Dear Editor,
Angio-immunoblastic T-cell lymphoma (AITL) is a rare subtype of non-Hodgkins lymphoma (NHL), accounting for about 1–2% of all NHLs and 15–27% of peripheral T-cell lymphomas [1]. Most patients present with systemic lymphadenopathy, constitutional symptoms or abnormal immunological features. Abnormal laboratory test findings include cytopenias, positive Coomb’s test, polyclonal hypergammaglobulinemia, elevated LDH or presence of autoimmune antibodies. Circulating plasma cells and plasmacytoid lymphocytes have been occasionally detected in AITL patients. However, plasma cells >2 × 103 cells/µl mimicking plasma cell leukemia or exuberant reactive plasmacytosis in bone marrow in the order of >50% plasma cells including atypical forms is infrequently reported in AITL [2, 3]. We reviewed twelve cases of AITL reported in last 5 years at our institution. Bone marrow involvement by AITL was seen in one case (1/12 = 8.1%) while two cases (2/12 = 16.6%) revealed extensive bone marrow involvement by plasmacytes along with peripheral blood spillage, that led us to investigate for a coexisting myeloma or plasma cell leukemia.
Case 1
A 54 year old male presented with progressive pallor, fever and cervical lymphadenopathy for 1 month. Complete hemogram showed Hb = 52 g/l, TLC = 38.4 × 109/l and Platelet count = 100 × 109/l with DLC of N:58, L:10, E:12, MY:02, MMY:02, plasma cells: 16; nRBC 3/100WBCs. Serum creatinine was mildly raised(1.5 mg/dl) and serum calcium was 8.7 mg %. Serum protein was raised (10.2 g/dl) with reversal of A:G ratio (albumin: 1.2 g/dl; globulin: 9 g/dl). Serum LDH was elevated (531 U/ml). Peripheral smear showed red cell agglutination with polychromasia and an absolute plasma cell count of 5.8 × 103/µl, including atypical plasmacytoid cells. Corrected reticulocyte count was 6.6%. Direct Coomb’s test was found to be 4+ positive on Gel card testing. A working diagnosis of Plasma cell leukemia with Coomb’s positive autoimmune hemolytic anemia (AIHA) was made and further investigations advised. Skeletal survey revealed no bony lesions. Serum protein electrophoresis revealed polyclonal hypergammaglobulinemia but no M band was seen. Bone marrow aspirate smears showed 50% plasmacytoid lymphoid cells and plasma cells including immature, binucleated and atypical forms. Bone marrow biopsy showed diffuse infiltration with plasma cells, along with few hematopoietic cells of all three lineages in intervening areas. However, monoclonality of these plasma cells (CD138++/CD3−/CD20−) could not be established by immunohistochemistry (IHC) and in situ hybridization (ISH). Excisional biopsy of cervical lymph node and subsequent IHC revealed findings consistent with AITL (Fig. 1). A final diagnosis of AITL with polyclonal hypergammaglobulinemia and AIHA was made.
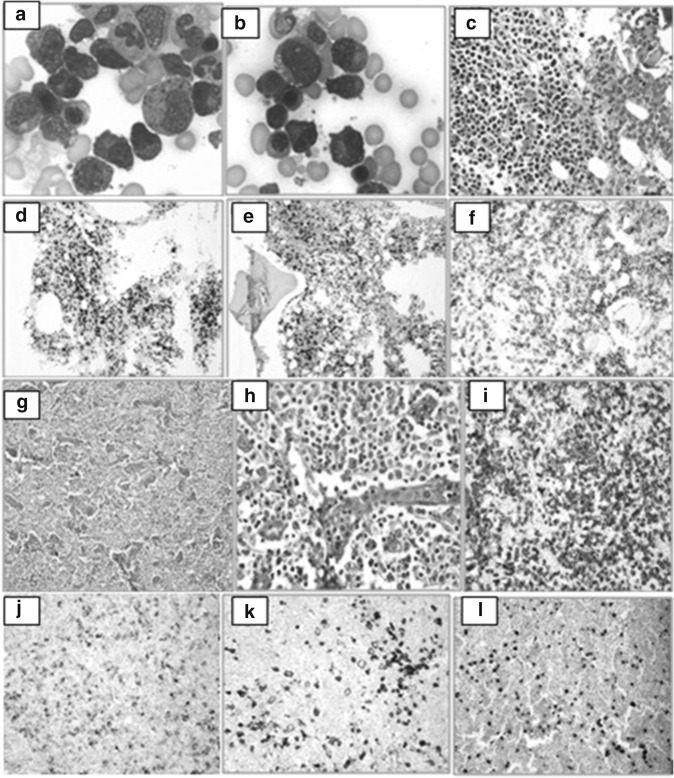
Fig. 1.
a, b Plasma cells including immature, plasmablastic and binucleated forms in bone marrow and peripheral blood. c Bone marrow biopsy shows diffuse sheets of plasma cells. d, e Staining for Kappa and Lambda light chains using ISH shows no clonal restriction. f Plasma cells are strongly positive for CD138. g, h Lymph node biopsy showing features of angioimmunoblastic lymphoma. i CD3 positivity in the neoplastic T cells. j–l IHC showing positivity for CD30, CD20 and EBER-ISH in the large RS-like B cells respectively
Case 2
A 54 year old male presented with pallor, dyspnea and generalized lymphadenopathy (LAD) for 1 month. Complete hemogram showed Hb = 103 g/l, TLC = 13.1 × 109/l and Platelet count = 144 × 109/l with a differential count of N:72, L:12, M:04, E:08, MY:01, MMY:03. Peripheral smear showed mild rouleaux formation with presence of occasional atypical plasmacytoid cells. Renal function tests revealed raised serum creatinine (3.5 mg/dl). Serum LDH was elevated (513 U/ml) and serum calcium was within normal limits. Serum protein was raised (9 g/dl) with reversal of A:G ratio. Serum protein electrophoresis revealed a ‘M’ band of 4.3 g/dl in gamma region. Skeletal survey was unremarkable. Nonetheless, no plasmacytomas were evidenced on tissue biopsy. PET Scan showed cervical, bilateral supraclavicular, mediastinal, abdomino-pelvic and inguinal LAD along with splenomegaly. Bone marrow aspirate smears showed 20% plasma cells including few atypical forms. Bone marrow biopsy showed infiltration with plasma cells lying singly as well as in large sheets. However, on IHC and ISH, these plasma cells were found to be polyclonal with no clonal restriction for kappa or lambda light chains. Histopathological examination of lymph node excisional biopsy was suggestive of AITL and further confirmed on IHC.
The lymph node biopsy in both these cases showed effacement of nodal architecture by large-sized atypical lymphoid cells with vesicular nuclei, scant cytoplasm and prominent nucleoli along with a few RS-like cells or immunoblasts and significant endothelial proliferation in a background of plasma cells, eosinophils and small lymphocytes. On IHC, these large atypical lymphoid cells were positive for CD3, CD5, CD2, CD10, CD4, PD-1 and bcl-6 with downregulation of CD7. The admixed RS-like cells expressed CD20, PAX-5, CD79a, CD30 and EBER (ISH).
Thus, both the presented cases showed exuberant polyclonal plasmacytic proliferation in association with angio-immunoblastic T-cell lymphoma. These patients presented with symptoms attributable to progressive anemia and had poor performance status. Presence of M band in the second case may be attributable to the EBV-driven abnormal B-cell proliferation seen in AITL. There was an initial delay in diagnosis due to inclination towards an associated diagnosis of plasma cell leukemia or multiple myeloma. Upon confirmation of diagnosis, both patients were started on CHOP-based regimen and showed regression of disease as evidenced on subsequent PET Scans.
Circulating plasma cells and plasmacytoid lymphocytes in bone marrow usually suggest a reactive etiology such as bacterial or viral infections, autoimmune phenomena and serum sickness [2]. It is less commonly associated with neoplastic process such as AITL and even rarer is such florid plasmacytic proliferation as seen in each of these two cases. Recently, several research groups have focused on the behavior of plasma cells in AITL, which ranged from reactive plasmacytosis to striking clonal proliferation. However, the role of plasma cells as a component of stromal microenvironment in AITL and the functional interaction between plasma cells and tumor cells has not yet been deciphered. Polyclonal proliferation in AITL may be multi-factorial, possibly due to associated EBV infection or increased release of various cytokines such as IL-6, IL-10, IL-21 and TNF-α, which are known to promote proliferation and survival of plasma cell progenitors as well as other systemic features such as fever, polyclonal hypergammaglobulinemia or presence of autoantibodies [3]. Moreover, some studies have proven that presence of exuberant plasmacytosis is not always a poor prognostic factor for AITL despite poor performance status of these patients at presentation [1]. Also, there are published case reports of AITL coexisting with myeloma [4]. Thus, all AITL cases with plasmacytosis must be thoroughly investigated to address the nature of plasma cell proliferation.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This case report does not contain any studies with human participants or animals performed by any of the authors.
References
- 1.Nagoshi H, Kuroda J, Kobayashi T, et al. Clinical manifestation of angioimmunoblastic T-cell lymphoma with exuberant plasmacytosis. Int J Hematol. 2013;98(3):366–374. doi: 10.1007/s12185-013-1411-z. [DOI] [PubMed] [Google Scholar]
- 2.Ahsanuddin AN, Brynes RK, Li S. Peripheral blood polyclonal plasmacytosis mimicking plasma cell leukemia in patients with angioimmunoblastic T-cell lymphoma: report of 3 cases and review of the literature. Int J Clin Exp Pathol. 2011;4(4):416–420. [PMC free article] [PubMed] [Google Scholar]
- 3.Grogg KL, Morice WG, Macon WR. Spectrum of bone marrow findings in patients with angioimmunoblastic T-cell lymphoma. Br J Haematol. 2007;137(5):416–422. doi: 10.1111/j.1365-2141.2007.06577.x. [DOI] [PubMed] [Google Scholar]
- 4.Xu J, Tang Y, Zhao S, et al. Angioimmunoblastic T-cell lymphoma with coexisting plasma cell myeloma: a case report and review of the literature. Tohoku J Exp Med. 2015;235(4):283–288. doi: 10.1620/tjem.235.283. [DOI] [PubMed] [Google Scholar]