Abstract
Surgical management of vitiligo is considered an excellent terapeutic option for recalcitrant cases, provided the disease is stable and there is absence of Koebner phenomenom. Among surgical modalities, Suction Blister Epidermal Graft is a low cost and effective option (65 to 100% repigmentation can be achieved in up to 80% of patients). We describe how it can be optimized by using an alternative suction equipment, by customization of graft format and by application of an anesthetic technique that substantially reduces procedure time.
Keywords: Vitiligo; Transplantation, Autologous; Surgical procedures, Minor
Vitiligo is an autoimmune condition that targets the melanocytes and affects approximately 0.5% of the world's population. It is characterized by depigmented patches that can cause significant mental and social impact in the patients.1 Medical therapeutic approaches such as phototherapy, corticotherapy and calcineurin inhibitors are considered first line treatments.2
Surgical treatment is seen as a great therapeutic option for cases resistant to medical treatment, provided the lesions are stable and there is no evidence of Köbner phenomenom.3 Disease stability is the most important factor for a good surgical outcome. It is currently defined by most authors as the absence of new lesions or enlargement of old lesions for one year.4
Suction blister epidermal grafting (SBEG) is considered a low-cost and effective procedure (65% to 100% of repigmentation can be obtained in up to 80% of patients).3,5 It is performed with the transfer of epidermal grafts from the donor site (usually thighs or arms) to the recipient site, commonly pre-treated with dermabrasion.3 In turn, the grafts are obtained from the roof of the subepidermal blisters, formed by prolonged vacuum application on the donor site. To achieve this, syringes without the plunger, connected to a 3-way connector are used (Figure 1).5 Although these are devices of easy access, syringes usually come off during the procedure, needing frequent reapplication of the vacuum by the surgeon.
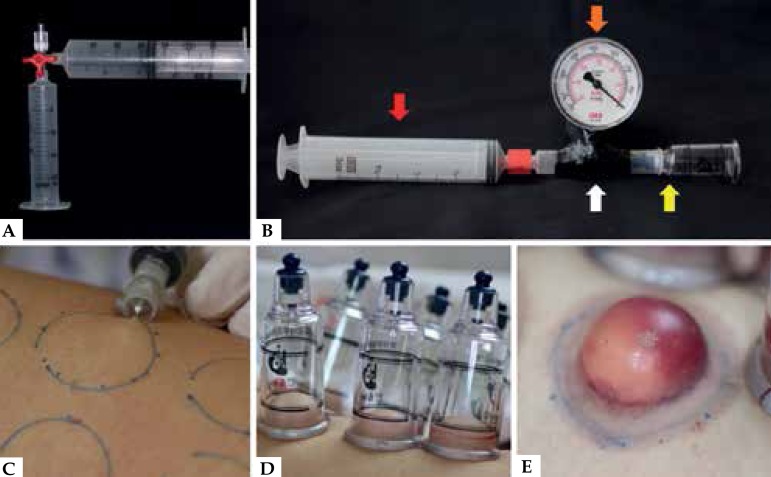
Figure 1.
A - Syringe without plunger connected to the suction syringe through a 3-way connector. B - 2.5 cm suction cup (yellow arrow) connected to a vacuum gauge (orange arrow) adapted to a 5 ml syringe (white arrow), which is then connected to a 60 ml syringe (red arrow). C - Infiltration in two planes in the donor area. D - Suction cups in position (-350 mmHg). E - Subepidermal blister completely formed after 40 minutes
Originally designed for cupping therapy (an Eastern alternative medicine technique), suction cups with valves (Handisol Medical Co., Paju, South Korea) can be used to replace syringes, with some advantages. Because they are longer, they remain more stable on the patient, and tend to decouple less often during suction. Their borders, thick and rounded, are more anatomical, causing less injury to the periphery of the donor site. The vacuum application by the physician is made easier by the presence of a unidirectional flow valve, that does not allow reentry of air into the cup. The device can be connected to a vacuum gauge in order to accurately measure the cup's internal pressure and can be sterilized and reutilized (Figure 1 and Video).
Watch the video on the site: anaisdedermatologia.org.br
The optimal vacuum pressure to be maintained during the suction period varies according to the diameter of the cup being used. A very low pressure prolongs the time needed for the blister to form. In contrast, a very high pressure can produce a defective blister.3
One of the main disadvantages of SBEG is the prolonged time for the formation of suction blisters. For example, with the usual technique, the formation of a 2.2 cm blister can take up to two hours.3 However, it was already shown that infiltration of intradermal anesthetic in the donor site reduces the time for blister formation in more than 50%, considerably decreasing the total time for the procedure.6 Despite this beneficial effect, intradermal anesthesia causes more tissue distension and pain on infiltration. For this reason, we suggest anesthesia in two levels: initially in the superficial subcutaneous level and then in the intradermal level, so as to make the patient more comfortable during the procedure (Figure 1).
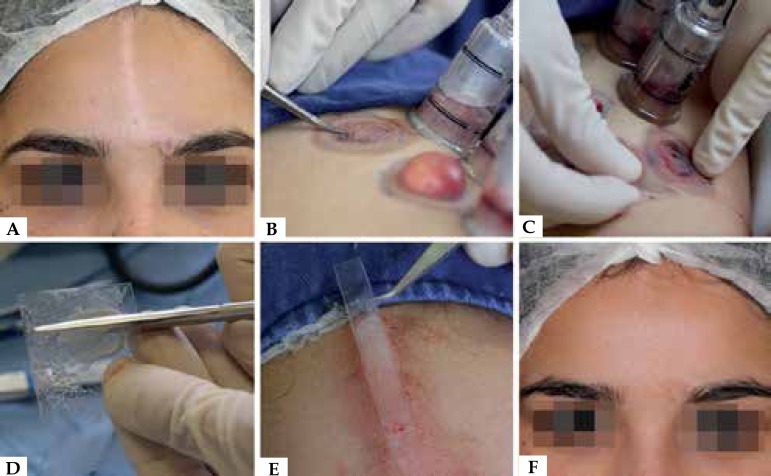
Because it is a very delicate graft, made of epidermis only, surgery is challenging. During removal from the donor site and transportation into the recipient site, the surgeon must be careful not to switch sides and avoid folding over, for both situations can jeopardize the procedure. After the graft is adequately incised and released from the donor site, the use of an acetate sheet (sterilizable and low-cost material) with petroleum jelly can make the transportto the recipient site easier (Figure 2). Because the sheet is flexible and transparent, it allows for the collection and release of the graft easily (Figure 2 and Video). Besides, the use of the acetate sheet facilitates cutting the graft, helping its use in cases of linear lesions such as the ones in segmental vitiligo (Figure 2).
Figure 2.
A - Segmental vitiligo with linear lesion on the forehead. B - Peripheral incision in the subepidermal blister. C - Epidermal graft transfer to the acetate sheet. D - Epidermal graft cut out. E - Application of the epidermal graft to the recipient site, treated with dermabrasion. F - Repigmentation higher than 90% six months after the procedure
Finally, SBEG has been a safe and effective therapeutic option, also for sensitive areas such as eyelids, perioral area and other facial areas.3,5,7 Possible complications include hyperpigmentation on the donor and recipient sites, peripheral dyspigmentation, milia and, rarely, infection.8,9 The technique can be improved with the aim of decreasing the time for the procedure, considered long so far, as well as guaranteeing better use of the epidermal grafts.
Footnotes
Study conducted at Hospital Santa Casa de Curitiba - Curitiba (PR), Brazil.
Financial support: none.
Conflict of interest: none.
REFERENCES
- 1.Tarlé RG, Nascimento LM, Mira MT, Castro CC. Vitiligo--part 1. An Bras Dermatol. 2014;89:461–470. doi: 10.1590/abd1806-4841.20142573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Faria AR, Tarlé RG, Dellatorre G, Mira MT, Castro CC. Vitiligo--Part 2--classification, histopathology and treatment. An Bras Dermatol. 2014;89:784–790. doi: 10.1590/abd1806-4841.20142717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gupta S, Olsson MJ, Kanwar AJ, Ortonne J-P. Surgical management of vitiligo. Oxford, UK: Blackwell Publishing; 2007. [Google Scholar]
- 4.Sahni K Parsad D. Stability in Vitiligo: Is there a Perfect Way to Predict it? J Cutan Aesthet Surg. 2013;6:75–82. doi: 10.4103/0974-2077.112667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gou D, Currimbhoy S, Pandya AG. Suction blister grafting for vitiligo: efficacy and clinical predictive factors. Dermatol Surg. 2015;41:633–639. doi: 10.1097/DSS.0000000000000341. [DOI] [PubMed] [Google Scholar]
- 6.Kim T, Roh HJ, Kim JY, Noh S, Oh SH. Rapid formation of suction blister through intradermal injection of local anesthetics in epidermal graft for vitiligo. Dermatol Surg. 2010;36:1642–1643. doi: 10.1111/j.1524-4725.2010.01700.x. [DOI] [PubMed] [Google Scholar]
- 7.Maleki M, Banihashemi M, Sanjari V. Efficacy of suction blister epidermal graft without phototherapy for locally stable and resistant vitiligo. Indian J Dermatol. 2012;57:282–284. doi: 10.4103/0019-5154.97669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ashique KT, Kaliyadan F. Long-Term Follow-up and Donor Site Changes Evaluation in Suction Blister Epidermal Grafting Done for Stable Vitiligo: A Retrospective Study. Indian J Dermatol. 2015;60:369–372. doi: 10.4103/0019-5154.160482. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khunger N, Kathuria SD, Ramesh V. Tissue grafts in vitiligo surgery - past, present, and future. Indian J Dermatol. 2009;54:150–158. doi: 10.4103/0019-5154.53196. [DOI] [PMC free article] [PubMed] [Google Scholar]