponding normal tissues. By contrast, a recent study showed downregulation of EP expression in BC specimens, compared with normal urothelial tissues (von der Emde et al, 2014). We here found significant upregulation of EP2/EP3/EP4 expression in bladder tumours, supporting the promoting role of EP2/EP4 in tumourigenesis, as shown using the in vitro transformation system. Our immunohistochemistry in muscle-invasive tumours further revealed strong associations between EP2/EP4 expression, as independent prognosticators, and cancer-specific mortality. These results also support our preclinical data indicating that EP2/EP4 activation correlates with the promotion of BC progression. However, EP2 expression was shown to correlate (P=0.08) with better outcomes in patients with upper urinary tract urothelial carcinoma (Miyata et al, 2006), although EP4 expression was strongly (P=0.002) associated with worse prognosis in the same cohort of patients (Miyata et al, 2005). Our results also indicated a potential discrepancy between EP2 and EP4 expression in relation to tumour grade and invasiveness, which might imply their divergent upstream pathways in BC. Meanwhile, the positive rates of EP2/EP4 expression in muscle-invasive BCs from patients who failed to respond to CDDP-based neoadjuvant chemotherapy were higher than those from responders, suggesting that EP2/EP4 expression may predict responses to CDDP therapy. Correspondingly, increased levels of plasma PGE2 have been reported in patients with gynaecologic malignancies, compared with healthy women, which are further elevated during chemotherapy (Suzuki et al, 1987). Considerable increases in the levels of plasma PGE2 have also been documented in dogs with BC, compared with normal controls (Knapp et al, 1994). These findings may need to be confirmed in patients with urothelial cancer.
It must be acknowledged that the pharmacologic agonists/antagonists we used could show ‘off-target’ effects on various signalling pathways. For instance, an EP2 antagonist AH6809 has been shown to function as a weak antagonist for other prostaglandin receptors, such as EP1 and EP3 (Abramovitz et al, 2000). Similarly, an EP4 antagonist ONO-AE3-208 has an affinity for EP3 (Mutoh et al, 2002). These, as well as other undiscovered effects of EP2/EP4 antagonists and agonists on intracellular signalling, imply that the interpretation of our current data using such antagonists/agonists must be done carefully.
In conclusion, our results suggest that EP2 and EP4 have an important role in inducing urothelial tumourigenesis, bladder tumour progression, and chemoresistance in BC cells, presumably via downregulating PTEN expression. Thus, EP2/EP4 inactivation, using available inhibitors, has the potential of being not only a chemopreventive and therapeutic option for urothelial cancer but also a means of chemosensitisation particularly in patients with EP2/EP4-positive tumour.
Footnotes
Supplementary Information accompanies this paper on British Journal of Cancer website (http://www.nature.com/bjc)
This work is published under the standard license to publish agreement. After 12 months the work will become freely available and the license terms will switch to a Creative Commons Attribution-NonCommercial-Share Alike 4.0 Unported License.
The authors declare no conflict of interest.
Supplementary Material
References
- Abbosh PH, McConkey DJ, Plimack ER (2015) Targeting signaling transduction pathways in bladder cancer. Curr Oncol Rep 17: 58. [DOI] [PubMed] [Google Scholar]
- Abramovitz M, Adam M, Boie Y, Carrière M, Denis D, Godbout C, Lamontagne S, Rochette C, Sawyer N, Tremblay NM, Belley M, Gallant M, Dufresne C, Gareau Y, Ruel R, Juteau H, Labelle M, Ouimet N, Metters KM (2000) The utilization of recombinant prostanoid receptors to determine the affinities and selectivities of prostaglandins and related analogs. Biochim Biophys Acta 483: 285–293. [DOI] [PubMed] [Google Scholar]
- Altorki NK, Keresztes R, Port J, Libby D, Korst R, Flieder D, Ferrara CA, Yankelevitz DF, Subbaramaiah K, Pasmantier MW, Dannenberg AJ (2003) Celecoxib, a selective cyclo-oxygenase-2 inhibitor, enhances the response to preoperative paclitaxel and carboplatin in early-stage non–small-cell lung cancer. J Clin Oncol 21: 2645–2650. [DOI] [PubMed] [Google Scholar]
- Aoki T, Nishimura M, Matsuoka T, Yamamoto K, Furuyashiki T, Kataoka H, Kitaoka S, Ishibashi R, Ishibazawa A, Miyamoto S, Morishita R, Ando J, Hashimoto N, Nozaki K, Narumiya S (2011) PGE2-EP2 signalling in endothelium is activated by haemodynamic stress and induces cerebral aneurysm through an amplifying loop via NF-κB. Br J Pharmacol 163: 1237–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arjona-Sánchez Á, Ruiz-Rabelo J, Perea MD, Vázquez R, Cruz A, Muñoz Mdel C, Túnez I, Muntané J, Padillo FJ (2010) Effects of capecitabine and celecoxib in experimental pancreatic cancer. Pancreatology 10: 641–647. [DOI] [PubMed] [Google Scholar]
- Aveyard J, Skilleter A, Habuchi T, Knowles M (1999) Somatic mutation of PTEN in bladder carcinoma. Br J Cancer 80: 904–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baras AS, Gandhi N, Munari E, Faraj S, Shultz L, Marchionni L, Schoenberg M, Hahn N, Hoque MO, Berman D, Bivalacqua TJ, Netto G (2015) Identification and validation of protein biomarkers of response to neoadjuvant platinum chemotherapy in muscle invasive urothelial carcinoma. PLoS ONE 10: e0131245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brouxhon S, Kyrkanides S, O'Banion MK, Johnson R, Pearce DA, Centola GM, Miller JN, McGrath KH, Erdle B, Scott G, Schneider S, VanBuskirk J, Pentland AP (2007) Sequential down-regulation of E-cadherin with squamous cell carcinoma progression: loss of E-cadherin via a prostaglandin E2-EP2–dependent posttranslational mechanism. Cancer Res 67: 7654–7664. [DOI] [PubMed] [Google Scholar]
- Castellone MD, Teramoto H, Williams BO, Druey KM, Gutkind JS (2005) Prostaglandin E2 promotes colon cancer cell growth through a Gs-axin-β-catenin signaling axis. Science 310: 1504–1510. [DOI] [PubMed] [Google Scholar]
- Coussens LM, Werb Z (2002) Inflammation and cancer. Nature 420: 860–867. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhawan D, Craig BA, Cheng L, Snyder PW, Mohammed SI, Stewart JC, Zheng R, Loman RA, Foster RS, Knapp DW (2010) Effects of short-term celecoxib treatment in patients with invasive transitional cell carcinoma of the urinary bladder. Mol Cancer Ther 9: 1371–1377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dhawan D, Jeffreys AB, Zheng R, Stewart JC, Knapp DW (2008) Cyclooxygenase-2 dependent and independent antitumor effects induced by celecoxib in urinary bladder cancer cells. Mol Cancer Ther 7: 897–904. [DOI] [PubMed] [Google Scholar]
- Dorsam RT, Gutkind JS (2007) G-protein-coupled receptors and cancer. Nature Rev Cancer 7: 79–94. [DOI] [PubMed] [Google Scholar]
- Fernández-Martínez AB, Lucio-Cazaña J (2015) Intracellular EP2 prostanoid receptor promotes cancer-related phenotypes in PC3 cells. Cell Mol Life Sci 72: 3355–3373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fromont G, Rouprêt M, Amira N, Sibony M, Vallancien G, Validire P, Cussenot O (2005) Tissue microarray analysis of the prognostic value of E-cadherin, Ki67, p53, p27, survivin and MSH2 expression in upper urinary tract transitional cell carcinoma. Eur Urol 48: 764–770. [DOI] [PubMed] [Google Scholar]
- Gurpinar E, Grizzle WE, Piazza GA (2014) NSAIDs inhibit tumorigenesis, but how? Clin Cancer Res 20: 1104–1113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson A, Hansson E, Kressner U, Nordgren S, Andersson M, Wang W, Lönnroth C, Lundholm K (2007) EP1-4 subtype, COX and PPARγ receptor expression in colorectal cancer in prediction of disease-specific mortality. Int J Cancer 121: 232–240. [DOI] [PubMed] [Google Scholar]
- Hu PJ, Yu J, Zeng ZR, Leung WK, Lin HL, Tang BD, Bai AHC, Sung JJY (2004) Chemoprevention of gastric cancer by celecoxib in rats. Gut 53: 195–200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito Y, Kikuchi E, Tanaka N, Kosaka T, Suzuki E, Mizuno R, Shinojima T, Miyajima A, Umezawa K, Oya M (2015) Down-regulation of NF kappa B activation is an effective therapeutic modality in acquired platinum-resistant bladder cancer. BMC Cancer 15: 324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jabbour HN, Milne SA, Williams AR, Anderson RA, Boddy SC (2001) Expression of COX-2 and PGE synthase and synthesis of PGE2 in endometrial adenocarcinoma: a possible autocrine/paracrine regulation of neoplastic cell function via EP2/EP4 receptors. Br J Cancer 85: 1023–1031. [DOI] [PubMed] [Google Scholar]
- Jendrossek V (2013) Targeting apoptosis pathways by celecoxib in cancer. Cancer Lett 332: 313–324. [DOI] [PubMed] [Google Scholar]
- Jeon HG, Jeong IG, Bae J, Lee JW, Won JK, Paik JH, Kim HH, Lee SE, Lee E (2010) Expression of Ki-67 and COX-2 in patients with upper urinary tract urothelial carcinoma. Urology 76: 513.e7–e12. [DOI] [PubMed] [Google Scholar]
- Kashiwagi E, Ide H, Inoue S, Kawahara T, Zheng Y, Reis LO, Baras AS, Miyamoto H (2016) Androgen receptor activity modulates responses to cisplatin treatment in bladder cancer. Oncotarget 7: 49169–49179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kashiwagi E, Shiota M, Yokomizo A, Inokuchi J, Uchiumi T, Naito S (2014) EP2 signaling mediates suppressive effects of celecoxib on androgen receptor expression and cell proliferation in prostate cancer. Prostate Cancer Prostatic Dis 17: 10–17. [DOI] [PubMed] [Google Scholar]
- Kashiwagi E, Shiota M, Yokomizo A, Itsumi M, Inokuchi J, Uchiumi T, Naito S (2013) Prostaglandin receptor EP3 mediates growth inhibitory effect of aspirin through androgen receptor and contributes to castration resistance in prostate cancer cells. Endocr Relat Cancer 20: 431–441. [DOI] [PubMed] [Google Scholar]
- Kawahara T, Kashiwagi E, Li Y, Zheng Y, Miyamoto Y, Netto GJ, Ishiguro H, Miyamoto H (2016) Cyclosporine A and tacrolimus inhibit urothelial tumorigenesis. Mol Carcinogen 55: 161–169. [DOI] [PubMed] [Google Scholar]
- Keith RL, Geraci MW, Nana-Sinkam SP, Breyer RM, Hudish TM, Meyer AM, Malkinson AM, Dwyer-Nield LD (2006) Prostaglandin E2 receptor subtype 2 (EP2) null mice are protected against murine lung tumorigenesis. Anticancer Res 26: 2857–2861. [PubMed] [Google Scholar]
- Kim JI, Lakshmikanthan V, Frilot N, Daaka Y (2010) Prostaglandin E2 promotes lung cancer cell migration via EP4-βArrestin1-c-Src signalsome. Mol Cancer Res 8: 569–577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knapp DW, Richardson RC, Chan TC, Bottoms GD, Widmer WR, DeNicola DB, Teclaw R, Bonney PL, Kuczek T (1994) Piroxicam therapy in 34 dogs with transitional cell carcinoma of the urinary bladder. J Vet Intern Med 8: 273–278. [DOI] [PubMed] [Google Scholar]
- Kurtova AV, Xiao J, Mo Q, Pazhanisamy S, Krasnow R, Lerner SP, Chen F, Roh TT, Lay E, Ho PL, Chan KS (2015) Blocking PGE2-induced tumour repopulation abrogates bladder cancer chemoresistance. Nature 517: 209–213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li Y, Ishiguro H, Kawahara T, Miyamoto Y, Izumi K, Miyamoto H (2014) GATA3 in the urinary bladder: suppression of neoplastic transformation and down-regulation by androgens. Am J Cancer Res 4: 461–467. [PMC free article] [PubMed] [Google Scholar]
- Lin MT, Lee RC, Yang PC, Ho FM, Kuo ML (2001) Cyclooxygenase-2 inducing Mcl-1-dependent survival mechanism in human lung adenocarcinoma CL1.0 cells. Involvement of phosphatidylinositol 3-kinase/Akt pathway. J Biol Chem 276: 48997–49002. [DOI] [PubMed] [Google Scholar]
- Liu H, Huang P, Xu X, Liu J, Guo C (2009) Anticancer effect of celecoxib via COX-2 dependent and independent mechanisms in human gastric cancers cells. Dig Dis Sci 54: 1418–1424. [DOI] [PubMed] [Google Scholar]
- Ma X, Aoki T, Tsuruyama T, Narumiya S (2015) Definition of prostaglandin E2–EP2 signals in the colon tumor microenvironment that amplify inflammation and tumor growth. Cancer Res 75: 2822–2832. [DOI] [PubMed] [Google Scholar]
- Ma X, Kundu N, Rifat S, Walser T, Fulton AM (2006) Prostaglandin E receptor EP4 antagonism inhibits breast cancer metastasis. Cancer Res 66: 2923–2927. [DOI] [PubMed] [Google Scholar]
- Majumder M, Landman E, Liu L, Hess D, Lala PK (2015) COX-2 elevates oncogenic miR-526b in breast cancer by EP4 activation. Mol Cancer Res 13: 1022–1033. [DOI] [PubMed] [Google Scholar]
- Miyamoto H, Yao JL, Chaux A, Zheng Y, Hsu I, Izumi K, Chang C, Messing EM, Netto GJ, Yeh S (2012) Expression of androgen and oestrogen receptors and its prognostic significance in urothelial neoplasm of the urinary bladder. BJU Int 109: 1716–1726. [DOI] [PubMed] [Google Scholar]
- Miyata Y, Kanda S, Nomata K, Eguchi J, Kanetake H (2005) Expression of cyclooxygenase-2 and EP4 receptor in transitional cell carcinoma of the upper urinary tract. J Urol 173: 56–60. [DOI] [PubMed] [Google Scholar]
- Miyata Y, Ohba K, Kanda S, Nomata K, Eguchi J, Hayashi T, Kanetake H (2006) Pathological function of prostaglandin E2 receptors in transitional cell carcinoma of the upper urinary tract. Virchows Arch 448: 822–829. [DOI] [PubMed] [Google Scholar]
- Mohammed SI, Knapp DW, Bostwick DG, Foster RS, KNM Khan, Masferrer JL, Woerner BM, Snyder PW, Koki AT (1999) Expression of cyclooxygenase-2 (COX-2) in human invasive transitional cell carcinoma (TCC) of the urinary bladder. Cancer Res 59: 5647–5650. [PubMed] [Google Scholar]
- Mutoh M, Watanabe K, Kitamura T, Shoji Y, Takahashi M, Kawamori T, Tani K, Kobayashi M, Maruyama T, Kobayashi K, Ohuchida S, Sugimoto Y, Narumiya S, Sugimura T, Wakabayashi K (2002) Involvement of prostaglandin E receptor subtype EP4 in colon carcinogenesis. Cancer Res 62: 28–32. [PubMed] [Google Scholar]
- Nakanishi K, Hiroi S, Tominaga S, Aida S, Kasamatsu H, Matsuyama S, Matsuyama T, Kawai T (2005) Expression of hypoxia-inducible factor-1α protein predicts survival in patients with transitional cell carcinoma of the upper urinary tract. Clin Cancer Res 11: 2583–2590. [DOI] [PubMed] [Google Scholar]
- Narumiya S, Sugimoto Y, Ushikubi F (1999) Prostanoid receptors: Structures, properties, and functions. Physiol Rev 79: 1193–1226. [DOI] [PubMed] [Google Scholar]
- Pagliarulo V, Ancona P, Martines I, Spadavecchia R, Di Stasi S, Alba S, Cormio L, Fanizza C, Salerno A, Carrieri G, Pagliarulo A (2015) Celecoxib for the prevention of nonmuscle invasive bladder cancer: results from a matched control study. Ther Adv Urol 7: 303–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Puzio-Kuter AM, Castillo-Martin M, Kinkade CW, Wang X, Shen TH, Matos T, Shen MM, Cordon-Cardo C, Abate-Shen C (2009) Inactivation of p53 and Pten promotes invasive bladder cancer. Genes Dev 23: 675–680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reznikoff CA, Loretz LJ, Christian BJ, Wu SQ, Meisner LF (1988) Neoplastic transformation of SV40-immortalized human urinary tract epithelial cells by in vitro exposure to 3-methylcholanthrene. Carcinogenesis 9: 1427–1436. [DOI] [PubMed] [Google Scholar]
- Shiota M, Yokomizo A, Itsumi M, Uchiumi T, Tada Y, Song Y, Kashiwagi E, Masubuchi D, Naito S (2011) Twist1 and Y-box-binding protein-1 promote malignant potential in bladder cancer cells. BJU Int 108: E142–E149. [DOI] [PubMed] [Google Scholar]
- Siegel RL, Miller KD, Jemal A (2017) Cancer statistics, 2017. CA Cancer J Clin 67: 7–30. [DOI] [PubMed] [Google Scholar]
- Suzuki M, Ohwada M, Tamada T (1987) Plasma prostaglandin levels in patients with gynecologic malignancies and its fluctuations during chemotherapeutically-induced gastrointenstinal toxicity. Jpn J Clin Oncol 17: 215–220. [PubMed] [Google Scholar]
- Tanaka M, Koul D, Davies MA, Liebert M, Steck PA, Grossman HB (2000) MMAC1/PTEN inhibits cell growth and induces chemosensitivity to doxorubicin in human bladder cancer cells. Oncogene 19: 5406–5412. [DOI] [PubMed] [Google Scholar]
- Taylor JA, Ristau B, Bonnemaison M, Voznesensky OS, Hegde P, Kuchel GA, Pilbeam CC (2009) Regulation of the prostaglandin pathway during development of invasive bladder cancer in mice. Prostaglandins Other Lipid Mediat 88: 36–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasudevan KM, Gurumurthy S, Rangnekar VM (2004) Suppression of PTEN expression by NF-κB prevents apoptosis. Mol Cell Biol 24: 1007–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vidal AC, Howard LE, Moreira DM, Castro-Santamaria R, Andriole GL, Freedland SJ. (2015) Aspirin, NSAIDs, and risk of prostate cancer: Results from the REDUCE study. Clin Cancer Res 21: 756–762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- von der Emde L, Goltz D, Latz S, Müller SC, Kristiansen G, Ellinger J, Syring I (2014) Prostaglandin receptors EP1-4 as a potential marker for clinical outcome in urothelial bladder cancer. Am J Cancer Res 4: 952–962. [PMC free article] [PubMed] [Google Scholar]
- Xu HB, Shen FM, Lv QZ (2016) Celecoxib enhanced the cytotoxic effect of cisplatin in chemo-resistant gastric cancer xenograft mouse models through a cyclooxygenase-2-dependent manner. Eur J Pharmacol 776: 1–8. [DOI] [PubMed] [Google Scholar]
- Yeh HC, Huang CH, Yang SF, Li CC, Chang LL, Lin HH, Ke HL, Wei YC, Wu WJ (2010) Nuclear factor-κB activation predicts an unfavourable outcome in human upper urinary tract urothelial carcinoma. BJU Int 106: 1223–1229. [DOI] [PubMed] [Google Scholar]
- Zheng Y, Izumi K, Yao JL, Miyamoto H (2011) Dihydrotestosterone upregulates the expression of epidermal growth factor receptor and ERBB2 in androgen receptor-positive bladder cancer cells. Endocr Relat Cancer 18: 451–464. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.