Abstract
Background
National rates of lateral epicondylitis and surgical treatment are poorly defined. Disease burden of lateral epicondylitis (LE) continues to increase annually. Further study is necessary to optimize treatment algorithms to reduce associated health-care expenditures.
Questions/Purposes
The purpose of this study is to review the annual incidence of LE, surgical rates, and associated health-care costs in a population setting.
Methods
A national database was queried for LE from 2007 to 2014. Surgical cases were identified and annual rates were recorded. Demographic and epidemiologic data were reported with descriptive statistics, while trends over time were analyzed using linear regression.
Results
Eighty-five thousand three hundred eighteen cases of LE were identified. The annual incidence per 10,000 patients remained constant (p = 0.304). The proportion of diagnoses in patients <65 years decreased (p ≤ 0.002) and ≥65 years increased (p < 0.001) over the study period. One thousand six hundred ninety-four patients (2%) required operative treatment. The annual rate of surgical intervention remained constant (p = 0.623). The proportion of patients <40 years requiring surgery decreased (p < 0.001) as the proportion of patients ≥65 years needing surgery increased (p = 0.003). Total reimbursement for LE procedures during the study period was $7,220,912. Average per-patient reimbursement was $4263. Both annual total reimbursement (p = 0.006) and per-patient reimbursement rates (p = 0.002) significantly increased.
Conclusion
The annual incidence of LE and rate of surgical intervention have remained constant from 2007 to 2014. The proportion of patients over >65 years diagnosed with, and receiving surgical treatment for, LE has significantly increased in recent years. Total reimbursement and average per-patient reimbursement have steadily risen, demonstrating the increasing burden of cost on the health-care system.
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9559-3) contains supplementary material, which is available to authorized users.
Keywords: lateral epicondylitis, tennis elbow, epidemiology, incidence, cost
Introduction
Lateral epicondylitis, or “tennis elbow,” is a degenerative process, most commonly involving the extensor carpi radialis brevis at its origin [5, 10]. It is frequently seen in general and specialist orthopedic practices, with previous studies estimating that it affects 1 to 3% of adults annually [2, 11]. An additional study reported that the overall age- and sex-adjusted incidence of lateral epicondylitis is 3.4 per 1000, with a higher incidence among male and female patients 40 to 49 years old and 50 to 59 years old, respectively [6]. Despite an apparently high annual incidence in these sampled populations, there is limited evidence from a national sample to corroborate these rates.
Generally, treatment begins with conservative management consisting of a combination of nonsteroidal anti-inflammatory drugs, orthotics (including counter-force bracing), eccentric physical therapy regimens, or injections. While conservative treatments are often effective, some patients may eventually require surgical management for recalcitrant cases. Open, arthroscopic, or percutaneous surgical techniques have all been described [1, 2, 6, 10]. Recent data has suggested that the percentage of cases being treated surgically has increased [6]. However, reports of associated health-care costs have been highly variable [7, 8].
With the identified limitations in the available literature, we sought to study national trends in the diagnosis, treatment, and health-care expenditures associated with lateral epicondylitis. The primary purpose of this study was to review the annual incidence of lateral epicondylitis from 2007 to 2014 in a large population setting. Additionally, we analyzed the annual rates of surgical intervention and financial impact of lateral epicondylitis over the study period. We hypothesized that the annual number of lateral epicondylitis diagnoses, rates of surgical intervention, and associated health-care costs would all increase over the course of the study period.
Patients and Methods
An insurance-based database of patient records, the PearlDiver patient record database (www.pearldiverinc.com, Fort Wayne, IN), was utilized for this study. All data is de-identified and anonymous and was thus exempt from Institutional Review Board approval. The database contains data from several different insurers, including both Medicare and a private insurer, Humana. The patients from the present study were all taken from the Humana database within PearlDiver. This particular database was chosen for the present study as it contains patients of all ages, not just patients largely above the age of 65 years as would be found in the Medicare database.
The database contains procedural volumes, basic patient demographics, laboratory data, and prescription drug information, among numerous other data for patients with International Classification of Diseases, 9th Revision (ICD-9) diagnoses and procedures or Current Procedural Terminology (CPT) codes. The database covers patients insured from the years 2007 through the fourth quarter of 2014, and patients can be tracked across all locations (inpatient, outpatient, etc.) throughout the database years. Overall, the database contains approximately 20 million patients with orthopedic diagnoses. The database is maintained on a password-protected server maintained by PearlDiver that was accessed by the senior author. The senior author performed all data queries.
The database was then queried to identify patients carrying a diagnosis of lateral epicondylitis using ICD-9 code 726.32 (lateral epicondylitis) from 2007 to 2014. To prevent duplicative results, patients with multiple diagnoses of lateral epicondylitis were only counted once when the diagnostic code first appeared in their record. Further analysis of this cohort included identification of surgically treated cases of lateral epicondylitis using CPT codes 24350, 24351, 24352, 24354, 24356, 24357, 24358, and 24359 with an associated ICD-9 for lateral epicondylitis (Table 1). For all diagnosed cases, patient demographics were recorded and analyzed including age, gender, and region within the USA. For surgical cases, annual rates were collectively recorded, and the different methods of extensor carpi radialis brevis (ECRB) debridement (open versus arthroscopic) were recorded.
Table 1.
Diagnosis and procedural codes for lateral epicondylitis
| Diagnosis codes | |
| ICD-9-726.32: lateral epicondylitis | |
| Procedural codes | |
| CPT-24350: fasciotomy, lateral or medial (e.g., tennis elbow or epicondylitis) | |
| CPT-24351: fasciotomy, lateral or medial (e.g., tennis elbow or epicondylitis); with extensor origin detachment | |
| CPT-24352: fasciotomy, lateral or medial (e.g., tennis elbow or epicondylitis); with annular ligament resection | |
| CPT-24354: fasciotomy, lateral or medial (e.g., tennis elbow or epicondylitis); with stripping | |
| CPT-24356: fasciotomy, lateral or medial (e.g., tennis elbow or epicondylitis); with partial ostectomy | |
| CPT-24357: tenotomy, elbow, lateral or medial (e.g., epicondylitis, tennis elbow, and golfer’s elbow); percutaneous | |
| CPT-24358: debridement, soft tissue and/or bone, open | |
| CPT-24359: debridement, soft tissue and/or bone, open with tendon repair or reattachment |
The financial burden of lateral epicondylitis was determined using the reimbursement for the Diagnosis-Related Group (DRG) for each procedure. The reimbursement for the DRG is provided by the PearlDiver database directly from the private insurer, Humana. This reimbursement reflects the amount reimbursed by the insurer for the entire episode of care, including surgical costs, surgeon costs, and global period expenses. It does not necessarily include fees for providers or products not associated with the surgical procedure, such as braces or physical therapy. The reimbursement values provided represent the actual amount paid by the insurer, and not the amount billed by the provider/hospital, which allows for a more accurate assessment of the actual financial burden to the health-care system.
Epidemiologic data was then analyzed to report descriptive statistics including number, percentage, mean, median, and ranges where appropriate. The significance of trends in annual procedural rates over time was determined using linear regression. For all statistical comparisons, p < 0.05 was considered to represent statistical significance.
Results
A total of 85,318 patients with a diagnosis of lateral epicondylitis were identified over the study period. While there was a significant increase in the annual incidence from 2007 to 2014 (R 2 = 0.721, p < 0.001), the overall incidence per 10,000 patients in the database remained constant (R 2 = 0.174, p = 0.304) (Table 2). The proportion of male and female patients diagnosed did not significantly change during this period (R 2 = 0.001, p = 0.950). Interestingly, the annual proportion of diagnoses comprised by patients under the age of 65 years significantly decreased (R 2 ≥ 0.822, p ≤ 0.002), while the proportion in those ≥ 65 years significantly increased (R 2 = 0.924, p < 0.001) over the study period (Table 2). Geographically, there was a significant decrease in the incidence of lateral epicondylitis per 10,000 patients in the Midwest (R 2 = 0.611, p = 0.022) and a significant increase (R 2 = 0.731, p = 0.007) in the South (Table 2).
Table 2.
Trends in diagnosis of lateral epicondylitis 2007–2014
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | |||||||||||||||||
| n | 9154 | 9497 | 9532 | 9707 | 10,012 | 10,786 | 11,722 | 14,908 | <0.001 | ||||||||
| Incidence per 10,000 patients | 14.5 | 13.8 | 15.2 | 16.4 | 15.3 | 15.0 | 14.9 | 15.5 | 0.304 | ||||||||
| Gender | |||||||||||||||||
| Female | 4707 | (51.4%) | 4848 | (51.0%) | 4740 | (49.7%) | 5031 | (51.8%) | 5184 | (51.8%) | 5430 | (50.3%) | 5925 | (50.5%) | 7659 | (51.4%) | 0.950 |
| Male | 4447 | (48.6%) | 4649 | (49.0%) | 4792 | (50.3%) | 4676 | (48.2%) | 4828 | (48.2%) | 5356 | (49.7%) | 5797 | (49.5%) | 7249 | (48.6%) | |
| Age (years) | |||||||||||||||||
| <25 | 155 | (1.7%) | 177 | (1.9%) | 170 | (1.8%) | 154 | (1.6%) | 122 | (1.2%) | 156 | (1.4%) | 126 | (1.1%) | 150 | (1.0%) | 0.002 |
| 25–39 | 1171 | (12.8%) | 1126 | (11.9%) | 1038 | (10.9%) | 927 | (9.5%) | 861 | (8.6%) | 917 | (8.5%) | 937 | (8.0%) | 1100 | (7.4%) | <0.001 |
| 40–64 | 6135 | (67.0%) | 6170 | (65.0%) | 6071 | (63.7%) | 5826 | (60.0%) | 5917 | (59.1%) | 6320 | (58.6%) | 6496 | (55.4%) | 8643 | (58.0%) | <0.001 |
| ≥65 | 1693 | (18.5%) | 2024 | (21.3%) | 2253 | (23.6%) | 2800 | (28.8%) | 3112 | (31.1%) | 3393 | (31.5%) | 4163 | (35.5%) | 5015 | (33.6%) | <0.001 |
| Region (incidence per 10,000 patients) | |||||||||||||||||
| Northeast | 1.8 | 2.3 | 3.5 | 4.4 | 3.3 | 3.0 | 3.9 | 3.9 | 0.067 | ||||||||
| Midwest | 16.8 | 15.9 | 16.1 | 17.4 | 16.0 | 14.3 | 14.7 | 14.0 | 0.022 | ||||||||
| West | 9.8 | 9.7 | 11.6 | 12.9 | 11.0 | 11.1 | 9.7 | 9.0 | 0.627 | ||||||||
| South | 16.6 | 15.5 | 16.8 | 18.0 | 17.6 | 17.9 | 17.8 | 19.2 | 0.007 | ||||||||
Of the diagnosed cases, 1694 (2%) required operative treatment. The annual number of procedures performed significantly increased (R 2 = 0.642, p = 0.017) over the study duration (2007–2014); however, this matched the growth in diagnoses, as the annual proportion of diagnosed cases proceeding to surgery remained constant (R 2 = 0.043, p = 0.623) (Table 3). The proportion of male and female patients undergoing surgical intervention did not significantly change (R 2 = 0.463, p = 0.063). Similar to the diagnostic trends, the proportion of patients undergoing surgery represented by patients under the age of 40 years significantly decreased over the observation period (R 2 = 0.932, p < 0.001), while the proportion represented by patients over the age of 65 years significantly increased (R 2 = 0.796, p = 0.003) (Table 3). There were no significant changes in regional procedural rates (R 2 < 0.192, p > 0.277). Lastly, there did not appear to be any significant change in the rates of open or arthroscopic treatment (R 2 < 0.40, p > 0.169) (Table 3).
Table 3.
Trends in surgery for lateral epicondylitis 2007–2014
| 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | p | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Overall | |||||||||||||||||
| n | 171 | 178 | 234 | 193 | 198 | 233 | 223 | 264 | 0.017 | ||||||||
| Percent of diagnosed | 1.9% | 1.9% | 2.5% | 2.0% | 2.0% | 2.2% | 1.9% | 1.8% | 0.623 | ||||||||
| Gender | |||||||||||||||||
| Female | 102 | (59.6%) | 103 | (57.9%) | 130 | (55.6%) | 96 | (49.7%) | 111 | (56.1%) | 122 | (52.4%) | 115 | (51.6%) | 141 | (53.4%) | 0.063 |
| Male | 69 | (40.4%) | 75 | (42.1%) | 104 | (44.4%) | 97 | (50.3%) | 87 | (43.9%) | 111 | (47.6%) | 108 | (48.4%) | 123 | (46.6%) | |
| Age (years) | |||||||||||||||||
| <40 | 28 | (16.4%) | 27 | (15.2%) | 29 | (12.4%) | 23 | (11.9%) | 21 | (10.6%) | 20 | (8.6%) | 20 | (9.0%) | 22 | (8.3%) | <0.001 |
| 40–64 | 137 | (80.1%) | 139 | (78.1%) | 190 | (81.2%) | 155 | (80.3%) | 144 | (72.7%) | 179 | (76.8%) | 169 | (75.8%) | 202 | (76.5%) | 0.121 |
| ≥65 | 6 | (3.5%) | 12 | (6.7%) | 15 | (6.4%) | 15 | (7.8%) | 33 | (16.7%) | 34 | (14.6%) | 34 | (15.2%) | 40 | (15.2%) | 0.003 |
| Region (incidence per 100,000 patients) | |||||||||||||||||
| Northeast | 0.8 | 0.2 | 1.5 | 0.3 | 0.7 | 0.9 | 0.6 | 0.8 | 0.918 | ||||||||
| Midwest | 3.3 | 2.5 | 4.2 | 3.3 | 2.8 | 3.6 | 2.9 | 2.4 | 0.438 | ||||||||
| West | 2.0 | 1.9 | 3.2 | 3.4 | 1.6 | 2.4 | 1.4 | 1.6 | 0.370 | ||||||||
| South | 2.9 | 3.2 | 3.8 | 3.6 | 3.8 | 3.6 | 3.5 | 3.4 | 0.277 | ||||||||
| Surgical approach | |||||||||||||||||
| Open | 164 | (95.9%) | 171 | (96.1%) | 226 | (96.6%) | 184 | (95.3%) | 192 | (97.0%) | 217 | (93.1%) | 204 | (91.5%) | 252 | (95.5%) | 0.169 |
| Arthroscopic | 12 | (7.0%) | 9 | (5.1%) | 14 | (6.0%) | 12 | (6.2%) | 6 | (3.0%) | 20 | (8.6%) | 24 | (10.8%) | 18 | (6.8%) | 0.327 |
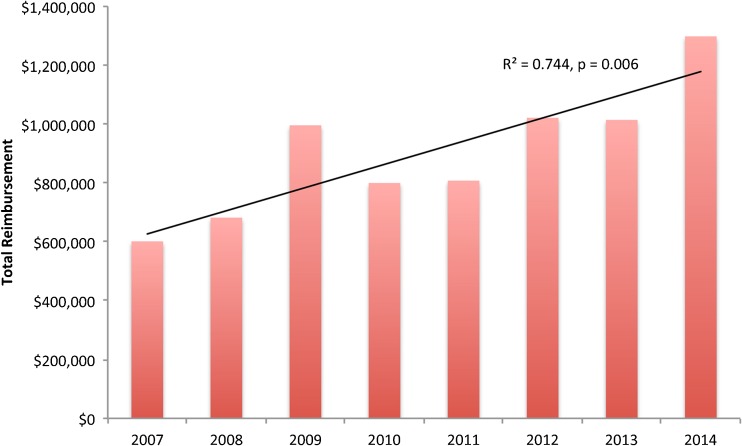
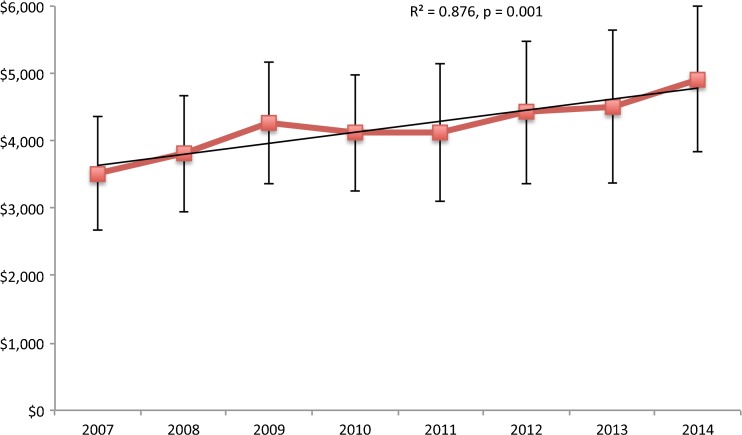
Reviewing the associated procedural cost and health-care burden, total reimbursement during the study period was $7,220,912. The average annual total reimbursement was $902,614. Average per-patient cost for the entire cohort was $4263. More specifically, the average per-patient reimbursement for open surgery was $4203, while the average per-patient reimbursement for arthroscopic surgery was $5190. Comparing annual expense trends, there was a significant increase in both annual total reimbursement (R 2 = 0.744, p = 0.006) (Fig. 1) and annual per-patient reimbursement (R 2 = 0.876, p = 0.002) (Fig. 2).
Fig. 1.
Total annual reimbursement for lateral epicondylitis surgery from 2007 to 2014.
Fig. 2.
Annual per-patient reimbursement for lateral epicondylitis surgery from 2007 to 2014.
Discussion
While highly prevalent in both general and subspecialty orthopedic clinics, particularly among injured workers, the incidence of lateral epicondylitis in a national setting has not been well defined. Similarly, the rates of surgical intervention and associated health-care-related costs are poorly quantified. In our review of over 85,000 cases of lateral epicondylitis from a national database, we identified a relatively constant annual incidence (average 15.1 cases/10,000 patients), and contrary to our hypothesis, the proportion of cases treated surgically remained steadily low (2%). Lastly, the procedural costs and associated disease burden were both found to have increased, with a significant increase in annual total and per-patient reimbursement rates.
There are several limitations of this study, most of which are inherent to the utilization of a large-scale national administrative database. The purported power of the analysis relies on the accuracy of procedural coding within the database. Thus, miscoding and noncoding by physicians and other providers are potential sources of error, jeopardizing the validity of our results. Additionally, while this study aims to provide a representative cross-sectional analysis of the USA, only data from a single insurer was included, and the results might not be truly reflective of the entire population. Lastly, if a diagnosis or procedure did not properly have laterality coded, it was excluded, which could have lead to an underestimation of lateral epicondylitis (LE) diagnosis or surgical intervention rates.
Prior to this work, the majority of epidemiologic reports on the incidence of lateral epicondylitis stemmed from single-institution reports or smaller case series with smaller sample sizes. The majority of these studies reviewed high-risk populations, such as injured workers, and grossly overestimate population rates of lateral epicondylitis. One large sample study was performed by Sanders et al., reporting on the incidence of lateral epicondylitis in a subset of patients (n = 576) from a population database in Olmstead County, MN, from 2000 to 2012 [6]. They identified an annual incidence of approximately 34 cases/10,000 patients, with a significant decrease in annual incidence over time (from 45 to 24 cases per 10,000 patients). These rates are moderately higher than those identified in our cohort (average 15.1 cases/10,000 patients). The reasons for this are likely multifactorial; however, our study identified regional variation with a relatively higher incidence in the Midwest, potentially explaining this discrepancy. Interestingly, Sanders et al. also identified a higher incidence of epicondylitis among patients under the age of 40 years [6], in contrast to the results identified here, where rates in patients <65 years old decreased in conjunction with an increase in the proportion of diagnoses in patients ≥65 years of age. This discrepancy may result from a smaller, biased sample, which may not be completely reflective of national trends.
The rate of surgical intervention following a diagnosis of lateral epicondylitis has also varied significantly between published studies. With the use of a national database, we identified a 2% rate of surgical intervention, with no appreciable change in the annual proportion of cases managed surgically (range 1.8–2.5%, p = 0.623). This rate is lower than what has previously been reported in cohort studies. Knutsen et al. were among the first to attempt to quantify surgical intervention rates. They reviewed 580 patients diagnosed with lateral epicondylitis at their institution [4]. They identified an operative rate of approximately 16%, identifying a number of patient-specific risk factors for requiring surgical intervention, including symptom duration of >12 months, presence of an active worker compensation claim, concomitant radial tunnel syndrome, and previous orthopedic surgery. An additional study by Kachooie et al. reviewed a larger database from 3 academic institutions, identifying 5964 cases of LE, and reported a 4% rate of surgery within 12 months of initial presentation [3]. However, among included care providers in this study, there was significant variability in practice patterns with surgical rates ranging from 0 to 22% of cases encountered. Similar to the collective surgical intervention rate reported by Kachooie et al., Sanders et al. reviewed 931 cases of LE treated at their institution and reported a surgical incidence of 4% [7]. They separately reviewed an additional 576 patients, where they reported a significant increase in surgical rates from 1.1% in 2000–2002 to 3.2% after 2009 [6]. As evidenced by the findings of these studies, there is significant heterogeneity in the available literature, which likely relates to the relatively small sample sizes of the respective studies and inclusion of vastly different patient populations. Additionally, the variability between surgeon’s operative rates likely relates to the lack of a comprehensive, standardized treatment algorithm among practitioners. The information presented from this study provides a more accurate representation of national trends in the operative treatment of lateral epicondylitis. This clinical information is helpful for surgeons and patients to better predict the anticipated need for surgical treatment when presenting with lateral epicondylitis, without previously outlined risk factors for requiring surgical treatment.
Finally, the cost associated with the surgical treatment of lateral epicondylitis was also reviewed. We identified an average per-patient cost of $4263. This figure was comparable to previous reports, such as that by Sanders et al., reporting a similar per-patient cost of nearly $4000 in their review of 931 patients [7]. However, we also identified a significant increase in both the average annual total reimbursement and per-patient reimbursement, indicating that the financial burden of LE is likely to continue to grow in future years. To our knowledge, this is the first study to demonstrate an increasingly large financial burden associated with the treatment of lateral epicondylitis. This highlights the need for ongoing study to improve treatment algorithms and identify cost-effective procedures to eliminate unnecessary cost associated with treatment. For example, Solheim et al. performed a comparative analysis of tenotomy versus debridement as treatment for LE [9]. They identified similar improvements with shorter recovery and less time on disability in the debridement group, potentially favoring this strategy as a potential mechanism to reduce the costs associated with treatment and disability. This represents an interesting area for future study.
The annual incidence of lateral epicondylitis per 10,000 patients and corresponding proportion of cases treated surgically per year have not significantly changed from 2007 to 2014. Most notably, the proportion of patients aged greater than 65 years diagnosed with, and receiving surgical treatment for, lateral epicondylitis has significantly increased in recent years. Over time, both the total reimbursement and the average per-patient reimbursement for lateral epicondylitis surgery have steadily risen, demonstrating the increasing burden of cost on the health-care system.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
Conflict of Interest
Ryan M. Degen, MD; Matthew S. Conti, MD; Christopher L. Camp, MD; David W. Altchek, MD; and Brian C. Werner, MD, have declared that they have no conflict of interest. Joshua S. Dines, MD, reports personal fees from Arthrex, Conmed Linvatec, and Ossur, outside the work.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Electronic supplementary material
The online version of this article (doi:10.1007/s11420-017-9559-3) contains supplementary material, which is available to authorized users.
References
- 1.Buchbinder R, Johnston R V, Barnsley L, Assendelft WJ, Bell SN, Smidt N (2011) Surgery for lateral elbow pain. Cochrane Database Syst. Rev. CD003525. [DOI] [PubMed]
- 2.Calfee RP, Patel A, DaSilva MF, Akelman E. Management of lateral epicondylitis: current concepts. J. Am. Acad. Orthop. Surg. 2008;16:19–29. doi: 10.5435/00124635-200801000-00004. [DOI] [PubMed] [Google Scholar]
- 3.Kachooei AR, Talaei-Khoei M, Faghfouri A, Ring D. Factors associated with operative treatment of enthesopathy of the extensor carpi radialis brevis origin. J. Shoulder Elb. Surg. Elsevier Inc. 2016;25:666–670. doi: 10.1016/j.jse.2015.12.019. [DOI] [PubMed] [Google Scholar]
- 4.Knutsen EJ, Calfee RP, Chen RE, Goldfarb CA, Park KW, Osei DA. Factors associated with failure of nonoperative treatment in lateral epicondylitis. Am. J. Sports Med. 2015;43:2133–2137. doi: 10.1177/0363546515590220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nirschl RP, Pettrone FA. Tennis elbow. The surgical treatment of lateral epicondylitis. J. Bone Joint Surg. Am. 1979;61:832–9. doi: 10.2106/00004623-197961060-00005. [DOI] [PubMed] [Google Scholar]
- 6.Sanders TL, Maradit Kremers H, Bryan A. J, Ransom JE, Smith J, Morrey BF (2015) The epidemiology and health care burden of tennis elbow: a population-based study. Am. J. Sports Med. [DOI] [PMC free article] [PubMed]
- 7.Sanders TL, Maradit Kremers H, Bryan AJ, Ransom JE, Morrey BF. Health care utilization and direct medical costs of tennis elbow: a population-based study. Sport. Heal. A Multidiscip. Approach. 2016;8:355–358. doi: 10.1177/1941738116650389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Silverstein B, Welp E, Nelson N, Kalat J. Claims incidence of work-related disorders of the upper extremities: Washington State, 1987 through 1995. Am. J. Public Health. 1998;88:1827–1833. doi: 10.2105/AJPH.88.12.1827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Solheim E, Hegna J, ∅yen J, Inderhaug E. Arthroscopic treatment of lateral epicondylitis: tenotomy versus debridement. Arthrosc. - J. Arthrosc. Relat. Surg. Arthroscopy Association of North America. 2016;32:578–585. doi: 10.1016/j.arthro.2015.10.008. [DOI] [PubMed] [Google Scholar]
- 10.Taylor SA, Hannafin JA. Evaluation and management of elbow tendinopathy. Sports Health. 2012;4:384–93. doi: 10.1177/1941738112454651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Verhaar JA. Tennis elbow. Anatomical, epidemiological and therapeutic aspects. Int. Orthop. 1994;18:263–7. doi: 10.1007/BF00180221. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)