Abstract
Arthroscopic pancapsular release has been recommended for recalcitrant frozen shoulder, but regaining range of motion has not been sufficient compared with the unaffected side. There is no consensus about the reasons for these remaining restrictions in range of motion, but residual capsular or connective tissue must be considered a candidate. A thickened coracohumeral ligament at the rotator interval has been reported as one of the most specific manifestations of frozen shoulder. It covers wider portions of the subscapularis tendon, supraspinatus tendon, and infraspinatus tendon than previously reported. We describe an arthroscopic surgical technique for the release of the entire coracohumeral ligament including the subscapularis and supraspinatus portions and the release of the inferior and posterior parts of the glenohumeral ligament using the 7-o'clock portal. These procedures are essential and reliable methods to release the entire joint capsule to regain full range of motion for frozen shoulder.
Patients with frozen shoulder present with painful restriction of both active and passive shoulder motion. In cases of limited range of motion (ROM) after appropriate conservative treatment, an arthroscopic pancapsular release could be a treatment option to regain ROM.1 However, it has been difficult to regain full ROM even after the procedure compared with the unaffected side.2 Although there is no consensus about the reasons for these remaining restrictions in ROM, residual capsular and subacromial tissue is assumed to be a candidate.
The coracohumeral ligament (CHL) has been described as originating from the base and the horizontal limb of the coracoid process, enclosing the subscapularis, supraspinatus, and infraspinatus tendons.3 On the basis of a recent study, it envelops vaster areas of the subscapularis than previously reported.4 A thickened CHL at the rotator interval has been well known to be one of the most specific manifestations of frozen shoulder and the primary restraint against external rotation (ER).5 However, a thickened CHL covering the subscapularis and supraspinatus contributes to restrictions of internal rotation (IR), and its arthroscopic release improves ER as well as IR for patients with frozen shoulder after manipulation under anesthesia (MUA).6 Furthermore, obliteration of the subcoracoid fat triangle and the thickness of the CHL positively correlated with ROM restrictions (forward flexion [FF], ER, and hand behind the back [HBB]—measured by asking the patient to place the thumb at the highest possible spinal vertebra), and these changes were greater with age for recurrent anterior shoulder instability evaluated by magnetic resonance arthrography.7 The thickening of the CHL has the potential to restrict ER as well as IR. We present an arthroscopic surgical technique for the release of the entire CHL including the subscapularis and supraspinatus portions to regain full ROM for patients with frozen shoulder.
Physical Examination and Imaging
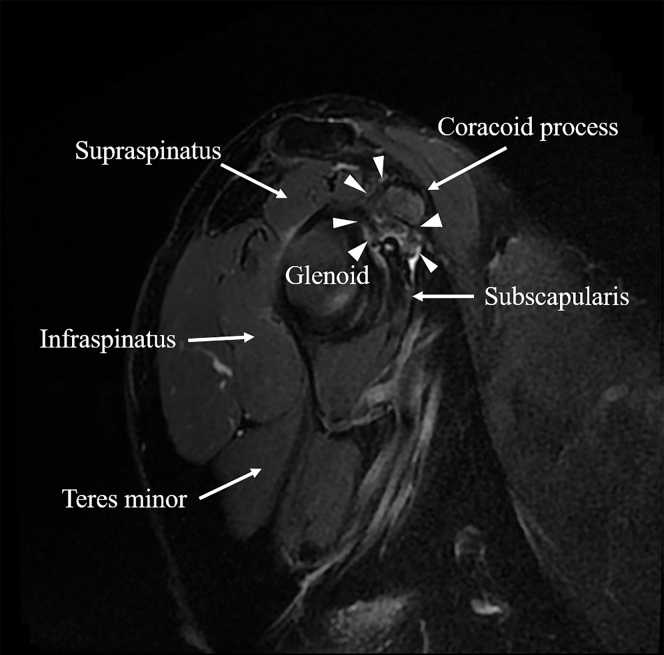
Passive ROM measurements of both the affected and unaffected sides before surgery, including FF, abduction (ABD), ER with the arm at the side, ER at 90° of ABD, IR at 90° of ABD, horizontal flexion, ER at 90° of FF (third ER), IR at 90° of FF (third IR), and HBB, are measured with a goniometer with the patient in the standing position in an outpatient clinic. However, these procedures include combined motion of the glenohumeral joint and scapulothoracic motion. To evaluate true ROM of the glenohumeral joint, which is assumed to reflect faint capsular changes, the scapula is fixed by an examiner with 1 hand (with no palpation of scapular motion), and passive ROM is also measured in the same manner with the patient under general anesthesia in the beach-chair position in the outpatient clinic. In cases of difficulty in 90° of FF and ABD, ROM is evaluated at the maximum degrees of FF and ABD. The thickening of the CHL is evaluated by magnetic resonance imaging on the sagittal oblique view. Deep fibrous tissues are observed around the base of the coracoid process, as well as the subcoracoid fat triangle, in patients with frozen shoulder (Fig 1). Restrictions of ROM in horizontal flexion, in third ER, in third IR, and with HBB with scapular fixation are more specific manifestations of the thickening of the CHL, as well as obliteration of the subcoracoid fat triangle (Table 1).
Fig 1.
Sagittal oblique view of magnetic resonance imaging (right shoulder, fat-suppression image). The thickened coracohumeral ligament and obliteration of the subcoracoid fat triangle are observed (arrowheads).
Table 1.
Indications and Contraindications of Arthroscopic Coracohumeral Ligament Release
| Indications |
| Recalcitrant frozen shoulder |
| Thickening of coracohumeral ligament and obliteration of subcoracoid fat triangle evaluated by magnetic resonance imaging on sagittal oblique view |
| Restriction in range of motion, especially in horizontal flexion, in external rotation and internal rotation at 90° of forward flexion, and with hand behind back |
| Contraindications |
| Patients with bleeding tendency |
Surgical Technique
Preoperative Patient Positioning
The patient is placed in the beach-chair position (T-MAX Beach Chair; Smith & Nephew, Boston, MA) under general anesthesia, and the index shoulder is sterilized.
Initial Exposure
A 30° arthroscope (1488 Full HD; Stryker, San Jose, CA) is introduced through a standard posterior portal, and diagnostic arthroscopy is performed. The rotator interval and subscapularis tendon are covered with thick fibrous tissues accompanying synovitis and development or formation of blood vessels. The superomedial capsule and the long head of the biceps are usually adhered together with synovitis with decreasing sliding motion. The middle and anterior inferior glenohumeral ligaments change to dark yellow with synovitis like the rotator interval. An anterior portal just superior to the subscapularis tendon as well as just lateral to the tip of the conjoint tendon is created by the outside-in technique with the use of an 18-gauge spinal needle.
Capsular Release of Rotator Interval, CHL, Superior Capsule, and Middle and Anterior Inferior Glenohumeral Ligaments
The rotator interval and middle glenohumeral ligament of the operative shoulder are dissected with forceps (Oval Punches Straight; Smith & Nephew) or a shaver (Dyonics Powermax Elite Handpiece and Dyonics Incisor Plus Platinum; Smith & Nephew) until a clear view of the CHL, conjoint tendon, and subscapularis tendon or muscle is obtained (Fig 2). At this time, the superior glenohumeral ligament and a part of the CHL are resected. The remaining CHL under the coracoid process to the subscapularis tendon or muscle and the base of the coracoid process to the supraspinatus tendon, as well as adhesions between the subscapularis and conjoint tendon or glenoid neck, are also dissected with forceps and a shaver (Fig 3). The superomedial capsule, just above the long head of the biceps, is dissected with radiofrequency (VAPR Angled Side Effect; DePuy Mitek, Raynham, MA) to the base of the coracoid process until clear vision of the posterior margin of the coracoacromial ligament is obtained (Fig 4). The superior capsule is dissected as far posteriorly as possible, usually until the 9-o'clock position (right shoulder) (Fig 5). In the next step, the residual middle and anterior inferior glenohumeral ligaments are resected with forceps or radiofrequency along the margin of the glenoid as far inferiorly as possible, usually around the 6-o'clock position (right shoulder), with a clear view of the subscapularis muscle (Figs 6 and 7). Meticulous care should be taken not to damage the axillary nerve.
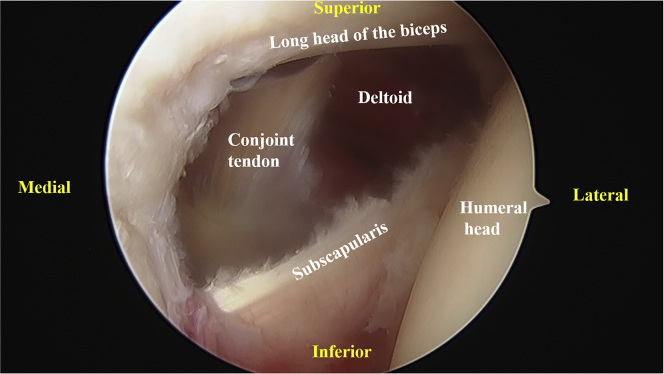
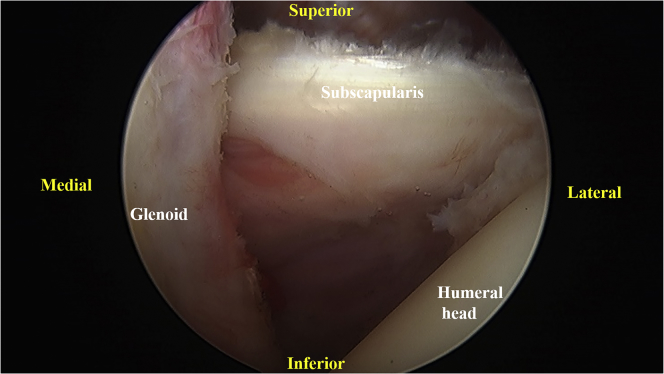
Fig 2.
Right shoulder with patient in beach-chair position and camera in posterior portal. The rotator interval, superior glenohumeral ligament, and part of the coracohumeral ligament are released. The subscapularis and conjoint tendons are clearly visualized. Dissection of fibrous tissues just lateral to the conjoint tendon can make observation of the deltoid muscle possible.
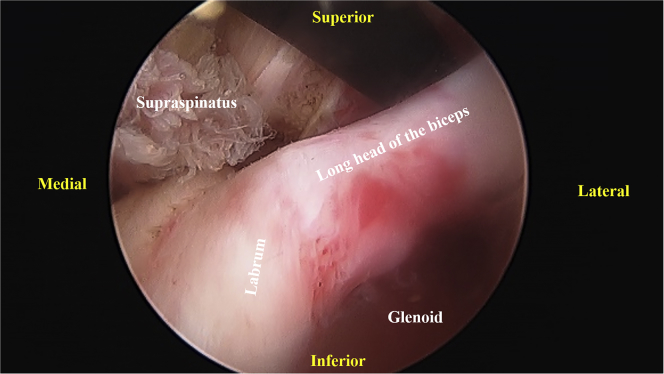
Fig 3.
Right shoulder with patient in beach-chair position and camera in posterior portal. After release of the coracohumeral ligament under the coracoid process, as well as both the anterior and posterior parts of the subscapularis, the subscapularis tendon is clearly observed until the medial margin of the coracoid process. The subscapularis tendon can move smoothly under the coracoid process. The posterior border of the coracoacromial ligament is observed after release of the coracohumeral ligament around the base of the coracoid process.
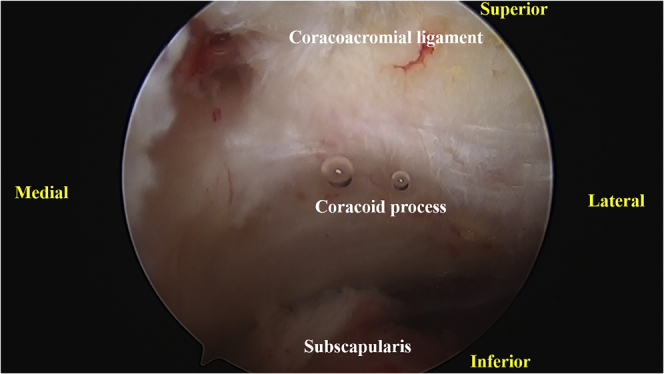
Fig 4.
Right shoulder with patient in beach-chair position and camera in posterior portal. After release of the superomedial capsule and the coracohumeral ligament around the coracoid process, the supraspinatus muscle is clearly observed. The supraspinatus muscle can move smoothly around the coracoid process and supraglenoid tubercle.
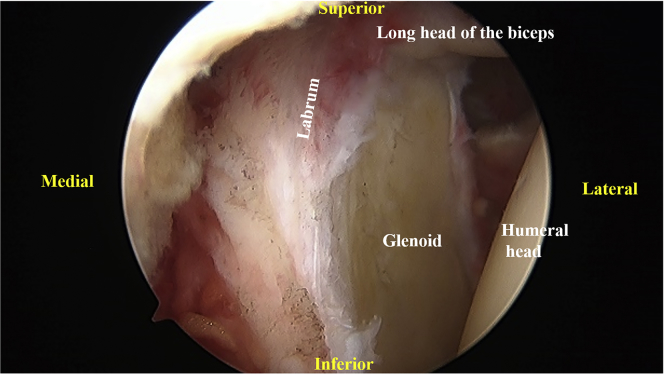
Fig 5.
Right shoulder with patient in beach-chair position and camera in posterior portal. The superior margin of the labrum is dissected with an angled radiofrequency device over the long head of the biceps until the supraspinatus and infraspinatus muscles are confirmed. For release of the posterior part, it is easier to pass the radiofrequency device under the long head of the biceps.
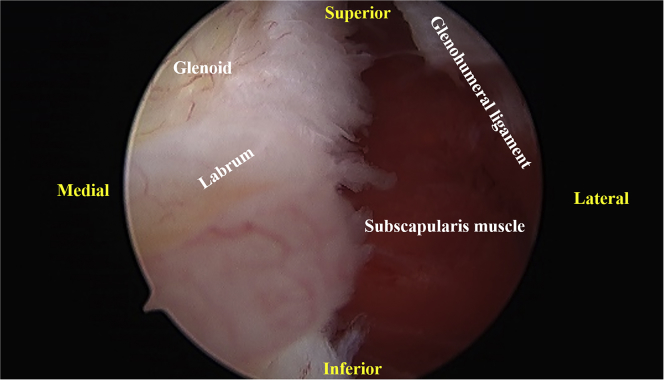
Fig 6.
Right shoulder with patient in beach-chair position and camera in posterior portal. The subscapularis muscle is clearly seen after release of the middle glenohumeral ligament. The subscapularis tendon can move smoothly around the glenoid neck.
Fig 7.
Right shoulder with patient in beach-chair position and camera in posterior portal. After release of the anterior inferior glenohumeral ligament, the inferior part of the subscapularis muscle is clearly seen. The subscapularis muscle can move smoothly around the glenoid neck.
Posterior Inferior Glenohumeral Ligament Release
In the last step, the residual posterior inferior glenohumeral ligament is dissected with radiofrequency by use of the 7-o'clock portal until the long head of the triceps tendon is confirmed and the stump of the residual superior capsule is linked (Fig 8). The entire procedure is completed from the standard posterior portal, without changing the view from the posterior portal to the anterior portal (Video 1).
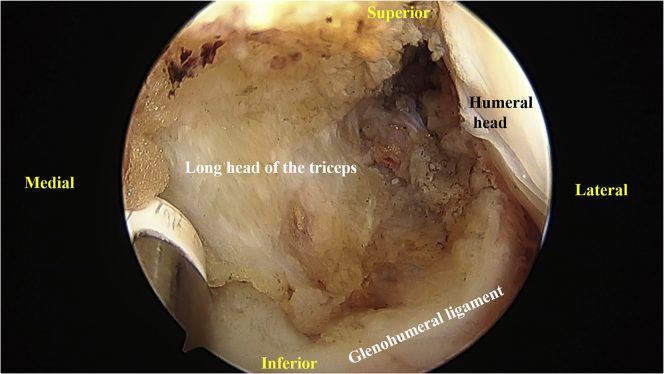
Fig 8.
Right shoulder with patient in beach-chair position and camera in posterior portal. To dissect completely around the inferior part of the glenohumeral ligament, the angled radiofrequency device is passed by use of the 7-o'clock portal. The residual posterior inferior glenohumeral ligament is dissected from the 7-o'clock portal to link the stump of the residual superior capsule until the infraspinatus and teres minor muscles are confirmed. The muscles can move smoothly around the glenoid neck.
Postoperative Rehabilitation
In the case of severe pain during motion after surgery, the affected shoulder is immobilized in a sling for a few days. After pain decreases, active FF in a lying position starts with the support of the unaffected side. Physiotherapy, especially including scapulothoracic flexibility as well as glenohumeral motion, is initiated with the help of a physiotherapist specializing in the shoulder. According to the patient's condition, he or she can return to daily activities and strenuous labor gradually, approximately within 2 months after surgery.
Discussion
A conventional arthroscopic pancapsular release, without releasing the entire CHL, for frozen shoulder is widely accepted and recognized as a safe procedure.2, 8 It improves ROM, pain frequency and severity, and function.9 However, it is difficult to regain full ROM compared with the unaffected side. Other parts of the joint capsule as well as the subacromial tissue are assumed to influence ROM restriction.
MUA can reduce the duration of symptoms and appears to be safer and more reliable than previous reports with adequate caution against complications.10 However, other studies have reported few effects of MUA or destruction of the intra-articular tissues and recommended arthroscopic capsular release for recalcitrant cases.11 MUA with a controlled force to the humerus induced a rupture of the posteroinferior glenohumeral ligament, but the thickened CHL and the intact superomedial capsule were identified by consecutive arthroscopic capsular release.6 After these are released arthroscopically, ROM can be recovered to a normal level, including IR.6
The CHL is divided into 2 parts by macroscopic findings: 1 part spreads fibers over the rotator interval to the posterior portion of the greater tuberosity, and the other part envelops the superior portion of the subscapularis and the whole supraspinatus tendon.4 Because the thickness of the CHL and obliteration of the subcoracoid fat are associated with restriction of ROM including IR,7 it is imperative to release the entire CHL to regain full ROM. Releasing the CHL around and under the coracoid process and both the anterior and posterior parts of the subscapularis tendon is assumed to alter the rotational center between the glenoid and humeral head, which can make it easier to slide both the supraspinatus and subscapularis tendons and muscles. Complete dissection of the CHL is supposed to be a necessary procedure to gain full ROM for frozen shoulder.
Because the described procedure dissects the whole rotator interval between the long head of the biceps and the subscapularis tendon, it is easier to recognize the coracoid process and conjoint and subscapularis tendons. Furthermore, releasing the superomedial capsule makes it easier to reach the base of the coracoid process with resection of the remaining CHL. By use of clear vision, both motions of the supraspinatus and subscapularis tendons are visualized and residual tissues that restrict ROM can be easily recognized during surgery. However, it should be considered that tissues that adhere bleed easily. The base and inferior margin of the coracoid process in particular should be released carefully to avoid unnecessary bleeding. Furthermore, there remains the risk of bleeding as well as musculocutaneous nerve damage while releasing tissues between the subscapularis and conjoint tendons. Releasing the entire CHL in a patient with the tendency to bleed should be avoided (Table 2).
Table 2.
Advantages and Disadvantages of Arthroscopic Coracohumeral Ligament Release
| Advantages |
| Use of standard arthroscopic shoulder setup and portals |
| Viewing only from posterior portal with 30° arthroscope |
| Use of standard surgical equipment |
| Clear visualization of base of coracoid process, coracoacromial ligament, conjoint tendon, and supraspinatus and subscapularis tendons or muscles |
| Confirmation of motion of supraspinatus and subscapularis tendons and muscles |
| Disadvantages |
| Relatively technically demanding |
| Bleeding around base and inferior margin of coracoid process |
| Risk of musculocutaneous nerve damage |
Besides the release of the entire CHL, the other joint capsule is released from the glenoid with confirmation by sight of the muscles. This procedure can make it easier to slide the muscles around the glenoid, which can increase ROM. To dissect the inferior part of the glenohumeral ligament (6-o'clock position, right shoulder), changing the viewing portal from the posterior portal to the anterior portal has been reported.2 However, the use of the 7-o'clock portal is a safe and effective method to completely dissect the inferior glenohumeral ligament clearly. To avoid damage to the axillary nerve, this technique is an essential and reliable method. Further biomechanical and follow-up studies are needed to clarify the efficacy of these procedures.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
Arthroscopic coracohumeral ligament release for a patient with frozen shoulder (right shoulder) in the beach-chair position. The release is performed viewing only from the standard posterior portal with a 30° arthroscope.
References
- 1.Holloway G.B., Schenk T., Williams G.R., Ramsey M.L., Iannotti J.P. Arthroscopic capsular release for the treatment of refractory postoperative or post-fracture shoulder stiffness. J Bone Joint Surg Am. 2001;83:1682–1687. doi: 10.2106/00004623-200111000-00010. [DOI] [PubMed] [Google Scholar]
- 2.Hagiwara Y., Sugaya H., Takahashi N. Effects of intra-articular steroid injection before pan-capsular release in patients with refractory frozen shoulder. Knee Surg Sports Traumatol Arthrosc. 2015;23:1536–1541. doi: 10.1007/s00167-014-2936-2. [DOI] [PubMed] [Google Scholar]
- 3.Clark J.M., Harryman D.T., II Tendons, ligaments, and capsule of the rotator cuff. Gross and microscopic anatomy. J Bone Joint Surg Am. 1992;74:713–725. [PubMed] [Google Scholar]
- 4.Arai R., Nimura A., Yamaguchi K. The anatomy of the coracohumeral ligament and its relation to the subscapularis muscle. J Shoulder Elbow Surg. 2014;23:1575–1581. doi: 10.1016/j.jse.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 5.Ozaki J., Nakagawa Y., Sakurai G., Tamai S. Recalcitrant chronic adhesive capsulitis of the shoulder. Role of contracture of the coracohumeral ligament and rotator interval in pathogenesis and treatment. J Bone Joint Surg Am. 1989;71:1511–1515. [PubMed] [Google Scholar]
- 6.Koide M., Hamada J., Hagiwara Y., Kanazawa K., Suzuki K. A thickened coracohumeral ligament and superomedial capsule limit internal rotation of the shoulder joint: Report of three cases. Case Rep Orthop. 2016;2016:9384974. doi: 10.1155/2016/9384974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kanazawa K., Hagiwara Y., Kawai N. Correlations of coracohumeral ligament and range of motion restriction in patients with recurrent anterior glenohumeral instability evaluated by magnetic resonance arthrography. J Shoulder Elbow Surg. 2017;26:233–240. doi: 10.1016/j.jse.2016.09.016. [DOI] [PubMed] [Google Scholar]
- 8.Jerosch J. 360 degrees arthroscopic capsular release in patients with adhesive capsulitis of the glenohumeral joint—Indication, surgical technique, results. Knee Surg Sports Traumatol Arthrosc. 2001;9:178–186. doi: 10.1007/s001670100194. [DOI] [PubMed] [Google Scholar]
- 9.Jerosch J., Nasef N.M., Peters O., Mansour A.M. Mid-term results following arthroscopic capsular release in patients with primary and secondary adhesive shoulder capsulitis. Knee Surg Sports Traumatol Arthrosc. 2013;21:1195–1202. doi: 10.1007/s00167-012-2124-1. [DOI] [PubMed] [Google Scholar]
- 10.Farrell C.M., Sperling J.W., Cofield R.H. Manipulation for frozen shoulder: Long-term results. J Shoulder Elbow Surg. 2005;14:480–484. doi: 10.1016/j.jse.2005.02.012. [DOI] [PubMed] [Google Scholar]
- 11.Loew M., Heichel T.O., Lehner B. Intraarticular lesions in primary frozen shoulder after manipulation under general anesthesia. J Shoulder Elbow Surg. 2005;14:16–21. doi: 10.1016/j.jse.2004.04.004. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Arthroscopic coracohumeral ligament release for a patient with frozen shoulder (right shoulder) in the beach-chair position. The release is performed viewing only from the standard posterior portal with a 30° arthroscope.