ABSTRACT
The genetic disease cystic fibrosis (CF) is associated with chronic airway infections that are a proximal cause of death in many patients with this affliction. Classic microbiology studies focusing on canonical pathogens resulted in the development of a common set of views regarding the nature of the airway infections associated with this disease, and these ideas have influenced everything from the way infections are treated to how clinical trials for new CF-targeted antibiotics are designed and the focus of CF-related research topics. Recent culture-independent studies have prompted us to rethink, and in some cases discard, some of these long-held views. In this piece, I argue that an updated view of the complicated chronic infections associated with CF, thanks in large part to culture-independent studies of sputum and bronchoalveolar lavage fluid samples, should be leveraged to develop new strategies to treat these recalcitrant infections.
KEYWORDS: cystic fibrosis, microbiome, infection, sputum, airway
INTRODUCTION
Mary Anderson first described “cystic fibrosis of the pancreas,” now known as cystic fibrosis (CF), in 1938 (1), and it was recognized fairly early on that airway infection is a significant component of the CF disease process (2). As children lived longer and grew into adulthood, the progression of CF-associated airway disease became, and remains, a major clinical problem. Thus, the efforts to understand the microbiology of infections in the CF airway intensified (3). Classical culture-based clinical microbiology approaches for the identification of pathogens defined some key players in these chronic airway infections and simultaneously helped develop commonly held views regarding which microbes caused lung damage and how the microbial signature of infection changes over the course of infection (3, 4).
In more recent years, arguably starting in 2004 with a report by Rogers et al. (5), culture-independent approaches have been used to try to gain an additional understanding of the CF airway microbiota. This work has not been without controversy. In particular, questions often arise as to whether the sputum used as a source of DNA for culture-independent studies might be contaminated with oral microbiota and, importantly, what the extent of this contamination is, thus misleading the interpretation of the findings (6–9). A second critique often voiced is whether sputum is truly representative of the airway microbiota more broadly (7). Of course, these issues are also relevant to classical microbiology analysis of sputum, with the caveat that plate-based studies often employ a selective medium that supports the growth of only a portion of the microbes in the sample (3, 10). Nevertheless, the question has been raised for microbiome studies as to whether a single sputum sample truly represents the breadth of microbes present in the CF airway.
I would argue that lost in this critical narrative are a number of important contributions from these culture-independent studies to our thinking about the composition and role of microbes in the airway infections that are critical components of CF disease (Fig. 1). Indeed, as presented here, several “dogmatic” views of these chronic infections, often restated in the introductions of papers or just simply “general knowledge,” have been overturned by recent culture-independent studies. Importantly, the rethinking of our understanding of CF-associated airway infections on the basis of this new evidence positions us to deal with our current reality. While antibiotic therapies and the new waves of CF transmembrane conductance regulator (CFTR) corrector and potentiator drugs have the potential to mitigate airway infection, many patients still bear the burden of long-term lung function decline due to chronic infection (11). Reconsidering our long-held views of CF microbiology should also help the community of CF researchers and clinicians to rethink how to treat these chronic infections.
FIG 1.
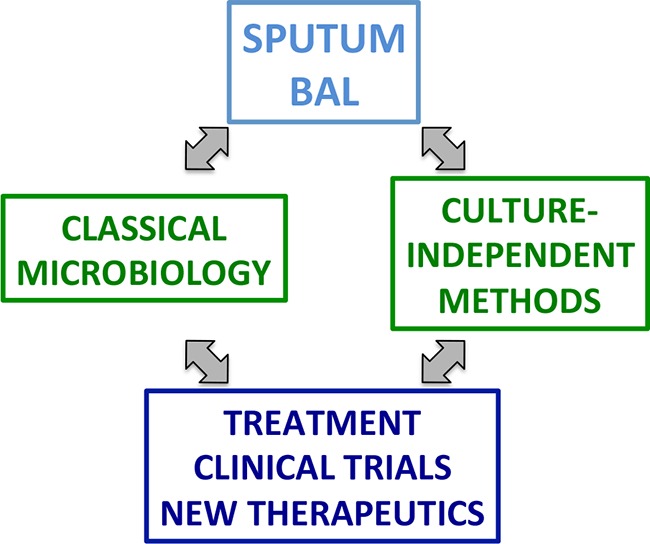
Role of culture-independent approaches for studying the microbiology of the CF airway. Sputum and BAL fluid, in most cases, are the sources of material used for elucidating the microbiology of the CF airway. New culture-independent methods have built on and complemented classical microbiology approaches. The culture-independent methods (largely 16S rRNA gene sequencing) have provided new insight into the nature of these infections.
I have decided to take a somewhat unusual tack in the format of this review article. I first present the “classic” view of CF microbiology developed from culture studies and clinical observations and then highlight how that view must be altered in light of culture-independent work. It is important to note that our current consensus understanding cannot often be pinpointed to a particular publication; rather, these views are commonly held and recited when the field discusses issues related to microbiology and infection in CF.
“PSEUDOMONAS AERUGINOSA IS THE DOMINANT BUG IN >80% OF CF PATIENTS”
Many talks or papers discussing CF microbiology typically include some variation of the statement, “The airway of >80% of CF patients is dominated by P. aeruginosa,” including work from my own lab (see references 12 to 21 for some examples). This statement is likely derived from plots of culture data showing that up to 70 to 80% of adult CF patients are culture positive for this important CF pathogen (22). It is also important to note that the terms “dominant” and “prevalent” have been sometimes conflated in the literature. As outlined below, I define dominant as meaning the majority of microbes in the infection are P. aeruginosa. Prevalent, in contrast, is defined as a microbe found among a large number of patients. Thus, a microbe can be prevalent (i.e., found in 90% of patients) but not dominant (for example, only comprising a small percentage of the microbes present). As outlined below, we see that while P. aeruginosa is indeed prevalent, it is the most abundant microbe and thus dominant in only ∼40% of CF patients. Thus, as illustrated below, the statement “The airway of >80% of CF patients is dominated by P. aeruginosa” is not formally correct.
A number of recent culture-independent studies of adults and children with CF dispute the view that P. aeruginosa is the dominant pathogen in most patients with CF if we define dominant colonization by P. aeruginosa as >50% of the total reads from culture-independent analysis of the 16S rRNA gene. My review of 16 different studies that include 507 patients (9, 12, 15, 18, 23–35) shows that only 42.4% of the airways of adult CF patients are dominated by P. aeruginosa. As an aside, it is important to note that the abundance and prevalence of P. aeruginosa vary with the age of the patient, with a general reduction in diversity of the airway communities in older patients and examples of total dominance of the CF airway by P. aeruginosa in end-stage disease as determined by analyzing tissue samples of such lungs removed during transplant (12, 32, 36–39). As outlined above, however, the picture of end-stage disease appears to be distinct from that of patients who still retain higher levels of lung function. Additionally, a recent study by Limoli et al. analyzing >200 adult patients with CF showed that P. aeruginosa was detectable in approximately one-third of the patients, while one-third had a mixture of P. aeruginosa and S. aureus, and the remaining third were culture positive for neither organism (40). Such findings are more than simply academic observations, given that the study design for currently approved antibiotics targeting pathogens in CF, as well as the treatment regimens for these patients, including eradication therapy, are largely focused on targeting P. aeruginosa (41–55). Such information may also be useful for clinicians making the often complicated decision about what antibiotic(s) should be used to treat patients with these complex infections. Similarly, clinical trial designs may need to incorporate a baseline microbiome study and potentially stratify patients by the dominant microbe present in the individual. If such baseline and endpoint microbiome studies are adopted, it is also critical to recognize that the lack of dynamics in culture-independent studies may reflect, at least in part, the stability of DNA (versus viable microbes) in sputum (56). The focus on the reduction in P. aeruginosa burden as an endpoint for the success of a trial for a new antibiotic may effectively ignore the microbiota and/or pathogens of over half of the patients with CF or even alter the “success” or “failure” outcomes of such studies. Interestingly, studies of the efficacy of aztreonam for inhalation solution (AZLI), an antibiotic that targets P. aeruginosa in the context of the CF airway, used alternative outcomes of benefits to CF patients, given the modest impact of this antibiotic on P. aeruginosa burden (15, 20, 48, 57). It may be that the benefit observed for AZLI arose from the impact on microbes other than P. aeruginosa. Given recent findings of the broad diversity of microbes in CF patients, it may be reasonable to consider other clinical trial outcome metrics.
P. AERUGINOSA BURDEN INCREASES WITH EXACERBATION AND IS REDUCED WHEN THE EXACERBATION IS TREATED WITH ANTIBIOTICS
A common refrain in explaining the cause of exacerbation was an increase in either P. aeruginosa numbers or bacterial load more broadly (58, 59). Patients diagnosed with an exacerbation (admittedly, a poorly defined condition) are then hospitalized and treated with intravenous (i.v.) antibiotics (58–61). The i.v. antibiotic chosen is typically informed by the antibiotic resistance profile of the P. aeruginosa isolates cultured during the last quarterly visit to the clinic.
Recent microbiome studies tell a different story. Using a common study design of recruiting stable CF patients and then tracking these patients during the course of exacerbation, the treatment and subsequent exacerbation resolution revealed no significant relationship between absolute or relative levels of P. aeruginosa or the total load of bacteria (measured by 16S rRNA gene) and the onset or resolution of the exacerbation (13, 18, 32, 62–65). Thus, these 7 studies of 102 patients revealed no obvious or consistent pattern in community structure, P. aeruginosa abundance, or overall bacterial load that could explain the onset of exacerbation. In contrast, a study from several years ago by Sibley et al. (65), combining culture and culture-independent approaches to dissect airway communities in CF, as well as follow-up studies from this and other groups (12, 23, 24, 27, 66–68), suggests the underappreciated role of Streptococcus spp. in CF airway disease, including the link of the Streptococcus milleri group (S. constellatus, S. intermedius, and S. anginosus) to at least a subset of exacerbation events. The work of Surette's group provides what is perhaps the most compelling mechanism for exacerbation onset, but a role for the S. milleri group microbes could only account for ∼40% of exacerbations. The impact of culture-independent microbiome studies, alone or combined with culture, on the thinking about exacerbations is reflected in a 2016 review article by Smyth (58) highlighting the need to rethink exacerbation diagnosis and treatment in light of these recent data. As it stands, while the older view of factors driving exacerbation appears to be off base, we do not yet understand what triggers an exacerbation event.
SPUTUM DOES NOT REFLECT THE MICROBIOLOGY OF THE AIRWAY
A review of the literature relevant to the microbiome and the CF airway would not be complete without a discussion of whether sputum acts as a relevant surrogate for the microbiota in the CF airway. This discussion has disproportionately dominated the narrative regarding the value of such microbiome studies. While end-stage disease, represented by the analysis of transplanted lungs for example (6, 36, 37, 69), is indeed commonly associated with P. aeruginosa-dominated infections, several studies have independently verified that the lung microbiota in CF is polymicrobial in nature and well reflected in sputum samples, at least for the major genera identified. A few recent studies speak to this controversy.
Rogers et al. (70) used 16S rRNA gene profiling by terminal restriction fragment length polymorphism analysis to compare mouthwash and sputum samples from 19 adults with CF. Based on this analysis, they concluded that their sputum samples were not subject to “profound contamination by oral cavity bacteria” (70). They based their conclusion on the markedly different profiles and the lack of overlap between mouthwash and sputum samples. That is, if oral microbes were substantially contaminating sputum, then the two samples should look quite similar—this is not what these investigators observed (70). Using a complementary approach, Hogan et al. (9) compared the profiles of microbes from spontaneously expectorated sputum samples with those from bronchoalveolar lavage (BAL) fluid and/or protected brush samples. Based on the analysis of 6 patients for which there were both sputum and bronchoscope-harvested samples, they concluded that, for typical CF pathogens (P. aeruginosa, Stenotrophomonas, Achromobacter, Burkholderia, Staphylococcus, and Haemophilus spp.), there was a concordance between the dominant pathogen from sputum and BAL fluid samples by deep sequencing and classical microbiological approaches (9). Protected brush sampling of the airway, using a methodology that shielded the sample from oral contamination, revealed that Streptococcus, Rothia, Peptostreptococcus, and Gemella are indeed found in the airway and cannot be explained by oral contamination. It is important to note that while this study did show clear differences between sputum and BAL fluid, likely driven in part from the contribution of oral contaminants, sputum used for culture-independent or classic microbiological analysis provides important information regarding the microbiota of the CF airway.
Another important point raised by the study from Hogan et al. (9) comes from regional (upper, middle, and lower) sampling of the right airway by BAL or protected brushes. These investigators found no significant difference among the communities between regions or as a function of differential regional lung damage (9). These data suggest that the original source of the sputum may not matter in terms of the information provided. Also consistent with this finding is a previous study of serial sputum samples from adults showing consistent communities over a 7-month period (71). Similarly, a recent study of the microbiota from 95 daily sputum samples of four patients with CF showed little in the way of day-to-day changes (72). Taken together, these data can be taken to mean the source of the sputum in the airway does not dictate the microbes identified; rather, the relative uniformity of the microbial community in the airway means that sputum samples are quite likely to paint the general picture of the microbiota present in the lung. Furthermore, given the complexity of standard quantitative microbiological counts from clinical samples, the relative low cost of culture-independent methods, and the advantage of determining relative and absolute abundance values of microbes in the airway, sputum analysis could provide an important aspect of the overall clinical picture.
Finally, the controversy regarding oral contamination of sputum has also potentially resulted in undervaluing the role of anaerobes in CF airway disease. Publications from several groups, including the works of Gilligan and of Tunney and colleagues, using a combination of culture-dependent and -independent studies to analyze sputum and bronchoalveolar lavage fluid samples have associated anaerobes and their metabolic products with negative respiratory outcomes and inflammation and demonstrated that these microbes can be nonresponsive to typical CF-specific antimicrobial treatments (5, 9, 73–78). Thus, the narrative of oral contamination of sputum should not close the door on exploring the potentially important impact of anaerobes in CF airway infection.
CONCLUSIONS
The value of microbiome studies in the context of the CF airway, in this author's opinion, has been underestimated. A discussion dominated by methodological debates and driven by considerations that appear to stem from misleading paper titles has resulted in many outside the field underappreciating CF airway microbiome studies over the past decade. In fact, data from the culture-independent analysis of sputum and bronchoalveolar lavage fluid samples should (and can) be impacting everything from the therapeutic choices of physicians to clinical trial design. I would argue that culture-independent studies of sputum and bronchoalveolar lavage fluid from the CF airway have overturned several long-held, but inaccurate, ideas in the field. The enhanced, and clearly more complex, picture of the nature of infections in the CF airway will enable the field to move forward. While antibiotic therapies have benefited many CF patients, there are clearly limitations of the current antimicrobial therapeutic regimens. Perhaps our newly enhanced understanding of the important role of pathogens other than P. aeruginosa, as well as the reality of polymicrobial biofilm-like infections in the CF airway, will spur new thinking, model systems, and strategies to treat these chronic infections.
ACKNOWLEDGMENTS
This work was supported by R37 AI83256-06 and funds from the Cystic Fibrosis Foundation (OTOOLE16G0) to G.A.O.
I thank D. A. Hogan for her critical comments on the manuscript.
Biography

George A. O'Toole is a professor of microbiology and immunology at the Geisel School of Medicine at Dartmouth in Hanover, NH. He received his Ph.D. with Dr. Jorge Escalante-Semerena at the University of Wisconsin—Madison in 1994 and was a postdoctoral fellow with Roberto Kolter at Harvard Medical School. He started his faculty position at Dartmouth in 1999. Dr. O'Toole started working on cystic fibrosis (CF) research as a postdoctoral fellow with support from a Medical Foundation Senior Postdoctoral Fellowship, and his interest in CF research continued with support from the CF Foundation and the Lung Biology Center at Dartmouth.
REFERENCES
- 1.Anderson DH. 1938. Cystic fibrosis of the pancreas and its relation to celiac disease: a clinical and pathological study. Am J Dis Child 56:344–399. doi: 10.1001/archpedi.1938.01980140114013. [DOI] [Google Scholar]
- 2.Di Sant'Agnese PE, Anderson DH. 1946. Celiac syndrome; chemotherapy in infections of the respiratory tract associated with cystic fibrosis of the pancreas; observations with penicillin and drugs of the sulfonamide group, with special reference to penicillin aerosol. Am J Dis Child 72:17–61. doi: 10.1001/archpedi.1946.02020300024003. [DOI] [PubMed] [Google Scholar]
- 3.Govan JR, Nelson JW. 1992. Microbiology of lung infection in cystic fibrosis. Br Med Bull 48:912–930. doi: 10.1093/oxfordjournals.bmb.a072585. [DOI] [PubMed] [Google Scholar]
- 4.Boucher RC. 2004. New concepts of the pathogenesis of cystic fibrosis lung disease. Eur Respir J 23:146–158. doi: 10.1183/09031936.03.00057003. [DOI] [PubMed] [Google Scholar]
- 5.Rogers GB, Carroll MP, Serisier DJ, Hockey PM, Jones G, Bruce KD. 2004. Characterization of bacterial community diversity in cystic fibrosis lung infections by use of 16s ribosomal DNA terminal restriction fragment length polymorphism profiling. J Clin Microbiol 42:5176–5183. doi: 10.1128/JCM.42.11.5176-5183.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goddard AF, Staudinger BJ, Dowd SE, Joshi-Datar A, Wolcott RD, Aitken ML, Fligner CL, Singh PK. 2012. Direct sampling of cystic fibrosis lungs indicates that DNA-based analyses of upper-airway specimens can misrepresent lung microbiota. Proc Natl Acad Sci U S A 109:13769–13774. doi: 10.1073/pnas.1107435109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch SV, Bruce KD. 2013. The cystic fibrosis airway microbiome. Cold Spring Harb Perspect Med 3:a009738. doi: 10.1101/cshperspect.a009738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Prevaes SM, de Steenhuijsen Piters WA, de Winter-de Groot KM, Janssens HM, Tramper-Stranders GA, Chu ML, Tiddens HA, van Westreenen M, van der Ent CK, Sanders EA, Bogaert D. 2017. Concordance between upper and lower airway microbiota in infants with cystic fibrosis. Eur Respir J 49:1602235. doi: 10.1183/13993003.02235-2016. [DOI] [PubMed] [Google Scholar]
- 9.Hogan DA, Willger SD, Dolben EL, Hampton TH, Stanton BA, Morrison HG, Sogin ML, Czum J, Ashare A. 2016. Analysis of lung microbiota in bronchoalveolar lavage, protected brush and sputum samples from subjects with mild-to-moderate cystic fibrosis lung disease. PLoS One 11:e0149998. doi: 10.1371/journal.pone.0149998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Govan JR, Deretic V. 1996. Microbial pathogenesis in cystic fibrosis: mucoid Pseudomonas aeruginosa and Burkholderia cepacia. Microbiol Rev 60:539–574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hisert KB, Heltshe SL, Pope C, Jorth P, Wu X, Edwards RM, Radey M, Accurso FJ, Wolter DJ, Cooke G, Adam RJ, Carter S, Grogan B, Launspach JL, Donnelly SC, Gallagher CG, Bruce JE, Stoltz DA, Welsh MJ, Hoffman LR, McKone EF, Singh PK. 2017. Restoring cystic fibrosis transmembrane conductance regulator function reduces airway bacteria and inflammation in people with cystic fibrosis and chronic lung infections. Am J Respir Crit Care Med 195:1617–1628. doi: 10.1164/rccm.201609-1954OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Coburn B, Wang PW, Diaz Caballero J, Clark ST, Brahma V, Donaldson S, Zhang Y, Surendra A, Gong Y, Elizabeth Tullis D, Yau YC, Waters VJ, Hwang DM, Guttman DS. 2015. Lung microbiota across age and disease stage in cystic fibrosis. Sci Rep 5:10241. doi: 10.1038/srep10241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fodor AA, Klem ER, Gilpin DF, Elborn JS, Boucher RC, Tunney MM, Wolfgang MC. 2012. The adult cystic fibrosis airway microbiota is stable over time and infection type, and highly resilient to antibiotic treatment of exacerbations. PLoS One 7:e45001. doi: 10.1371/journal.pone.0045001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hampton TH, Green DM, Cutting GR, Morrison HG, Sogin ML, Gifford AH, Stanton BA, O'Toole GA. 2014. The microbiome in pediatric cystic fibrosis patients: the role of shared environment suggests a window of intervention. Microbiome 2:14. doi: 10.1186/2049-2618-2-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heirali AA, Workentine ML, Acosta N, Poonja A, Storey DG, Somayaji R, Rabin HR, Whelan FJ, Surette MG, Parkins MD. 2017. The effects of inhaled aztreonam on the cystic fibrosis lung microbiome. Microbiome 5:51. doi: 10.1186/s40168-017-0265-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keravec M, Mounier J, Prestat E, Vallet S, Jansson JK, Burgaud G, Rosec S, Gouriou S, Rault G, Coton E, Barbier G, Hery-Arnaud G. 2015. Insights into the respiratory tract microbiota of patients with cystic fibrosis during early Pseudomonas aeruginosa colonization. Springerplus 4:405. doi: 10.1186/s40064-015-1207-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lim YW, Evangelista JS III, Schmieder R, Bailey B, Haynes M, Furlan M, Maughan H, Edwards R, Rohwer F, Conrad D. 2014. Clinical insights from metagenomic analysis of sputum samples from patients with cystic fibrosis. J Clin Microbiol 52:425–437. doi: 10.1128/JCM.02204-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Price KE, Hampton TH, Gifford AH, Dolben EL, Hogan DA, Morrison HG, Sogin ML, O'Toole GA. 2013. Unique microbial communities persist in individual cystic fibrosis patients throughout a clinical exacerbation. Microbiome 1:27. doi: 10.1186/2049-2618-1-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hampton TH, Ballok AE, Bomberger JM, Rutkowski MR, Barnaby R, Coutermarsh B, Conejo-Garcia JR, O'Toole GA, Stanton BA. 2012. Does the ΔF508-CFTR mutation induce a proinflammatory response in human airway epithelial cells? Am J Physiol Lung Cell Mol Physiol 303:L509–L518. doi: 10.1152/ajplung.00226.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yu Q, Griffin EF, Moreau-Marquis S, Schwartzman JD, Stanton BA, O'Toole GA. 2012. In vitro evaluation of tobramycin and aztreonam versus Pseudomonas aeruginosa biofilms on cystic fibrosis-derived human airway epithelial cells. J Antimicrob Chemother 67:2673–2681. doi: 10.1093/jac/dks296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ballok AE, Bahl CD, Dolben EL, Lindsay AK, St Laurent JD, Hogan DA, Madden DR, O'Toole GA. 2012. Epoxide-mediated CifR repression of cif gene expression utilizes two binding sites in Pseudomonas aeruginosa. J Bacteriol 194:5315–5324. doi: 10.1128/JB.00984-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cystic Fibrosis Foundation. 2016. Cystic Fibrosis Foundation patient registry 2010 annual data report. Cystic Fibrosis Foundation, Bethesda, MD. [Google Scholar]
- 23.Filkins LM, Hampton TH, Gifford AH, Gross MJ, Hogan DA, Sogin ML, Morrison HG, Paster BJ, O'Toole GA. 2012. Prevalence of streptococci and increased polymicrobial diversity associated with cystic fibrosis patient stability. J Bacteriol 194:4709–4717. doi: 10.1128/JB.00566-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Acosta N, Whelan FJ, Somayaji R, Poonja A, Surette MG, Rabin HR, Parkins MD. 2017. The evolving cystic fibrosis microbiome: a comparative cohort study spanning 16 years. Ann Am Thorac Soc 14:1288–1297. doi: 10.1513/AnnalsATS.201609-668OC. [DOI] [PubMed] [Google Scholar]
- 25.Salipante SJ, Sengupta DJ, Rosenthal C, Costa G, Spangler J, Sims EH, Jacobs MA, Miller SI, Hoogestraat DR, Cookson BT, McCoy C, Matsen FA, Shendure J, Lee CC, Harkins TT, Hoffman NG. 2013. Rapid 16S rRNA next-generation sequencing of polymicrobial clinical samples for diagnosis of complex bacterial infections. PLoS One 8:e65226. doi: 10.1371/journal.pone.0065226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Feigelman R, Kahlert CR, Baty F, Rassouli F, Kleiner RL, Kohler P, Brutsche MH, von Mering C. 2017. Sputum DNA sequencing in cystic fibrosis: non-invasive access to the lung microbiome and to pathogen details. Microbiome 5:20. doi: 10.1186/s40168-017-0234-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Whelan FJ, Heirali AA, Rossi L, Rabin HR, Parkins MD, Surette MG. 2017. Longitudinal sampling of the lung microbiota in individuals with cystic fibrosis. PLoS One 12:e0172811. doi: 10.1371/journal.pone.0172811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quinn RA, Phelan VV, Whiteson KL, Garg N, Bailey BA, Lim YW, Conrad DJ, Dorrestein PC, Rohwer FL. 2016. Microbial, host and xenobiotic diversity in the cystic fibrosis sputum metabolome. ISME J 10:1483–1498. doi: 10.1038/ismej.2015.207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Quinn RA, Lim YW, Maughan H, Conrad D, Rohwer F, Whiteson KL. 2014. Biogeochemical forces shape the composition and physiology of polymicrobial communities in the cystic fibrosis lung. mBio 5:e00956-. doi: 10.1128/mBio.00956-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Smith DJ, Badrick AC, Zakrzewski M, Krause L, Bell SC, Anderson GJ, Reid DW. 2014. Pyrosequencing reveals transient cystic fibrosis lung microbiome changes with intravenous antibiotics. Eur Respir J 44:922–930. doi: 10.1183/09031936.00203013. [DOI] [PubMed] [Google Scholar]
- 31.Willger SD, Grim SL, Dolben EL, Shipunova A, Hampton TH, Morrison HG, Filkins LM, O'Toole GA, Moulton LA, Ashare A, Sogin ML, Hogan DA. 2014. Characterization and quantification of the fungal microbiome in serial samples from individuals with cystic fibrosis. Microbiome 2:40. doi: 10.1186/2049-2618-2-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao J, Schloss PD, Kalikin LM, Carmody LA, Foster BK, Petrosino JF, Cavalcoli JD, VanDevanter DR, Murray S, Li JZ, Young VB, LiPuma JJ. 2012. Decade-long bacterial community dynamics in cystic fibrosis airways. Proc Natl Acad Sci U S A 109:5809–5814. doi: 10.1073/pnas.1120577109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zhao J, Evans CR, Carmody LA, LiPuma JJ. 2015. Impact of storage conditions on metabolite profiles of sputum samples from persons with cystic fibrosis. J Cyst Fibros 14:468–473. doi: 10.1016/j.jcf.2015.02.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zemanick ET, Harris JK, Wagner BD, Robertson CE, Sagel SD, Stevens MJ, Accurso FJ, Laguna TA. 2013. Inflammation and airway microbiota during cystic fibrosis pulmonary exacerbations. PLoS One 8:e62917. doi: 10.1371/journal.pone.0062917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nguyen LD, Deschaght P, Merlin S, Loywick A, Audebert C, Van Daele S, Viscogliosi E, Vaneechoutte M, Delhaes L. 2016. Effects of propidium monoazide (PMA) treatment on mycobiome and bacteriome analysis of cystic fibrosis airways during exacerbation. PLoS One 11:e0168860. doi: 10.1371/journal.pone.0168860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Cox MJ, Allgaier M, Taylor B, Baek MS, Huang YJ, Daly RA, Karaoz U, Andersen GL, Brown R, Fujimura KE, Wu B, Tran D, Koff J, Kleinhenz ME, Nielson D, Brodie EL, Lynch SV. 2010. Airway microbiota and pathogen abundance in age-stratified cystic fibrosis patients. PLoS One 5:e11044. doi: 10.1371/journal.pone.0011044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rudkjøbing VB, Thomsen TR, Alhede M, Kragh KN, Nielsen PH, Johansen UR, Givskov M, Hoiby N, Bjarnsholt T. 2012. The microorganisms in chronically infected end-stage and non-end-stage cystic fibrosis patients. FEMS Immunol Med Microbiol 65:236–244. doi: 10.1111/j.1574-695X.2011.00925.x. [DOI] [PubMed] [Google Scholar]
- 38.Bjarnsholt T, Jensen PO, Fiandaca MJ, Pedersen J, Hansen CR, Andersen CB, Pressler T, Givskov M, Hoiby N. 2009. Pseudomonas aeruginosa biofilms in the respiratory tract of cystic fibrosis patients. Pediatr Pulmonol 44:547–558. doi: 10.1002/ppul.21011. [DOI] [PubMed] [Google Scholar]
- 39.Jorth P, Staudinger BJ, Wu X, Hisert KB, Hayden H, Garudathri J, Harding CL, Radey MC, Rezayat A, Bautista G, Berrington WR, Goddard AF, Zheng C, Angermeyer A, Brittnacher MJ, Kitzman J, Shendure J, Fligner CL, Mittler J, Aitken ML, Manoil C, Bruce JE, Yahr TL, Singh PK. 2015. Regional isolation drives bacterial diversification within cystic fibrosis lungs. Cell Host Microbe 18:307–319. doi: 10.1016/j.chom.2015.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Limoli DH, Yang J, Khansaheb MK, Helfman B, Peng L, Stecenko AA, Goldberg JB. 2016. Staphylococcus aureus and Pseudomonas aeruginosa coinfection is associated with cystic fibrosis-related diabetes and poor clinical outcomes. Eur J Clin Microbiol Infect Dis 35:947–953. doi: 10.1007/s10096-016-2621-0. [DOI] [PubMed] [Google Scholar]
- 41.Mazurek H, Chiron R, Kucerova T, Geidel C, Bolbas K, Chuchalin A, Blanco-Aparicio M, Santoro D, Varoli G, Zibellini M, Cicirello HG, Antipkin YG. 2014. Long-term efficacy and safety of aerosolized tobramycin 300 mg/4 ml in cystic fibrosis. Pediatr Pulmonol 49:1076–1089. doi: 10.1002/ppul.22989. [DOI] [PubMed] [Google Scholar]
- 42.Tappenden P, Harnan S, Uttley L, Mildred M, Carroll C, Cantrell A. 2013. Colistimethate sodium powder and tobramycin powder for inhalation for the treatment of chronic Pseudomonas aeruginosa lung infection in cystic fibrosis: systematic review and economic model. Health Technol Assess 17:1–181. doi: 10.3310/hta17560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Cipolla D, Chan HK. 2013. Inhaled antibiotics to treat lung infection. Pharm Pat Anal 2:647–663. doi: 10.4155/ppa.13.47. [DOI] [PubMed] [Google Scholar]
- 44.Konstan MW, Flume PA, Kappler M, Chiron R, Higgins M, Brockhaus F, Zhang J, Angyalosi G, He E, Geller DE. 2011. Safety, efficacy and convenience of tobramycin inhalation powder in cystic fibrosis patients: the EAGER trial. J Cyst Fibros 10:54–61. doi: 10.1016/j.jcf.2010.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Banerjee D, Stableforth D. 2000. The treatment of respiratory pseudomonas infection in cystic fibrosis: what drug and which way? Drugs 60:1053–1064. doi: 10.2165/00003495-200060050-00006. [DOI] [PubMed] [Google Scholar]
- 46.Wiesemann HG, Steinkamp G, Ratjen F, Bauernfeind A, Przyklenk B, Doring G, von der Hardt H. 1998. Placebo-controlled, double-blind, randomized study of aerosolized tobramycin for early treatment of Pseudomonas aeruginosa colonization in cystic fibrosis. Pediatr Pulmonol 25:88–92. [DOI] [PubMed] [Google Scholar]
- 47.Elborn JS, Henig NR. 2010. Optimal airway antimicrobial therapy for cystic fibrosis: the role of inhaled aztreonam lysine. Expert Opin Pharmacother 11:1373–1385. doi: 10.1517/14656566.2010.482102. [DOI] [PubMed] [Google Scholar]
- 48.Retsch-Bogart GZ, Quittner AL, Gibson RL, Oermann CM, McCoy KS, Montgomery AB, Cooper PJ. 2009. Efficacy and safety of inhaled aztreonam lysine for airway Pseudomonas in cystic fibrosis. Chest 135:1223–1232. doi: 10.1378/chest.08-1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Retsch-Bogart GZ, Burns JL, Otto KL, Liou TG, McCoy K, Oermann C, Gibson RL, AZLI Phase II Study Group. 2008. A phase 2 study of aztreonam lysine for inhalation to treat patients with cystic fibrosis and Pseudomonas aeruginosa infection. Pediatr Pulmonol 43:47–58. doi: 10.1002/ppul.20736. [DOI] [PubMed] [Google Scholar]
- 50.Westerman EM, Le Brun PP, Touw DJ, Frijlink HW, Heijerman HG. 2004. Effect of nebulized colistin sulphate and colistin sulphomethate on lung function in patients with cystic fibrosis: a pilot study. J Cyst Fibros 3:23–28. doi: 10.1016/j.jcf.2003.12.005. [DOI] [PubMed] [Google Scholar]
- 51.Griese M, Muller I, Reinhardt D. 2002. Eradication of initial Pseudomonas aeruginosa colonization in patients with cystic fibrosis. Eur J Med Res 7:79–80. [PubMed] [Google Scholar]
- 52.Frederiksen B, Koch C, Hoiby N. 1997. Antibiotic treatment of initial colonization with Pseudomonas aeruginosa postpones chronic infection and prevents deterioration of pulmonary function in cystic fibrosis. Pediatr Pulmonol 23:330–335. [DOI] [PubMed] [Google Scholar]
- 53.Elphick HE, Scott A. 2016. Single versus combination intravenous anti-pseudomonal antibiotic therapy for people with cystic fibrosis. Cochrane Database Syst Rev 12:CD002007. doi: 10.1002/14651858.CD002007.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Campbell CT, McCaleb R, Manasco KB. 2016. New inhaled antimicrobial formulations for use in the cystic fibrosis patient population. Ann Pharmacother 50:133–140. doi: 10.1177/1060028015621916. [DOI] [PubMed] [Google Scholar]
- 55.Langan KM, Kotsimbos T, Peleg AY. 2015. Managing Pseudomonas aeruginosa respiratory infections in cystic fibrosis. Curr Opin Infect Dis 28:547–556. doi: 10.1097/QCO.0000000000000217. [DOI] [PubMed] [Google Scholar]
- 56.Rogers GB, Marsh P, Stressmann AF, Allen CE, Daniels TV, Carroll MP, Bruce KD. 2010. The exclusion of dead bacterial cells is essential for accurate molecular analysis of clinical samples. Clin Microbiol Infect 16:1656–1658. doi: 10.1111/j.1469-0691.2010.03189.x. [DOI] [PubMed] [Google Scholar]
- 57.Wainwright CE, Quittner AL, Geller DE, Nakamura C, Wooldridge JL, Gibson RL, Lewis S, Montgomery AB. 2011. Aztreonam for inhalation solution (AZLI) in patients with cystic fibrosis, mild lung impairment, and P. aeruginosa. J Cyst Fibros 10:234–242. doi: 10.1016/j.jcf.2011.02.007. [DOI] [PubMed] [Google Scholar]
- 58.Smyth A. 2016. Treatment of pulmonary exacerbations in cystic fibrosis - could do better? Paediatr Respir Rev 20 Suppl:6–7. doi: 10.1016/j.prrv.2016.06.004. [DOI] [PubMed] [Google Scholar]
- 59.Stenbit AE, Flume PA. 2011. Pulmonary exacerbations in cystic fibrosis. Curr Opin Pulm Med 17:442–447. doi: 10.1097/MCP.0b013e32834b8c04. [DOI] [PubMed] [Google Scholar]
- 60.Newton TJ. 2009. Respiratory care of the hospitalized patient with cystic fibrosis. Respir Care 54:769–776. [DOI] [PubMed] [Google Scholar]
- 61.Gibson RL, Burns JL, Ramsey BW. 2003. Pathophysiology and management of pulmonary infections in cystic fibrosis. Am J Respir Crit Care Med 168:918–951. doi: 10.1164/rccm.200304-505SO. [DOI] [PubMed] [Google Scholar]
- 62.Cuthbertson L, Rogers GB, Walker AW, Oliver A, Green LE, Daniels TW, Carroll MP, Parkhill J, Bruce KD, van der Gast CJ. 2016. Respiratory microbiota resistance and resilience to pulmonary exacerbation and subsequent antimicrobial intervention. ISME J 10:1081–1091. doi: 10.1038/ismej.2015.198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Carmody LA, Zhao J, Schloss PD, Petrosino JF, Murray S, Young VB, Li JZ, LiPuma JJ. 2013. Changes in cystic fibrosis airway microbiota at pulmonary exacerbation. Ann Am Thorac Soc 10:179–187. doi: 10.1513/AnnalsATS.201211-107OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Reid DW, Latham R, Lamont IL, Camara M, Roddam LF. 2013. Molecular analysis of changes in Pseudomonas aeruginosa load during treatment of a pulmonary exacerbation in cystic fibrosis. J Cyst Fibros 12:688–699. doi: 10.1016/j.jcf.2013.03.008. [DOI] [PubMed] [Google Scholar]
- 65.Sibley CD, Parkins MD, Rabin HR, Duan K, Norgaard JC, Surette MG. 2008. A polymicrobial perspective of pulmonary infections exposes an enigmatic pathogen in cystic fibrosis patients. Proc Natl Acad Sci U S A 105:15070–15075. doi: 10.1073/pnas.0804326105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Sibley CD, Surette MG. 2011. The polymicrobial nature of airway infections in cystic fibrosis: Cangene Gold Medal Lecture. Can J Microbiol 57:69–77. doi: 10.1139/W10-105. [DOI] [PubMed] [Google Scholar]
- 67.Sibley CD, Grinwis ME, Field TR, Parkins MD, Norgaard JC, Gregson DB, Rabin HR, Surette MG. 2010. McKay agar enables routine quantification of the ‘Streptococcus milleri’ group in cystic fibrosis patients. J Med Microbiol 59:534–540. doi: 10.1099/jmm.0.016592-0. [DOI] [PubMed] [Google Scholar]
- 68.Flight WG, Smith A, Paisey C, Marchesi JR, Bull MJ, Norville PJ, Mutton KJ, Webb AK, Bright-Thomas RJ, Jones AM, Mahenthiralingam E. 2015. Rapid detection of emerging pathogens and loss of microbial diversity associated with severe lung disease in cystic fibrosis. J Clin Microbiol 53:2022–2029. doi: 10.1128/JCM.00432-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rudkjøbing VB, Thomsen TR, Alhede M, Kragh KN, Nielsen PH, Johansen UR, Givskov M, Hoiby N, Bjarnsholt T. 2011. True microbiota involved in chronic lung infection of cystic fibrosis patients found by culturing and 16S rRNA gene analysis. J Clin Microbiol 49:4352–4355. doi: 10.1128/JCM.06092-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Rogers GB, Carroll MP, Serisier DJ, Hockey PM, Jones G, Kehagia V, Connett GJ, Bruce KD. 2006. Use of 16S rRNA gene profiling by terminal restriction fragment length polymorphism analysis to compare bacterial communities in sputum and mouthwash samples from patients with cystic fibrosis. J Clin Microbiol 44:2601–2604. doi: 10.1128/JCM.02282-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gifford AH, Alexandru DM, Li Z, Dorman DB, Moulton LA, Price KE, Hampton TH, Sogin ML, Zuckerman JB, Parker HW, Stanton BA, O'Toole GA. 2014. Iron supplementation does not worsen respiratory health or alter the sputum microbiome in cystic fibrosis. J Cyst Fibros 13:311–318. doi: 10.1016/j.jcf.2013.11.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Carmody LA, Zhao J, Kalikin LM, LeBar W, Simon RH, Venkataraman A, Schmidt TM, Abdo Z, Schloss PD, LiPuma JJ. 2015. The daily dynamics of cystic fibrosis airway microbiota during clinical stability and at exacerbation. Microbiome 3:12. doi: 10.1186/s40168-015-0074-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Tunney MM, Klem ER, Fodor AA, Gilpin DF, Moriarty TF, McGrath SJ, Muhlebach MS, Boucher RC, Cardwell C, Doering G, Elborn JS, Wolfgang MC. 2011. Use of culture and molecular analysis to determine the effect of antibiotic treatment on microbial community diversity and abundance during exacerbation in patients with cystic fibrosis. Thorax 66:579–584. doi: 10.1136/thx.2010.137281. [DOI] [PubMed] [Google Scholar]
- 74.Thomassen MJ, Klinger JD, Badger SJ, van Heeckeren DW, Stern RC. 1984. Cultures of thoracotomy specimens confirm usefulness of sputum cultures in cystic fibrosis. J Pediatr 104:352–356. doi: 10.1016/S0022-3476(84)81094-X. [DOI] [PubMed] [Google Scholar]
- 75.Sherrard LJ, Tunney MM, Elborn JS. 2014. Antimicrobial resistance in the respiratory microbiota of people with cystic fibrosis. Lancet 384:703–713. doi: 10.1016/S0140-6736(14)61137-5. [DOI] [PubMed] [Google Scholar]
- 76.Mirković B, Murray MA, Lavelle GM, Molloy K, Azim AA, Gunaratnam C, Healy F, Slattery D, McNally P, Hatch J, Wolfgang M, Tunney MM, Muhlebach MS, Devery R, Greene CM, McElvaney NG. 2015. The role of short-chain fatty acids, produced by anaerobic bacteria, in the cystic fibrosis airway. Am J Respir Crit Care Med 192:1314–1324. doi: 10.1164/rccm.201505-0943OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Tunney MM, Field TR, Moriarty TF, Patrick S, Doering G, Muhlebach MS, Wolfgang MC, Boucher R, Gilpin DF, McDowell A, Elborn JS. 2008. Detection of anaerobic bacteria in high numbers in sputum from patients with cystic fibrosis. Am J Respir Crit Care Med 177:995–1001. doi: 10.1164/rccm.200708-1151OC. [DOI] [PubMed] [Google Scholar]
- 78.Gilligan PH. 2014. Infections in patients with cystic fibrosis: diagnostic microbiology update. Clin Lab Med 34:197–217. doi: 10.1016/j.cll.2014.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]


