Abstract
Patients with pubic symphysis instability who had failed nonoperative treatments may benefit from surgical repair. This disease process is rare, most commonly seen in postpartum women and athletes, and its surgical treatment is invasive and nonphysiological. Currently described surgical interventions, although limited, include plating, which provides an overly rigid construct with the risk of failure and possibly poor long-term outcomes particularly in athletes, and treatments such as curettage, more commonly used in the treatment of osteitis pubis. An emerging option is minimally invasive laparoscopic fixation using knotless anchors with a tape suture in a crisscross configuration. This possibly allows more physiological movement of the pubic symphysis in a less invasive manner. A detailed technical description and discussion of the technique are provided.
Although rare, pubic symphysis instability is seen, particularly in athletes with repetitive micro trauma as well as in urologic, gynecologic, obstetric, and other pelvis conditions. Common sports with pubis symphysis instability include contact sports such as rugby, American football, as well as extreme sports and heavy weight lifting. Postpartum mothers frequently have issues with this condition and may be the largest cohort. More common than true instability is osteitis pubis, which is a general term for painful inflammation of the pubic bones, pubic symphysis, and nearby structures.1 The cause of this condition is often difficult to ascertain. Core weakness commonly plays a role in this pathology. Furthermore, it is essential that other causes of hip pain be investigated and addressed such as underlying femoral acetabular impingement because oftentimes the issue is multifactorial.
Symptoms, again, are many times nonspecific and may include groin pain and increased pain with weight bearing and performing sport. Tenderness over the pubic symphysis with direct palpation is common without evidence of hernia. The origin of the adductors can also be tender to palpation and may be painful with resistant adduction as well as with full hip abduction. Pelvic springing in the lateral decubitus position also commonly elicits pain. Furthermore, physical examination findings can overlap with those of hip impingement such as irritability with flexion abduction external rotation and flexion adduction internal rotation. Diagnosis of true symphysis instability is multifactorial and often relies on imaging.1
Imaging modalities include standard anteroposterior pelvis and bilateral lateral views of the hips as well as weight bearing flamingo views. This specialized imaging technique evaluates vertical instability and involves the patient standing on an elevated step with one leg hanging off the edge of the step and all the patient's weight on the contralateral leg (Figs 1 and 2). This is done with both legs individually where ≥2 mm of vertical displacement indicates instability and is diagnostic. Magnetic resonance imaging can be obtained as well, particularly in the high-level athletic population, to evaluate adductor pathology, intra-articular hip pathology, and other soft tissues.
Fig 1.
Radiograph showing a flamingo view of the discussed patient standing on a step with his right leg and left leg suspended. The image shows >2 mm displacement of the pubic symphysis, indicating instability.
Fig 2.
Radiograph showing a flamingo view of the discussed patient standing on a step with his left leg and right leg suspended. The image shows >2 mm displacement of the pubic symphysis, indicating instability.
First-line treatment is nonoperative and includes nonsteroidal anti-inflammatories, rest, activity modification, pelvic therapy, physical therapy including lower abdominal and hip strengthening, ultrasound therapy, and injections. The importance of the multidisciplinary team approach including a well-trained pelvic and hip therapist is key. Pelvic stabilization and core and gluteal strengthening are paramount and many times can relieve symptoms. Patients should be reassessed after these conservative treatments have been attempted for at least 2 to 3 months. At that time if no improvement occurs, pubic symphysis direct injections can be considered. If, again, direct injections do not provide relief and the patient continues to have complaints of symptoms described previously that are unrelenting and interfere with daily life, surgical advantages and complications can be discussed (Tables 1 and 2).2
Table 1.
Indications and Contraindications of Anchor and Suture Tape Stabilization of Pubic Symphysis Instability
| Indications | Contraindications |
|---|---|
| Failure of nonoperative treatments | No trial of nonoperative treatments |
| Pubic symphysis instability ≥2 mm on flamingo radiograph view | Intra-articular hip pathology on examination with no improvement with symphysis injection |
| Magnetic resonance imaging with intra-articular hip or adductor pathology with consistent physical examination findings |
Table 2.
Advantages and Disadvantages of Anchor and Suture Tape Stabilization of Pubic Symphysis Instability
| Advantages | Disadvantages |
|---|---|
| Minimally invasive | Requires a general surgeon with laparoscopic skills |
| Less rigid construct | Technically challenging |
| Allows more physiological motion | Risk of aberrant anchor placement |
| Smaller wounds | Undertensioning may lead to continued pain |
| Less postoperative pain | Risk of inadvertent symphysis destabilization |
| Less hernia risk | Rely on implant |
| No need for hardware removal |
Surgical Technique
Surgery is rarely indicated in this condition, but if all nonoperative treatments have failed as described above, it is a viable option. In this Technical Note, an endoscopic crisscross tape suture technique using knotless suture anchors is described. Other open techniques involving plating as well as curettage have also been described.1, 3 The patient in this study is a 27-year-old woman with 1.5 years of progressive pubic symphysis pain after her second vaginal child birth. She was found to have pain over her pubis as well as instability on flamingo views. She had failed exhaustive nonoperative treatments. A step-by-step procedure can be seen in Video 1.
Patient Setup and Approach
The patient is placed in the supine position with general endotracheal anesthesia. A Foley catheter is placed to decompress the bladder. This surgery is performed laparoscopically with the assistance of a general surgeon. An infraumbilical incision is made and dissection carried down to the rectus sheath that is then opened on one side. The rectus muscle is then swept laterally and the posterior rectus sheath is identified. A dissecting balloon system is placed into the preperitoneal space toward the pubic bone and inflated under direct visualization. This space is infiltrated to a pressure of 12 mmHg. Two additional standard 5-mm laparoscopic ports are then placed in this extraperitoneal space. The space of Retzius is then opened using a laparoscopic bovie, and the bony borders of the symphysis are exposed. Its borders are probed, with care not to open the symphysis joint itself with the risk of possible further destabilization (Fig 3).
Fig 3.
Laparoscopic view of the space of Retzius showing the bilateral dissection of the pubic bone leaving the symphysis joint preserved: symphysis (white *), right pubic bone (black *), left pubic bone (black +).
Right-Sided Anchor Placement
Using fluoroscopy, the first anchor location is identified approximately 10 mm to the right of the symphysis and in line with the joint (Fig 4), allowing enough room for a second anchor 1 cm anterior to this one. The location is drilled and hand tapped, and the first 4.75-mm knotless anchor loaded with a tape-type suture is placed (Arthrex SwiveLock anchor loaded with FiberTape, Arthrex, Naples, FL). A percutaneous suprapubic portal is then placed on the patient's right to obtain a 1 cm more anterior anchor placement 90° to the first anchor and again 10 mm from the pubic symphysis. After fluoroscopic confirmation (Fig 5), this is drilled and hand tapped and a second 4.75-mm knotless anchor loaded with a tape suture is placed on the right of the pubic symphysis (Fig 6).
Fig 4.
Fluoroscopic view showing appropriate placement of the right superior anchor approximately 10 mm from and 90° to the symphysis. This anchor is placed through the standard right-sided laparoscopic port.
Fig 5.
Fluoroscopic view showing appropriate placement of the left posterior anchor approximately 10 mm from and 90° to the symphysis. This anchor is placed through the percutaneous suprapubic portal.
Fig 6.
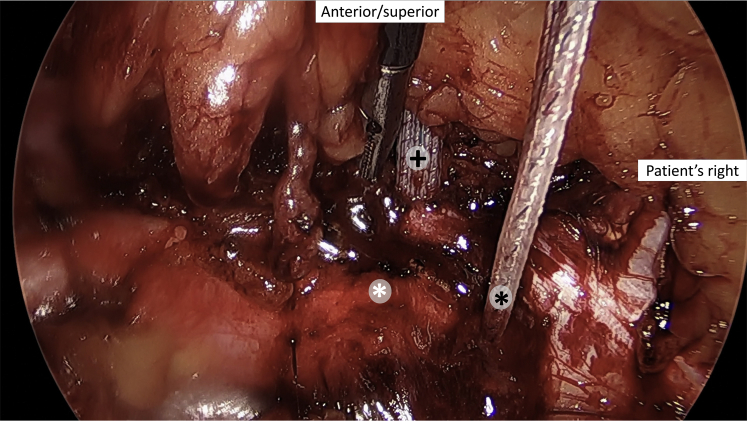
Laparoscopic view of the right superior anchor (+), right posterior anchor (black *), and pubic symphysis (white *).
Left-Sided Anchor Placement and Compression Fixation
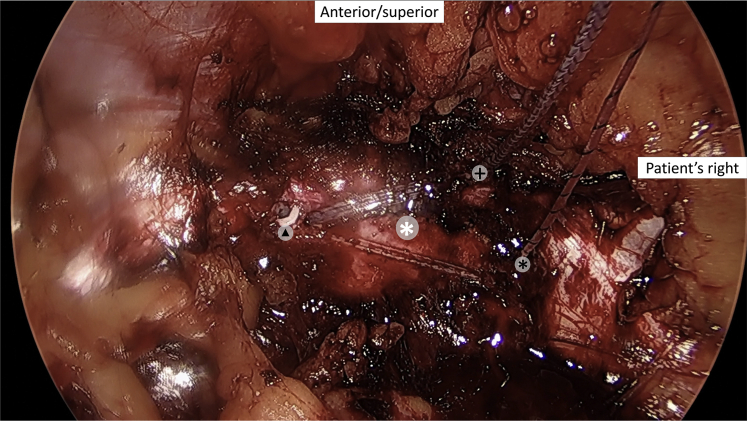
The posterior left-sided anchor location is identified again with the help of fluoroscopy in the same manner, in line with the posterior right-sided anchor, 10 mm from the symphysis at 90°. The location is then drilled through the traditional left laparoscopic portal in line with the first, posterior anchor. This is tapped and then the 4.75-mm knotless anchor is loaded with a limb from both the posterior and anterior right-sided anchor. The anchor is placed with the final tightening being performed with side-to-side compression across the pubic symphysis to provide underlying stability (Fig 7). An identical percutaneous now left-sided suprapubic incision is made and a portal placed, and an anchor is placed and drilled and tapped on the left of the symphysis, again, 90° and 10 mm to the symphysis and in line with the right anterior anchor, 1 cm from the left-sided posterior anchor. The remaining sutures from the right anterior and posterior anchors are brought through the left suprapubic cannula, and an anchor is loaded onto another 4.75-mm knotless anchor. This loaded anchor is then placed again, with side-to-side compression across the pubic symphysis manually compressing the pelvis to provide stability. A crisscrossed suture configuration is created across the pubic symphysis and completes the internal brace technique (Fig 8).
Fig 7.
Laparoscopic view of the left posterior anchor (▴), right superior anchor (+), right posterior anchor (black *), and pubic symphysis (white *).
Fig 8.
Laparoscopic view of the final construct: superior left anchor (▪), posterior left anchor (▴), superior right anchor (+), posterior left anchor (black *), and pubic symphysis (white *).
Hemostasis is assured using the laparoscope and the retroperitoneum is allowed to fall back into place. The ports are removed and the patient's anterior rectus sheath is closed with 0 Polysorb figure-of-eight suture and the skin closed with a 4-0 Polysorb subcuticular stitch and a sterile dressing is applied. A final radiograph shows the appropriate anchor placement (Fig 9). Pearls and pitfalls of the procedure are described in Table 3.
Fig 9.
Final radiograph showing appropriate anchor placement approximately 10 mm from the symphysis.
Table 3.
Pearls and Pitfalls of Anchor and Suture Tape Stabilization of Pubic Symphysis Instability
| Pearls | Pitfalls |
|---|---|
| Proper surgical indications | Did not exhaust nonsurgical treatments |
| Skilled, interested, and flexible general surgeon | Inexperienced therapist |
| Make proper laparoscopic portals to obtain the appropriate angle for anchor placement | Rule out other causes of groin pain |
| Do not destabilize the symphysis | |
| Obtain an appropriate intraoperative radiograph for anchor placement | |
| Appropriately tension tape suture |
Postoperatively, the patient is full weight bearing with limitation in activities for approximately 2 weeks, with then slow progression to activities as tolerated. Activities beyond those of daily living should be avoided that include exercise, weightlifting, and impact activities for the first 2 weeks. After 2 weeks, patients should advance these above activities slowly over the next 4 weeks with impact activities being the last to be incorporated. At 6 weeks postoperatively, symptoms should be improved and patients typically are able to return to their usual activities.
Discussion
Because of the rarity of pubic symphysis instability, cited to be less than 5% of groin injuries in athletes, literature is limited.1 This consists of mostly case reports and other studies that focus on the treatment of chronic osteitis pubis; however, many times these conditions can occur in concert. One study evaluated 7 rugby players with vertical pubic symphysis instability treated with open reduction, internal fixation with bone grafting, and compression plating. This was done after a minimum of 13 months of nonoperative treatments including nonsteroidal anti-inflammatories, activity modification, ultrasound therapy, and injections failed. Although a small cohort, all 7 rugby players were pain free at 64.4 months and returned to sport successfully. The authors illustrate that the addition of bone graft is essential as healing must occur in high-level athletes or fixation with compression plating may fail.
In the current surgical technique, no bone graft was placed, and the symphysis joint was not violated with the thought being that the tape suture with anchor fixation construct allows small amounts of motion and a less rigid construct, and therefore a more physiological symphysis. One also could entertain the notion of using biologics as adjuncts; however, these outcomes have not been reported. One must also be cognoscente not to destabilize the symphysis further that may lead to failure of the implant. Other advantages to this procedure include smaller wounds that decrease the risk of wound complications and hernias that are commonly seen with open symphysis treatments.
The disadvantages of the current technique include aberrant placement of anchors into the symphysis if fluoroscopy is not used, possible implant failure, and continued pain from the lack of tension and therefore continued instability. The difficulties with this technique are obtaining the appropriate angle for anchor placement and applying appropriate tension. Although no literature exists that evaluates outcomes of this technique, internal brace techniques has been used extensively and studied in the ankle. Furthermore, syndesmotic fixation, using suture and buttons, uses a similar technique with the idea of allowing more physiological motion than screw fixation, and has shown good results.
Other studies have evaluated many different surgical techniques for recalcitrant osteitis pubis. One study performed open curettage of the symphysis in 23 patients, and at 19.1 months pain was significantly improved and postoperative magnetic resonance imaging showed no residual osteitis pubis.4 Another study of 5 soccer players underwent arthroscopic curettage and adductor reattachment and also found good results.5 One study compared 8 patients treated with laparoscopic retropubic mesh and 8 patients treated nonoperatively; the study found that 7 of 8 (88%) returned to sport in the operative group and had lower pain scores and concluded that mesh was a viable surgical option.6
Multiple surgical techniques exist with small sample sizes reported for the treatment of osteitis pubis, but there are limited studies evaluating the surgical treatment of pubic symphysis instability. Although rare, the key to the treatment of pubic symphysis instability is appropriate diagnosis and exhaustive evaluation of other groin pain generators with postpartum women and athletes such as heavy weightlifters and rugby players commonly being affected. This internal suture brace technique allows for small amounts of continued motion, closer to normal physiology, when compared with the commonly performed open plating that can lead to implant failure from the rigidity of the implant. If pubic symphysis instability is recalcitrant to exhaustive nonoperative treatments, the current surgical technique is minimally invasive, possibly more physiological and something that one should consider in conjunction with a general surgery colleague.
Footnotes
The authors report that they have no conflicts of interest in the authorship and publication of this article. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The patient is placed in the supine position, a Foley catheter placed, an infraumbilical incision made, and under direct visualization, 2 additional standard laparoscopic portals are placed. The space of Retzius is opened and the bony boarders of the symphysis are exposed. Then the first tape-loaded anchor is placed 10 mm from the symphysis through a percutaneous portal, and a second tape-loaded anchor placed ipsilateral and anteriorly. On the contralateral side, a tape limb from each of the right anchors is loaded onto an anchor that is placed with appropriate tension through another percutaneous portal and then the remaining 2 tapes are loaded onto the fourth anchor which is placed on this same side of the symphysis, creating a crisscross pattern.
References
- 1.Williams P.R., Thomas D.P., Downes E.M. Osteitis pubis and instability of the pubic symphysis. When nonoperative measures fail. Am J Sports Med. 2000;28:350–355. doi: 10.1177/03635465000280031101. [DOI] [PubMed] [Google Scholar]
- 2.Holt M.A., Keene J.S., Graf B.K., Helwig D.C. Treatment of osteitis pubis in athletes. Results of corticosteroid injections. Am J Sports Med. 1995;23:601–606. doi: 10.1177/036354659502300515. [DOI] [PubMed] [Google Scholar]
- 3.Hopp S., Culemann U., Ojodu I., Pohlemann T., Kelm J. Arthroscopic debridement of the pubic symphysis: An experimental study. Knee Surg Sports Traumatol Arthrosc. 2015;23:2568–2575. doi: 10.1007/s00167-014-3105-3. [DOI] [PubMed] [Google Scholar]
- 4.Radic R., Annear P. Use of pubic symphysis curettage for treatment-resistant osteitis pubis in athletes. Am J Sports Med. 2008;36:122–128. doi: 10.1177/0363546507306160. [DOI] [PubMed] [Google Scholar]
- 5.Hopp S.J., Culemann U., Kelm J., Pohlemann T., Pizanis A. Osteitis pubis and adductor tendinopathy in athletes: A novel arthroscopic pubic symphysis curettage and adductor reattachment. Arch Orthop Trauma Surg. 2013;133:1003–1009. doi: 10.1007/s00402-013-1777-7. [DOI] [PubMed] [Google Scholar]
- 6.Paajanen H., Hermunen H., Karonen J. Pubic magnetic resonance imaging findings in surgically and conservatively treated athletes with osteitis pubis compared to asymptomatic athletes during heavy training. Am J Sports Med. 2008;36:117–121. doi: 10.1177/0363546507305454. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The patient is placed in the supine position, a Foley catheter placed, an infraumbilical incision made, and under direct visualization, 2 additional standard laparoscopic portals are placed. The space of Retzius is opened and the bony boarders of the symphysis are exposed. Then the first tape-loaded anchor is placed 10 mm from the symphysis through a percutaneous portal, and a second tape-loaded anchor placed ipsilateral and anteriorly. On the contralateral side, a tape limb from each of the right anchors is loaded onto an anchor that is placed with appropriate tension through another percutaneous portal and then the remaining 2 tapes are loaded onto the fourth anchor which is placed on this same side of the symphysis, creating a crisscross pattern.