Abstract
Background
Early surgical intervention for hip fractures in the elderly has proven efficacious. However, surgical delays commonly occur in this patient population due to comorbid conditions that put these patients at a high risk for hypotension-related complications of general or neuraxial anesthesia or anticoagulants that delay the safe use of neuraxial anesthesia.
Questions/Purposes
The questions/purposes of this study are (1) to investigate if a fascia iliaca block in conjunction with light to moderate sedation could provide adequate analgesia throughout open surgery for intertrochanteric hip fractures (AO/OTA 31-1) without requiring conversion to general anesthesia with airway support and (2) to assess its perioperative complication profile.
Methods
A retrospective chart review was conducted to identify patients with intertrochanteric hip fractures who underwent anesthesia with a fascia iliaca block over a 1.5-year period.
Results
In the six patients identified, there were no intraoperative conversions to general anesthesia requiring airway support. Additionally, there were no intraoperative complications, no mortalities within 30 days, 2 patients on anticoagulation who required a blood transfusion, and a single patient who developed a postoperative hospital-acquired pneumonia that resolved with an antibiotic course.
Conclusions
In this series of patients, we demonstrate that a fascia iliaca block can reliably be utilized as the primary anesthetic for patients undergoing surgical fixation of intertrochanteric hip fractures, with an acceptable perioperative complication profile. Although concomitant sedation was provided with the block, this anesthesia strategy has the potential to reduce preoperative delays and minimize the overall burden of sedative and anesthetic medications in a geriatric population. These initial findings may serve as a basis for future, higher-quality prospective and comparative studies.
Electronic supplementary material
The online version of this article (10.1007/s11420-017-9582-4) contains supplementary material, which is available to authorized users.
Keywords: intertrochanteric hip fracture surgery, regional anesthesia, fascia iliaca block, high-risk surgical candidates
Introduction
The majority of hip fractures occur in elderly patients with multiple major medical comorbidities. Over 90% of hip fractures occur in patients over 65 years of age [15], and as the current population ages, the incidence of hip fractures is predicted to rapidly increase in the coming years [13, 18]. Perioperative management of these patients is optimized when a multi-disciplinary approach is used [4]. Multiple studies have demonstrated that medical optimization should take place in a timely manner so that patients can return to ambulation and thereby decrease the rate of complications associated with prolonged immobility. Several factors contribute to surgical delay in hip fractures, including the time of admission, medical comorbidities, and use of anticoagulation [5]. Patients admitted with an international normalized ratio (INR) over 2.0 are at an increased risk for delay to surgery and mortality [5, 19].
Neuraxial anesthesia has many benefits as compared to general anesthesia for elderly patients with hip fractures and results in shorter length of stay, decreased postoperative delirium, and less alteration of cardiopulmonary status [12, 16]. Despite these benefits, as many as 40% of patients with hip fractures use anticoagulation regularly [2], which precludes a significant portion from receiving spinal anesthesia. Although there is limited evidence in the literature to guide perioperative management of individuals on anticoagulation [8], it is a common practice to require an INR < 1.5 in order to perform spinal anesthesia. Patients anticoagulated with a reversible medication such as warfarin may be treated with early reversal and later may become candidates for spinal anesthesia. Medications without reversal options, including the antiplatelet agent clopidogrel, should be stopped at least 7 days prior to receiving spinal anesthesia. A delay of this duration is unacceptable for a patient with a hip fracture. Furthermore, in those with severe cardiac comorbidities including pulmonary hypertension (PAH) or aortic stenosis (AS) induction of either neuraxial or general anesthesia (GA) can lead to blood pressure volatility, which can increase the risk of right ventricular failure [6] or coronary hypoperfusion [1], respectively. Given the aforementioned challenges, an alternative anesthesia strategy is necessary. Fortunately, patients presenting with intertrochanteric hip fractures (AO/OTA 31-1) are ideal candidates for peripheral regional anesthesia techniques, as the surgical options for fixation (cephalomedullary nails (CMN) or sliding hip screws (SHS)) require minimal soft tissue dissection through small incisions using fluoroscopic guidance.
The fascia iliaca (FI) block is a type of peripheral regional anesthesia first described over two decades ago [3] consisting of a full or partial blockade of the lateral femoral cutaneous, genitofemoral, femoral, and obturator nerves that traverse the compartment just deep to the fascia of which the block derives its name. The FI block has been described for use as a pain control modality perioperatively, most commonly in the emergency room as a nonnarcotic alternative, [7, 14] or as a part of multimodal pain control postoperatively [17, 20].
The purposes of this study were (1) to investigate whether a FI block in conjunction with light to moderate sedation could provide adequate analgesia throughout open surgery for AO/OTA 31-1 intertrochanteric hip fractures without requiring conversion to GA with airway support and (2) to assess the perioperative and early postoperative complication profile using this technique.
Patients and Methods
After approval from the institutional review board (IRB), a retrospective chart review was conducted at the lead author’s institution, an urban orthopedic hospital, to identify patients with AO/OTA 31-1 who underwent anesthesia with a FI block between June 2014 and December 2015. The requirement of written informed consent was waived by the IRB. A total of six patients were identified, and their medical records were reviewed to ascertain all medical comorbidities—operative details including durations of surgery and anesthesia, intraoperative blood loss estimated based upon surgeon and anesthesiologist observation, conversions to GA with airway support for either oversedation or inadequate analgesia, and any perioperative or in-hospital complications that occurred throughout their hospital stay or related readmissions within 30 days from surgery. Both surgical and medical complications were collected including intraoperative and postoperative blood transfusions, neurovascular injury, hematoma either at the anesthetic site or surgical site, stroke, pulmonary embolus, respiratory failure, myocardial infarction, pneumonia, surgical site infection, urinary tract infection, pressure ulceration, thromboembolic disease, gastrointestinal bleed, Clostridium difficile infection, renal failure, or death. This manuscript is written in accordance with the STROBE guidelines.
The senior author performed the FI block under ultrasound guidance in the operative suite. In each case, the anesthesiologist made the decision to avoid deep GA due to each individual’s comorbid conditions. All patients had either medical comorbidities (severe AS, severe PAH, severe congestive heart failure (CHF)) or were on an anticoagulant that precluded the use of spinal anesthesia on the day of surgery (Table 1). Subsequently, one of four attending orthopedic surgeons at a teaching institution performed the surgical procedure. In all cases, the anesthesia staff was prepared to convert to GA with airway support if necessary.
Table 1.
Summary of individual patient characteristics
| Case | Age/gender | Comorbidities | Contraindication to GA/SA | Time to surgery (days) | Time to discharge (days) | EBL | Complications |
|---|---|---|---|---|---|---|---|
| 1 | 89F | CAD and CHF with an EF of 35–40%, moderate AS, ESRD, and AFib on warfarin | GA—poor cardiac status SA—anticoagulation |
5 | 14 | 200 | 1 unit pRBCs |
| 2 | 92F | CAD with multiple cardiac stents on clopidogrel, mitral and aortic regurgitation, HTN, and HLD. | GA—poor cardiac status SA—use of clopidogrel |
2 | 7 | 100 | None |
| 3 | 82M | HTN, HLD, and CAD with previous MI for which he underwent CABG in addition to cardiac stenting and prostate cancer. An echocardiogram upon admission revealed severe ICM with class III CHF with an EF of 10% | GA—EF 10% SA—poor cardiac status |
1 | 7 | 100 | None |
| 4 | 92F | AFib, CVA, HTN, chronic kidney disease, and breast cancer in remission with previous mastectomy, and severe AS (valve area 0.5 cm2) | GA—severe AS SA—poor cardiac status |
3 | 20 | 100 | On postoperative day 1, she was started on empirically on broad spectrum antibiotics for fevers, leukocytosis, and bibasilar infiltrates on chest radiography concerning for PNA. |
| 5 | 97F | AS s/p failed bovine aortic valve replacement and later a TAVR, HLD, and asymptomatic CHF | GA—severe AS SA—clopidogrel use |
2 | 6 | 50 | 1 unit pRBCs |
| 6 | 86F | HTN, HLD, CAD with cardiac stents, CHF, prior mitral valve replacement, and AS with previous bioprosthesis now with restenosis and an aortic valve area less than 1 cm2 | GA—severe AS SA—poor cardiac status |
1 | 4 | 50 | None |
AFib atrial fibrillation, AS aortic stenosis, CABG coronary artery bypass graft, CAD coronary artery disease, CHF congestive heart failure, CVA cerebrovascular accident, EBL estimated blood loss (mL), EF ejection fraction, ESRD end-stage renal disease, GA general anesthesia, HLD hyperlipidemia, HTN hypertension, MI myocardial infarction, ICM ischemic cardiomyopathy, pRBC 1 unit packed red blood cells, PNA pneumonia, SA spinal anesthesia, TAVR transcatheter aortic valve replacement
The data are reported using descriptive statistics only.
Technique
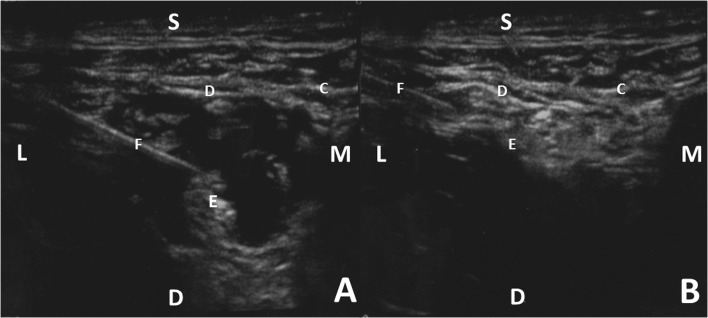
With the patient in the supine position, the operative extremity is draped to expose the inguinal region and superior thigh. After chlorohexidine preparation of the skin, a line is drawn with a marking pen from the anterior superior iliac spine to the pubic tubercle. The starting point is located approximately one third of the way on the line from the anterior superior iliac spine [21]. After placement of the ultrasound probe and identification of the ultrasonic regional anatomy including the fascia lata, fascia iliaca, and femoral artery, a 90-mm 22-gauge needle is advanced through the skin, subcutaneous fat, fascia lata, and just underneath the fascia iliaca. The femoral nerve, hyperechoic when visualized ultrasonically and located adjacent to the femoral artery, is identified just deep to the fascia iliaca (Fig. 1). At this point, approximately 20 mL of a mixture containing 20 mL of 0.5% ropivacaine and 20 mL of 2% lidocaine with 0.005 mg/mL of epinephrine is injected in the region around the femoral nerve (Fig. 2). The needle is then withdrawn laterally but with care to remain deep to the fascia iliaca at which point 10 mL is injected deep to the fascia iliaca (Fig. 2).
Fig. 1.
The relevant anatomy of a FI block.
Fig. 2.
a The infiltration of local anesthesia around the femoral nerve. b The infiltration of local anesthesia deep to the fascia iliaca. S superficial, D deep, M medial, L lateral, C fascia lata, D fascia iliaca, E femoral nerve, F 22-gauge needle.
Following FI block placement, the patient is positioned supine on a fracture table with the ipsilateral leg in traction and the contralateral leg flexed and abducted to facilitate the positioning of the fluoroscopy machine. The incision site is pretreated with 10 mL of 1% lidocaine. At this point, open reduction internal fixation is performed in the standard fashion using either a CMN or SHS. Light to moderate intravenous sedation is helpful, as some parts of the positioning and procedure may cause the patient to experience mild discomfort or pressure. Total doses of medications provided included 1–2 mg of midazolam, 0–50 mcg of fentanyl, and propofol infusions ranging from 0–30 mcg/kg/min.
Results
The six patients included in this case series were admitted to our hospital with an intertrochanteric fracture (AO/OTA 31-A) during an 18-month period between June 2014 and December 2015. The patients ranged in age from 82 to 97 years of age and included five females and one male. Two patients were contraindicated for spinal anesthesia due to recent clopidogrel use, two for severe AS, one for severe PAH, and one for severe CHF who had a documented systolic ejection fraction of 10%. Five patients were treated with CMNs, and one patient was treated with a SHS. The mean time from admission to surgery was 2.3 days (range, 1–5 days). Further details for each case are summarized in Table 1.
All of the patients tolerated their surgical procedures without evidence of pain or perturbation, there were no deviations from the surgical plan, and none of the patients required conversion to general anesthesia with airway support during the operation. A single patient received no supplemental sedative medications during the procedure due to preexisting hypotension.
In regard to safety, there were no intraoperative complications. Postoperatively, one patient developed pneumonia and was treated with a course of antibiotics prior to discharge. Two patients required a unit of packed red blood cells each for acute blood loss anemia. The mean length of stay post-surgery was 7.5 days (range, 3–18 days). All patients were discharged to a subacute rehabilitation facility. There were no hospital readmissions or mortalities within the first 30 days postoperatively.
Discussion
Balancing appropriate medical optimization with the need for early surgical intervention presents a challenge faced by anesthesiologists and orthopedic surgeons when treating patients with hip fractures [10, 11, 23]. When a patient uses clopidogrel, or another irreversible anticoagulant, and has concomitant comorbidities such as AS or PAH, neither spinal anesthesia nor GA is an ideal option. We set out to investigate whether a peripheral regional anesthesia technique, the FI block, with light to moderate sedation could provide adequate analgesia throughout open surgery for AO/OTA 31-1 intertrochanteric hip fractures, without requiring conversion to GA with airway support and to assess its safety perioperatively through an assessment of its complication profile.
In pursuit of these goals, however, this study is most obviously limited by its small sample size and retrospective nature. Additionally, no long-term follow-up is reported, but as the purpose was to investigate an anesthetic technique, the decision was made to focus only on the early perioperative safety and efficacy. Despite these limitations, this series serves as an initial report of using the FI block as the primary intraoperative anesthetic for hip fracture surgery. As preliminary efficacy and safety have been demonstrated in a high-risk patient population, these results can serve as a pilot study for future, higher quality prospective and comparative types of designs.
In our study, no patients undergoing hip fracture surgery required conversion to general anesthesia. Although intravenous sedation was provided throughout the procedure, the overall amounts of anesthetic administered are much lower than would be required for a deep GA with airway assistance. One other study in the literature used a peripheral nerve block technique involving a blockade of both the femoral and lateral femoral cutaneous nerves in conjunction with mild sedation for the surgical treatment of hip fractures [9]. The authors reported a 7.2% conversion rate to GA due to inadequate analgesia provided by their block. Unfortunately, it is difficult to compare this study to ours, because nearly half of the surgeries performed in their cohort were hemiarthroplasties which are more invasive procedures than those in our series. Furthermore, the peripheral nerve block used only anesthetized a portion of the nerves affected by a FI block.
We report three total complications: two transfusions and a single postoperative pneumonia. Excluding transfusions, the complication rate in this high-risk cohort of patients is similar to the 18% complication rate (also excluding transfusions) reported in a recent large database review examining surgically treated hip fractures [22]. In our series, both transfusions occurred in patients who were anticoagulated preoperatively (1 warfarin, 1 clopidogrel). Although the use of a FI block can minimize surgical delays in patients taking anticoagulation medications, surgery before anticoagulant neutralization may involve more intraoperative and postoperative bleeding and thus contribute to a higher transfusion rate. Finally, despite observing no deaths within the first 30 days after surgery in our series, the overall mortality rate in this patient population has been reported to be about 6% at this early time point [9].
In conclusion, in individuals who sustain hip fractures with severe pulmonary and cardiac comorbidities or are on anticoagulants that render them poor candidates for either GA or neuraxial anesthesia, a FI block in conjunction with light to moderate sedation is a unique anesthesia alternative that may result in decreased morbidity by avoiding the complications of GA while expediting surgery. In our small case series, we demonstrate that a FI block (1) can reliably be used as the primary anesthetic for a patient undergoing surgical fixation of intertrochanteric hip fractures and (2) has a perioperative complication profile consistent with similar surgeries performed under GA or neuraxial anesthesia. Anesthesiologists and orthopedic surgeons should be aware of this alternative and consider its use in high-risk hip fracture patients.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
Compliance with Ethical Standards
This protocol was IRB approved on 2/22/2016 at the New York Presbyterian Queens.
Conflict of Interest
Joseph J. Ruzbarsky, MD; Isaac P. Lowenwirt, MD; Elan M. Goldwyn, MD; and Vitaly Kotlyar, MD, have declared that they have no conflict of interest. Elizabeth B. Gausden, MD, has received funding from the Samuel and May Rudin Foundation.
Human/Animal Rights
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008 (5).
Informed Consent
Informed consent was waived from all patients for being included in the study.
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
Footnotes
Level of Evidence: Case series: Level IV
Electronic supplementary material
The online version of this article (10.1007/s11420-017-9582-4) contains supplementary material, which is available to authorized users.
References
- 1.Brown J, Morgan-Hughes NJ. Aortic stenosis and non-cardiac surgery. Contin Educ Anaesth Crit Care Pain. 2005;5(1):1–4. 10.1093/bjaceaccp/mki001.
- 2.Collinge CA, Kelly KC, Little B, Weaver T, Schuster RD. The effects of clopidogrel (Plavix) and other oral anticoagulants on early hip fracture surgery. J Orthop Trauma. 2012;26:568–73. doi: 10.1097/BOT.0b013e318240d70f. [DOI] [PubMed] [Google Scholar]
- 3.Dalens B, Vanneuville G, Tanguy A. Comparison of the fascia iliaca compartment block with the 3-in-1 block in children. Anesth Analg. 1989;69:705–13. [PubMed] [Google Scholar]
- 4.Dy CJ, Dossous PM, Ton QV, Hollenberg JP, Lorich DG, Lane JM. The medical orthopaedic trauma service: an innovative multidisciplinary team model that decreases in-hospital complications in patients with hip fractures. J Orthop Trauma. 2012;26:379–83. doi: 10.1097/BOT.0b013e3182242678. [DOI] [PubMed] [Google Scholar]
- 5.Eardley WG, Macleod KE, Freeman H, Tate A. “Tiers of delay”: warfarin, hip fractures, and target-driven care. Geriatr Orthop Surg Rehabil. 2014;5:103–8. doi: 10.1177/2151458514532469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Forrest P. Anaesthesia and right ventricular failure. Anaesth Intensive Care. 2009;37:370–85. doi: 10.1177/0310057X0903700314. [DOI] [PubMed] [Google Scholar]
- 7.Foss NB, Kristensen BB, Bundgaard M, Bak M, Heiring C, Virkelyst C, Hougaard S, Kehlet H. Fascia iliaca compartment blockade for acute pain control in hip fracture patients: a randomized, placebo-controlled trial. Anesthesiology. 2007;106:773–8. doi: 10.1097/01.anes.0000264764.56544.d2. [DOI] [PubMed] [Google Scholar]
- 8.Gleason LJ, Friedman SM. Preoperative management of anticoagulation and antiplatelet agents. Clin Geriatr Med. 2014;30:219–27. doi: 10.1016/j.cger.2014.01.013. [DOI] [PubMed] [Google Scholar]
- 9.Johnston DF, Stafford M, McKinney M, Deyermond R, Dane K. Peripheral nerve blocks with sedation using propofol and alfentanil target-controlled infusion for hip fracture surgery: a review of 6 years in use. J Clin Anesth. 2016;29:33–9. doi: 10.1016/j.jclinane.2015.10.012. [DOI] [PubMed] [Google Scholar]
- 10.Juliebo V, Krogseth M, Skovlund E, Engedal K, Wyller TB. Medical treatment predicts mortality after hip fracture. J Gerontol A Biol Sci Med Sci. 2010;65:442–9. doi: 10.1093/gerona/glp199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40:692–7. doi: 10.1016/j.injury.2009.01.010. [DOI] [PubMed] [Google Scholar]
- 12.Luger TJ, Kammerlander C, Luger MF, Kammerlander-Knauer U, Gosch M. Mode of anesthesia, mortality and outcome in geriatric patients. Z Gerontol Geriatr. 2014;47:110–24. doi: 10.1007/s00391-014-0611-3. [DOI] [PubMed] [Google Scholar]
- 13.Morris AH, Zuckerman JD, AAOS Council of Health Policy and Practice, USA. American Academy of Orthopaedic Surgeons. National consensus conference on improving the continuum of care for patients with hip fracture. J Bone Joint Surg Am. 2002;84-A:670–4. [DOI] [PubMed]
- 14.Mouzopoulos G, Vasiliadis G, Lasanianos N, Nikolaras G, Morakis E, Kaminaris M. Fascia iliaca block prophylaxis for hip fracture patients at risk for delirium: a randomized placebo-controlled study. J Orthop Traumatol. 2009;10:127–33. doi: 10.1007/s10195-009-0062-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.National Hospital Discharge Survey (NHDS), National Center for Health Statistics. Health Data Interactive, Health Care Use and Expenditures. 2012. www.cdc.gov/nchs/hdi.htm. Accessed 21 December 2012.
- 16.Neuman MD, Silber JH, Elkassabany NM, Ludwig JM, Fleisher LA. Comparative effectiveness of regional versus general anesthesia for hip fracture surgery in adults. Anesthesiology. 2012;117:72–92. doi: 10.1097/ALN.0b013e3182545e7c. [DOI] [PubMed] [Google Scholar]
- 17.Nie H, Yang YX, Wang Y, Liu Y, Zhao B, Luan B. Effects of continuous fascia iliaca compartment blocks for postoperative analgesia in hip fracture patients. Pain Res Manag. 2015;20:210–2. doi: 10.1155/2015/872651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nikkel LE, Fox EJ, Black KP, Davis C, Andersen L, Hollenbeak CS. Impact of comorbidities on hospitalization costs following hip fracture. J Bone Joint Surg Am. 2012;94:9–17. doi: 10.2106/JBJS.J.01077. [DOI] [PubMed] [Google Scholar]
- 19.Ranhoff AH, Martinsen MI, Holvik K, Solheim LF. Use of warfarin is associated with delay in surgery for hip fracture in older patients. Hosp Pract (1995) 2011;39:37–40. doi: 10.3810/hp.2011.02.372. [DOI] [PubMed] [Google Scholar]
- 20.Shariat AN, Hadzic A, Xu D, Shastri U, Kwofie K, Gandhi K, McCally CM, Gratenstein K, Vandepitte C, Gadsden J, Unis D. Fascia lliaca block for analgesia after hip arthroplasty: a randomized double-blind, placebo-controlled trial. Reg Anesth Pain Med. 2013;38:201–5. doi: 10.1097/AAP.0b013e31828a3c7c. [DOI] [PubMed] [Google Scholar]
- 21.Ultrasound-Guided Fascia Iliaca Block. 2013. http://www.nysora.com/updates/3107-ultrasound-guided-fascia-iliaca-block.html. Accessed 3/24 2016.
- 22.Whiting PS, Molina CS, Greenberg SE, Thakore RV, Obremskey WT, Sethi MK. Regional anaesthesia for hip fracture surgery is associated with significantly more peri-operative complications compared with general anaesthesia. Int Orthop. 2015;39:1321–7. doi: 10.1007/s00264-015-2735-5. [DOI] [PubMed] [Google Scholar]
- 23.Zuckerman JD, Skovron ML, Koval KJ, Aharonoff G, Frankel VH. Postoperative complications and mortality associated with operative delay in older patients who have a fracture of the hip. J Bone Joint Surg Am. 1995;77:1551–6. doi: 10.2106/00004623-199510000-00010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)
(PDF 1224 kb)