Abstract
Objectives
We evaluate how the size and composition of care networks changes with increasing morbidity count (i.e. multimorbidity) and how larger care networks relate to recipient psychological well-being.
Methods
Using the National Health and Aging Trends study (NHATS; N=7026), we conduct multivariate regressions to analyze size and compositional differences in care networks by morbidity count and recipient gender, and to examine differences in recipient psychological well-being linked to care network size.
Results
Women report larger and more diverse care networks than men. These gender differences strengthen with increasing morbidity count. Larger care networks are associated with diminished psychological well-being among care recipients, especially as morbidity increases.
Discussion
These findings reveal how increasing morbidity translates differently to care network size and diversity for men and women. They also suggest that having multiple caregivers may undermine the psychological well-being of care recipients who face complex health challenges.
Keywords: Caregiving, Epidemiology, Social Networks, Mental Health
Multimorbidity, or having multiple chronic health conditions, has become more prevalent in the US population and other advanced societies in recent decades, due to population aging and extended longevity (Boult and Wieland 2010; Salive 2013; Suls et al. 2016). Upwards of 80 million individuals in the US are expected to have multiple health conditions by 2020, and approximately two-thirds of health care dollars in the US are spent on these patients (Suls et al. 2016). Accordingly, multimorbidity is shaping the delivery of health care and services now more than ever, presenting clinicians with a variety of challenges in providing optimal patient care geared toward combinations of patient health conditions (Tinetti and Studenski 2011). Meanwhile, epidemiologists increasingly are moving toward examining multimorbidity rather than singular conditions, in order to more accurately delineate and understand the complex sources of health vulnerability and risk in the population (Suls et al. 2016).
Despite its clear and growing relevance to clinical care and public health, multimorbidity remains poorly understood in the context of informal elder caregiving. Clinically, patient multimorbidity often manifests as a provider network spanning primary care as well as diverse specialists such as orthopedists, oncologists, cardiologists and endocrinologists, with primary care physicians often serving as “quarterbacks” in the coordination and delivery of complex patient care across providers (Tinetti et al. 2016). Outside of a clinical context, however, it remains unclear whether and how informal elder caregiving networks might reflect or address the needs of individuals with multimorbidity. In many ways, chronic conditions dictate the specific daily and long-term health needs of care recipients (Gross et al. 2007; Stanton et al. 2007), and thus should carry profound consequences for the formation and functioning of care networks. Clinical and epidemiological research already have demonstrated that treatment regimens for multimorbidity are unique and are not simply reducible to singular conditions such as osteoporosis, cancer, dementia or heart disease (Salive 2013; Suls et al. 2016), suggesting that informal care may also reflect combinations or synergies among recipient health problems.
The increasing number of older adults with multimorbidity combined with broader social and economic changes in the US has likely increased demands on family members, making them more likely to outsource care. Care networks may be becoming larger and more of a mixture of kin, non-kin, and formal caregivers. Kin such as spouses or adult children usually shoulder most of the burden of informal care, but kin care is becoming more precarious. “Sandwiched” caregivers are trying to raise children in a nation that offers no guaranteed paid parental leave benefits at the same time as they provide care informally for their own ailing parents (Pines, Neal, Hammer and Icekson 2011). Meanwhile, these caregivers often try to hold down full-time careers, not only for purposes of self-fulfillment but also for purposes of economic security for themselves and their families in the face of recent market volatility and downturns. Being overwhelmed across multiple roles may lead to the recruitment of additional caregivers who can fill in gaps in instrumental help. Having multiple caregivers is not uncommon, especially for those recipients who have substantial health limitations or who have constrained access to kin help (Aneshensel et al. 1995; Freedman and Spillman 2014).
However, networks of elder care remain poorly characterized across diverse recipient morbidities or increasing morbidity count (Carpenter and Ducharme 2003; Freedman and Spillman 2014; Koehly et al. 2015; Kwak et al. 2013). Important and timely knowledge gaps are situated at the intersection of multimorbidity and informal caregiving. Identifying who cares and the social network contexts in which informal care unfolds for multiple chronic health conditions represents a concrete and relevant objective for understanding the present and future of informal care in America. Population aging, extensions in longevity for many population groups, and the multiple role involvements of informal caregivers will only continue to increase the broad policy relevance of networked informal caregiving for multimorbidity in the coming decades.
Key Determinants of Care Network Composition: Morbidity and Gender
Following core findings on informal elder caregiving, close family members such as spouses or adult children typically are the ones to take on caregiving demands, and often mostly by themselves (Aneshensel et al. 1995; Pavalko 201l). At the same time, however, care networks may often reflect contingencies linked to specific health conditions. For instance, kin may assist in caring for acute and debilitating conditions such as cancer, dementia, or stroke, whereas less severe conditions like arthritis may be handled more easily by routine non-kin or formal caregivers (Kim and Schulz 2008; Pinquart and Sörensen 2011).
In addition, recipient gender is likely to structure informal care networks. Men tend to have smaller caregiving networks than women more generally, making them more reliant on spousal care (Moen and Spencer 2011; Pinquart and Sörensen 2011). Meanwhile, not having a living spouse due to premature male mortality is likely to carry consequences for women's informal care networks, such that they may have to rely more extensively on non-spousal kin such as adult children, or on non-kin or formal care. Moreover, prevalence estimates for most chronic health conditions are higher for women than for men (Stanton et al. 2007), suggesting that women may have more varied or intense health needs than men, thereby reinforcing a need among women for larger or more diverse informal care networks.
In general, women tend to have larger emotional and instrumental social support networks than men across a variety of social settings. Men and women have been shown to differ systematically in terms of how they recruit and maintain support in the face of personal health stressors, with women typically showing more robust support formation tendencies than men as a means of coping with major health-related needs and stressors (Taylor and Stanton 2007). Altogether, women's care networks should be both larger and more diverse compared to men's, and should be more responsive to chronic health challenges than men's.
Hypothesis 1 (Gender and Care Network Size and Diversity)
Men's care networks will be smaller and less diverse than women's.
Hypothesis 2 (Gender, Morbidity, and Care Networks)
Men's care networks will be less affected by multimorbidity than women's.
Relating Care Networks to Recipient Psychological Well-Being
In addition to characterizing informal care networks across gender and morbidity count, understanding how complex care networks relate to recipient well-being is an important priority. Because social integration is a known cornerstone of psychological well-being (Cohen and Wills 1985; Thoits 2011), and because informal care networks represent a primary, routine form of social integration for care recipients, network structures may bear large associations with recipient psychological well-being. While much research has been directed at understanding threats to psychological well-being that informal caregivers face, comparatively less research has been directed at understanding the psychological well-being of care recipients themselves, likely because recipients' physical or health limitations that necessitate informal caregiving in the first place tend to be conflated with their psychological well-being (Ejem et al. 2015; Kwak et al. 2013; Lin and Wu 2011; Malhotra et al. 2016). In contrast to physical health conditions, psychological well-being specifically represents ongoing social, cognitive, and emotional processes that can independently shape the prognosis of physical health conditions by influencing how care recipients are motivated to treat or cope with their acute and chronic health challenges and limitations (Bayliss et al. 2007; Lin and Wu 2011; Taylor and Stanton 2007).
Larger care networks may either help or hinder recipient psychological well-being. If, on average, accumulation of caregivers occurs because it represents a rational response to increasing recipient care needs, then recipient psychological well-being should increase with network size due to support needs being better met. Alternatively, if the accumulation of caregivers shapes or reflects inefficiency or conflict between caregivers, recipient psychological well-being may be lower in such networks. For instance, larger networks may arise when caregivers do not communicate well with each other or have issues coordinating care among themselves.
Of course, these mechanisms are not strictly exclusive, and observed patterns in recipient well-being may reflect greater instrumental support at the same time that they reflect inefficiency or suboptimal coordination among caregivers. Moreover, larger networks may represent a rational response to barriers to care provision, such as geographic separation between family members or inflexible work schedules of potential care providers, which may or may not impact conflict or miscommunication among multiple caregivers.
Because it is not clear from previous research whether care network size represents a predominantly rational response to care needs or is predominantly an indication or cause of inadequate care provision, we propose the following competing hypotheses for recipient psychological well-being:
Hypothesis 3a (Network Size as Rational Response)
Larger care networks will be associated with higher levels of recipient psychological well-being.
Hypothesis 3b (Network Size and Inadequate Care)
Larger care networks will be associated with lower levels of recipient psychological well-being.
It also is unclear whether larger care networks tend to be composed of certain types of caregivers, making network composition important to isolate in any examinations of network size and recipient psychological well-being. Prior work has shown that caregiving performed by kin, such as spouses, siblings, or adult children, may contribute positively to care recipient well-being, depending on the quality, extent and nature of instrumental kin help (e.g., Djundeva et al. 2014; Kim et al. 2008; Kwak et al. 2013; Wolff and Agree 2004). However, non-kin and formal caregiving may fill unique needs that kin caregiving cannot. It may be the case that care recipients feel happier when they know their family members are being supported and that they are not placing too much burden on a particular loved one. Further, non-kin or formal care may save people from the awkwardness of family members having to help with activities of daily living like bathing. However, provision of non-kin or formal help in place of kin care may violate cultural expectations about task-specific provisions by family members or hierarchical deployment of help according to degree of biological relatedness (Cong and Silverstein 2009; Litwak et al. 2003), potentially undermining recipient well-being by instilling a sense of resentment, anger, or loneliness.
Regardless of these network compositional aspects, we maintain that care network size will be important to understanding differences in care recipient psychological well-being. Specifically, for reasons stated earlier regarding rational care response or care inadequacy associated with growing network size, we maintain that care network size will still be related to recipient psychological well-being, even after controlling or adjusting for network composition.
Hypothesis 4 (Robustness of Network Size and Recipient Well-Being)
Associations between care network size and recipient psychological well-being will hold after adjusting for kin, non-kin and formal care network composition.
Competing Perspectives on Multimorbidity and Care Recipient Psychological Well-Being
While we expect to observe associations between care network size and recipient well-being, we also expect that these associations may be fundamentally shaped or moderated by multimorbidity. Multimorbidity is one general index of the overall degree and severity of health problems. From a network coordination perspective, multimorbidity is likely to increase any associations between care networks and recipient well-being. Multimorbidity determines the overall volume and nature of recipient health needs that networks need to handle effectively in order to ensure recipient psychological well-being. As multimorbidity becomes more severe, the consequences or stakes of care network operation for recipient psychological well-being should also increase, as any faults or inefficiencies in the network likely will be more consequential for recipients' ongoing levels of well-being.
In contrast, from a stress buffering perspective (Pearlin 2010; Thoits 2011), care networks should reduce associations between multimorbidity and recipient psychological well-being, by offering emotional and instrumental resources to offset personal health challenges. That is, this perspective focuses on the moderating or buffering potential of networks themselves, rather than the moderating capacity of multimorbidity. Care networks represent social support that may buffer acute and chronic personal health stressors triggered by multimorbidity. Larger or more extensive care networks may be more effective at buffering care recipient stress than smaller networks, due to their greater potential capacity to provide support.
These two perspectives are tested by a statistical interaction term between care network size and multimorbidity in the prediction of recipient psychological well-being. If a network coordination perspective is predominantly supported, increasing morbidity count should strengthen associations between recipient psychological well-being and care network size. If a stress buffering perspective is predominantly supported, increasing care network size should weaken associations between more multimorbidity and less psychological well-being.
Hypothesis 5a (Network Operational Perspective)
Multimorbidity will increase the association between care network size and recipient psychological well-being.
Hypothesis 5b (Stress Buffering Perspective)
Greater care network size will diminish the association between greater multimorbidity and recipient lower psychological well-being.
The overall conceptual model for this paper is diagrammed in Figure 1.
Figure 1. Proposed Associations among Key Concepts in Study.
Methods
Data
We draw on the first wave of the National Health and Aging Trends study (NHATS), collected in 2011, to analyze interrelationships among multimorbidity, care network size and diversity, and care recipient psychological well-being. NHATS is a national sample of Medicare beneficiaries aged at least 65, conducted by the Bloomberg School of Public Health at Johns Hopkins University. Older individuals and African-Americans are oversampled. While the NHATS allows for proxy respondents in cases of health or ability limitations (e.g., illness or cognitive impairment), we focus here on those who provided data on their own circumstances (i.e. “sample persons”; about 90% of original sample) so that recipient well-being is self-reported and so that samples are consistent across all analyses. This restriction generally screens out individuals with severe dementia or other cognitive disabilities that prevent survey participation.
Care Recipient Psychological Well-Being:Depression and Anxiety Symptoms
NHATS administered short screening instruments for frequency of depression and anxiety symptoms (PHQ-2 and GAD-2, respectively). Both instruments are commonly used in studies of community and public health to assess mental health symptomatology (Kroenke et al. 2009). The PHQ-2 asks how often during the last month the respondent “had little interest or pleasure in doing things” or “felt down, depressed, or hopeless,” while the GAD-2 asks how often the respondent “felt nervous, anxious, or on edge” or has “been unable to stop or control worrying” (1=not at all, 2=several days, 3=more than half the days, 4=nearly every day). To obtain frequency measures of depressive and anxiety symptoms, we sum items within scales (scale min=2, scale max=8).1
Care Network Size and Composition and Intensity of Care
Each NHATS respondent is asked whether they receive help for mobility, self-care, household tasks, medical care or transportation, and to identify and state relationships of each person who provides such help. This roster-style helper assessment provides a conventional identification of informal caregiving, as it focuses whether instrumental help is provided for the respondent and by whom. For each identified helper, intensity of care also is assessed, in terms of number of hours of help provided per day. The total care network size is calculated as the total number of helpers for each respondent, and total number of kin, non-kin and formal caregivers is computed based on stated relationships. Hours of total and kin, non-kin and formal help per day are computed likewise.
Care Recipient Variables: Health Conditions
Respondents reported whether a doctor had ever diagnosed them with a variety of diseases or conditions (yes or no; heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, dementia or Alzheimer's disease, or cancer). We use responses to these items to determine the overall count of major health conditions for each care recipient, and to determine the most prevalent multimorbidities in the overall NHATS sample. Although self-reported ever-diagnosis, as queried in NHATS, does not technically capture current diagnosis, the diseases or conditions examined here tend to be associated with underlying related health complications that persist even when symptoms subside to subclinical levels.
Regression Control Variables: Recipient Sociodemographic and General Health Characteristics
Across our analyses of care networks and recipient psychological well-being, we adjust for recipient sociodemographic characteristics and a variety of general physical health indicators, to ensure patterns hold across basic demographic groups and to reduce confounding due to severe or specific health conditions.
Sex is measured as a binary variable (male or female); age is queried in terms of age ranges (imputed using midpoints to produce a continuous measure of years); racial status is measured here as a binary variable (white vs. non-white primary race, due to limited detail in NHATS racial/ethnic identification questions); and educational attainment is measured in terms of year ranges (imputed using midpoints to produce a continuous measure of years).
Marital status is ascertained by NHATS as well. However, marital status is not used as a control variable in the analyses presented due to its substantial overlap with care network size and kin network size in particular. Additional analyses controlling for marital status produced the same substantive findings regarding the study hypotheses.
In terms of general health characteristics, we also control for self-rated ill-health (“Would you say that in general your health is 1=excellent, 2=very good, 3=good, 4=fair, or 5=poor?”) and for whether the respondent reports any severe health conditions not included in the multimorbidity count (1=yes, 0=no). Including additional physical health control variables, such as recent hospitalization or activity limitations, led to the same general findings and upheld the substantive results (available on request).2
Analytic Plan
Our analyses comprise a series of multivariate regression models. These models test each of the hypotheses proposed earlier. All regressions are estimated with robust standard errors and control for recipient sociodemographic and general health characteristics.
First, we conduct regressions to determine associations between gender and informal care network composition. In these models, we assess associations between gender and care network size and diversity (total number of caregivers, total hours of care/day across network, number of kin caregivers, presence of non-kin caregiver, presence of formal caregiver). We consider both the main effect of gender and the interaction of gender with morbidity count in predicting care network aspects (Hypotheses 1 and 2).
The second set of regression models estimates associations of recipient psychological well-being (depression or anxiety) with care network size and morbidity count. In a first model, psychological well-being is regressed on morbidity count and number of caregivers (Hypotheses 3a, 3b; Network Size as Rational Response or Inadequate Care). A second model controls for the type of care provided (proportion kin, non-kin and formal) and intensity of care (total care hours/day), thus establishing an estimated net effect of the accumulation of multiple caregivers on recipient well-being independent of who provides care or how often they provide it (Hypothesis 4; Robustness of Network Size and Recipient Well-Being). In a third model, a two-way statistical interaction between morbidity count and number of caregivers is specified (Hypotheses 5a, 5b; Network Operational and Stress Buffering Perspectives).
In additional analyses, care network differences by gender were examined across the ten most common multimorbidities in the NHATS sample (listed in Table 1). These analyses revealed that, within genders, care networks generally are quite similar across particular multimorbidity statuses (tables available on request). Therefore, we focus our presented results on total morbidity count rather than particular morbidity statuses.
Table 1. Descriptive Statistics, National Health and Aging Trends Study (2011).
| Female Respondents (N=4076) | Male Respondents (N=2950) | |||||||
|---|---|---|---|---|---|---|---|---|
| Mean | SD | 95% CI (Mean) | Mean | SD | 95% CI (Mean) | |||
| Morbidity Count (0 to 7) | 2.661 | 1.552 | 2.614 | 2.709 | 2.377 | 1.580 | 2.320 | 2.434 |
| Total Number of Caregivers (0 to 6) | 1.526 | 1.213 | 1.489 | 1.564 | 1.313 | 0.951 | 1.279 | 1.348 |
| Hours of Care/Day (0 to 96) | 4.049 | 6.944 | 3.836 | 4.262 | 4.639 | 7.332 | 4.374 | 4.903 |
| Number of Kin Caregivers (0 to 5) | 1.239 | 1.066 | 1.206 | 1.272 | 1.106 | 0.831 | 1.076 | 1.136 |
| Has Kin Caregiver (0/1) | 0.746 | 0.435 | 0.732 | 0.759 | 0.819 | 0.385 | 0.805 | 0.833 |
| Has Non-Kin Caregiver (0/1) | 0.185 | 0.389 | 0.173 | 0.197 | 0.137 | 0.344 | 0.125 | 0.150 |
| Has Formal Caregiver (0/1) | 0.049 | 0.216 | 0.042 | 0.056 | 0.042 | 0.201 | 0.035 | 0.049 |
| Depression Score (PHQ-2; 2 to 8) | 3.038 | 1.402 | 2.995 | 3.081 | 2.862 | 1.337 | 2.814 | 2.910 |
| Anxiety Score (GAD-2; 2 to 8) | 3.064 | 1.462 | 3.019 | 3.109 | 2.729 | 1.271 | 2.683 | 2.775 |
| Age (Years; 67.5 to 95) | 78.370 | 8.157 | 78.120 | 78.621 | 77.173 | 7.639 | 76.897 | 77.449 |
| White (0/1) | 0.699 | 0.459 | 0.685 | 0.713 | 0.707 | 0.455 | 0.690 | 0.724 |
| Years of Education (0 to 19) | 12.337 | 3.548 | 12.227 | 12.446 | 12.820 | 4.123 | 12.671 | 12.970 |
Note. Overall Ns = 6947 to 7026.
Results
Descriptive Statistics: Morbidity, Caregiving Networks, Psychological Well-Being, Demographics
Table 1 reports descriptive statistics for the 2011 NHATS sample. The average respondent had between 2 and 3 chronic health conditions and between 1 and 2 caregivers, though women reported significantly more conditions as well as more caregivers than did men. However, men received more care hours than women (about half an hour more, on average). And while women reported a greater number of kin caregivers, men were more likely to possess any kin care than were women, which is consistent with men's markedly higher odds of being married in old age (68.0% of men are married, 35.5% of women). Meanwhile, a greater proportion of women reported having a non-kin caregiver, and a greater though not statistically different proportion of women reported having formal care. Thus, overall, women's caregiving networks are larger and more diverse on average than are men's.
Descriptive statistics for respondent psychological well-being (depression and anxiety scores) and demographic factors also are reported. In line with well-known gender differences in mental health reporting and early mortality, women in the NHATS sample report experiencing depressive or anxiety symptoms more often than men, and women are slightly older (just over one year older, on average). Frequencies of depressive and anxiety symptoms are moderately correlated (r = 0.58).
Table 2 summarizes morbidity rates in the NHATS sample by gender, by singular morbidities and then by the most commonly observed multimorbidities. High blood pressure, arthritis, cancer, and diabetes are the most common single conditions across both genders (prevalence > 20% for both women and men). Meanwhile, the most common multimorbidities across both genders are arthritis and high blood pressure, diabetes and high blood pressure, cancer and high blood pressure, arthritis and cancer, and arthritis and diabetes (prevalence > 13% for both women and men).
Table 2. Morbidity Rates in NHATS sample.
| Female (N=4076) | Male (N=2950) | |
|---|---|---|
| NHATS Morbidities | ||
| Heart Attack | 11.77% | 19.63% |
| Heart Disease | 16.21% | 20.29% |
| High Blood Pressure (HBP) | 69.32% | 63.67% |
| Arthritis | 62.90% | 45.45% |
| Osteoporosi | 30.49% | 5.37% |
| Diabetes | 23.93% | 27.13% |
| Lung Disease | 16.39% | 13.67% |
| Stroke | 10.31% | 10.79% |
| Dementia or Alzheimer's | 2.90% | 2.37% |
| Cancer | 22.71% | 29.93% |
| Most Common Multimorbidities | ||
| Arthritis & HBP | 46.63% | 31.58% |
| Diabetes & HBP | 20.28% | 21.13% |
| Cancer & HBP | 16.92% | 20.34% |
| Arthritis & Cancer | 16.62% | 14.60% |
| Arthritis & Diabetes | 15.33% | 13.38% |
| Arthritis, Diabetes, & HBP | 14.83% | 10.85% |
| Arthritis, Cancer, & HBP | 11.55% | 10.30% |
| Arthritis, Diabetes, Heart Disease, & HBP | 3.94% | 4.12% |
| Arthritis, Cancer, Diabetes, & HBP | 3.13% | 3.37% |
| Arthritis, Heart Disease, Cancer, & HBP | 2.59% | 2.83% |
Caregiving Networks by Gender and Morbidity Count
Table 3 summarizes results from regressions of care network characteristics. For each network characteristic, two models are presented. In a first model, main effects of gender and morbidity count are specified (Hypothesis 1; Gender and Care Networks). A second model tests whether accumulating health problems organizes care networks differently for men and women, by statistically interacting gender and morbidity count (Hypothesis 2; Gender, Morbidity and Care Networks). Thus the models examine care network differences linked to accumulating health problems and needs, not worsening overall health.
Table 3. Multivariate Negative Binomial and Logistic Regressions of Care Network Characteristics on Multimorbidity and Gender.
| Total Number of Caregivers (Negative Binomial) | Number of Kin Caregivers (Negative Binomial) | Total Hours/Day (Negative Binomial) | Has Non-Kin Caregiver (Logit) | Has Formal Caregiver (Logit) | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | 1 | 2 | |
| Male | 0.892*** (0.016) | 0.896*** (0.016) | 0.93*** (0.018) | 0.935*** (0.018) | 1.265*** (0.051) | 1.265*** (0.051) | 0.691*** (0.047) | 0.691*** (0.047) | 0.894 (0.109) | 0.907 (0.114) |
| MorbidityCount | 1.048*** (0.007) | 1.059*** (0.008) | 1.048*** (0.007) | 1.061*** (0.009) | 1.081*** (0.014) | 1.094*** (0.019) | 1.036 (0.025) | 1.040 (0.029) | 1.097* (0.045) | 1.113* (0.054) |
| Male × Morbidity Count | 0.974* (0.011) | 0.969** (0.011) | 0.974 (0.023) | 0.988 (0.043) | 0.965 (0.075) | |||||
Note. Exponentiated coefficients are shown. Model type (negative binomial regression or logistic regression) is given in parentheses under outcome. All models adjust for sociodemographic characteristics and general health measures (not shown).
p < .001;
p < .01;
p < .05 (two-tailed)
Model 1 for total number of caregivers shows that men have approximately 11% smaller care networks on average (exponentiated coefficient = 0.892, p < .001), and that each additional health problem translates to about a 5% gain in network size (coefficient = 1.048, p < .001). However, Model 2 reveals that accumulating health problems are more weakly associated with care network size gains for men than they are for women (Male × Morbidity Count = 0.974, p < .05). The top panel of Figure 2 graphs this statistical interaction, based on network size predictions holding sociodemographic and general health control variables at their mean values.
Figure 2. Care Network Size by Respondent Morbidity Count and Gender (2011 NHATS).
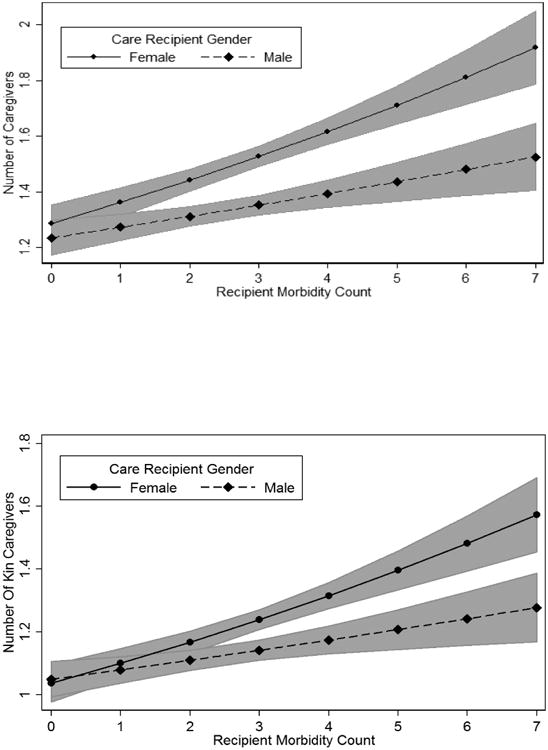
Note. 95% confidence bands are shown in gray.
For total number of kin caregivers, Model 1 documents a 5% increase in the number of kin caregivers for each additional health problem, while men show 7% fewer kin caregivers on average. Model 2 reveals that men exhibit more modest gains in the number of kin caregivers for each additional health problem. The bottom panel of Figure 2 depicts this gender difference.
Model 1 for total hours of care per day reveals that men have 27% greater hour counts on average and that each additional health condition is associated with an 8% increase in care hours. However, Model 2 shows no gender difference in how multimorbidity translates to care hours.
The remaining models for having either a non-kin or formal caregiver show that men have robustly lower odds of non-kin care across differing morbidity counts (31% smaller, on average), but men and women do not differ in their counts of formal caregivers (in line with the prior descriptive results). Accumulating health problems translate to non-kin and formal care equivalently across genders, as shown by the nonsignificant statistical interactions in Model 2.
Overall, Hypothesis 1 (Gender and Care Networks) is supported for total number of caregivers, number of kin caregivers, and having any non-kin care, as these network aspects are either smaller or less common for men than for women. Hypothesis 2 (Gender, Morbidity, and Care Networks) is supported for total number of caregivers and number of kin caregivers, as these network aspects are more weakly associated with increasing morbidity count among men.
Analyzing Respondent Psychological Well-Being: Gender, Multimorbidity and Care Networks
Table 4 presents results from multivariate regressions of respondent psychological well-being. In Model 1 for depressive symptoms (PHQ-2), morbidity count and number of caregivers both are positively associated with more frequent symptoms (p < .001). In Model 2, these associations are robust to controls for network composition and overall number of care hours. A two-way interaction in Model 3 is significant, demonstrating that having multiple caregivers is associated with diminished recipient well-being especially when multimorbidity is present.
Table 4. Multivariate OLS Regressions of Respondent Psychological Well-Being, 2011 NHATS.
| Depressive Symptoms (PHQ-2; N=6870) | ||||||
|---|---|---|---|---|---|---|
| 1 | 2 | 3 | ||||
| b | β | b | β | b | β | |
| Morbidity Count (0-7) | 0.089*** | 0.102 | 0.088*** | 0.101 | 0.085*** | 0.098 |
| Num. of Caregivers (0-6) | 0.102*** | 0.083 | 0.099*** | 0.081 | 0.088*** | 0.072 |
| Caregivers × Morbidity | 0.027** | 0.036 | ||||
| Proportion Kin (0-1) | -0.165*** | -0.050 | -0.136** | -0.041 | ||
| Proportion Non-Kin (0-1) | -0.049 | -0.009 | -0.016 | -0.003 | ||
| Proportion Formal (0-1) | 0.093 | 0.008 | 0.118 | 0.010 | ||
| Total Care Hours/Day | 0.010*** | 0.053 | 0.010*** | 0.051 | ||
| Male | -0.104*** | -0.038 | -0.099** | -0.036 | -0.099** | -0.036 |
| Self-Rated Ill Health (1-5) | 0.348*** | 0.281 | 0.343*** | 0.278 | 0.345*** | 0.279 |
| Other Serious Illness (0/1) | 0.120*** | 0.040 | 0.124*** | 0.041 | 0.128*** | 0.042 |
| Anxiety Symptoms (GAD-2; =6889) | ||||||
| 1 | 2 | 3 | ||||
| b | β | b | β | b | β | |
| Morbidity Count (0-7) | 0.099*** | 0.112 | 0.098*** | 0.111 | 0.094*** | 0.107 |
| Num. of Caregivers (0-6) | 0.125*** | 0.100 | 0.118*** | 0.095 | 0.104*** | 0.083 |
| Caregivers × Morbidity | 0.035*** | 0.046 | ||||
| Proportion Kin (0-1) | -0.094 | -0.028 | -0.057 | -0.017 | ||
| Proportion Non-Kin (0-1) | -0.036 | -0.007 | 0.008 | 0.001 | ||
| Proportion Formal (0-1) | 0.340* | 0.028 | 0.372* | 0.031 | ||
| Total Care Hours/Day | 0.006* | 0.032 | 0.006* | 0.029 | ||
| Male | -0.259*** | -0.092 | -0.257*** | -0.091 | -0.258*** | -0.092 |
| Self-Rated Ill Health (1-5) | 0.304*** | 0.243 | 0.301*** | 0.240 | 0.303*** | 0.241 |
| Other Serious Illness (0/1) | 0.160*** | 0.052 | 0.163*** | 0.053 | 0.167*** | 0.054 |
Note. Unstandardized (b) and standardized (β) estimates are shown. Robust standard errors are given in parentheses. All models also control for sociodemographic characteristics (not shown).
p < .001;
p < .01;
p < .05 (two-tailed)
The top panel of Figure 3 graphs this interaction. Here, having an increasing number of caregivers shows a null marginal linear association with frequency of depressive symptoms when only 0 or 1 chronic health conditions are present (25th percentile of chronic illness in NHATS sample). However, when 3 to 4 health conditions are present (approximately 80th percentile), having more caregivers is linked to more frequent depressive symptoms (slightly more than one third of a standard deviation in moving from zero to four caregivers).
Figure 3. Depressive and Anxiety Symptoms by Size of Caregiver Network and Respondent Morbidity Count (2011 NHATS).
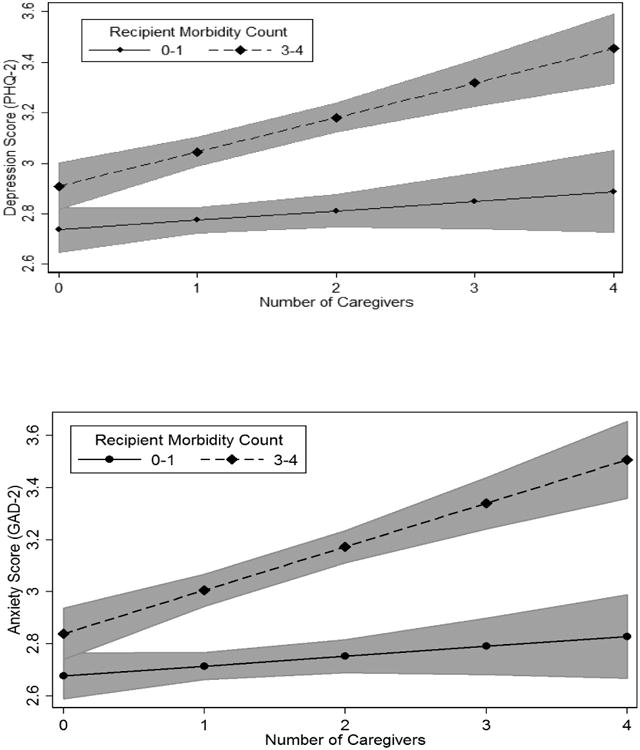
Note. 95% confidence bands are shown in gray.
Models 1-3 for frequency of anxiety symptoms (GAD-2) yield a highly similar set of findings. Morbidity count and number of caregivers show negative associations with frequency of anxiety symptoms, and these associations are robust to network composition controls. Moreover, a two-way interaction between number of caregivers and morbidity count is both positive and significant. The bottom panel of Figure 3 depicts this interaction, showing patterns highly similar to those observed for depression.
Overall, these psychological well-being models lend support to Hypothesis 3b (Network Size and Inadequate Care) and reject Hypothesis 3a (Network Size as Rational Response), given that higher network size is consistently associated with higher frequency of depressive and anxiety symptoms. The models also support Hypothesis 4, as the associations of network size with psychological well-being are robust to additional controls for network composition. Finally, Hypothesis 5a (Network Operational Perspective) is supported and Hypothesis 5b (Stress Buffering Perspective) is rejected, given that well-being is predicted to be lowest for recipients who show multiple chronic conditions and who are embedded in large care networks.
Discussion
Population aging is on the rise, making multimorbidity a prominent organizing factor in the delivery of elder care in America. In this study, we analyzed informal care networks in a national sample of Medicare recipients in the United States. After establishing how care networks vary according to gender and multimorbidity, we examined associations between networks and recipient well-being. Overall, we found that men possess smaller care networks than women on average and are also less likely to possess a non-kin caregiver. While total morbidity count predicted the total number of caregivers and number of kin caregivers in networks, both of these associations were contingent on gender, such that greater multimorbidity significantly translated to larger networks for women only.
Our finding that care networks became larger with increasing morbidity is consistent with prior work in clinical settings that has established positive associations between the complexity of recipient health problems and the complexity of provider networks upon which they must draw in order to meet their daily needs (Boult and Wieland 2010; Tinetti and Studenski 2011). While this literature typically focuses on the complexity of formal care and institutional medical support, we show in these results that this pattern extends to informal care networks as well.
Having established patterns in care network size and composition according to multimorbidity, we then examined the associations between network features and recipient psychological well-being. Our models revealed that recipients with multimorbidity show especially diminished psychological well-being in larger informal care networks. This key finding persisted even with a variety of controls for sociodemographic background, recipient health status or severe health conditions, and network compositional aspects, which suggests that larger networks may in part undermine the psychological well-being of care recipients due to network scaling or coordination issues and not any correlated physical health conditions or particular sources of care. Future research should attempt to explicate how this occurs. As we posited earlier, larger networks may make it increasingly challenging to coordinate multimorbidity care across tasks, individuals, and social settings. With this, such networks may erode a care recipient's sense of mastery or control over their life situation.
Overall, the present study's findings advance several important knowledge frontiers with regard to morbidity and caregiving. First, they reveal the nature and extent of associations between health problems and care network size and diversity, an issue which had been overlooked in prior caregiving research that had analyzed caregiving in terms of overall rates or dyadic care relationships rather than taking a network approach. Moreover, they foreground differences by gender in how networks may form in response to chronic health problems. While gender differences in social support and coping tendencies are well-known, and while gender differences in mortality and spousal caregiving also are well-established, gender differences in care network size and composition had not yet been examined using comprehensive national data. Finally, this study forged a nexus between the literatures on recipient well-being and care networks, by examining associations between well-being and networks both in general and across differing levels of recipient morbidity. By showing that recipient morbidity tends to amplify negative associations between network size and recipient well-being, this study provided preliminary evidence in support of the importance of network coordination for care recipient well-being. That is, rather than serving as a source of stress buffering for recipients, increasing network size may reflect a “pileup” of caregivers around a complex medical situation in which the resources and commitments of multiple individuals are activated – and in which informal delivery of care may be fraught with various difficulties relative to less demanding care situations involving fewer recipient health conditions.
While NHATS collects rich information on basic care network features, a valuable future research direction would involve piecing together how kin and non-kin dynamically work together, or how multiple family members balance care, in the context of various combinations of health conditions. Larger informal networks may indicate greater objective care needs and they may reflect a “pileup” or lack of coordination among caregivers because no one caregiver is doing a satisfactory job. As in clinical care networks, informal care networks may benefit from having a “quarterback” or primary decision-maker (Tinetti et al. 2016). Because multimorbidity status is such a fundamental organizing factor in the delivery of care, future research would be well-served by taking a closer look at network dynamics that are particular to idiosyncratic combinations of health conditions. For example, frameworks such as the social convoy model may help to analyze care roles and duties within a network (e.g., Antonucci and Akiyama 1995).
Another valuable future direction for research would be examining interfaces between practitioner or provider networks and informal care networks more directly, in order to reveal the unique dynamics of coordination that occur across time as different informal caregivers interface with different medical providers, and as caregivers and medical providers continue to interface with each other. Lack of coordination across the network may manifest in setbacks for recipient health, such as poor disease management or inadvertent therapeutic competition among treatment regimes (Lorgunpai et al. 2014).
While the current findings extend gerontological research in a number of ways, they are not without several limitations worth noting. First, while the NHATS data compile a roster of helpers involved in recipient care, these data do not reveal the circumstances or conditions under which caregivers work together. Additional analyses using supplemental NHATS data on the nature of help (i.e. mobility, self-care, household tasks, medical care or transportation) suggested that some forms of help may be more relevant to explaining recipient psychological well-being than others. However, helpers often provided multiple forms of help, as is typical in informal caregiving, making it difficult with these data to establish the particular situations for which network dynamics may be particularly detrimental to recipient well-being. Future research should develop typologies of help provided in order to better measure and analyze interrelationships among forms of help (e.g., Freedman and Spillman 2014), as this may offer an important window into mechanisms behind the current study's findings concerning care networks and recipient psychological well-being.
A second important limitation of this study pertains to the estimation of associations between network size and recipient psychological well-being. Because physical and mental health are intertwined in a number of ways, some of the estimated association between growing network size and heightened depressive or anxiety symptoms in care recipients may be based in health processes not captured by growing morbidity count. To help address this, we controlled for general health status and the presence of any additional severe health problems, and in additional analyses we introduced an extensive suite of additional physical health control variables as well. Altogether, negative associations between network size and diminished well-being were robust, as were statistical interactions between network size and morbidity count in predicting recipient well-being, though these findings did change in magnitude somewhat depending on the physical health controls included in the model. Because our analyses are based in cross-sectional data, we are unable to establish temporal ordering among mental and physical health statuses or processes. Longitudinal analysis would help address this issue, as might experiential or momentary data involving real-time collection of fluctuations in mood over the course of short time frames such as hours, days or weeks.
Finally, these results leave unclear why non-kin and formal care showed different associations with gender than did kin care or total number of caregivers. Specifically, while women showed larger and more diverse care networks on the whole than did men, morbidity count did not shape gender differences in non-kin or formal care, and men and women did not differ with regard to probability of formal care. To some extent, these findings may reflect small observed network sizes, as the gender trends were in the expected directions but did not achieve statistical significance. However, another important possibility to consider is that formal care tends to be more of an obligatory response to severe recipient health problems whereas kin and non-kin care may be recruited more at the discretion of the care recipient, in the absence of any institutional care arrangements.
In conclusion, by continuing to examine care recipient well-being at the intersection of kin and non-kin informal assistance, future work will be poised to reveal how recipient well-being is influenced by common yet understudied networked care arrangements. In such arrangements, family members who are struggling to negotiate barriers of work-family balance and geographic distance, for example, cannot be entirely present or available to help a family member in need. Such care arrangements are routinely encountered in today's society, given the intensification of work-family conflict in a “sandwiched generation” that raises children while caring for parents.
Acknowledgments
Deborah Carr and participants in the session on Caregiver Well-Being at the 2016 Population Association of America (PAA) Annual Meeting in Washington, D.C. provided valuable feedback. M.A. Andersson received support from a postdoctoral fellowship at Yale University and J.K. Monin received support from an NIA K Award (K01 AG042450) and a Yale Pepper Scholar Award (P30 AG21342).
Footnotes
Using a combined depression and anxiety scale (i.e. PHQ-4, which merges the PHQ-2 and the GAD-2) led to similar overall findings, as did using thresholds or cutoffs rather than a continuous measure of symptom frequency. Prior analyses have supported the presence of distinct depression and anxiety factors, so we analyze them separately here (Kroenke et al. 2009).
In additional analyses, we also controlled for particular severe conditions (dementia, cancer, stroke). However, our basic findings remained unchanged. We are only able to control for a limited set of specific conditions in order to maintain statistical independence (i.e. non-collinearity) between these disease indicators and the total morbidity count variable.
Contributor Information
Matthew A. Andersson, Baylor University.
Joan K. Monin, Yale University
References
- Aneshensel CA, Pearlin LI, Mullan JT, Zarit SH, Whitlatch CJ. Profiles in caregiving: The unexpected career. New York: Academic Press; 1995. [Google Scholar]
- Antonucci TC, Akiyama H. Convoys of social relations: Family and friendships within a life span context. In: Blieszner R, Bedford VH, editors. Handbook of Aging and the Family. Westport, CT: Greenwood Press; 1995. pp. 355–371. [Google Scholar]
- Bayliss EA, Ellis JL, Steiner JF. Barriers to self-management and quality-of-life outcomes in seniors with multimorbidities. Annals of Family Medicine. 2007;5:395–402. doi: 10.1370/afm.722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boult C, Wieland GD. Comprehensive primary care for older patients with multiple chronic conditions. JAMA. 2010;304:1936–1943. doi: 10.1001/jama.2010.1623. [DOI] [PubMed] [Google Scholar]
- Carpenter N, Ducharme F. Care-giver network transformations: The need for an integrated perspective. Ageing and Society. 2003;23:507–525. [Google Scholar]
- Cohen S, Wills TA. Stress, social support and the buffering hypothesis. Psychological Bulletin. 1985;98:310–357. [PubMed] [Google Scholar]
- Cong Z, Silverstein M. Intergenerational support and depression among elders in rural China: Do daughters-in-law matter? Journal of Marriage and Family. 2009;70:599–612. [Google Scholar]
- Djundeva M, Mills M, Wittek R, Steverink N. Receiving instrumental support in late parent-child relationships and parental depression. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2014 doi: 10.1093/geronb/gbu136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ejem DB, Drentea P, Clay OJ. The effects of caregiver emotional stress on the depressive symptomatology of the care recipient. Aging & Mental Health. 2015;19:55–62. doi: 10.1080/13607863.2014.915919. [DOI] [PubMed] [Google Scholar]
- Freedman V, Spillman BC. Disability and care needs among older Americans. Milbank Quarterly. 2014;92:509–541. doi: 10.1111/1468-0009.12076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gross CP, McAvay GJ, Guo Z, Tinetti ME. The impact of chronic illnesses on the use and effectiveness of adjuvant chemotherapy for colon cancer. Cancer. 2007;109:2410–2419. doi: 10.1002/cncr.22726. [DOI] [PubMed] [Google Scholar]
- Kim Y, Schulz R. Family caregivers' strains: comparative analysis of cancer caregiving with dementia, diabetes, and frail elderly caregiving. Journal of Aging and Health. 2008;20:483–503. doi: 10.1177/0898264308317533. [DOI] [PubMed] [Google Scholar]
- Koehly LM, Ashida S, Schafer EJ, Ludden A. Caregiving networks—Using a network approach to identify missed opportunities. Journals of Gerontology, Series B: Psychological and Social Sciences. 2015;70:143–154. doi: 10.1093/geronb/gbu111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW, Löwe B. An ultra-brief screening scale for anxiety and depression: The PHQ-4. Psychosomatics. 2009;50:613–621. doi: 10.1176/appi.psy.50.6.613. [DOI] [PubMed] [Google Scholar]
- Kwak M, Ingersoll-Dayton B, Burgard S. Receipt of care and depressive symptoms in later life: The importance of self-perceptions of aging. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences. 2013 doi: 10.1093/geronb/gbt128. [DOI] [PubMed] [Google Scholar]
- Lin IF, Wu HS. Does informal care attenuate the cycle of ADL/IADL disability and depressive symptoms in late life? Journal of Gerontology: Social Sciences. 2011;66B:585–594. doi: 10.1093/geronb/gbr060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Litwak E, Silverstein M, Bengtson VL, Hirst YW. Theories about families, organizations, and social supports. In: Bengtson VL, Lowenstein A, editors. Global aging and challenges to families. New York: Aldine de Gruyter; 2003. pp. 27–53. [Google Scholar]
- Lorgunpai SJ, Grammas M, Lee DSH, McAvay G, Charpentier P, Tinetti ME. Potential therapeutic competition in community-living older adults in the U.S.: Use of medications that may adversely affect a coexisting condition. PLoS One. 2014;9:1–10. doi: 10.1371/journal.pone.0089447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moen P, Spencer D. Converging divergences in age, gender, health, and well-being. In: Binstock RH, George LK, Cutler SJ, Hendricks J, Schulz JH, editors. Handbook of Aging and the Social Sciences. New York: Academic Press; 2011. pp. 127–144. [Google Scholar]
- Malhotra R, Chei CL, Menon E, Chow WL, Quah S, et al. Short-term trajectories of depressive symptoms in stroke survivors and their family caregivers. Journal of Stroke and Cerebrovascular Diseases. 2016;25:172–181. doi: 10.1016/j.jstrokecerebrovasdis.2015.09.012. [DOI] [PubMed] [Google Scholar]
- Pavalko E. Caregiving and the life course: Connecting the personal and the public. In: Settersten RA Jr, Angel JL, editors. Handbook of Sociology of Aging. New York: Springer; 2011. pp. 603–618. [Google Scholar]
- Pearlin LI. The life course and the stress process: Some conceptual comparisons. Journal of Gerontology: Social Sciences. 2010;65B:207–215. doi: 10.1093/geronb/gbp106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pines AM, Neal MB, Hammer LB, Icekson T. Job burnout and couple burnout in dual-earner couples in the sandwiched generation. Social Psychology Quarterly. 2011;74:361–386. [Google Scholar]
- Pinquart M, Sörensen S. Spouses, adult children, and children-in-law as caregivers of older adults: A meta-analytic comparison. Psychology and Aging. 2011;26:1–14. doi: 10.1037/a0021863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salive ME. Multimorbidity in older adults. Epidemiologic Reviews. 2013;35:75–83. doi: 10.1093/epirev/mxs009. [DOI] [PubMed] [Google Scholar]
- Stanton AL, Revenson TA, Tennen H. Health psychology: Psychological adjustment to chronic disease. Annual Review of Psychology. 2007;58:565–592. doi: 10.1146/annurev.psych.58.110405.085615. [DOI] [PubMed] [Google Scholar]
- Suls J, Green PA, Davidson KW. A behavioral framework to address the emerging challenge of multimorbidity. Psychosomatic medicine. 2016;78:281–289. doi: 10.1097/PSY.0000000000000294. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taylor SE, Stanton AL. Coping resources, coping processes, and mental health. Annual Review of Psychology. 2007;3:377–401. doi: 10.1146/annurev.clinpsy.3.022806.091520. [DOI] [PubMed] [Google Scholar]
- Thoits PA. Mechanisms linking social ties and support to physical and mental health. Journal of Health and Social Behavior. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Studenski SA. Comparative effectiveness research and patients with multiple chronic conditions. NEJM. 2011;364:2478–2481. doi: 10.1056/NEJMp1100535. [DOI] [PubMed] [Google Scholar]
- Tinetti ME, Esterson J, Ferris R, Posner P, Blaum CS. Patient priority-directed decision making and care for older adults with multiple chronic conditions. Clinics in Geriatric Medicine. 2016 doi: 10.1016/j.cger.2016.01.012. Advance online publication. [DOI] [PubMed] [Google Scholar]
- Wolff JL, Agree EM. Depression among recipients of informal care: The effects of reciprocity, respect, and adequacy of support. Journals of Gerontology, Series B, Psychological Sciences and Social Sciences. 2004;59:S173–S180. doi: 10.1093/geronb/59.3.s173. [DOI] [PubMed] [Google Scholar]


