Abstract
Background
This study examines whether performance of bout-related physical activity (PA) during morning hours is related to greater overall bout-related PA increases within a preoperative PA intervention for bariatric surgery (BS) patients.
Methods
Participants with severe obesity (n = 33; mean age = 45.6 ± 9.6 years; BMI = 45.7 ± 7.0 kg/m2) seeking BS were randomized to and completed 6 weeks of preoperative PA counseling (retention = 82.5%). Participants were encouraged to walk daily at a moderate intensity in bouts ≥ 10 minutes during morning hours to overcome time-related obstacles and establish a PA habit. Timing and amount of bout-related moderate-to-vigorous PA (MVPA) was assessed via objective monitor at pre- and postintervention.
Results
Greater proportion of bout-related MVPA performed during morning hours (4:00 AM–12:00 PM) at postintervention was associated with larger total increases in bout-related MVPA minutes/day (β = .40, P = .03). At postintervention, a greater proportion of participants whose longest MVPA bouts occurred during morning hours (n = 11) achieved the public health guideline (ie, ≥150 bout-related MVPA minutes/week) versus those whose longest MVPA bouts occurred during nonmorning hours (n = 19; 63.6% vs. 26.3%, P = .04).
Conclusions
Intervention-related increases in PA tended to be greatest when PA was performed in the morning. Morning exercise may be a viable strategy for promoting habitual PA in inactive BS patients.
Keywords: obesity, exercise, accelerometer, behavioral intervention
Nearly all bariatric surgery (BS) patients are inactive preoperatively based on public health guidelines, accumulating < 150 weekly minutes of moderate-to-vigorous physical activity (MVPA) in bouts ≥ 10-minutes (ie, bout-related MVPA).1,2 Further, approximately two-thirds of BS patients do not perform any bout-related MVPA.3–5 Efforts to increase bout-related MVPA in BS patients preoperatively are needed given that most patients fail to make substantial MVPA changes postoperatively,4,5 and higher preoperative MVPA strongly predicts higher postoperative PA.1,6 One common obstacle to habitual MVPA adoption in obese populations, including BS patients, is perceived lack of time.7–9 Performing MVPA in the morning, before work and other distractions can interfere, might help to counter this obstacle. Additionally, performing MVPA during morning hours at a consistent time each day might help to establish a PA habit through routine and repetition.10
No previous study has examined the role of time of day of MVPA in amount of MVPA performed by BS patients. We recently showed in the Bari-Active trial, a 6-week preoperative physical activity intervention (PAI) designed to increase moderate-intensity daily walking exercise in bouts ≥ 10-minutes produced significant increases in objectively measured daily bout-related MVPA relative to standard surgical care control.11 Intervention participants were encouraged to perform walking exercise at a consistent time each day during morning hours.
In this secondary analysis, we examine whether adherence to morning exercise is associated with total bout-related MVPA performed within the Bari-Active intervention. In PAI completers, we evaluated whether: 1) performing a larger percentage of MVPA during morning hours was associated with higher levels of total bout-related MVPA after intervention; and 2) morning exercisers who accumulated their longest MVPA bouts during 4:00 AM–12:00 PM performed more total bout-related MVPA after intervention and were more likely to achieve the public health guideline (≥150 bout-related MVPA minutes/week1) compared with nonmorning exercisers who accumulated their longest MVPA bouts after 12:00 PM.
Methods
Participants
Figure 1 shows flow of participants throughout the Bari-Active Trial. The current study focused on participants (n = 33) who were randomized to and completed the PAI. Eligibility criteria included: aged 18 to 70 years, body mass index (BMI) ≥ 35 kg/m2, and inactive but able to walk ≥ 2 blocks unassisted. Individuals were ineligible if scheduled for BS < 10 weeks during screening, participating in another exercise/weight loss program, intending to relocate geographically, or had limitations that could interfere with protocol adherence.
Figure 1.
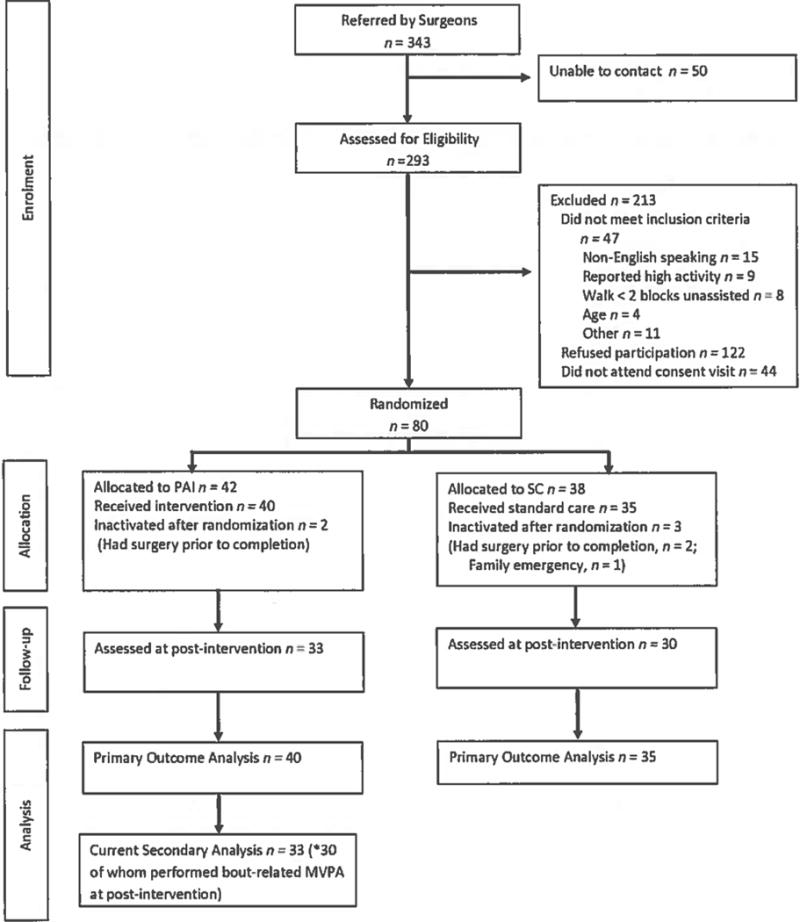
Flow of participants through the trail.
Design/Procedures
BS-seeking individuals were referred by surgical clinics in Rhode Island, USA between April 2010 and January 2014. Patients who sought to participate and received surgeon approval for walking exercise were screened by telephone. Eligible patients were invited to an orientation/baseline session where they completed informed consent and the baseline assessment protocol, and received an activity monitor to wear for 7 consecutive days. Participants were then randomized to 6 weeks of intervention or control. Participants wore the activity monitor again at postintervention and received $50 for assessment completion. The Miriam Hospital IRB approved study procedures (clinicaltrials.gov NCT00962325).
Intervention
Participants received 2 intervention goals: increase bout-related moderate intensity walking exercise by 30 minutes/day and steps by 5000/day from baseline. To help achieve these goals, participants received 6 weekly individual face-to-face counseling sessions (each lasting 30 to 45 min), a hip-worn pedometer (ie, Accusplit Digi-Walker Step Pedometer AE120XL to track daily steps), and PA planning/monitoring paper-and-pencil logs (to record both bout-related walking exercise minutes and steps at the end of each day). Counseling sessions focused on: 1) reviewing self-monitoring records and goal progress; and 2) problem-solving barriers and teaching standard behavioral strategies (eg, stimulus control, behavioral contracting, goal-setting, action planning, etc.) to achieve goals. Additionally, participants were encouraged to identify a consistent time each day during morning hours for longer walking bouts, so as to overcome time-related obstacles to habitual physical activity (PA) adoption, use time as a cue for initiating PA behavior, and establish a PA habit through routine/repetition.8 Additionally, shorter walking bouts ≥ 10 minutes were encouraged whenever possible throughout the remainder of the day. See Bond et at11 for a more detailed description of weekly intervention content/strategies. Regarding goal-related progression of PA over the intervention period, participants were instructed to maintain their usual pattern of PA during the initial week to establish baseline levels. For the second week, participants were given goals to add 10 minutes of bout-related walking exercise and 1000 steps per day to baseline amounts. For each subsequent week, participants added 5 minutes of bout-related walking exercise and 1000 steps per day to the totals accumulated during the previous week.
Measures
Objectively Measured MVPA
Participants were asked to wear the SenseWear Armband (SWA; BodyMedia, Inc., Pittsburgh PA) during waking hours for 7 consecutive days at pre- and postintervention (ie, immediately after the 6th and final week of intervention) as an objective measure of daily bout-related MVPA.12,13 SenseWear Professional Software (Version 7.0) calculated wear time and provided minute-by-minute metabolic equivalent (MET) values used to define MVPA (≥3 METs). Allowance of ≤ 1 min at < 3 METs was used in identifying MVPA bouts ≥ 10 min. Proportion of bout-related MVPA minutes during morning hours was calculated by dividing the sum of that occurring after 4:00 AM and before 12:00 PM by total bout-related MVPA minutes. Participants were identified as morning or nonmorning exercisers based on whether the majority of their longest MVPA bouts occurred during morning versus nonmorning hours. Bouts of longer duration serve as a proxy for structured exercise.14 To determine average bout duration for each hour of the day, total bout-related MVPA minutes within each hour was divided by total number of bouts occurring in that hour across days of monitor wear. Bouts spanning 2 hours were divided evenly between hours. Wear time ≥ 8 hours/day on ≥ 4 days for was required for inclusion in analysis.
Other Measures
At baseline, weight was measured and demographic information (ie, age, sex, race/ethnicity, education, occupation) was collected via questionnaire.
Statistical Analysis
Analyses were performed using SPSS Statistics for Windows (version 20.0; SPSS, IBM Corp, Armonk, NY). Means and standard deviations (SD) and frequency counts were calculated to describe participant characteristics. Independent t tests and χ tests compared differences between both PAI completers and noncompleters and morning exercisers and nonmorning exercisers. Linear regression evaluated association between proportion of bout-related MVPA during morning hours and average bout-related MVPA minutes/day at postintervention, adjusting for baseline bout-related MVPA. Analysis of covariance (ANCOVA) compared total bout-related MVPA minutes/day at poslintervention in morning and nonmorning exercisers, adjusting for baseline bout-related MVPA. Chi-square compared proportions of morning and nonmorning exercisers who achieved the PA public health guideline (ie, ≥150 bout-related MVPA minutes/week1). Significance tests were two-tailed (α = .05).
Results
Participant Characteristics
Table 1 shows baseline characteristics of the 33 PAI completers (retention = 82.5%). On average, participants were middle-aged with severe obesity. The majority were female, non-Hispanic White, had < 4 years college/university education, and were employed mostly in professional, administrative, or executive occupational roles. Overall, participants were inactive, averaging < 5 bout-related MVPA minutes/day (due to that 42% of participants performed 0 ≥ 10-min bouts, 38% performed at least 1 ≥ 10-minute bout, and only 20% performed least 1 ≥ 10-min bout during each individual day of the 7-day monitoring period) and < 5000 steps/day. PAI completers and noncompteters did not significantly differ on any of the above variables (P > .05). There was a nonsignificant trend for completers to be older versus noncompleters (45.8 ± 9.6 vs. 38.6 ± 8.3 years, P = .07).
Table 1.
Baseline Characteristics of Physical Activity Intervention Completers
| Demographic and anthropometric characteristics | |
|---|---|
| Sex (%) | |
| Men | 12.1 |
| Women | 87.9 |
| Age, mean (SD), years | 45.9 (9.5) |
| Race (%) | |
| Native Hawaiian/Other Pacific Islander | 3.0 |
| Black | 6.1 |
| White | 78.8 |
| Other | 12.1 |
| Ethnicity (%) | |
| Hispanic | 12.1 |
| Education (%) | |
| ≥ 4-year college/university degree | 30.3 |
| Employed (%) | 75.8 |
| Professional, administrator, or executive | 60.0 |
| Clerical work, administrative support, sales, or technician | 36.0 |
| Crafts, trade, factory work, service or labor | 4.0 |
| Body Mass Index, mean (SD), kg/m2 | 45.7 (7.0) |
| Physical Activity | |
| Bout-related MVPA minutes/day, mean (SD) | 4.2 (5.4) |
| Steps/day, mean (SD) | 4991(2539) |
Association Between Time of Day of Bout-Related MVPA and Total Amount of Bout-Related MVPA
Analysis included 30 (90.9%) of 33 PAI participants who performed bout-related MVPA at postintervention and wore the SWA for 12.5 ± 1.4 hours/day on 6.6 ± 1.1 days. Greater proportion of bout-related MVPA during morning hours was associated with greater increases in bout-related MVPA minutes/day, adjusting for baseline bout- related MVPA (β=.40, P =.036). Figure 2A–B presents descriptive data on timing of bout-related MVPA amount and frequency during each hour of the day. Participants on average performed 27.0 ± 21.8 bout-related MVPA minutes/day, of which 34.9% was accumulated during morning hours. On average, the longest bouts appeared to occur during morning hours, whereas bout frequency appeared to be higher during nonmorning hours, particularly between 12:00 PM and 8:00 PM.
Figure 2.
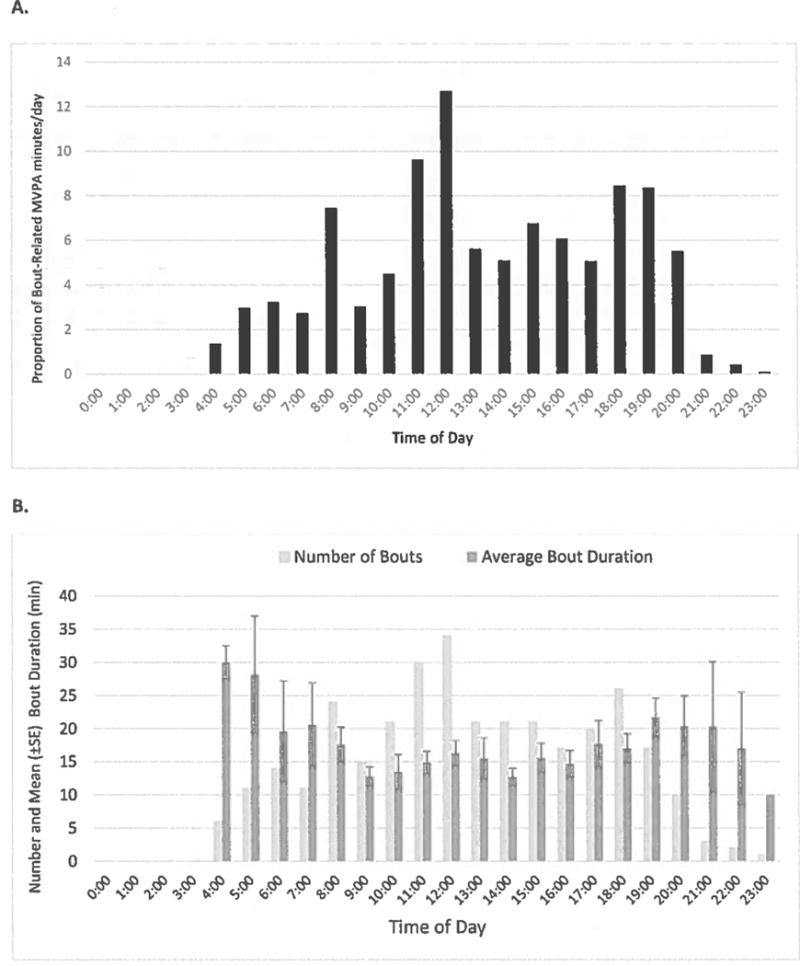
A. Mean proportion of daily bout-related moderate-to-vigorous physical activity (MVPA) minutes by hour of the day at post-intervention. B. Number and mean duration of MVPA bouts by hour of the day across the 7-day monitoring period at postintervention.
Figure 3 shows average total bout-related MVPA minutes/day performed at postintervention across morning hours, nonmorning hours, and all waking hours for morning (n = 11) and nonmorning (N = 19) exercising PAI participants. At baseline, morning and nonmorning exercisers did not significantly differ on demographic characteristics (ie, age, sex, race/ethnicity, education, marital status, all P > .10), employed status and type of occupation (all P > .20), and daily bout-related MVPA (P= .62). However, morning exercisers were significantly heavier versus nonmorning exercisers (mean BMI = 49.3 ± 8.4 vs. 43.0 ± 5.1 kg/m2, P = .016).
Figure 3.
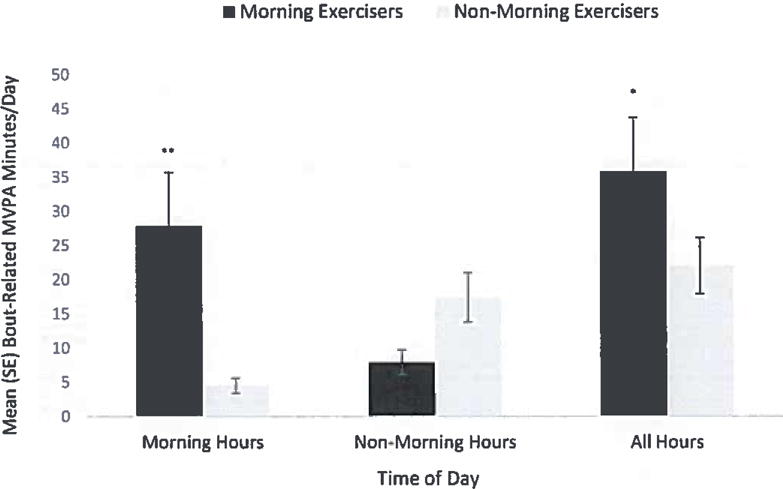
Differences between morning and non-morning exercisers in bout-related moderate-to-vigorous physical activity performed during morning hours, nonmorning hours, and all hours at postintervention. *P < .05. **P < .001 for morning exercisers vs. nonmorning exercisers.
As per design, morning exercisers performed more bout-related MVPA minutes/day during morning hours (27.9 ± 25.9 vs. 4.5 ± 4.6 minutes/day, P < .001) versus nonmorning exercisers. Morning exercisers also performed more daily bout-related MVPA versus nonmorning exercisers (35.8 ± 26.1 vs. 22.0 ± 17.8 minutes/day, P = .043), adjusting for baseline bout-related MVPA. A greater proportion of morning exercisers achieved ≥ 150 bout-related MVPA minutes/week, compared with nonmorning exercisers (63.6% vs. 26.3%, P = .044).
Discussion
This study is the first to objectively evaluate adherence to prescribed timing of free-living exercise in the context of a physical activity intervention (PAI). Specifically, we examined whether performance of PA during morning hours was associated with greater PA increases after a preoperative PAI for BS patients that involved recommended daily morning walking exercise. Among PAI participants, greater proportion of daily bout-related MVPA performed during morning hours was associated with more total bout-related MVPA after intervention. Moreover, nearly two-thirds of morning exercisers achieved bout-related MVPA levels consistent with public health guidelines,1 compared with one-quarter of nonmorning exercisers. These findings suggest that patients with better adherence to morning exercise tended to be more successful in increasing PA. Thus, prescribing morning PA may be a potentially viable strategy to promote habitual PA adoption in BS patients. Identifying effective strategies for increasing MVPA in BS patients is important given that the vast majority are inactive preoperatively and bariatric surgery has shown to have limited if any impact on MVPA levels postoperatively.2–5 Further, morning exercise may help to counter perceived lack of time, a frequently reported barrier to PA participation in BS patients and one which is unlikely to be affected by weight loss and other surgical outcomes.7,8
Previous research suggests that morning PA may also carry additional health benefits, which in turn, could promote greater PA participation in BS patients. In the Women’s Health Study, participants who performed less PA during the morning had higher odds of obesity versus those who performed more, suggesting morning PA assists with weight control.15 Morning PA might also positively impact body weight and energy to perform PA by improving nocturnal sleep patterns via increased parasympathetic nerve activity and circadian rhythms through increased light exposure.16–18 Additionally, morning PA, particularly in the fasted state, may contribute to improved metabolic control on the day of and day after exercise.19,20 Additional research is needed to confirm whether morning exercise confers similar benefits in BS patients, and if such benefits can enhance the effects of exercise on postoperative weight and metabolic outcomes.
This study has limitations. While use of objectively measured MVPA bouts as an exercise proxy and detailed analysis of hourly data to estimate morning exercise adherence is novel and a strength, we cannot definitely determine whether participants were exercising nor the type of exercise being performed. While this study provides correlational data to support the potential benefit of performing exercise in the morning for increasing overall exercise participation in BS patients who were willing to complete a PAI, future experimental research that directly tests the effects of a morning versus later day exercise prescription is needed to corroborate these findings. This study did not include long-term follow-up assessment. Future research is warranted to determine whether morning exercise is a useful strategy for promoting PA maintenance as well as adoption. It should be noted that while morning exercise might be a useful strategy for some BS patients, it might not be desirable/feasible for all. For example, we did not collect data on caregiver status, which might limit ability to engage in morning exercise. In addition, we did not conduct qualitative interviews of participants to obtain reasons for participating or not participating in morning exercise. Thus, another aim of future research in this area should be to gain greater insight into acceptability and feasibility of prescribing and performing morning exercise in this patient population. Finally, it should be noted that the best time for patients to exercise is when they are able and motivated to do so.
Conclusion
In this sample of BS patients, intervention-related increases in preoperative bout-related MVPA tended to be greatest when bout-related MVPA was performed in the morning. Morning exercise may be a promising strategy for promoting a more active lifestyle in BS patients.
Acknowledgments
The authors would like to express appreciation to Drs. G. Dean Roye (The Miriam Hospital, Providence RI, USA) Harry C. Sax (Cedars Sinai Hospital, Hollywood CA, USA), and Dieter Pohl (Roger Williams Hospital, Providence, RI) for assistance with recruitment. This work was supported by a grant (DK083438) from the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health. This study is registered at clinicaltrials.gov (NCT00962325)
Contributor Information
Dale S. Bond, Dept of Psychiatry and Human Behavior, Alpert Medical School of Brown University/The Miriam Hospital Weight Control and Diabetes Research Center, Providence, RI
Hollie A. Raynor, Dept of Nutrition, University Of Tennessee, Knoxville, TN
J. Graham Thomas, Dept of Psychiatry and Human Behavior, Alpert Medical School of Brown University/The Miriam Hospital Weight Control and Diabetes Research Center, Providence, RI.
Jessica Unick, Dept of Psychiatry and Human Behavior, Alpert Medical School of Brown University/The Miriam Hospital Weight Control and Diabetes Research Center, Providence, RI.
Jennifer Webster, Dept of Psychiatry and Human Behavior, Alpert Medical School of Brown University/The Miriam Hospital Weight Control and Diabetes Research Center, Providence, RI.
Beth Ryder, Dept of Surgery, Alpert Medical School of Brown University/The Miriam Hospital, Providence, RI.
Sivamainthan Vithiananthan, Dept of Surgery, Alpert Medical School of Brown University/The Miriam Hospital, Providence, RI.
References
- 1.Haskell WL, Lee IM, Pate RR, et al. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation. 2007;116:1081–1093. doi: 10.1161/C1RCULATIONAHA.107.185649. [DOI] [PubMed] [Google Scholar]
- 2.Bond DS, Thomas JG. Measurement and intervention on physical activity and sedentary behaviors in bariatric surgery patient: emphasis on mobile technology. Eur Eat Disord Rev. 2015;23:470–478. doi: 10.1002/erv.2394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bond DS, Jakicic JM, Vithiananthan S, et al. Objective quantification of physical activity in bariatric surgery candidates and normal-weight controls. Surg Obes Relat Dis. 2010;6:72–78. doi: 10.1016/j.soard.2009.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bond DS, Jakicic JM, Unick JL, et al. Pre- to postoperative changes in bariatric surgery patients: self-report vs. objective measures. Obesity (Silver Spring) 2010;18:2395–2397. doi: 10.1038/oby.2010.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.King WC, Chen JY, Bond DS, et al. Objective assessment of changes in physical activity and sedentary behavior: pre- through 3 years post-bariatric surgery. Obesity (Silver Spring) 2015;23:1143–1150. doi: 10.1002/oby.21106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.King WC, Hsu JY, Belle SH, et al. Pre- to postoperative changes in physical activity: report from the longitudinal assessment of bariatric surgery-2 (LABS-2) Sitrg Obes Relat Dis. 2012;8:522–532. doi: 10.1016/j.soard.2011.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bond DS, Thomas JG, Ryder BA, Vithiananthan S, Pohl D, Wing RR. Ecological momentary assessment of the relationship between intention and physical activity behavior in bariatric surgery patients. Int J Behav Med. 2013;20:82–87. doi: 10.1007/s12529-011-9214-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zabatiero J, Hill K, Gucciardi DF, et al. Beliefs, barriers, and facilitators to physical activity in bariatric surgery candidates. Obes Surg. 2016;26(5):1097–1099. doi: 10.1007/s11695-015-1867-4. [DOI] [PubMed] [Google Scholar]
- 9.Napolitano MA, Papandonalos GD, Borradaile KE, Whiteley JA, Marcus BH. Effects of weight status and barriers on physical activity adoption among previously inactive women. Obesity (Silver Spring) 2011;19:2183–2189. doi: 10.1038/oby.2011.87. [DOI] [PubMed] [Google Scholar]
- 10.Pimm R, Vandelanotte C, Rhodes RE, Short C, Duncan MJ, Rebar AL. Cue consistency associated with physical activity automaticity and behavior. Behav Med. 2016;42(4):248–53. doi: 10.1080/08964289.2015.1017549. [DOI] [PubMed] [Google Scholar]
- 11.Bond DS, Vithiananthan S, Thomas JG, et al. Bari-Active: a randomized controlled trial of a preoperative intervention to increase physical activity in bariatric surgery patients. Surg Obes Relat Dis. 2015;11:169–177. doi: 10.1016/j.soard.2014.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mackey DC, Manini TM, Schoeller DA, et al. Validation of an armband to measure daily energy expenditure in older adults. J Gerontol A Biol Sci Med Sci. 2011;66:1108–1113. doi: 10.1093/gerona/glr101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Unick JL, Bond DS, Jakicic JM, et al. Comparison of two objective monitors for assessing physical activity and sedentary behaviors in bariatric surgery patients. Obes Surg. 2012;22:347–352. doi: 10.1007/s11695-011-0491-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Catenacci VA, Grunwald GK, Ingebrigtsen JP, et al. Physical activity patterns using accelerometry in the National Weight Control Registry. Obesity (Silver Spring) 2011;19:1163–1170. doi: 10.1038/oby.2010.264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chomistek AK, Shiroma EJ, Lee IM. The relationship between time of day of physical activity and obesity in older women. J Phys Act Health. 2016;13:416–418. doi: 10.1123/jpah.2015-0152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tworoger SS, Yasui Y, Vitiello MV, et al. Effects of a year-long moderate-intensity exercise and a stretching intervention on sleep quality in postmenopausal women. Sleep. 2003;26:830–836. doi: 10.1093/sleep/26.7.830. [DOI] [PubMed] [Google Scholar]
- 17.Yamanaka Y, Hashimoto S, Takasu NN, et al. Morning and evening physical exercise differentially regulate the autonomic nervous system during nocturnal sleep in humans. Am J Physiol Regul Integr Comp Physiol. 2015;309:R1112–R1121. doi: 10.1152/ajp-regu.00127.2015. [DOI] [PubMed] [Google Scholar]
- 18.Reid KJ, Santostasi G, Baron KG, et al. Timing and intensity of light correlate with body weight in adults. PLoS One. 2014;9:392251. doi: 10.1371/journal.pone.0092251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gomez AM, Gomez C, Aschner P, et al. Effects of performing morning versus afternoon exercise on glycemic control and hypoglycemia frequency in type 1 diabetes patients on sensor-augmented insulin pump therapy. J Diabetes Sci Technol. 2015;9:619–624. doi: 10.1177/1932296814566233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Van Proeyen K, Szlufcik K, Nielens H, et al. Training in the fasted state improves glucose tolerance during fat-rich diet. J Physiol. 2010;588(Pt 21):4289–4302. doi: 10.1113/jphysiol.2010.196493. [DOI] [PMC free article] [PubMed] [Google Scholar]


