Abstract
The extralaryngeal bifurcation point of the recurrent laryngeal nerve (RLN) is typically located in a mean distance of 0–2 cm from the cricothyroid joint (CTJ). In the presented case though, the left RLN was unexpectedly identified bifurcating in a mean distance of 7 cm from the left CTJ in a young woman with multinodular goiter during total thyroidectomy. The RLN was carefully exposed throughout its course for the avoidance of iatrogenic injury of the nerval structure. The operation was uneventful. The present manuscript aims to highlight a scarce anatomic variation and its implications for thyroidectomy. Rare anatomic variations of the RLN such as the presented one encumber thyroid surgery and represent a severe risk factor of RLN injury. Meticulous operative technique combined with surgeons’ perpetual awareness concerning this peculiar anatomical aberration leads to an injury-free thyroid surgery.
INTRODUCTION
Identification and preservation of the recurrent laryngeal nerve (RLN) and its branches during thyroidectomy is a step of paramount clinical significance [1]. Anatomic variations of the RLN represent a major risk factor of RLN injury [2]. Although current monitoring procedures reduce the potentiality of accidental injury, direct visual detection of the RLN remains the gold standard in thyroidectomy [3]. In the presented case, the left RLN was incidentally detected during total thyroidectomy, bifurcating in a mean distance of 7 cm from the cricothyroid joint (CTJ). The present manuscript aims to underline a peculiar anatomic variation and its implications for thyroidectomy.
CASE REPORT
A 33-year-old Caucasian female was operated to our institution for resistant to medication multinodular goiter. Upon admission the patient had palpable thyroid nodules. The patient had nor hoarseness neither discernible cervical lymph nodes. Blood tests including TSH, T3 and T4 were in the normal spectrum. An ultrasound scan detected tumescent masses on the surface of both thyroid lobes. Following these, total thyroidectomy was finally scheduled.
A standard thyroid collar incision of ~6 cm was made, 1–2 cm above the sternal notch and was extended over the sternocleidomastoid muscles. At first, the middle thyroid vein was ligated and the superior poles were mobilized. Both the carotid artery and the jugular vein were gently retracted.
Surgeons performed gradual dissection along with the tracheoesophageal groove until the RLN’s entry in the larynx and unexpectedly identified that the extralaryngeal bifurcation point (ELBP) of the left RLN was located at a mean distance of 7 cm from the left CTJ (Fig. 1). Such an anatomic variation may augment the probability of the RLN injury or of its branches. Subsequently, identification of the RLN at a single point is not suffice for safe thyroidectomy. Then, surgeons exposed the right RLN which was detected as in common, in the right tracheoesophageal groove, medially to the common carotid artery, branching within the proximal 1–2 cm of the CTJ.
Figure 1:
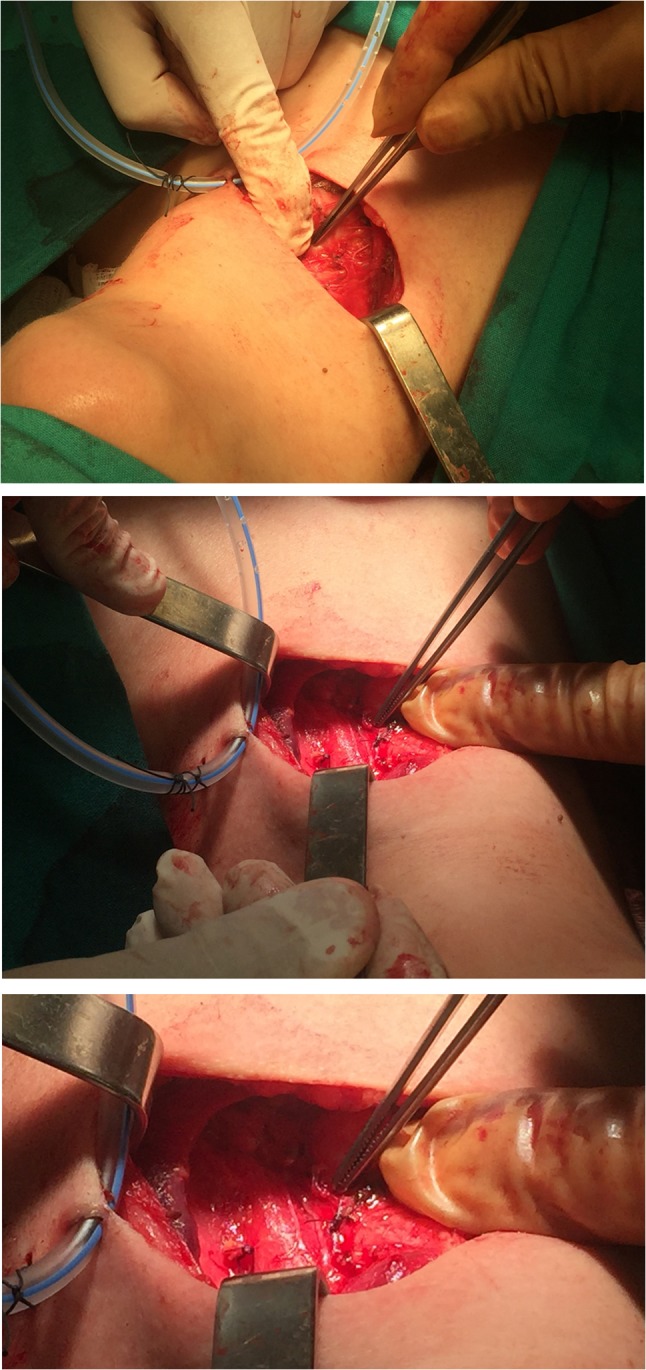
Extralaryngeal division of the left RLN was incidentally located at a mean distance of 7 cm from the left CTJ.
Thyroidectomy continued in usual fashion and was uneventful. The patient was discharged the second postoperative day, when the drainage placed was removed. At the follow-up, the 10th postoperative day, the patient had none complication.
DISCUSSION
The RLN is a branch of the vagus nerve (CN: X) that arises in the inferior neck and carries sensory, motor and parasympathetic fibers to the intrinsic muscles of the larynx apart from the cricothyroid muscle [4]. The main trunk of the RLN divides in order its terminal branches to innervate their respective muscles. This branching may occur within the larynx or extralaryngeally [5, 6].
The extralaryngeal branching (ELB) of RLN is a common anatomic variation that poses an increased potentiality of surgical morbidity in thyroid surgery [2]. In fact, the prevalence of ELB is 60% and this variation is symmetrical in 36.5% of individuals [1]. Its prevalence has no differences in geographic or sex-based subgroups [1].
The most common pattern of RLN extralaryngeal division is bifurcation, as in the presented case, with an incidence of 51% [1]. However, extralaryngeal trifurcation or multiple branches may also occur [1, 2, 5]. When the RLN bifurcates extralangyngeally, the motor branch is the anterior one and the sensory branch runs posterior and medial [5].
The ELBP is typically located in a mean distance of 0–1 cm, or 1–2 cm from the CTJ [1, 5]. Nevertheless in some cases, the ELBP was located at 3.1–4 cm away from the CTJ, with incidence 1.3% [5]. Surprisingly though, in the presented case, the left RLN bifurcated within the proximal 7 cm of the left CTJ.
Specific classification systems aim to present probable ELB anatomic variations, but still it seems that they are not all yet elucidated [1]. Subsequently, when performing thyroid surgery it is essential to expose meticulously the main trunk of RLN and the course of its extralaryngeal branches [7]. This surgical step is of vital significance, since the majority of intraoperative RLN injuries result from failure to recognize all the nerval structures [8].
In particular, when surgeons perform the capsular dissection to thyroidectomy, it is possible that the posterior branch could be presumed as the sole branch of RLN. Herein, the anterior branch is susceptible to injury that may lead to vocal cord palsy [1, 8]. Due to the extended distance of the ELBP from the CTJ, as in the presented case, the probability of RLN iatrogenic injury is even higher.
The identification of the RLN and of its external branches is potential by the utilization of current intraoperative monitoring devices (IONM). However, such procedures are only an adjunct to the visual nerve identification that remains the gold standard in thyroid surgery [3, 8].
Hereby, the use of several anatomic landmarks, such as the Berry’s ligament, the tracheoesophageal groove and the inferior thyroid artery may guide surgeons to the detection of RLN [1, 5]. Unfortunately though, the relation between RLN and these structures may not be helpful in case of a large goiter, inflammation, extended edema or of anatomic variation, as in the presented case [1, 2].
Iatrogenic injury of the RLN is a severe postoperative complication in thyroid surgery that can lead to RLN palsy with symptoms ranging from almost indescribable hoarseness to stridor or even acute airway obstruction, in case of bilateral RLN accidental damage [9, 10].
The incidence of temporary paresis of RLN is ranging from 0.4 to 7.2% and from 0 to 5.2% to permanent nerve paralysis [8]. Therefore, it is reasonable that RLN injury remains a common cause of litigation in thyroid surgery [8].
Hence, fundamentals to avoid RLN iatrogenic injury are: (i) exposure of the RLN and of its extralaryngeal branches throughout their course, since it is quite evident that probable novel anatomic variations of the RLN may be unexpectedly detected during the operation (ii) good haemostasis and (iii) use of IONM when the intraoperative nerve identification is difficult.
In conclusion, even an anatomic variation of minor degree may affect the outcome of thyroidectomy. Subsequently, surgeons’ deep knowledge in addition to meticulous operative technique are the cornerstone for an injury-free thyroid surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
REFERENCES
- 1. Henry BM, Vikse J, Graves JM, Sanna S, Sanna B, Tomaszewska IM, et al. Extralaryngeal branching of the recurrent laryngeal nerve: a meta-analysis of 28,387 nerves. Langenbecks Arch Surg 2016;401:913–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Shao T, Qiu W, Yang W. Anatomical variations of the recurrent laryngeal nerve in Chinese patients: a prospective study of 2,404 patients. Sci. Rep 2016;6:25475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Page C, Monet P, Peltier J, Bonnaire B, Strunski V. Non-recurrent laryngeal nerve related to thyroid surgery: report of three cases. J Laryngol Otol 2008;122:757–61. [DOI] [PubMed] [Google Scholar]
- 4. Moore KL, Dalley AF, Agur AM. Clinically Oriented Anatomy. 7th edn Philadelphia: Lippincott Williams & Wilkins, 2014. [Google Scholar]
- 5. Asgharpour E, Maranillo E, Sañudo J, Pascual-Font A, Rodriguez-Niedenfurh M, Valderrama FJ, et al. Recurrent laryngeal nerve landmarks revisited. Head Neck 2012;34:1240–6. [DOI] [PubMed] [Google Scholar]
- 6. Schweizer V, Dörfl J. The anatomy of the inferior laryngeal nerve. Clin Otolaryngol Allied Sci 1997;22:362–9. [DOI] [PubMed] [Google Scholar]
- 7. Hisham AN, Lukman MR. Recurrent laryngeal nerve in thyroid surgery: a critical appraisal. ANZ J Surg 2002;72:887–9. [DOI] [PubMed] [Google Scholar]
- 8. Barczynski M, Konturek A, Pragacz K, Papier A, Stopa M, Nowak W. Intraoperative nerve monitoring can reduce prevalence of recurrent laryngeal nerve injury in thyroid reoperations: results of a retrospective cohort study. World J Surg 2014;38:599–606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Erbil Y, Barbaros U, Işsever H, Borucu I, Salmaslioğlu A, Mete O, et al. Predictive factors for recurrent laryngeal nerve palsy and hypoparathyroidism after thyroid surgery. Clin Otolaryngol 2007;32:32–7. [DOI] [PubMed] [Google Scholar]
- 10. Jeannon JP, Orabi AA, Bruch GA, Abdalsalam HA, Simo R. Diagnosis of recurrent laryngeal nerve palsy after thyroidectomy: a systematic review. Int J Clin Pract 2009;63:624–9. [DOI] [PubMed] [Google Scholar]


