Abstract
Objective
Conduct a cost-effectiveness analysis of FreeO2 technology versus manual oxygen-titration technology for patients with chronic obstructive pulmonary disease (COPD) hospitalised for acute exacerbations.
Setting
Tertiary acute care hospital in Quebec, Canada.
Participants
47 patients with COPD hospitalised for acute exacerbations.
Intervention
An automated oxygen-titration and oxygen-weaning technology.
Methods and outcomes
The costs for hospitalisation and follow-up for 180 days were calculated using a microcosting approach and included the cost of FreeO2 technology. Incremental cost-effectiveness ratios (ICERs) were calculated using bootstrap resampling with 5000 replications. The main effect variable was the percentage of time spent at the target oxygen saturation (SpO2). The other two effect variables were the time spent in hyperoxia (target SpO2+5%) and in severe hypoxaemia (SpO2 <85%). The resamplings were based on data from a randomised controlled trial with 47 patients with COPD hospitalised for acute exacerbations.
Results
FreeO2 generated savings of 20.7% of the per-patient costs at 180 days (ie, −$C2959.71). This decrease is nevertheless not significant at the 95% threshold (P=0.13), but the effect variables all improved (P<0.001). The improvement in the time spent at the target SpO2 was 56.3%. The ICERs indicate that FreeO2 technology is more cost-effective than manual oxygen titration with a savings of −$C96.91 per percentage point of time spent at the target SpO2 (95% CI −301.26 to 116.96).
Conclusion
FreeO2 technology could significantly enhance the efficiency of the health system by reducing per-patient costs at 180 days. A study with a larger patient sample needs to be carried out to confirm these preliminary results.
Trial registration number
Keywords: cost-effectiveness, oxygen-titration, copd, bootstrap, freeo2, canada
Strengths and limitations of this study.
A microcosting (or bottom-up) approach with bootstrap resampling was used to assess the cost-effectiveness of FreeO2 for patients with COPD.
Various cost-effectiveness analyses were conducted, showing robust results.
The size of the sample used is small and a larger study should be conducted to confirm the cost-effectiveness of FreeO2.
Introduction
Context
Chronic obstructive pulmonary disease (COPD) is an umbrella term used to describe chronic lung diseases that obstruct airflow from the lungs.1 According to WHO, COPD is actually the fifth leading cause of mortality worldwide and could move into third place by 2030.1 A recent study conducted in Canada also shows that the number of patients with COPD could increase by 150% in 2030 compared with 2010.2 Among the elderly aged 75 years or older, the increase could be as high as 220%.2 The prevalence of COPD in Canada was 4.3% for individuals aged 35 years or older in 2010,3 and COPD exacerbation was the leading cause of hospitalisation among chronic diseases with an average length of stay of about 10 days.4 5 There is considerable heterogeneity in the economic burden and prevalence of COPD, but the trend is an increase related to population growth and ageing.6 Depending on the study, the estimated costs of an episode of exacerbation varied widely, ranging from US$88 for simple medication to US$7757 or more for hospitalisation.7 8 In the USA, the hospitalisation costs for a principal diagnosis of COPD are estimated at US$6.1 billion per year8 and can be as much as several tens of billions of dollars per year when secondary diagnoses of COPD and absenteeism costs are included.9
Inadequate oxygenation (hyperoxia or hypoxaemia) increases the risks of medical complications and can, in certain cases, lead to increased mortality among patients with COPD.10 11 It is therefore essential to optimise oxygen therapy to bolster patient safety and the quality of care provided.12 From this perspective, certain studies have demonstrated shortcomings in oxygen administration to patients,13 despite the recommendations of many medical societies,14 15 in particular, the fact that certain patients with COPD received excessive oxygen flows.16 17 It also appears that the current system for administering oxygen—the float-ball flowmeter, in use for more than a century—can have serious limitations that urgently call for more effective and practical solutions. In the hospital setting, several studies showed poor compliance with recommendations. Cousins et al. 13 review included the analysis of 29 papers evaluating oxygen prescription in the general medical or respiratory ward. Overall, the literature suggests that the practice of prescribing oxygen therapy is poor for prescription, administration and monitoring, and that specific interventions may improve the practices. One study demonstrated that the rate of compliance with oxygen prescriptions increased after educational interventions (eg, audit, audit presentation, groups of discussion, modification of the prescription chart, stickers); however, few years later, the benefits of the intervention on the rate of adequate prescription were lost.18 Automated oxygen-titration systems have been recently developed in an attempt to resolve this problem.19–21 The FreeO2 system, in particular, was designed to automatically titrate, every second, the oxygen flow delivered to patients as they breathe spontaneously. The flow adjustment is based on the target for saturated pulse oxygen (SpO2) set by the clinician. Its main objective is to reduce hyperoxia and hypoxaemia, automatically perform patient oxygen weaning while reducing caregiver workload, and improve monitoring.19 22
By better managing patient oxygen needs through automated oxygen titration and weaning, the FreeO2 system could reduce the risks of medical complications and promote shorter duration of oxygen therapy and hospital stays so that patients could more rapidly resume to their normal quality of life and their normal activities. To date, only two studies on this technology involving hospitalised patients have been conducted: one with patients with COPD hospitalised for acute exacerbations22; the other with patients admitted to emergency departments for acute respiratory distress.23 Neither of these studies assessed the cost-effectiveness of the FreeO2 system.
Objective
The objective of this study was to assess the cost-effectiveness ratio of FreeO2 technology based on data from a randomised controlled study comparing automated and manual oxygen titration in patients with COPD hospitalised for acute exacerbations.22
Methods
We conducted a cost-effectiveness analysis using bootstrapping (data resampling)24 and the criteria in the Consolidated Health Economic Evaluation Reporting Standards checklist.25 The analysis perspective was hospital costs to Quebec’s healthcare system over 180 days subsequent to the initial hospitalisation. A microcosting (or bottom-up) approach was used to collect data.
Target population
We used the same database as the first study on FreeO2 with patients with COPD.22 That study—conducted between 2011 and 2015—was a randomised clinical trial of 50 patients over the age of 40 hospitalised for acute exacerbations. The patients were randomly separated into two groups of 25. Only one of the two oxygen-titration methods (FreeO2 or manual) was used for the patients in each group during their hospital stay. Two patients in the FreeO2 group and one in the control group withdrew during the study. Our study therefore included 23 patients in the FreeO2 group and 24 in the control group. Note that patients were on FreeO2 (or manual) until weaning of oxygen therapy. In this study, some patients (not all) used FreeO2 during mobilisation (ie, walk in the corridors).
Interventions assessed
We compared the FreeO2 system (OxyNov, Quebec, QC, Canada)—the new automated oxygen-titration technology—to manual oxygen titration using the standard flowmeter (Western Medica, Westlake, Ohio, USA) currently in use at the Institut Universitaire de Cardiologie et de Pneumologie de Québec—Université Laval (IUCPQ-UL). The FreeO2 system automatically adjusts oxygen flow delivered through a nasal cannula or a simple mask according to an algorithm based on the patient’s physiological data, in particular, the patient’s SpO2, which is continually measured. As a result, FreeO2 provides continuous monitoring of respiratory parameters in spontaneously breathing patients.19 In contrast, manual oxygen titration was conducted by nurses each time the target SpO2 was not reached based on local protocols.
Principal outcome indicator
We used the incremental cost-effectiveness ratio (ICER)24 to assess the cost-effectiveness of FreeO2 technology. This ratio corresponds to the difference in costs (ΔC) divided by the difference in effects (ΔE) of two interventions, namely: ICER = (CostFreeO2 – CostManual) / (EffectFreeO2 – EffectManual).
Effectiveness measurement
Given the clear recommendations for oxygenation targets for patients with COPD,14 the main effectiveness variable was the proportion of time spent by the patient at the target SpO2 (±2%). The data were systematically measured in both two groups by an oximeter transducer placed on the patient’s finger. We also conducted analyses with two other effectiveness variables: percentage of time spent in hyperoxia and percentage of time spent in severe hypoxaemia. Hyperoxia was deemed to be when the patient’s SpO2 was five percentage points above the target and severe hypoxaemia when the patient’s SpO2 was <85%.
Cost estimates
This study included all the costs related to the patients’ hospitalisation on inclusion, as well as rehospitalisation costs at 180 days. These costs were broken down into two categories: clinical costs and compressible costs for clinical support activities. The clinical costs included remuneration for physicians and nursing staff as well as all other costs for medications, consumables, diagnostic tests and miscellaneous items. The compressible costs for clinical support activities included costs to support clinical activities and that can be affected by the duration and nature of the clinical activities (eg, diet, laundry, archives and supernumerary staff). The incompressible costs for clinical support activities (eg, safety services, general management and computer science) were excluded. Costs for depreciation and using the technology were included in the calculations based on information provided by the manufacturer. All costs are expressed in 2015 Canadian dollars ($C). The data were collected in current dollars and then actualised using the Consumer Price Index provided by Statistics Canada.26
Data collection
The data were collected from the pilot study’s clinical database,22 examination of patient clinical records and IUCPQ-UL financial databases, as well as discussions with healthcare staff to provide us with information about some resources used to deliver various clinical activities to hospitalised patients with COPD (see the details in online supplementary appendix 1).
bmjopen-2017-018835supp001.pdf (3.2MB, pdf)
Model selection
Various bootstrap resampling techniques with 5000 replications were used. This choice was dictated by the small size of our sample (ie, n=47). We conducted both univariate and multivariate bootstrap analyses. The explanatory variables used for the multivariate bootstrap corresponded to the intervention assessed (ie, whether FreeO2 technology was used or not) and several variables in the literature for accounting for the length and frequency of hospitalisations for exacerbations in patients with COPD (ie, for the cost variable), as well as to account for the intervention’s effectiveness (ie, effectiveness variables). These variables of control were the age of the patient, the forced expiratory volume in per cent, hypercapnia, diabetes, diabetes or smoking, number of hospitalisation 12 months preinclusion and number of emergency department visits 12 months preinclusion.27–32
Statistical analysis
For continuous and normally distributed variables, Student’s t-tests were conducted between groups. Wilcoxon rank sum tests were performed for data that did not fulfil the normality assumption. Categorical variables were compared using Χ2 exact tests. Four ICER calculations were made: manual, non-parametric bootstrap, univariate parametric bootstrap and multivariate parametric bootstrap. For the parametric bootstraps, Spearman’s correlation tests were carried out in order to choose an estimation method: seemingly unrelated regression (SUR) or ordinary least squares. The ICER was calculated using the ratios of the coefficients obtained in the simulations with bootstrap resampling. In the case of the non-parametric bootstrap, once the data had been resampled and the averages of the cost and effectiveness variables for each group calculated, we calculated the ICER using the usual equation: bsICER=(1/B)×Σb=1,B bsICERb.33 34 To correct for estimate bias, we subtracted the bootstrap result from twice the ICER calculated manually: bsICERbc=2×ICER–bsICER. Any results at the threshold of 95% were considered statistically significant.
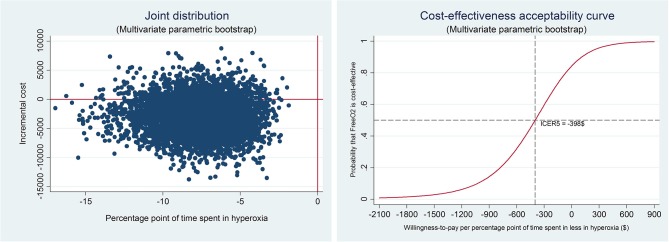
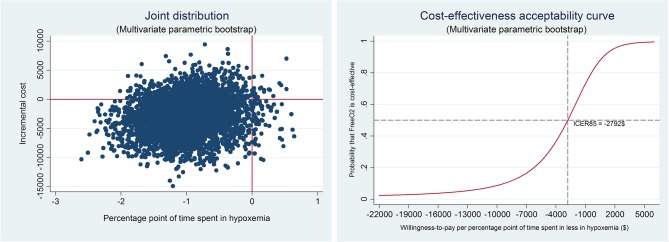
To visually present our results, we generated joint-distribution diagrams and cost-effectiveness acceptability curves. The cost-effectiveness acceptability curves provided for comparing cost-effectiveness ratios for various cost thresholds per unit of gain on a probabilistic basis.35
Results
Descriptive statistics
Table 1 provides the details of the cost data. Table 2 gives the main characteristics of the study participants. Table 1 breaks the clinical costs down into major categories, whereas the compressible costs for clinical support activities were organised in a single category (see online supplementary table A1 for details about the compressible costs). Table 1 indicates that hospitalisation expenditures on inclusion represent the major portion of total expenditures (55.7%), followed by rehospitalisation expenditures (44.3%). In the case of rehospitalisations, up to five rehospitalisation episodes per patient were observed in the 180 days subsequent to patient inclusion. It should be noted that the FreeO2 technology was used solely for the initial hospitalisation; patients received only manual titration when rehospitalised.
Table 1.
Cost structure per patient and by sector of activity (2015 $C)
| Group | Overall (n=47) | Control (n=24) | FreeO2 (n=23) |
| Emergency | 261.48 | 257.71 | 265.40 |
| Nursing | |||
| Medicine units | 2422.04 | 2627.99 | 2 207.14 |
| Intensive care | 157.90 | 309.23 | 0.00 |
| Outpatient consultations | 1.01 | 1.35 | 0.65 |
| Day medicine | 3.45 | 6.76 | 0.00 |
| Subtotal | 2584.41 | 2945.33 | 2207.79 |
| Medical imaging and nuclear medicine | 207.55 | 259.08 | 153.79 |
| Laboratories | 354.30 | 418.25 | 287.57 |
| Pharmacy | |||
| Labour | 235.94 | 278.89 | 191.12 |
| Supplies | 378.23 | 461.38 | 291.48 |
| Subtotal | 614.17 | 740.27 | 482.60 |
| Endoscopy | 99.74 | 80.63 | 119.68 |
| Occupational therapy | 57.10 | 83.23 | 29.83 |
| Physiotherapy | 139.89 | 145.00 | 134.55 |
| Social services | 92.27 | 81.08 | 103.95 |
| Respiratory physiology | 11.94 | 13.87 | 9.92 |
| Respiratory therapy | 564.71 | 687.60 | 436.47 |
| Compressible costs for clinical support activities | 968.72 | 1127.36 | 803.18 |
| Specialist costs | |||
| Pneumology | 820.39 | 904.39 | 732.74 |
| Other specialties | 260.70 | 290.73 | 229.37 |
| Subtotal | 1081.09 | 1195.12 | 962.11 |
| FreeO2 depreciation | 26.41 | – | 53.97 |
| O2 flowmeter depreciation | 0.15 | 0.30 | – |
| O2 use | 76.99 | 105.27 | 47.48 |
| Hospitalisation subtotal | 7140.91 | 8 140.10 | 6098.30 |
| Rehospitalisation costs | |||
| Direct and indirect | 4814.13 | 5156.31 | 4457.09 |
| Medical specialists | 862.65 | 969.67 | 750.97 |
| Subtotal | 5676.78 | 6125.98 | 5208.06 |
| Total costs | 12 817.69 | 14 266.08 | 11 306.36 |
Source: data expressed as mean. Calculations provided by the authors and Direction de la performance clinique et organisationnelle, Institut Universitaire de Cardiologie et de Pneumologie de Québec— Université Laval.
Table 2.
Descriptive statistics per treatment group
| Control (n=24) | FreeO2 (n=23) | P value | |
| Total expenditures (2015 $C) | 10 269.79* (6448.28 to 17 785.93) |
5678.99* (4457.01 to 11 101.05) |
0.13 |
| Time spent at the target SpO2 (%) | 48.19* (39.86 to 64.87) | 83.83* (72.77 to 92.74) | 0.00 |
| Time spent in hyperoxia (%) | 6.33* (3.02 to 10.46) | 0.82* (0.20 to 2.06) | 0.00 |
| Time spent in hypoxaemia (%) | 1.32* (0.16 to 2.65) | 0.08* (0.04 to 0.18) | 0.00 |
| Length of hospitalisation (days) | 7.5* (6.0 to 11.0) | 6.0* (5.0 to 8.0) | 0.08 |
| Length of rehospitalisation (days)† | 0.5* (0.0 to 13.0) | 0.0* (0.0 to 7.17) | 0.47 |
| Length of rehospitalisation (days)‡ | 13.5* (5.43 to 21.0) | 20.0* (6.73 to 27.33) | 0.37 |
| Total number of rehospitalisation at 180 days | 21 | 9 | 0.09 |
| Rate of rehospitalisation at 180 days (%)§ | 50.00 (51.07) | 34.78 (48.70) | 0.29 |
| One rehospitalisation at 180 days (%) | 25.00 (9.03) | 30.43 (9.81) | 0.69 |
| Two or more rehospitalisations at 180 days (%) | 25.00 (9.03) | 4.35 (4.35) | 0.05 |
| Duration of oxygen therapy (days) | 5.5* (3.0 to 6.0) | 4.0* (2.26 to 5.0) | 0.12 |
| Oxygen consumption (L/min) | 0.69* (0.58 to 1.31) | 0.56* (0.33 to 0.76) | 0.05 |
| Total oxygen consumption (L) | 6192.0* (2687.4 to 10 969.4) | 3600.0* (1553.2 to 4426.3) | 0.05 |
| FEV1 on inclusion (% predicted) | 35.5* (30.7 to 43.7) | 32.0* (27.3 to 41.5) | 0.34 |
| Diabetic (%) | 37.50 (49.45) | 26.09 (44.90) | 0.40 |
| Active smoker (%) | 25.00 (44.23) | 47.83 (51.08) | 0.10 |
| Diabetic or active smoker (%) | 58.33 (50.36) | 65.22 (48.70) | 0.62 |
| Hypercapnia (PaCO2 >45 mm Hg) on inclusion (%) | 54.17 (50.90) | 34.78 (48.70) | 0.18 |
| Respiratory rate on inclusion (bpm) | 21.38 (2.26) | 21.83 (2.87) | 0.55 |
| Female (%) | 50.00 (51.07) | 43.48 (50.69) | 0.65 |
| Age (years) | 73.17 (8.62) | 71.17 (8.33) | 0.42 |
| Body mass index (kg/m²) | 26.97 (5.63) | 27.06 (6.34) | 0.96 |
| No. of hospitalisations in the 12 months preinclusion | 0.0* (0.0 to 1.0) | 0.0* (0.0 to 1.0) | 0.52 |
| No. of emergency department visits in the 12 months preinclusion | 1.0* (0.0 to 2.0) | 1.0* (0.0 to 1.0) | 0.97 |
| Hospitalised in the month preinclusion (%) | 12.50 (33.78) | 8.70 (28.81) | 0.67 |
Data expresses as mean with SD in parentheses, unless otherwise specified.
*Median and 95% CI in parentheses.
†Total number of days of rehospitalisation out of 180 days divided by the total number of patients (rehospitalised or not).
‡Length of rehospitalisation solely for rehospitalised patients.
§Percentage of the total of patients in that group that has one or more rehospitalisations in the 180 days.
FEV1, forced expiratory volume in 1 s.
The control group generated more costs than the FreeO2 group (ie, a mean difference of $C2959.71, equivalent to a 20.7% reduction) and none of the patients in the FreeO2 group required intensive care. In addition, the per-patient depreciation cost for the FreeO2 technology is relatively low despite the fact that we used the upper limit of the manufacturer’s suggested price (ie, $C12 000+annual operating costs).
Table 2 indicates that while there was a strong per-patient cost difference between the two groups, it was nevertheless not statistically significant (P=0.13). In contrast, in the case of effectiveness variables, the patients in the FreeO2 group spent significantly more time at the target SpO2 and less time spent in hyperoxia and hypoxaemia (P<0.001). In addition, we noted that the control-group patients spent more days hospitalised than the patients in the FreeO2 group. Similarly, the patients in the FreeO2 group spent, on average, fewer days on oxygen than those in the control group. This made it possible to save about $C57.79 on average per patient in oxygen costs, which is more than the per-patient depreciation cost for the FreeO2 system. Lastly, the patients did not appear to present any statistically significant differences in terms of clinical or demographic characteristics on inclusion.
Incremental cost-effectiveness ratio
Manual calculation
To note that to calculate an ICER, means are used and not medians. These values for the effectiveness variables are provided in online supplementary table A2. The ICER calculation is ($C11 306.36–$C14 266.08)/(81.19–51.94)=−$C101.21 per percentage point of additional time spent at the target SpO2. This ratio indicates that FreeO2 technology allows Quebec’s healthcare system to save $C101.21 per percentage point of additional time spent at the target SpO2. In other terms, compliance with oxygen-therapy recommendations is possible with FreeO2 without incurring additional costs, and using the technology will very probably yield lower costs. On a per-COPD-patient basis, that is equal to an average of 29.25 percentage points of additional time spent at the target SpO2 and a savings of $C2959.71 with FreeO2.
We used various bootstrap methods to calculate SD and CIs in order to estimate by how much the ratio might vary.
Bootstrap calculations
We calculated an ICER associated with the generated sample for each bootstrap resampling. The final ICER corresponds to the average of all the ICERs for each of the 5000 replications. In the case of the parametric bootstrap, all of our Spearman’s correlation results indicate a correlation between the cost variable and our three effectiveness variables (see online supplementary table A3). We therefore opted for an SUR model to calculate the difference between the average costs and average effects (see online supplementary table A4).
Table 3 summarises the ICERs obtained for each calculation method. Each time, the different ICERs were of relatively similar orders of magnitude. Given that multivariate bootstrapping provides for correcting differences related to patient characteristics, the results associated with this method serve as reference points. Consequently, an ICER of −$C96.91 per percentage point of additional time spent at the target SpO2 was observed. This outcome is not statistically significant at the threshold of 95%. That notwithstanding, when bias correction is applied with the normal CI, the ICER becomes significant. Similar results have been observed with the ICER associated with hyperoxia, but not for hypoxaemia, which indicates greater heterogeneity for this variable.
Table 3.
Incremental cost-effectiveness ratios (ICERs)
| ICER | ICER corrected for bias | Normal CI | Percentile CI (95%) | Normal CI (corrected for bias) |
||
| Target | Simple | −101.21 | – | – | – | – |
| Non-parametric BS | −104.55 | −97.87 | (−107.88 to −101.21) | (−352.59 to 120.26) | (−101.21 to −94.53) | |
| Univariate parametric BS | −96.58 | −105.84 | (−99.77 to −93.38) | (−312.78 to 144.74) | (−109.03 to −102.65) | |
| Multivariate parametric BS | −96.91 | −105.51 | (−99.84 to −93.99) | (−301.26 to 116.96) | (−108.43 to −102.59) | |
| Hyper | Simple | −369.22 | – | – | – | – |
| Non-parametric BS | −395.93 | −342.51 | (−408.95 to −382.91) | (−1380.61 to 467.07) | (−355.53 to −329.49) | |
| Univariate parametric BS | −379.03 | −359.41 | (−391.94 to −366.12) | (−1,294.23 to 537.07) | (−372.32 to −346.50) | |
| Multivariate parametric BS | −411.09 | −327.35 | (−424.28 to −397.91) | (−1,442.43 to 437.01) | (−340.54 to −314.16) | |
| Hypox | Simple | −1565.46 | – | – | – | – |
| Non-parametric BS | −1709.95 | −1420.97 | (−1766.64 to −1653.25) | (−6265.24 to 1894.99) | (−1477.67 to −1364.27) | |
| Univariate parametric BS | −1661.46 | −1469.46 | (−1718.62 to −1604.29) | (−5,911.79 to 2367.25) | (−1526.62 to −1412.30) | |
| Multivariate parametric BS | −2250.04 | −880.88 | (−4841.99 to 341.92) | (−17 091.61 to 6560.38) | (−3472.84 to 1711.01) | |
Target, percentage of time spent at the target SpO2.
BS, bootstrap; Hyper, percentage of time spent in hyperoxia (SpO2+5% above the target); Hypox, percentage of time spent in hypoxaemia (SpO2 <85%).
Joint-distribution diagrams and cost-effectiveness acceptability curves
As can be seen in the joint-distribution diagrams, the large majority of bootstrap points are located in the negative part of the incremental cost (figures 1–3 for multivariate parametric bootstrap; online supplementary figures A1-A6 for non-parametric and univariate parametric bootstrap). In the case of the diagrams with the percentage of time spent in hyperoxia (Hyper) or percentage of time spent in hypoxaemia (Hypox), the incremental target appears as a negative variation because the objective here of achieving better oxygen titration is to reduce these time percentages.
Figure 1.
Joint distribution and incremental cost-effectiveness acceptability curve for time spent at the target SpO2 (multivariate parametric bootstrap). ICER, incremental cost-effectiveness ratio.
Figure 2.
Joint distribution and incremental cost-effectiveness acceptability curve for time spent in hyperoxia (multivariate parametric bootstrap). ICER, incremental cost-effectiveness ratio.
Figure 3.
Joint distribution and incremental cost-effectiveness acceptability curve for time spent in hypoxaemia (multivariate parametric bootstrap). ICER, incremental cost-effectiveness ratio.
In examining the cost-effectiveness acceptability curve for the percentage of time spent at the target SpO2, it can be seen that the FreeO2 system has a probability of over 80% of being cost-effective given a zero willingness to pay (figure 1). For a willingness to pay of $C100 per percentage point gained at the target SpO2, the probability is 96%. The FreeO2 system is, moreover, 100% cost-effective with a willingness to pay of only $C200 per additional percentage point of time spent at the target SpO2. In the case of hyperoxia and hypoxaemia, the cost-effectiveness probabilities associated with a zero willingness to pay are higher, namely, 85% and 90%, respectively.
Discussion
General observation
This study examined the cost-effectiveness ratio of the new FreeO2 oxygen-titration technology in patients with COPD hospitalised for acute exacerbations. The comparison with conventional manual oxygen-titration indicates that FreeO2 technology is more cost-effective. Nevertheless, the study was conducted on a small sample, and the definitely large difference observed in the per-patient costs was not statistically significant. A study on a larger patient sample would quite probably confirm a reduction of >20% in the per-patient costs observed over 180 days. In fact, the savings achieved for a patient with COPD hospitalised for acute exacerbations averaged $C2960 herein. Consequently, it can be concluded that the relatively high cost of the FreeO2 automated titration system (ie, 100 times higher than the manual system) as well as its shorter life cycle, are not economic issues given the savings and health outcomes that it yields. From the clinical standpoint, FreeO2 technology indeed offers a definite advantage over conventional manual titration because it can maintain patients at the right target SpO2 longer, thereby reducing the risks of hypoxaemia and hyperoxia.
Despite the small size of our sample, our results remain stable and indicate that the FreeO2 system is in all probability cost-effective (ie, probability higher than 80% for a zero willingness to pay). The ICERs could nevertheless vary marginally with new underlying assumptions related to the cost of the technology and depreciation time. To illustrate, varying the depreciation of the FreeO2 device from 7 to 5 years yields an ICER of −$C100.47 per additional percentage point of time spent at the target SpO2. Moreover, based on our calculations while keeping all the other variables constant, the FreeO2 system would have to cost $C607 619.65 to yield the same ICER as a conventional manual titration device. A simple return-on-investment calculation also indicates that acquiring a FreeO2 device maintained over 7 years would pay for itself in <3 months, that is, after only eight to nine hospitalised patients.
As in all cost studies, it is difficult to generalise our results to other countries. Indeed, manufacturers can have very different cost structures and prices. Nevertheless, since the main cost factors in our study were hospitalisation and the number of rehospitalisations, it would appear likely that another such study conducted in a country with a healthcare system that shares many characteristics with Quebec’s could yield similar results. For example, extrapolating the clinical data of the study conducted by Lellouche et al 22 with patients with COPD in France could yield an ICER of −€48.41 (ie, $C72.63 at an exchange rate of €1 for $C1.5) per additional percentage point of time spent at the target SpO2. Indeed, based on the cost guidelines in France,36 the average cost at 180 days for a patient with COPD would be €6841.74. Applying a cost reduction of 20.7%, as in our study, for a gain of 29.25 percentage points at the target SpO2, would give an ICER of −€48.41. Moreover, it should be noted that the length of hospitalisation for acute exacerbations is about the same in our study and in France.37 In contrast, it would be more difficult to extrapolate results in the case of other countries, such as the USA, that have very different healthcare systems and often shorter hospital stays.38
To the best of our knowledge, there are two other automated systems on the market for adjusting oxygen flow. One has an algorithm adapted to a premature population39 40 and is integrated into an intensive care ventilator. Because of its specificities, this system is not actually comparable to the FreeO2 system. Moreover, we know of no cost-effectiveness studies on it. There is also an automated oxygen regulator marketed in Europe (O2 Flow Regulator, Dima Italia LRS, Bologna, Italy), but there have been few clinical assessments of it and there are no data on it in a context of COPD acute exacerbations.21
Strengths and weaknesses
This study was the first to conduct a cost-effectiveness analysis of automated oxygen-titration technology. The study’s main strength is that we were able to collect cost and effectiveness data for each of the patients using a bottom-up approach. As a result, we were able to very accurately measure individual variability, which allows us to be very confident about the degree of accuracy of our results. Another strength of our study is that we resampled a large number of times in order to reduce the bias related to its small size. Nevertheless, as an effect of a bottom-up approach, the initial sample showed high variability in the cost data, which led the bootstrap to simulate samples with value distributions containing a large number of extreme values. These extreme values broadened the CIs and consequently reduced the significance of the observed cost difference. One limitation of the study is thus the relatively small sample size of the population that may have influenced the results. The initial study was a pilot study and the cost-effectiveness outcomes used in the current study were not the primary outcomes in this pilot study. Larger randomised controlled studies will be required to confirm these results. Another limitation relates to some of the cost data collected. Specifically, we had to assign costs based on the averages in available data for the remuneration of specialists other than pneumologists. Since these costs amounted only to a few hundred dollars, this limitation is very unlikely to affect our results. Moreover, rehospitalisation costs herein are biased against the FreeO2 group insofar as all rehospitalised patients were systematically oxygenated with a conventional flowmeter and not with the FreeO2 system. Considering the shorter hospital stays among patients oxygenated with FreeO2, it is very likely that this group would have had shorter rehospitalisation stays if they had received oxygenation with FreeO2 technology for their subsequent hospitalisations. Consequently, the cost reduction observed in our study might have been even greater.
Conclusion
In our study, we observed a 20.7% reduction in costs with FreeO2 technology for an increased effectiveness of 56.3% at the target SpO2 (ie, the percentage of time at the target increased from 51.94% to 81.19%). Automated oxygen titration with FreeO2 therefore appears very cost-effective, and it would, in all probability, be very advantageous for the healthcare system to have this technology.
This technology delivers optimised oxygen therapy and allows patients with COPD to return home faster (which is the objective of all healthcare systems), and it yields substantial savings with patients with COPD hospitalised for acute exacerbations. The growing number of patients with COPD worldwide and in the Canadian population, in particular, must give pause for reflection on how to effectively manage such patients. A technology such as the FreeO2 system could therefore prove very useful in achieving this objective. At IUCPQ-UL, that could potentially yield savings of about $C1 468 000 per year (ie, $C2960 for 496 hospitalised patients). In the case of Quebec, where hospitals operate on a fixed-budget basis, the savings generated will make it possible to fund other activities or treat a larger number of patients with the same number of beds.
Supplementary Material
Acknowledgments
The authors are grateful to Dr Mathieu Simon, Jean-Luc Balzer, Djamel Zekri, Michelle Martineau, Josiane Courteau, Francine Lecours, Mendy Malachy and Alexandre Grenon Morin for their support and expert advice. TGP is member of the FRQS-funded Centre de recherche du CHUS.
Footnotes
Contributors: TGP, CRCK and FL conceived the study. TGP, PAB and VT collected the data. TGP, CRCK, SB, FM and FL participated to the analysis of data. TGP and CRCK conducted the bootstrap simulations. TGP and CRCK wrote the manuscript. All authors revised and approved the manuscript.
Funding: This research received support under Mitacs Acceleration programme. The Mitacs Acceleration programme is cofunded by Innovation, Sciences and Economic Development Canada (ISED) and the industry (Oxynov in this case). The funding body did not influence the study design and analysis.
Disclaimer: The funding body did not influence the study design and analysis.
Competing interests: FL is the coinventor of the FreeO2 system and cofounder of Oxynov, the firm that developed and productionised the FreeO2 system for marketing. The Fonds de Recherche en Santé du Québec contributes to Dr François Lellouche salary for research activities (clinical research scholar) and to the research assistant’s salary (clinical research grant). FM holds a GlaxoSmithKline/Canadian Institutes of Health Research chair on COPD at Laval University. FM participates in Innovair, a company that owns shares in OxyNov, the owner of the FreeO2 device.
Patient consent: Obtained.
Ethics approval: The RCT was approved by the Institutional Ethics Committee of the IUCPQ (# 20694), and a signed consent was obtained from each participant.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data sharing statement: Data are available on request to the corresponding author.
References
- 1. World Health Organization. Chronic obstructive pulmonary disease (COPD). 2016. http://www.who.int/respiratory/copd/en/ (accessed 23 Nov 2016).
- 2. Khakban A, Sin DD, FitzGerald JM, et al. . The Projected Epidemic of COPD Hospitalizations Over the Next 15 Years: A Population Based Perspective. Am J Respir Crit Care Med 2016. 10.1164/rccm.201606-1162PP [DOI] [PubMed] [Google Scholar]
- 3. Statistique Canada. Enquête sur la santé dans les collectivités canadiennes. 2010. http://www.cadretravailpulmonaire.ca/santerespiratoireauCanada/ (accessed 23 Nov 2016).
- 4. Agence de la santé publique du Canada. Faits saillants sur la maladie pulmonaire obstructive chronique (MPOC). 2011. http://www.phac-aspc.gc.ca/cd-mc/publications/copd-mpoc/ff-rr-2011-fra.php (accessed 23 Nov 2016).
- 5. Mittmann N, Kuramoto L, Seung SJ, et al. . The cost of moderate and severe COPD exacerbations to the Canadian healthcare system. Respir Med 2008;102:413–21. 10.1016/j.rmed.2007.10.010 [DOI] [PubMed] [Google Scholar]
- 6. GBD 2015 Chronic Respiratory Disease Collaborators. Global, regional, and national deaths, prevalence, disability-adjusted life years, and years lived with disability for chronic obstructive pulmonary disease and asthma, 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet Respir Med 2017;5:691–706. 10.1016/S2213-2600(17)30293-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Toy EL, Gallagher KF, Stanley EL, et al. . The economic impact of exacerbations of chronic obstructive pulmonary disease and exacerbation definition: a review. COPD 2010;7:214–28. 10.3109/15412555.2010.481697 [DOI] [PubMed] [Google Scholar]
- 8. Wier LM, Elixhauser A, Pfuntner A, et al. . OvervIew of hospitalizations among patients with COPD, 2008. Statistical Brief #106 2011. [PubMed] [Google Scholar]
- 9. Ford ES, Murphy LB, Khavjou O, et al. . Total and state-specific medical and absenteeism costs of COPD among adults aged ≥ 18 years in the United States for 2010 and projections through 2020. Chest 2015;147:31–45. 10.1378/chest.14-0972 [DOI] [PubMed] [Google Scholar]
- 10. Austin MA, Wills KE, Blizzard L, et al. . Effect of high flow oxygen on mortality in chronic obstructive pulmonary disease patients in prehospital setting: randomised controlled trial. BMJ 2010;341:c5462 10.1136/bmj.c5462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lellouche F, Lipes J, L’Her E. Optimal oxygen titration in patients with chronic obstructive pulmonary disease: a role for automated oxygen delivery? Can Respir J 2013;20:259–61. 10.1155/2013/376545 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Claure N, Bancalari E. Automated closed loop control of inspired oxygen concentration. Respir Care 2013;58:151–61. 10.4187/respcare.01955 [DOI] [PubMed] [Google Scholar]
- 13. Cousins JL, Wark PA, McDonald VM. Acute oxygen therapy: a review of prescribing and delivery practices. Int J Chron Obstruct Pulmon Dis 2016;11:1067–75. 10.2147/COPD.S103607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. O’Driscoll BR, Howard LS, Davison AG. British Thoracic Society. BTS guideline for emergency oxygen use in adult patients. Thorax 2008;63(Suppl 6):68 10.1136/thx.2008.102947 [DOI] [PubMed] [Google Scholar]
- 15. Global Initiative for Chronic Obstructive Lung Disease - GOLD. Global strategy for diagnosis, management, and prevention of COPD, 2016. [Google Scholar]
- 16. Ringbaek TJ, Terkelsen J, Lange P. Outcomes of acute exacerbations in COPD in relation to pre-hospital oxygen therapy. Eur Clin Respir J 2015;2:27283 10.3402/ecrj.v2.27283 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hale KE, Gavin C, O’Driscoll BR. Audit of oxygen use in emergency ambulances and in a hospital emergency department. Emerg Med J 2008;25:773–6. 10.1136/emj.2008.059287 [DOI] [PubMed] [Google Scholar]
- 18. Myers H, Taylor J, Finn RS, et al. . Doctors learn new tricks, but do they remember them? Lack of effect of an educational intervention in improving Oxygen prescribing. Respirology 2015;20:1229–32. 10.1111/resp.12614 [DOI] [PubMed] [Google Scholar]
- 19. Lellouche F, L’her E. Automated oxygen flow titration to maintain constant oxygenation. Respir Care 2012;57:1254–62. 10.4187/respcare.01343 [DOI] [PubMed] [Google Scholar]
- 20. Rice KL, Schmidt MF, Buan JS, et al. . AccuO2 oximetry-driven oxygen-conserving device versus fixed-dose oxygen devices in stable COPD patients. Respir Care 2011;56:1901–5. 10.4187/respcare.01059 [DOI] [PubMed] [Google Scholar]
- 21. Cirio S, Nava S. Pilot study of a new device to titrate oxygen flow in hypoxic patients on long-term oxygen therapy. Respir Care 2011;56:429–34. 10.4187/respcare.00983 [DOI] [PubMed] [Google Scholar]
- 22. Lellouche F, Bouchard PA, Roberge M, et al. . Automated oxygen titration and weaning with FreeO2 in patients with acute exacerbation of COPD: a pilot randomized trial. Int J Chron Obstruct Pulmon Dis 2016;11:1983–90. 10.2147/COPD.S112820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. L’Her E, Dias P, Gouillou M, et al. . Automation of oxygen titration in patients with acute respiratory distress at the emergency department. A multicentric international randomised controlled study. Intensive Care Med Exp 2015;3:A424 10.1186/2197-425X-3-S1-A424 [DOI] [Google Scholar]
- 24. Ramsey S, Willke R, Briggs A, et al. . Good research practices for cost-effectiveness analysis alongside clinical trials: the ISPOR RCT-CEA Task Force report. Value Health 2005;8:521–33. 10.1111/j.1524-4733.2005.00045.x [DOI] [PubMed] [Google Scholar]
- 25. Husereau D, Drummond M, Petrou S, et al. . Consolidated Health Economic Evaluation Reporting Standards (CHEERS) Statement. Value in Health 2013;16:e1–e5. 10.1016/j.jval.2013.02.010 [DOI] [PubMed] [Google Scholar]
- 26. Statistique Canada. Indice des prix à la consommation, par province (Québec). 2016. http://www.statcan.gc.ca/tables-tableaux/sum-som/l02/cst01/econ09f-fra.htm (accessed 24 Nov 2016).
- 27. Villalta J, Sequeira E, Cereijo A-C, et al. . Factors predicting a short length of stay for acute exacerbations of chronic obstructive pulmonary disease]. Med Clin 2005;124:648–50. [DOI] [PubMed] [Google Scholar]
- 28. Bahadori K, FitzGerald JM. Risk factors of hospitalization and readmission of patients with COPD exacerbation--systematic review. Int J Chron Obstruct Pulmon Dis 2007;2:241–51. [PMC free article] [PubMed] [Google Scholar]
- 29. Gadoury M-A, et al. . Self-management reduces both short- and long-term hospitalisation in COPD. Eur Respir J 2005;26:853–7. 10.1183/09031936.05.00093204 [DOI] [PubMed] [Google Scholar]
- 30. Yohannes AM, Connolly MJ. Predictors of hospital admission and mortality in patients with chronic obstructive pulmonary disease. Rev Clin Gerontol 2001;11:99–106. 10.1017/S0959259801011194 [DOI] [Google Scholar]
- 31. Wang Y, Stavem K, Dahl F, et al. . Factors associated with a prolonged length of stay after acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Int J Chron Obstruct Pulmon Dis 2014;9:99–105. 10.2147/COPD.S51467 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. LAU AC-W, YAM LY-C, Poon E. Hospital re-admission in patients with acute exacerbation of chronic obstructive pulmonary disease. Respir Med 2001;95:876–84. 10.1053/rmed.2001.1180 [DOI] [PubMed] [Google Scholar]
- 33. Burton A, Billingham LJ, Bryan S. Cost-effectiveness in clinical trials: using multiple imputation to deal with incomplete cost data. Clinical Trials 2007;4:154–61. 10.1177/1740774507076914 [DOI] [PubMed] [Google Scholar]
- 34. Black WC. The CE plane: a graphic representation of cost-effectiveness. Med Decis Making 1990;10:212–4. 10.1177/0272989X9001000308 [DOI] [PubMed] [Google Scholar]
- 35. Fenwick E, O’Brien BJ, Briggs A. Cost-effectiveness acceptability curves– facts, fallacies and frequently asked questions. Health Econ 2004;13:405–15. 10.1002/hec.903 [DOI] [PubMed] [Google Scholar]
- 36. Agence technique de l’information sur l’hospitalisation. Référentiel de coûts MCO 2013 | Stats ATIH. 2013. http://www.scansante.fr/r%C3%A9f%C3%A9rentiel-de-co%C3%BBts-mco-2013 (accessed 24 Nov 2016).
- 37. Fuhrman C, Roche N, Vergnenègre A, et al. . Hospital admissions related to acute exacerbations of chronic obstructive pulmonary disease in France, 1998–2007. Respir Med 2011;105:595–601. 10.1016/j.rmed.2010.11.014 [DOI] [PubMed] [Google Scholar]
- 38. Jinjuvadia C, Jinjuvadia R, Mandapakala C, et al. . Trends in outcomes, financial burden, and mortality for acute exacerbation of Chronic Obstructive Pulmonary Disease (COPD) in the United States from 2002 to 2010. COPD 2016. 1 8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. van Kaam AH, Hummler HD, Wilinska M, et al. . Automated versus manual oxygen control with different saturation targets and modes of respiratory support in preterm infants. J Pediatr 2015;167:545–50. 10.1016/j.jpeds.2015.06.012 [DOI] [PubMed] [Google Scholar]
- 40. Claure N, Bancalari E. Closed-loop control of inspired oxygen in premature infants. Seminars in Fetal and Neonatal Medicine 2015;20:198–204. 10.1016/j.siny.2015.02.003 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2017-018835supp001.pdf (3.2MB, pdf)