Abstract
The purpose of this investigation was to utilize several different technologies to compare body composition results across two phases of the menstrual cycle, and to investigate whether being on hormonal birth control or not has any effect on results. The secondary purpose was to determine if body satisfaction or perception of fluid retention differed across phases or between groups. A total of 39 females with a mean age of 26 ± 7 yrs were included in the study, 15 were on hormonal birth control (BC) and 24 were not (non-BC). Participants came into the lab for two trials: once while menstruating and another during the estimated pre-ovulation phase of the menstrual cycle. Demographic and body satisfaction questionnaires were completed prior to body composition testing. This testing included dual-energy x-ray absorptiometry, BOD POD®, and three separate bioelectrical impedance analyses. Participants completed the body satisfaction questionnaire and all body composition tests on each trial. No significant differences (P > 0.05) were found between body fat percentage or total body water estimates taken during menses and pre-ovulation for the BC or non-BC group. There was no significant difference (P > 0.05) in overall body satisfaction across the two phases for the non-BC group, though the BC group had significantly lower body satisfaction during menses (P < 0.01). Participants in both groups identified feeling more bloated during menses (P < 0.001). Results suggest that menses should not affect the reliability of body composition estimates regardless of whether or not females are on hormonal BC.
Keywords: Total body water, birth control, body satisfaction, body fat percent
INTRODUCTION
It has been established that women experience fluctuations in body mass throughout their menstrual cycle (29, 32). These fluctuations have been attributed to shifts in fluid retention, referred to as bloating, at certain phases of the menstrual cycle (32). These shifts in fluid retention have been partially attributed to hormonal changes that women experience throughout each phase of the cycle (6), though this relationship is not fully understood. The variation of body mass and fluid adjustments throughout the cycle have been well documented, however it is still unclear as to the effect this would have on overall body composition estimates.
Body mass alone does not give a total encompassing view of the health status of an individual. In order to better identify whether or not an individual is in a healthy state, it is ideal for body composition to be established. Body composition can be estimated in a multitude of ways, and can give us an estimation of several variables including body fat percentage (BF%), lean mass, fat mass, bone mineral content, and total body water (TBW), depending on which method is used. The different methods all vary in terms of cost as well as the amount of experience needed from the tester to perform the assessment correctly. BF% results can be practically applied across many different subgroups of people. In the general population, BF% is a useful estimate in tracking progress in a fitness or weight loss regimen. Additionally, it can also be used in athletic populations to track the advancements in performance as they train for their particular sport. BF% is also used to identify if an individual is at a risk of developing cardiovascular or metabolic disease.
These uses of body composition estimates are the reason that having the most accurate estimation of BF% is important. There are certain testing protocols that the manufacturers of body composition equipment set forth in order to ensure the most valid and reliable results. In order to get the most accurate estimates across methodologies, participants are generally asked to test when fasted and adequately hydrated. Additionally, participants are asked to refrain from exercise prior to testing to ensure that there is not an elevated body temperature or dehydration from sweat loss. Due to possible fluid retention, weight gain, and hormonal fluctuations that are happening throughout the menstrual cycle, it has been questioned as to whether or not menses could negatively impact the consistency of these assessments. It remains uncertain whether or not women should be tested while on their menstrual cycle.
The menstrual cycle can be depicted in three separate phases over an estimated 28 day period: the menstrual (days 1–5), proliferative (days 6–14), and secretory (days 15–28) phase (20). Each phase represents changes in the endometrial lining of the uterus in response to a fluctuation in ovarian hormones. These menstrual cycle phases are in concurrence with the phases of the ovarian cycle, which encompasses follicular maturation and hormonal fluctuations that occur with the stages of follicle development within the ovary. The ovarian cycle can be explained in three phases: the follicular phase (follicular maturation), ovulation (the release of the ovum from the mature follicle) and the luteal phase (corpus luteum develops from the ruptured follicle). The follicular phase coincides with the menstrual and proliferative phases (days 1–14), with ovulation occurring mid-cycle (estimated day 14) and the luteal phase coinciding with the secretory phase of the menstrual cycle (20).
Some research has been done to document body composition throughout different stages of the menstrual cycle, however these investigations are limited to single frequency bioelectrical impedance analysis (BIA) (6, 8, 10, 22, 26, 29). This methodology was likely chosen due to its reliance on TBW to in turn estimate BF%. In 2010, Daniusevičiūtė and colleagues (6) researched whether changes in estrogen levels would impact body mass and fluid retention levels between day two of the menstrual cycle (aligning with the follicular phase) and day 14 of the cycle (estimated ovulation) using the Tanita 300-A analyzer. Though estrogen levels were significantly higher at ovulation as compared to menstruation, there was not a significant change in BF% or TBW between the two phases, suggesting that differing levels of estrogen may not have an effect on fluid retention changes as originally hypothesized. These results are similar to the findings of Stachenfeld, who reported that changes in estrogen levels only mildly affected total body water estimates in healthy young women (26).
Some earlier studies testing body composition reliability throughout the menstrual cycle utilized BIA assessments via electrode placement on specific portions of the upper and lower limbs of the participant. In 2002, Gualdi-Russo and Toselli (10) assessed the influence of various factors, including the menstrual cycle, on BIA. Body composition was estimated between days 9 and 17 of their cycle (pre-ovulatory or secretory phase) and between days 5 and 8 of their cycle (end of menstruation or proliferative phase) (10). No significant differences in BF% were reported during the two different points of the cycle (10). In 1989, Gleichauf and Roe (8) researched reliability of BIA measurements throughout the menstrual cycle. BF% saw no significant changes, suggesting that BIA assessment appeared reliable throughout the menstrual cycle of a healthy female (8).
Though it is clear that fluid retention shifts throughout the cycle, it is unclear as to whether or not this would yield significant differences in TBW estimates as women progress through menstrual phases. In 2006, Tomazo-Ravnik and Jakopic (29) used the Tanita TBF-215 analyzer to estimate body composition during three separate phases of the menstrual/ovarian cycle: menstruation, late follicular phase, and middle luteal phase. TBW was only significantly different between the late follicular phase and middle luteal phase. Though TBW saw some fluctuations throughout the cycle, there were not significant differences found in BF% throughout any phases of the cycle (29). TBW also saw significant fluctuations in a study conducted by Mitchel et al. (22) where total body water was significantly higher in the late luteal phase in comparison to ovulation and the early luteal phase.
It remains unclear as to whether or not physiological changes occurring throughout a single menstrual cycle could alter the BF% estimates given by different methods. It has been predicted that that these body mass and fluid retention shifts could be associated with changing levels of body satisfaction (5, 27). Previous research has noted levels of higher appearance anxiety and negative body image thoughts were associated with higher levels of fluid retention throughout the menstrual cycle (5). Based on these results, it is hypothesized that increased levels of fluid retention, or bloating, could potentially cause women to feel anxiety that BF% estimates could be higher throughout menses. With this in mind, women with increased feelings of bloating may potentially not want to test on their cycle for fear of inaccurate results. Though past research has suggested that body composition does not seem to be significantly affected by the menstrual cycle, each study identified has only used BIA technology with a single frequency of either 50 kHz (6, 8, 29) or 100 kHz (10). BIA technology has evolved tremendously, with the ability to utilize multiple frequencies of up to 1000 kHz for body composition analyses. Research is needed to indicate whether these multi-frequency bioelectric impedance analyzers are more sensitive to changes occurring throughout the menstrual cycle. With these newer technologies, is possible that these higher levels of fluid retention, and therefore body dissatisfaction, during menses could be associated with changes in body composition estimates.
Finally, no research was found using air displacement plethysmography (ADP) or dual-energy x-ray absorptiometry (DXA) to assess body composition changes throughout the menstrual cycle. ADP utilizes body volume to estimate BF% and fat-free mass. With this in mind, fluid retention and weight gain could have a significant effect on body volume and thus BF% estimates. Additional research is needed using DXA technology. Past research has documented the sensitivity that DXA has with factors such as gastrointestinal tract contents and changes in tissue hydration, both of which can cause variation in DXA results (14, 23, 28, 31). With this in mind, it is possible that the DXA’s x-ray technology could be more sensitive to changes in fluid retention that may occur throughout the cycle, which could potentially alter body composition results. Furthermore, of the research that is available, there are not results to indicate if there are differences in women who are using hormonal birth control compared to those who are not and whether or not body satisfaction and perceptions of fluid retention differ between these groups. Therefore, the purpose of this investigation was to utilize several different technologies to compare body composition assessments across two phases of the menstrual cycle, including BIA, DXA, and ADP, and to investigate if being on hormonal birth control or not would yield different results. The secondary purpose was to determine if body satisfaction or perception of fluid retention differed across phases or between groups.
METHODS
Participants
Thirty-nine females were recruited via word-of-mouth in the community and social media to a southeastern university and gave written informed consent prior to participating. In order to qualify, participants needed to be pre-menopausal and between the ages of 18–54 years. Participants could be on birth control, so long as the method did not hinder them from menstruating each month. Individuals could not participate if they were missing any limbs or had a pacemaker implant. Copies of the results from body composition estimates were given as incentive to participate. All participants indicated that they had a “regular” period, identified as having a period each month.
Protocol
Prior to the start of testing, the study design was approved by the University’s Institutional Review Board. All testing was done within the University’s exercise physiology laboratory. Participants completed body composition testing in two separate trials. Trial one was on day one or two of their menstrual cycle, referred to as the menstrual phase. Trial two was seven to 14 days after their initial visit. This second trial was estimated to be in the proliferative (pre-ovulatory phase) of the menstrual cycle (20) and thus was referred to as the pre-ovulatory phase. It should be noted that in this study, women on hormonal birth control (BC) were welcome to participate. Though being on hormonal birth control stops the woman from ovulating, we still referred to the BC group’s trial two as the “pre-ovulatory phase” as we did for the non-BC group, which consisted of women not on hormonal birth control.
Testing procedures were the same for both trials
Before arriving to the laboratory, participants were given the same pre-participation instructions in order to standardize conditions during testing. Prior to testing participants were asked to abstain from eating or drinking, with the exception of water, for four hours, exercise 12 hours, and alcohol consumption for 24 hours. They were also asked to wear comfortable and light athletic attire free of metal. For the BOD POD® assessment, they were required to wear a swim cap, lycra compression shorts, and a sports bra. Upon consent, participants completed two questionnaires: a demographic questionnaire and a body satisfaction and bloatedness questionnaire. The demographic questionnaire inquired about duration of menstrual cycle and birth control information. The body satisfaction questionnaire, which was completed at both trials, had participants identify current levels of satisfaction with overall body appearance as well as individual parts of the body using a 0–100% satisfaction scale. Additionally, participants were asked how bloated they felt on a four point Likert scale (1 = none at all, 2 = slightly, 3 = moderate, 4 = extremely). Participants were informed to fill out the body satisfaction questionnaire based on how they felt in that moment. Before body composition assessments began, they were asked to void their bladder, then remove shoes, metal, and jewelry. Height and body mass were taken per the Tanita WB-3000 digital physician’s scale. After each method was complete, participants were given copies of their results along with an explanation of the values. All testing procedures were repeated during the second trial.
Bioelectrical Impedance Analysis (BIA)
Bioelectrical impedance analysis was conducted using three different models: Tanita BC-418 (TANITA Corporation of America, Inc., Arlington Heights, IL), InBody 230 (Biospace, Inc., Los Angeles, CA), and InBody 720 (Biospace, Inc., Los Angeles, CA). BIA works by sending small electrical currents throughout the body in order to detect the impedance, or resistance, to the electrical signal (frequency). All three devices estimate body composition by utilizing manufacturer-specific patented equations, which take into consideration variables such as age, height, weight, gender, and impedance. The physiological framework behind this methodology is that muscle is composed of a much larger quantity of water than fat is (3). Using this basis, it is possible that a higher percentage of fat-free mass could be estimated if an individual had a higher percentage of total body water. The Tanita BC-418 utilizes only one frequency, 50 kHz, for analysis (18). The InBody 230 is a portable analyzer which utilizes two different frequencies, 20 and 100 kHz (16). Impedance measures are performed through both arms, legs, and the trunk of the body using these two frequencies. Both of these devices estimate multiple variables including BF% and TBW. The InBody 720 utilizes six different frequencies (1, 5, 50, 250, 500, and 1000 kHz) to produce impedance values (18). Both the InBody 230 and 720 models run multiple impedance measurements based on frequency and body segment. In addition to estimating the same body composition variables as the previous two models, the InBody 720 also estimates intracellular water (ICW), fluid located inside of the cells, and extracellular water (ECW), or water located outside of the cells.
Each piece of equipment was properly maintained per manufacturer specifications
All three models utilized both hand and foot electrodes, which were used to send the current through the body of the participant for analysis. Age, sex, and height were manually entered into each device prior to assessment. Before stepping onto both the InBody 230 and 720, an antibacterial InBody tissue cloth was used to cleanse the palms of hands and bottoms of the feet. The hand and foot electrodes of the Tanita BC-418 were cleaned thoroughly with an antibacterial wipe prior to testing. Participants stood barefoot on each device, lining heels up with the posterior electrodes and their forefoot up with the anterior electrodes. After identifying correct feet placement, body mass was taken via the scale in each BIA. After body mass was measured, participants were instructed to grab the handles, which contained electrodes that would come into contact with each hand, and hold the handles at their sides away from the torso and to remain still for the duration of each assessment.
Dual-energy X-ray Absorptiometry (DXA)
A total body dual-energy x-ray absorptiometry (DXA) scan was completed using the GE Lunar iDXA (GE Healthcare, Madison, WI). DXA utilizes two x-ray beams with different energy levels to estimate body composition. Participants layed in the supine position on the padded scanning table. During the assessment, individuals were instructed to lay still and refrain from talking. This scan took seven to 14 minutes depending on the height and body mass of the participant. After the scan was complete, a trained researcher adjusted regions of interest per manufacturer specifications.
Air Displacement Plethysmography (ADP)
Air displacement plethysmography (ADP) was performed by using the BOD POD® (COSMED USA, Concord, CA). The BOD POD® was calibrated each day per manufacturer specifications. This methodology uses air displacement to provide estimates for body volume, which in turn is used to estimate BF% and fat-free mass. After performing the pre-test calibration as instructed by the manufacturer, participants were asked to enter the BOD POD®. This assessment requires two to three trials, each trial lasting approximately 50 seconds. During each trial, participants were asked to remain still, refrain from talking, and breathe normally.
Statistical Analysis
All statistical analyses were completed using SPSS for Microsoft Windows (version 24.0; IBM Corp., Armonk, NY). Descriptive statistics were calculated for age, height, body mass, duration of cycle, and number of days between trials. A one-way analysis of variance (ANOVA) was performed on the items of the body satisfaction questionnaire in addition to each body composition variable to assess the differences between the BC and non-BC groups. A repeated measures ANOVA was used to compare the BC and non-BC groups by trial. A paired-samples t-test was performed to identify changes body composition variables between trials for each group. A paired-samples t-test was performed for each question of the body satisfaction questionnaire to assess differences in satisfaction scores between trials for each group. Finally, Chi-Square analysis was used to determine any relationship between categorical variables of birth control use and bloatedness. All analyses were set at an alpha level of 0.05.
RESULTS
A total of 39 women (mean age = 26 ± 7 yrs) participated in the study. Of these women, 15 were on hormonal birth control (BC) and 24 were not (non-BC). Descriptive information is found in table 1.
Table 1.
Participant characteristics (Mean ± SD).
| BC (n=15) | Non-BC (n=24) | df | F value | p-value | |
|---|---|---|---|---|---|
| Age (years) | 25 ± 5 | 27 ± 8 | 38 | 1.339 | 0.255 |
| Body Mass visit one (kg) | 61.7 ± 9.7 | 68.6 ± 15.3 | 38 | 2.476 | 0.124 |
| Body Mass visit two (kg) | 61.6 ± 9.7 | 65.9 ± 9.4 | 38 | 1.881 | 0.178 |
| BMI (kg/m2) | 23.5 ± 3.8 | 25.7 ± 7.6 | 38 | 1.073 | 0.307 |
| Duration of Cycle (days) | 4.3 ± 1.0 | 5.4 ± 1.1 | 38 | 9.311 | 0.004* |
| Heaviness of Flow (1–4 Likert scale) | 0.6 ± 0.8 | 1.3 ± 0.6 | 38 | 9.701 | 0.004* |
| Days Between Trials | 9.7 ± 2.4 | 11.1 ± 3.1 | 38 | 2.422 | 0.128 |
Indicates significantly different (P < 0.05)
Body Composition - Body Fat Percentage
Repeated measures ANOVA revealed that there was no significant difference in BF% between trials for any of the methodologies used (P > 0.05), and there was no trial by group interaction across any of the methodologies (P > 0.05). Paired samples t-test found no differences in BF% between trials for either the BC (table 2) or non-BC group (table 3).
Table 2.
Body fat percentage across trials (Mean ± SE). Hormonal BC (n=15)
| Trial One | Trial Two | Mean Difference ± SD | ICC | Effect Size | p-value | |
|---|---|---|---|---|---|---|
| DXA (BF%) | 30.7 ± 1.5 | 30.8 ± 1.5 | −0.1 ± 0.7 | 1.00 | −0.01 | 0.706 |
| ADP (BF%) | 30.0 ± 1.8 | 29.2 ± 1.8 | 0.7 ± 1.3 | 0.99 | 0.05 | 0.064 |
| Tanita (BF%) | 26.6 ± 2.1 | 26.9 ± 2.0 | −0.3 ± 1.1 | 0.99 | −0.02 | 0.325 |
| InBody 720 (BF%) | 26.7 ± 1.9 | 26.7 ± 1.8 | 0.0 ± 1.7 | 0.99 | 0.00 | 0.964 |
| InBody 230 (BF%) | 27.4 ± 1.9 | 27.4 ± 1.7 | 0.0 ± 1.6 | 0.99 | 0.00 | 0.975 |
No measurements were significantly different from menstruation (P > 0.05)
Table 3.
Body fat percentage across trials (Mean ± SE). Non-BC (n=24)
| Trial One | Trial Two | Mean Difference ± SD | ICC | Effect Size | p-value | |
|---|---|---|---|---|---|---|
| DXA (BF%) | 30.6 ± 1.3 | 30.3 ± 1.4 | 0.2 ± 0.7 | 1.00 | 0.02 | 0.077 |
| ADP (BF%) | 28.8 ± 1.6 | 28.3 ± 1.6 | 0.5 ± 1.4 | 0.99 | 0.03 | 0.083 |
| Tanita (BF%) | 26.7 ± 1.5 | 27.1 ± 1.5 | −0.4 ± 1.1 | 0.99 | −0.03 | 0.122 |
| InBody 720 (BF%) | 26.1 ± 1.5 | 26.3 ± 1.5 | −0.3 ± 1.9 | 0.98 | −0.02 | 0.498 |
| InBody 230 (BF%) | 27.0 ± 1.4 | 26.8 ± 1.5 | 0.2 ± 1.4 | 0.99 | 0.02 | 0.523 |
No measurements were significantly different from menstruation (P > 0.05)
Total Body Water, Intracellular Water, and Extracellular Water
Repeated measures ANOVA revealed that there was no significant difference in TBW or ICW between trials (P > 0.05). There was a significant difference in ECW between trials (P = 0.022). There was no trial by group interaction for TBW, ICW, or ECW (P > 0.05). Paired samples t-test revealed no differences for the BC group between trials (table 4). There were no significant differences for the non-BC group between trials, with the exception of ECW (table 5).
Table 4.
Comparison of TBW, ICW, and ECW across trials (Mean ± SE). Hormonal BC (n=15)
| Trial One | Trial Two | Mean Difference ± SD | ICC | Effect Size | p-value | |
|---|---|---|---|---|---|---|
| Tanita TBW (kg) | 32.7 ± 0.9 | 32.6 ± 0.9 | 0.2 ± 0.8 | 0.99 | 0.02 | 0.492 |
| InBody 720 TBW (kg) | 32.8 ± 0.9 | 32.8 ± 0.9 | −0.0 ± 0.7 | 0.99 | −0.01 | 0.823 |
| InBody 720 ICW (kg) | 20.4 ± 0.6 | 20.5 ± 0.6 | −0.5 ± 0.4 | 0.99 | −0.01 | 0.694 |
| InBody 720 ECW (kg) | 12.4 ± 0.3 | 12.3 ± 0.3 | 0.1 ± 0.8 | 0.98 | 0.03 | 0.465 |
| InBody 230 TBW (kg) | 32.5 ± 0.9 | 32.5 ± 0.9 | 0.0 ± 0.8 | 0.99 | 0.00 | 0.891 |
No measurements were significantly different from menstruation (P > 0.05)
Table 5.
Comparison of TBW, ICW, and ECW across trials (Mean ± SE). Non-BC (n=24)
| Trial One | Trial Two | Mean Difference ± SD | ICC | Effect Size | p-value | |
|---|---|---|---|---|---|---|
| Tanita TBW (kg) | 35.1 ± 0.6 | 34.6 ± 0.6 | 0.5 ± 1.1 | 0.96 | 0.77 | 0.055 |
| InBody 720 TBW (kg) | 35.2 ± 0.7 | 35.0 ± 0.7 | 0.2 ± 0.9 | 0.98 | 0.03 | 0.212 |
| InBody 720 ICW (kg) | 22.0 ± 0.5 | 21.9 ± 0.4 | 0.1 ± 0.6 | 0.98 | 0.02 | 0.395 |
| InBody720 ECW (kg) | 13.3 ± 0.3 | 13.1 ± 0.3 | 0.2 ± 0.3 | 0.98 | 0.08 | 0.008* |
| InBody 230 TBW (kg) | 34.9 ± 0.7 | 34.8 ± 0.7 | 0.0 ± 0.9 | 0.98 | 0.01 | 0.806 |
Indicates significantly different from menstruation (P < 0.01)
Body Satisfaction
When participants were asked “what is your current level of satisfaction with the overall appearance of your body?” there was a significant difference when comparing responses between menstruation and the pre-ovulatory phase for BC females (menstruation = 63.3 ± 14.0%, pre-ovulatory = 70.7 ± 10.3%, P = 0.006). In contrast, non-BC females did not have significant differences in overall body satisfaction between the two phases (menstruation = 68.8 ± 13.3%, pre-ovulatory = 65.8 ± 19.3%, P = 0.284).
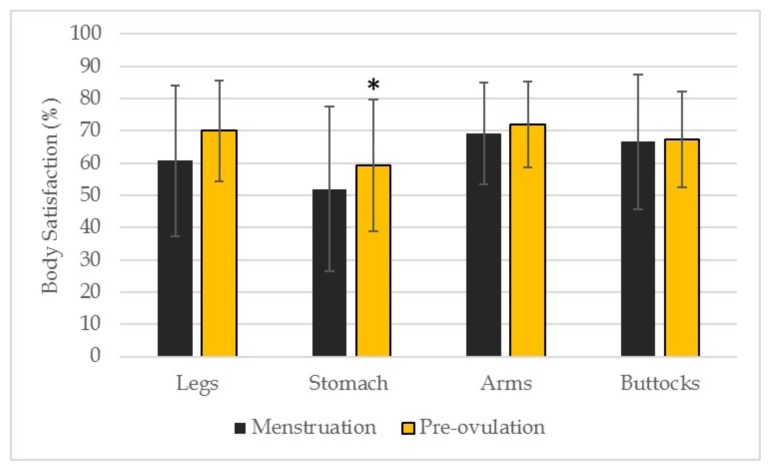
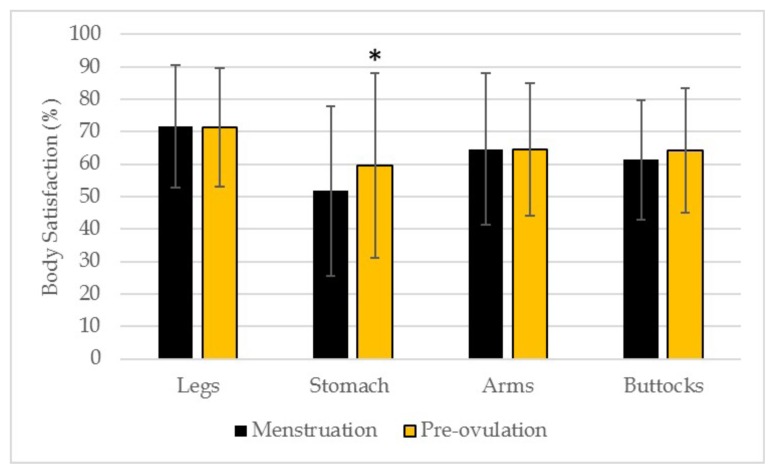
In regards to specific parts of the body, there were no significant differences between the two phases for either BC or non-BC females when they were asked about satisfaction of their legs, arms and buttocks as shown in figure 1 and figure 2. Both BC and non-BC females showed significant differences between phases when asked about satisfaction of their stomach/abdominal region. A one-way ANOVA revealed no significant differences between the BC and non-BC groups on any questions of the body satisfaction questionnaire (P > 0.05).
Figure 1.
Body satisfaction of different body parts across trials in the BC group (n = 15). * Statistically significant difference (P < 0.05) than menstruation.
Figure 2.
Body satisfaction of different body parts across trials in the non-BC group (n = 24). * Statistically significant difference (P < 0.05) than menstruation.
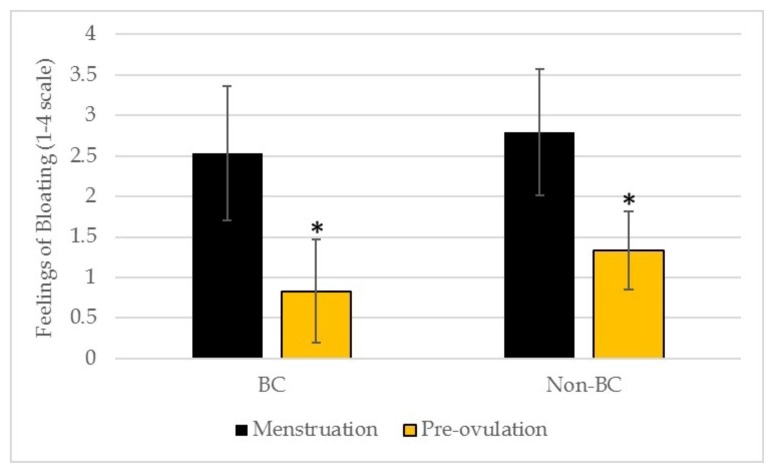
Individuals were asked to rank their feelings of fluid retention, or “bloating”, on a 1 to 4 scale (1 = none at all, 2 = slightly, 3 = moderate, 4 = extremely). When assessing the responses between trial one and trial two, perception of bloating was significantly different between the two phases for both BC and non-BC females (figure 3). Chi-square analyses revealed that feelings of bloatedness were not different for either group at both trials (P = 0.774 and P = 0.435, respectively).
Figure 3.
Perception of bloating across trials for the BC (n = 15) and non-BC (n = 24) groups. * Statistically significant difference (P < 0.001) than menstruation.
DISCUSSION
The purpose of this research was to utilize several different technologies to compare body composition assessments across two phases of the menstrual cycle, including BIA, DXA, and ADP, and to investigate the effects of birth control on the reliability of body composition results. The secondary purpose was to determine if body satisfaction or perception of fluid retention differed across phases or between groups. Overall, results indicate that the menstrual cycle may not affect body composition results across multiple methods. Though there was a significant difference in ECW for the non-BC group across the two phases, this difference was not enough to significantly alter BF% or TBW results.
White and colleagues (32) identified that there was a significant fluctuation in fluid retention throughout the menstrual cycle, where fluid retention peaked on day one of menstrual flow and then reached its lowest point immediately post-menstrual cycle. Fluid retention then saw a gradual rise from five days prior to ovulation up until the next onset of flow. One idea is that the bloated feelings that are associated with menses could be a result of fluid retention shifts and hormonal changes throughout the cycle (6, 32). With this in mind, it was hypothesized that TBW would be significantly higher during menses than in the pre-ovulatory phase. Of studies that have been done to assess body composition throughout the menstrual cycle, changes in TBW have had conflicting results. Some studies have identified no fluctuation in TBW (6) while others have seen fluctuations through certain points of the cycle (22, 29). However, much of this research was done using early BIA technology, which utilized only single frequency bioelectrical impedance analyzers. The inconsistencies in results among these studies might be attributed to the use of this early technology. BIA has evolved in the last decade and these technological advancements support the need for updated research on body composition throughout the menstrual cycle using the latest BIA equipment.
In the past, research that assessed changes in body composition throughout the menstrual cycle has not included women utilizing hormonal BC. The current investigation found no significant differences in any of the TBW estimates between menses and pre-ovulation for either the BC or non-BC groups among the Tanita BC-418, InBody 720, or InBody 230. These results support that birth control may not alter the reliability of BIA results at different phases of the menstrual cycle. Due to the fact that females indicated that they felt significantly more bloated while menstruating than in the pre-ovulatory phase, it was thought that TBW would be significantly different between stages of the cycle on each BIA. These data suggest that the bloated feeling experienced during the menstrual cycle is not due to a significant increase in TBW as estimated by the Tanita BC-418, InBody 720, or InBody 230.
When analyzing BF% differences during menses and the pre-ovulatory phase, no significant differences were seen in DXA, BIA, or BOD POD® for either group. These results are similar to previous research using only BIA, which cited no differences in BF% in different phases of the cycle (6, 10, 29). Though BF% and TBW remained consistent throughout the cycle for all methodologies, ECW was significantly different between trials for the non-BC group. Specifically, ECW was higher during menstruation. Perhaps this can be explained by the heavier menstrual flow for non-BC participants compared to the BC group.
When assessing the BC group, no significant differences were seen in BF% between menstruation and pre-ovulatory phase using any of the three methodologies. Overall, these data suggest that females on birth control can complete body composition testing using BIA, or other methods, on their menstrual cycle without affecting the reliability of results.
When assessing the non-BC group, there were no significant differences in BF% between menstruation and pre-ovulation for any of the three methodologies. Therefore, results suggest that the reliability of body composition assessments should not be affected by whether or not a woman is on birth control.
Body composition results can be used in a variety of populations. In the general population, BF% estimates are utilized to assess health risk and prescribe an appropriate exercise regimen. The reliability of these results is especially important when tracking an individual’s progress over time. In order to make results as accurate as possible, manufacturers of body composition equipment have set forth guidelines as to what participants should eat, drink, wear, and exercise limitations prior to assessment. This research was important to provide guidance on when women should assess their BF% throughout their menstrual cycle in order to see the most accurate results. Results from the current investigation suggest that BF% should not be affected by whether or not a woman is menstruating at the time of testing if they are being assessed with iDXA, BOD POD®, Tanita BC-418, InBody 720 or InBody 230.
The current investigation also assessed satisfaction of overall appearance, as well as for individual parts of the body (e.g. legs, buttocks, arms, and stomach/abdominal region). Though overall body satisfaction did not change due to menstruation for the non-BC group, significant differences were seen between the two menstrual phases for the BC group. Past research has noted higher levels of appearance anxiety and negative body image associated with higher levels of fluid retention, or bloating (5). The fact that body satisfaction did not fluctuate in the non-BC group was unexpected, as women did report feeling significantly more bloated during menses in both the BC and non-BC groups. Teixeira et al. (27) reported that body dissatisfaction was highest during menses and then significantly declined post-menstruation, though it should be noted that a different scale was used between the studies. This decline in body dissatisfaction was then maintained until flow began again (27). Therefore, further research may need to be done to better identify what could potentially cause fluctuations of body satisfaction throughout the menstrual cycle for different groups of women.
No significant changes in individual body part satisfaction between the menstrual and pre-ovulatory phase of the cycle were discovered with exception to the stomach/abdominal region. These results are in line with the original hypothesis that bloating or fluid retention during menstruation would cause satisfaction in the stomach/abdominal region to decrease. Bloating was consistent with women’s satisfaction with their stomach/abdominal region, with high dissatisfaction during menstruation.
Some strengths of this study design were that body composition was assessed using five different pieces of valid and reliable body composition equipment (1–3, 9, 11, 13, 15–19, 24, 30, 33). Much of the research on body composition throughout the menstrual cycle was done utilizing earlier BIA technologies. This can be limiting, as technology has changed, and thus so has the abilities of body composition equipment. The methodologies used in the current study range in cost and availability to the general public. That being said, using this wide range of methodologies supports the idea that body composition estimates are not adversely affected by menstruation in a variety of settings (e.g. research lab, hospital, doctor’s office, fitness settings, etc.)
Additionally, this is the first study that researchers were able to find that analyzed the body composition results between the menstrual cycle phases for women on hormonal birth control. The BC group’s body composition results remained stable throughout menses and pre-ovulation using all three methodologies. Therefore, this study has provided new data to support that women on birth control may have consistent body composition estimates throughout the menstrual cycle phases.
Though the study had several strengths, there were some limitations. The investigation only tested women during two phases of the menstrual cycle, the menstrual phase and estimated pre-ovulation phase. Further research is warranted to see if the consistency of body composition results remains throughout the later phases, identified as the luteal or secretory phase (20), leading up to menstruation. However, body fat percentage may actually change due to caloric balance shifts caused by a regular fitness routine and/or caloric intake adjustments over the course of the month. Therefore, caution should be taken with this type of study design. It should also be noted that a majority of the sample was young, and that perhaps results would differ with a primarily older sample, specifically those experiencing pre-menopause. Though pre-menopausal women continue to ovulate, their period is known to become less regular as they approach menopause and see shifts in reproductive hormone levels such as estradiol, progesterone, LH, and FSH (4, 7, 12, 21, 25). As previously stated, all females in this investigation indicated that they experience regular cycles. Perhaps the irregularity of menses in pre-menopausal women and hormonal shifts could yield different results in body composition throughout the menstrual cycle and further investigation is warranted. Finally, although women were encouraged to consume water as they normally would and voided their bladders prior to testing, hydration status was not assessed.
Overall, the results of this study suggest that the body composition results should not be affected by the menstrual cycle. When tracking BF%, these findings propose that females do not need to be tested at the same point in their menstrual cycle each month in order to get accurate BF% or TBW estimates when using the DXA, BOD POD®, Tanita BC-418, InBody 230, and InBody 720. It additionally supports that reliability is not affected by whether or not a woman is on birth control. Furthermore, though it was originally hypothesized that body satisfaction could fluctuate throughout the menstrual cycle, females displayed consistent overall body satisfaction throughout the menstrual and estimated pre-ovulatory phase for the non-BC group. Body satisfaction was significantly lower during menses for the BC group, however. Additionally, differences in satisfaction were discovered in the stomach/abdominal region between the two phases of the menstrual cycle, with higher levels of dissatisfaction during menstruation. These data were also associated with increased feelings of bloatedness. Therefore, though females may feel that they are more bloated and heavier throughout their menstrual cycle, those feelings are not accompanied by shifts in body composition results.
REFERENCES
- 1.American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription. Ninth ed. Lippincott Williams & Wilkins; 2013. [DOI] [PubMed] [Google Scholar]
- 2.Anderson DE. Reliability of air displacement plethysmography. J Strength Cond Res. 2007;21(1):169–172. doi: 10.1519/00124278-200702000-00030. [DOI] [PubMed] [Google Scholar]
- 3.Anderson LJ, Erceg DN, Schroeder ET. Utility of multifrequency bioelectrical impedance compared with dual-energy x-ray absorptiometry for assessment of total and regional body composition varies between men and women. Nutr Res. 2012;32(7):479–485. doi: 10.1016/j.nutres.2012.05.009. [DOI] [PubMed] [Google Scholar]
- 4.Buckler H. The menopause transition: endocrine changes and clinical symptoms. J Br Menopause Soc. 2005;11(2):61–65. doi: 10.1258/136218005775544525. [DOI] [PubMed] [Google Scholar]
- 5.Carr-Nangle RE, Johnson WG, Bergeron KC, Nangle DW. Body Image Changes over the Menstrual Cycle in Normal Women. Int J Eat Disord. 1994;16(3):267–273. doi: 10.1002/1098-108x(199411)16:3<267::aid-eat2260160307>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 6.Daniusevičiūtė L, Brazaitis M, Skurvydas A, Sipavičienė S, Linonis V, Piečaitienė J, Eimantas N. Changes in concentration of creatine kinase, body composition and lipoprotein during menstrual cycle. Ugdymas Kuno Kultura. 2010;77(2):11–17. [Google Scholar]
- 7.Fitzgerald C, Zimon A, Jones E. Aging and Reproductive Potential in Women. Yale J Biol Med. 1998;1999;71:367–381. [PMC free article] [PubMed] [Google Scholar]
- 8.Gleichauf CN, Roe DA. The menstrual cycle’s effect on the reliability of bioimpedance measurements for assessing body composition. Am J Clin Nutr. 1989;50(5):903–907. doi: 10.1093/ajcn/50.5.903. [DOI] [PubMed] [Google Scholar]
- 9.Going SB, Massett MP, Hall MC, Bare LA, Root PA, Williams DP, Lohman TG. Detection of small changes in body composition by dual-energy x-ray absorptiometry. Am J Clin Nutr. 1993;57(6):845–850. doi: 10.1093/ajcn/57.6.845. [DOI] [PubMed] [Google Scholar]
- 10.Gualdi-Russo E, Toselli S. Influence of various factors on the measurement of multifrequency bioimpedance. HOMO-J Comp Hum Biol. 2002;53(1):1–16. doi: 10.1078/0018-442x-00035. [DOI] [PubMed] [Google Scholar]
- 11.Haas V, Schütz T, Engeli S, Schröder C, Westerterp K, Boschmann M. Comparing single-frequency bioelectrical impedance analysis against deuterium dilution to assess total body water. Eur J Clin Nutr. 2012;66(9):994–997. doi: 10.1038/ejcn.2012.96. [DOI] [PubMed] [Google Scholar]
- 12.Hee J, MacNaughton J, Bangah M, Burger HG. Perimenopausal patterns of gonadotrophins, immunoreactive inhibin, oestradiol and progesterone. Maturitas. 1993;18:9–20. doi: 10.1016/0378-5122(93)90026-e. [DOI] [PubMed] [Google Scholar]
- 13.Hind K, Oldroyd B, Truscott J. In vivo precision of the GE Lunar iDXA densitometer for the measurement of total body composition and fat distribution in adults. Eur J Clin Nutr. 2011;65(1):140–142. doi: 10.1038/ejcn.2010.190. [DOI] [PubMed] [Google Scholar]
- 14.Horber FF, Thomi F, Casez JP, Fonteille J, Jaeger P. Impact of hydration status on body composition as measured by dual energy X-ray absorptiometry in normal volunteers and patients on haemodialysis. Br J Radiol. 1992;65(778):895–900. doi: 10.1259/0007-1285-65-778-895. [DOI] [PubMed] [Google Scholar]
- 15.Hurst PR, Walsh DC, Conlon CA, Ingram M, Kruger R, Stonehouse W. Validity and reliability of bioelectrical impedance analysis to estimate body fat percentage against air displacement plethysmography and dual-energy x-ray absorptiometry. Nutr Diet. 2015 [Google Scholar]
- 16.Karelis AD, Chamberland G, Aubertin-Leheudre M, Duval C. Validation of a portable bioelectrical impedance analyzer for the assessment of body composition. Appl Physiol Nutr Metab. 2013;38(1):27–32. doi: 10.1139/apnm-2012-0129. [DOI] [PubMed] [Google Scholar]
- 17.Kelly JS, Metcalfe J. Validity and reliability of body composition analysis using the tanita BC418-MA. J Exerc Physiol Online. 2012;15:74–83. [Google Scholar]
- 18.Kutáč P, Kopecký M. Comparison of body fat using various bioelectrical impedance analyzers in university students. Acta Gymnica. 2015;45(4):177–186. [Google Scholar]
- 19.Maddalozzo GF, Cardinal BJ, Snow CM. Concurrent validity of the BOD POD and dual energy x-ray absorptiometry techniques for assessing body composition in young women. J Am Diet Assoc. 2002;102(11):1677–1679. doi: 10.1016/s0002-8223(02)90358-5. [DOI] [PubMed] [Google Scholar]
- 20.Marieb EN, Hoehn Katja. Human Anatomy & Physiology. 7th ed. Pearson Benjamin Cummings; San Francisco: 2007. [Google Scholar]
- 21.Miro F, Parker SW, Aspinall LJ, Coley J, Perry PW, Ellis JE. Sequential classification of endocrine stages during reproductive aging in women: the FREEDOM study*. Menopause. 2005;12(3):281–290. doi: 10.1097/01.gme.0000147018.30796.25. [DOI] [PubMed] [Google Scholar]
- 22.Mitchell CO, Rose J, Familoni B, Winters S, Ling F. The use of multifrequency bioelectrical impedance analysis to estimate fluid volume changes as a function of the menstrual cycle. Basic Life Sci. 1993;60:189–191. doi: 10.1007/978-1-4899-1268-8_43. [DOI] [PubMed] [Google Scholar]
- 23.Nana A, Slater GJ, Stewart AD, Burke LM. Methodology Review: Using Dual-Energy X-Ray Absorptiometry (DXA) for the Assessment of Body Composition in Athletes and Active People. Int J Sport Nutr Exerc Metab. 2015;25(2):198. doi: 10.1123/ijsnem.2013-0228. [DOI] [PubMed] [Google Scholar]
- 24.Segal KR, Burastero S, Chun A, Coronel P, Pierson R, Wang J. Estimation of extracellular and total body water by multiple-frequency bioelectrical-impedance measurement. Am J Clin Nutr. 1991;54(1):26–29. doi: 10.1093/ajcn/54.1.26. [DOI] [PubMed] [Google Scholar]
- 25.Sherman BM, West JH, Korenman SG. The menopausal transition: analysis of LH, FSH, estradiol, and progesterone concentrations during menstrual cycles of older women. J Clin Endocrinol Metab. 1976;42(4):629–636. doi: 10.1210/jcem-42-4-629. [DOI] [PubMed] [Google Scholar]
- 26.Stachenfeld NS. Sex hormone effects on body fluid regulation. Exerc Sport Sci Rev. 2008;36(3):152. doi: 10.1097/JES.0b013e31817be928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Teixeira ALS, Dias MRC, Damasceno VO, Lamounier JA, Gardner RM. Association between different phases of menstrual cycle and body image measures of perceived size, ideal size, and body dissatisfaction. Percept Mot Skills. 2013;117(3):892–902. doi: 10.2466/24.27.PMS.117x31z1. [DOI] [PubMed] [Google Scholar]
- 28.Thomsen TK, Jensen VJ, Henriksen MG. In vivo measurement of human body composition by dual-energy X-ray absorptiometry (DXA) Eur J Surg. 1998;164(2):133–137. doi: 10.1080/110241598750004797. [DOI] [PubMed] [Google Scholar]
- 29.Tomazo-Ravnik T, Jakopič V. Changes in total body water and body fat in young women in the course of menstrual cycle. Int J Anthropol. 2006;21(1):55–60. [Google Scholar]
- 30.Tucker LA, Lecheminant JD, Bailey BW. Test-retest reliability of the bod pod: the effect of multiple assessments. Percept Mot Skills. 2014;118(2):563–570. doi: 10.2466/03.PMS.118k15w5. [DOI] [PubMed] [Google Scholar]
- 31.Vilaca KH, Ferriolli E, Lima NK, Paula FJ, Moriguti JC. Effect of fluid and food intake on the body composition evaluation of elderly persons. J Nutr Health Aging. 2009;13(3):183–186. doi: 10.1007/s12603-009-0055-4. [DOI] [PubMed] [Google Scholar]
- 32.White CP, Hitchcock CL, Vigna YM, Prior JC. Fluid retention over the menstrual cycle: 1-year data from the prospective ovulation cohort. Obstet Gynecol Int. 2011 doi: 10.1155/2011/138451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wingfield HL, Smith-Ryan AE, Woessner MN, Melvin MN, Fultz SN, Graff RM. Body composition assessment in overweight women: validation of air displacement plethysmography. Clin Physiol Funct Imaging. 2014;34(1):72–76. doi: 10.1111/cpf.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]