Abstract
Study Objectives:
Sleep improvement is a promising target for preventing and modifying many health problems. Hypnosis is considered a cost-effective and safe intervention with reported benefits for multiple health conditions. There is a growing body of research assessing the efficacy of hypnosis for various health conditions in which sleep was targeted as a primary or secondary outcome. This review aimed to investigate the effects of hypnosis interventions on sleep, to describe the hypnotic procedures, and to evaluate potential adverse effects of hypnosis.
Methods:
We reviewed studies (prior to January 2017) using hypnosis in adults for sleep problems and other conditions comorbid with sleep problems, with at least one sleep outcome measure. Randomized controlled trials and other prospective studies were included.
Results:
One hundred thirty-nine nonduplicate abstracts were screened, and 24 of the reviewed papers were included for qualitative analysis. Overall, 58.3% of the included studies reported hypnosis benefit on sleep outcomes, with 12.5% reporting mixed results, and 29.2% reporting no hypnosis benefit; when only studies with lower risk of bias were reviewed the patterns were similar. Hypnosis intervention procedures were summarized and incidence of adverse experiences assessed.
Conclusions:
Hypnosis for sleep problems is a promising treatment that merits further investigation. Available evidence suggests low incidence of adverse events. The current evidence is limited because of few studies assessing populations with sleep complaints, small samples, and low methodological quality of the included studies. Our review points out some beneficial hypnosis effects on sleep but more high-quality studies on this topic are warranted.
Citation:
Chamine I, Atchley R, Oken BS. Hypnosis intervention effects on sleep outcomes: a systematic review. J Clin Sleep Med. 2018;14(2):271–283.
Keywords: hypnosis, hypnotherapy, nonpharmacological, sleep disturbance, systematic review
INTRODUCTION
Up to 35% to 40% of the adult population in the United States suffers from sleep disturbances.1,2 Sleep problems may be precursors to many health issues, including cardiovascular disease, diabetes, mental health problems, and dementia.3–6 Therefore, timely treatment of sleep disturbances can contribute to prevention and modification of many health conditions often comorbid with sleep problems.
Conventional methods for treating sleep problems include pharmacological and nonpharmacological approaches. Sedative-hypnotic medications are commonly prescribed for sleep problems7; however their long-term effects remain unclear.8 Among nonpharmacological approaches, cognitive behavioral therapy for insomnia (CBT-I) has been endorsed as a first-line treatment for chronic sleep problems.8 Despite these choices the general public has a growing interest in pursuing integrative medicine approaches to complement conventional methods for alleviating sleep problems,9–11 due to a common perception that integrative medicine approaches are safe and cost-effective. One such approach is hypnosis, the state of consciousness that involves focused attention and reduced peripheral awareness and that brings about an enhanced capacity for response to suggestion.12 Hypnosis is appealing to clinicians and patients because it is typically brief and can provide long-term symptom relief; furthermore, this approach can be tailored to match the health complaint and patient characteristics.
Hypnosis has gained recognition as an effective therapy for managing pain and for relieving cancer treatment side effects and stress-related disorders.13–16 However, the evidence highlighting specific benefits of hypnosis for sleep problems is scarce.11,17 The most recent review and meta-analysis assessing the efficacy of randomized controlled trials (RCTs) that evaluated the effect of hypnotherapy on sleep disorders included 13 studies (6 assessing hypnotherapy and 7 assessing autogenic training or guided imagery, comprising 503 participants).17 Eleven of the included studies were of low methodological quality. This meta-analyses indicated hypnotherapy and hypnotherapy-like treatments shortened sleep latency compared to waitlist but not to sham intervention. Overall, the review and meta-analysis indicated some positive effects of hypnosis interventions on sleep. However, due to low sample size and methodological limitations the authors questioned the general-izability of the positive results and called for more research in this area because of the few rigorous RCTs to provide convincing generalizable evidence.17
In addition to RCTs focusing specifically on sleep problems, there has been a growing body of research focusing on conditions often comorbid with sleep problems (eg, pain, posttraumatic stress disorder [PTSD]), in which sleep was included as an outcome measure. This body of research is also of interest in evaluating hypnosis and its effects on sleep. Further, evaluating studies with other prospective designs may be of value to clarify the benefits of hypnotherapy for sleep outcomes.
The objective of this systematic review was to further describe and evaluate the available evidence on hypnosis for sleep improvement. Our goals also included describing the intervention procedures (eg, duration, techniques) and assessing adverse experiences associated with the hypnosis. To reach our objectives, we included RCTs and other study designs that tested hypnosis for sleep problems or a health condition co-morbid with sleep problems to gain a more comprehensive perspective on procedures and adverse effects potentially linked to hypnosis.
METHODS
Literature Search
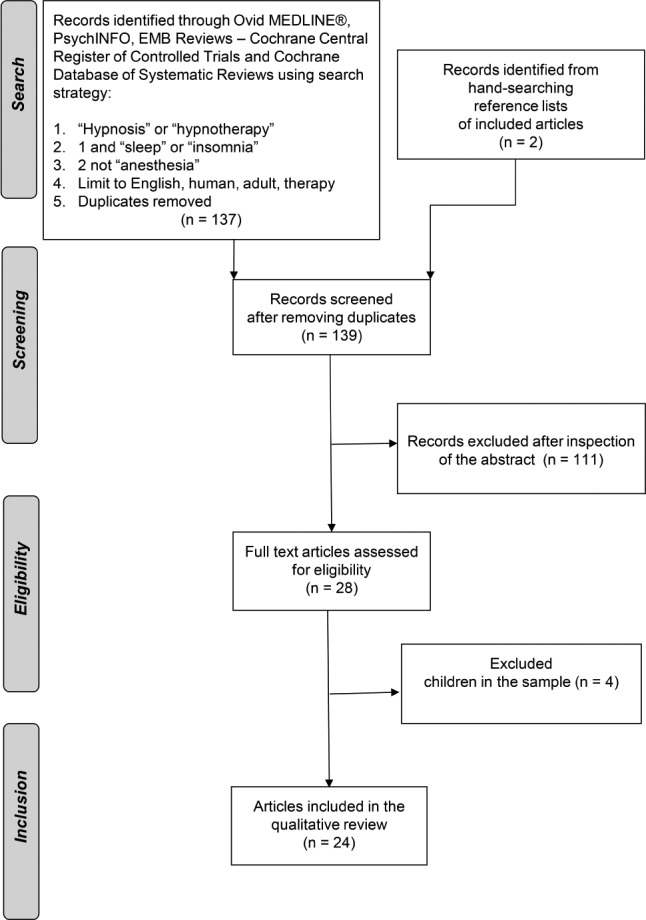
Records of Ovid MEDLINE, PsychINFO, EMB Reviews, and Cochrane Central Register of Controlled Trials and Cochrane Database of Systematic Reviews were searched to include the work published before January 12, 2017. The search strategy is described in Figure 1.
Figure 1. Search strategy and study inclusion.
Study Selection and Classification
Inclusion criteria were: (1) primary research published in English in a peer-reviewed scientific journal; (2) RCTs or prospective studies with at least 10 subjects; (3) included adults (18 years or older), regardless of health conditions; (4) outcomes of interest included measurable objective or subjective data reflecting sleep quality; and (5) hypnosis or hypnotherapy studied alone or as a part of a multicomponent intervention. Only interventions defined as “hypnosis,” “hypnotherapy” or “hypnotic” were considered. Approaches such as guided imagery or relaxation methods often used along with hypnosis were not included in this review on their own unless described as “hypnotic” to minimize heterogeneity in intervention approaches and to ensure that the interventions were likely to result in development of a hypnotic state with an increased capacity for response to suggestion inherent in hypnosis definition.12 The full text of studies meeting the inclusion/exclusion criteria, the relevant review articles, and the articles with insufficient information to determine eligibility from the abstract were retrieved and reviewed by two authors for determination for inclusion in this review (Figure 1).
Methodological Quality Assessment
The methodological quality of the included publications was evaluated using the modified Scale for Assessing Scientific Quality of Investigation-Complementary and Alternative Medicine (SASQI-CAM) version.18 The scale was derived from previous work19 with several items added for improving the quality of research on CAM and integrative medicine approaches based on expert suggestions.20,21 This modified 19-item scale has scores ranging from zero to 20, and it is specifically adapted to take into account special features of integrative medicine research (eg, challenges in blinding participants to the study interventions). A SASQI-CAM score higher than 9 is considered to be of sufficient scientific quality.22 Two reviewers independently assessed the risk of bias of each study in accordance with the guidelines provided for complementary and integrative approaches.18 Any discrepancies were resolved by consensus.
Data Extraction and Ratings
Both quantitative and qualitative data related to the study characteristics and outcome measures of interest were extracted for this review. For each study, data were extracted by one of the trained staff and then reviewed by a second member. Again, any discrepancies were resolved by consensus. The following data were collected: type of study, country where study was conducted, medical condition, number of participants, mean age, sex, whether sleep was primary or secondary outcome, hypnosis provider qualifications, hypnosis intervention type, intervention procedures, intervention length, length of trial, control groups, follow-up periods, rate of intervention completion, outcome measures, and results at postintervention and follow-up.
The outcomes were classified as positive when ≥ 50% of assessed sleep items had values of P < .05 or were described as more effective compared to a control group, mixed when fewer than 50% of measured items were positive; and negative when no group improved or both intervention and control groups improved but were not significantly different from each other.
RESULTS
Overview of the Included Studies
We identified 139 studies via searches, of which 24 met our inclusion criteria.23–46 The data from these publications were synthesized for qualitative analyses. Quantitative analyses and meta-analytical techniques were not applied due to heterogeneity related to the diversity of assessed populations and health conditions, as well as wide variability in hypnosis interventions and outcome measures.
Table 1 provides more detailed information about the included studies. The included studies were published between 1973 and 2016. More than half of the included studies (54.2%) were conducted in the United States, with the rest conducted in European countries (37.5%) including Denmark, England, France, Spain, and Switzerland; or countries in other regions (8.3%) including Australia, Canada, and Israel. The included studies collectively assessed 1,330 participants. The average study sample size was 55.3 (standard deviation = 43.7) with the range of 14 to 187. The participants' ages ranged from 18 to 83 years (weighted average for the 19 studies where participants' ages were reported was 41.2 years), and typically most of the participants for whom the sex was reported were women (mean = 66.1%, range 21% to 100%). The studies assessed participants with diverse health conditions including insomnia or other sleep complaints (eg, sleep walking or sleep terror), depressive symptoms, PTSD, cancer, chronic pain conditions including low back, orofacial, temporomandibular pain, irritable bowel syndrome, and fibromyalgia. Studies also enrolled participants suffering from hot flashes, as well as healthy participants, including college and medical students. Most of the included studies (66.7%) did not require sleep complaints for study inclusion.
Table 1.
Description of the included studies.
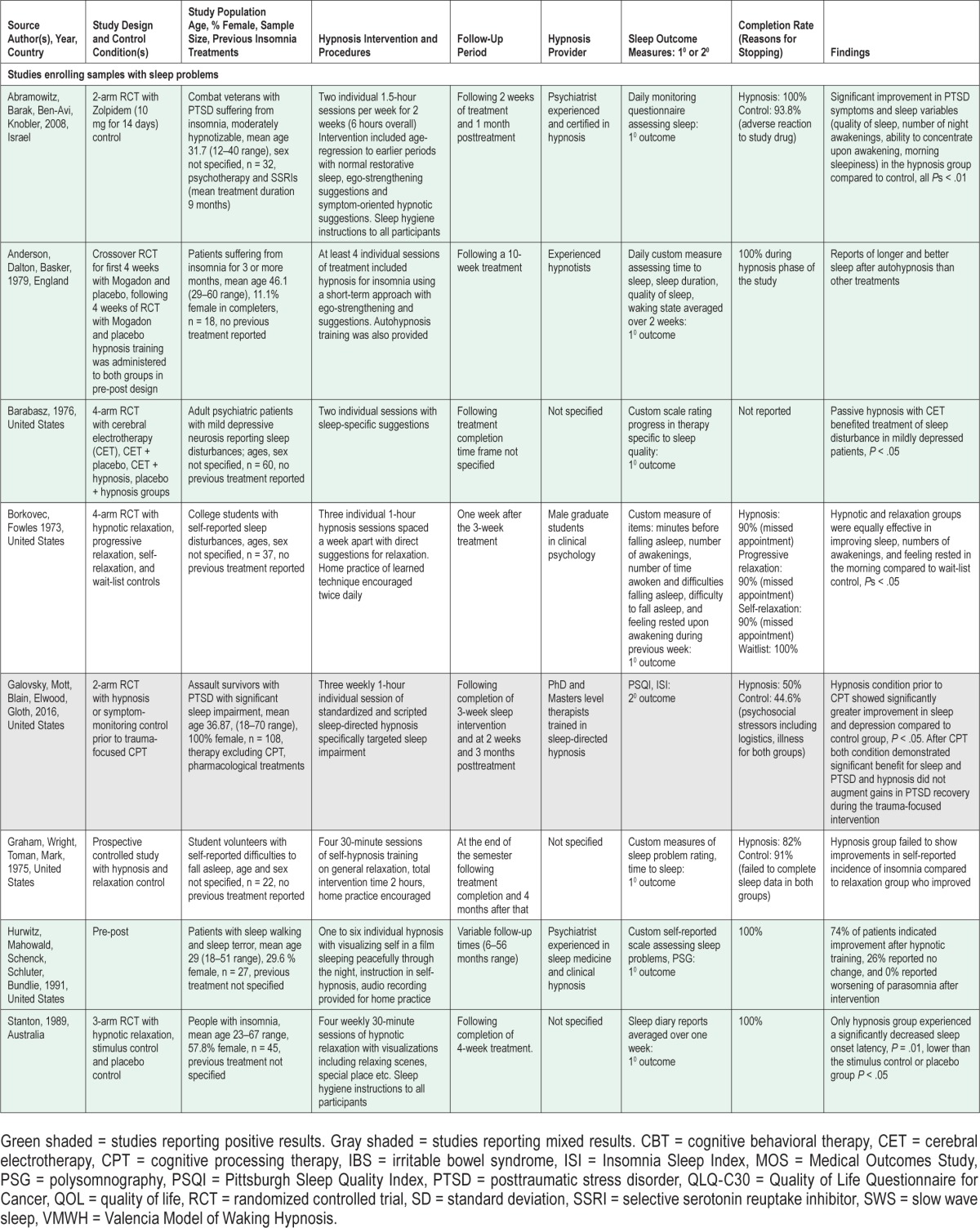
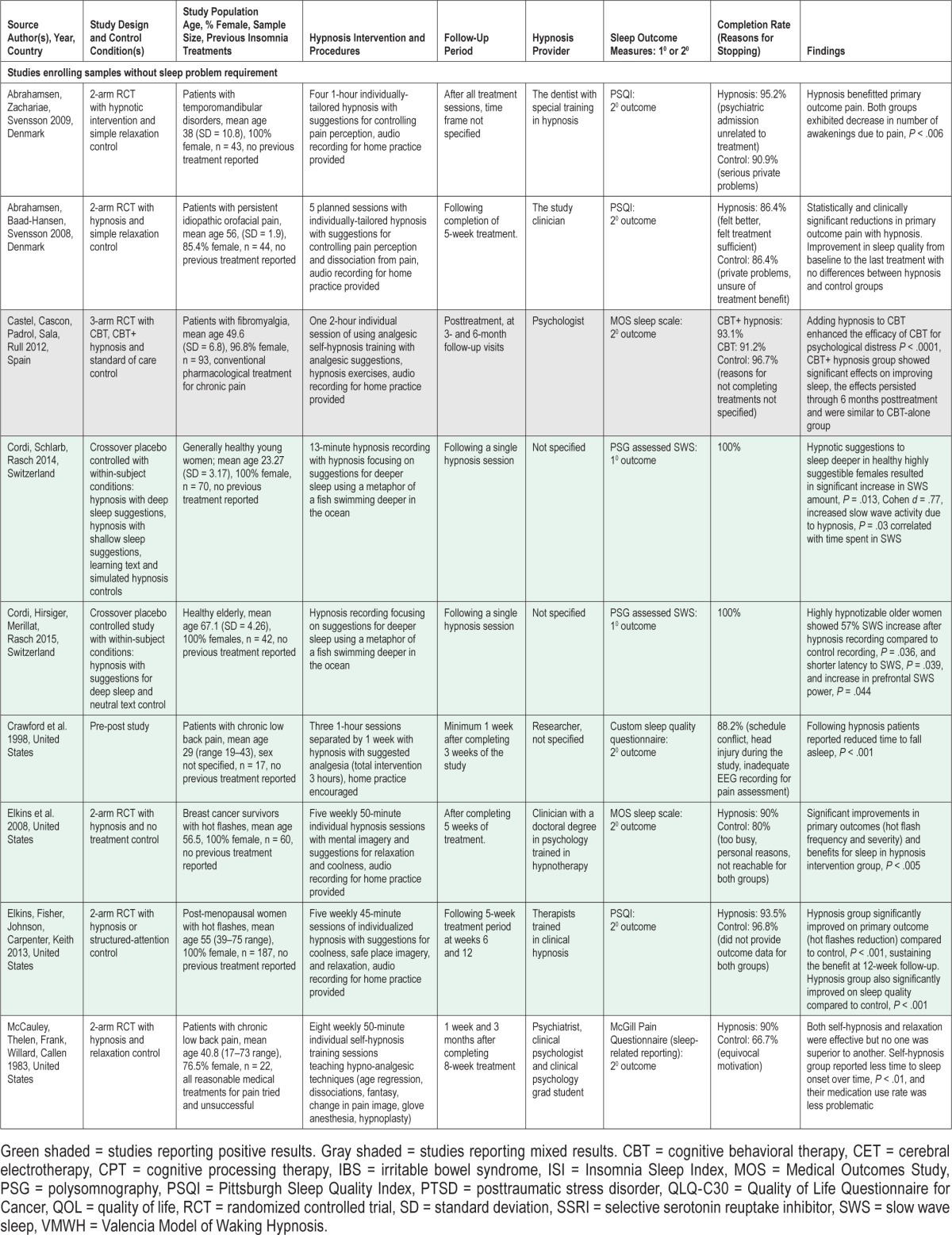
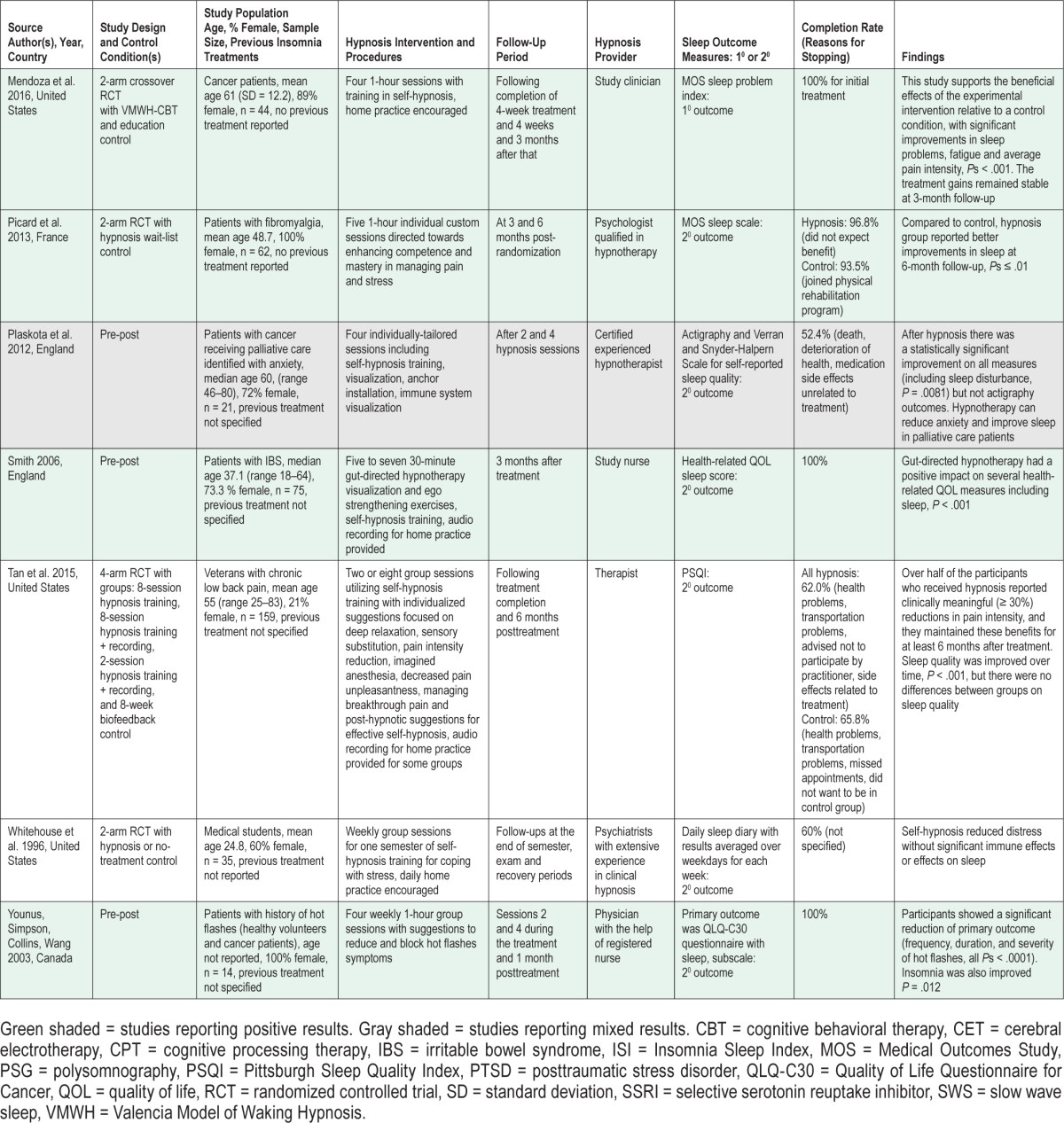
Among the controlled studies (75.0% of all included studies), 72.2% used active control groups (eg, relaxation, sedative-hypnotic medication, therapy, simple monitoring, structured attention, education, stimulus response), 16.7% employed non-active control groups (eg, standard treatment, waitlist), and 11.1% employed both active and nonactive control groups.
Sleep-related outcomes were primary in 50% of the included studies. The outcomes ranged from objective sleep assessment using polysomnography to custom sleep diaries. Most commonly used sleep assessments were the Pittsburgh Sleep Quality Index (PSQI)47 and the Medical Outcomes Survey (MOS) sleep problem index.48 Both instruments assess several dimensions of sleep quality (eg, sleep initiation, maintenance, etc.) over the previous month; both PSQI and MOS have been shown to have adequate reliability and validity in various settings and with diverse populations47,49–53 and are intended to be standardized sleep assessments for clinicians and researchers. The custom instruments used in 29.2% of the included studies were primarily diary-like assessments; however, it is difficult to ascertain the exact nature of the assessed outcomes when such custom instruments have been used.
Forty-five percent of the included studies assessed hypnosis effects not only immediately following the intervention but also included additional follow-up assessments. Follow-up periods ranged from 1 month to 24 months postintervention.
Methodological Quality Assessment
Of the included studies, 58.3% were RCTs. This review included other controlled trials such as within-subject crossover studies30,31 (16.7%), pre-post prospective observational studies32,37,41,42,46 (20.8%), and one RCT in which both arms underwent hypnosis following the completion of other treatments conditions.26 This RTC was considered pre/post in regard to the hypnosis portion of the intervention.26
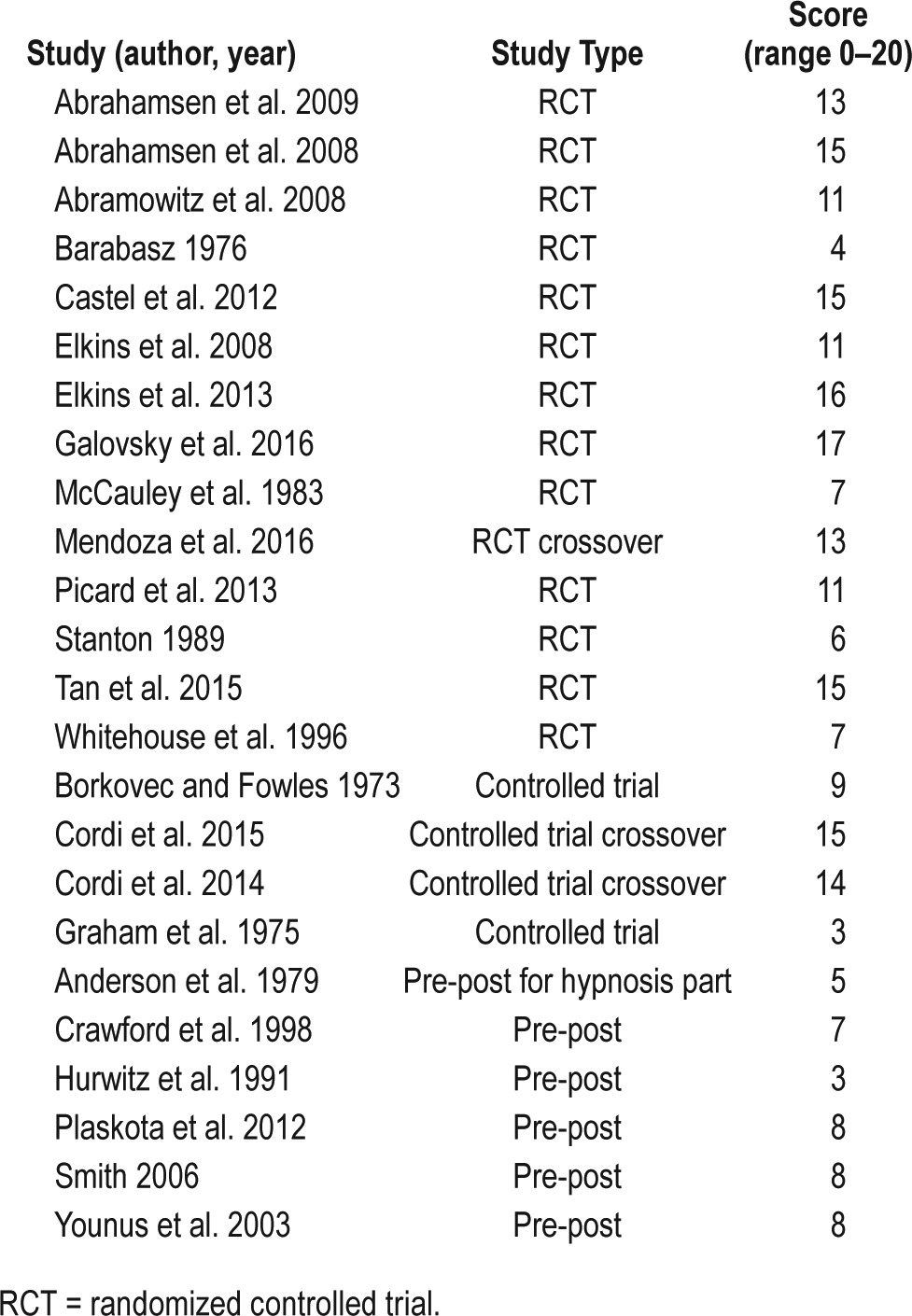
The mean overall SASQI-CAM score18 of the included studies was 10 out of 20 possible (standard deviation = 4.3) and the range was 3 to 17. The most commonly missed quality items were SASQI-CAM item 6, related to assessing subject's expectations of benefits from the intervention, with only one publication33 explicitly describing this, and item 10, which focused on monitoring and reporting side effects and adverse events; this information was included in only 2 publications.33,39 More recently published work received higher methodological quality scores compared to earlier research (Table 2).
Table 2.
Methodological quality of the included studies.
Comparison of Positive, Mixed, and Negative Studies
Of 24 of the included studies, more than half (58.3%) reported a positive effect of the hypnosis intervention on the assessed sleep outcome over time. Mixed results indicating improvements in some but not all sleep outcomes were presented in 12.5% of the included studies. The rest of the publications (29.2%) demonstrated negative results, with no effects of hypnosis or comparable effects of hypnosis and control conditions on sleep outcomes.
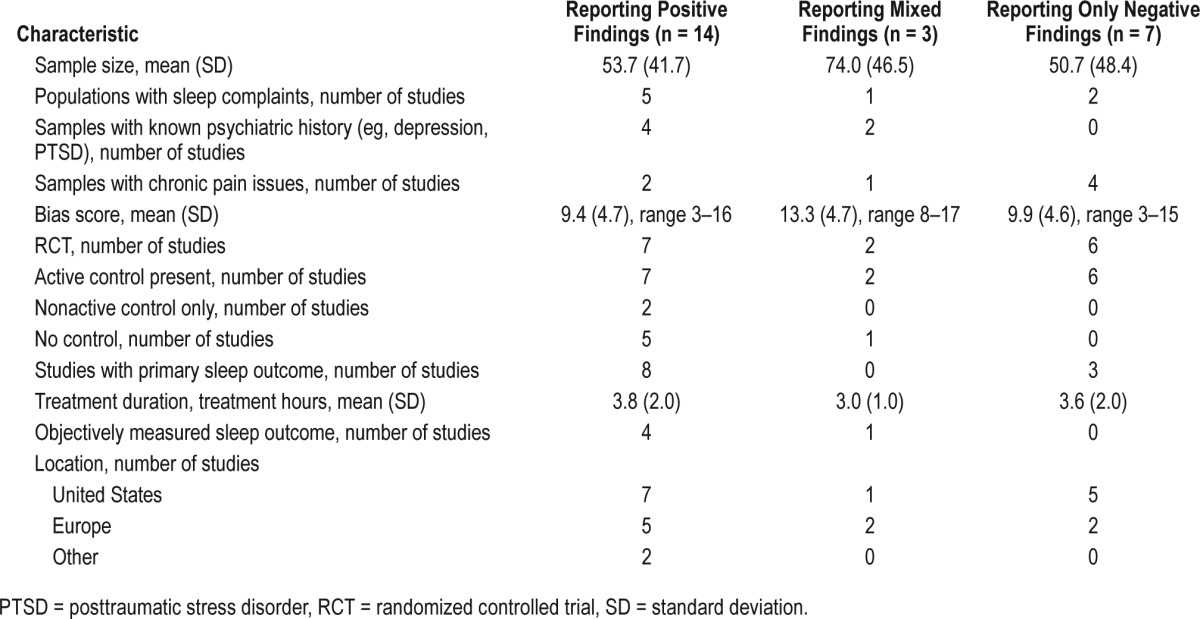
Table 3 presents comparisons of the positive, mixed, and negative studies on several variables. Positive and negative studies had similar average methodological quality scores (presented as mean ± standard deviation: 9.4 ± 4.7 and 9.9 ± 4.6, respectively), average sample size (53.6 ± 43.2 and 50.7 ± 48.4, respectively), and average intervention duration (3.8 ± 2.0 and 3.6 ± 2.0 hours, respectively). Among studies with negative hypnosis effects on sleep outcomes, 85.7% were RCTs and 85.7% used an active control group. Among the studies reporting positive effects, only 50% were RCTs, and an active control group was used in 50% of the positive studies, with 14.3% using a nonactive control group and 35.7% employing no control group. Samples with sleep complaints were recruited in 35.7% of the studies reporting a positive effect of hypnosis on sleep and in 28.6% of the studies reporting negative hypnosis effects on sleep. Next, sleep was the primary outcome in 57.1% of the studies showing benefits of hypnosis for sleep and in 42.9% of the studies showing no hypnosis effect on sleep.
Table 3.
Comparisons between positive, mixed, and negative studies.
Description of the Subset of Studies Targeting Sleep
Only one-third of the reviewed studies had inclusion criteria requiring participants to have sleep disturbances. Considering only the studies recruiting samples with sleep problem, most of them (62.5%) reported positive findings, 12.5% reported mixed results, and 25.0% reported negative results. All except one of these studies were controlled, and two studies focused on mechanistic aspects of hypnosis for sleep outcomes rather than efficacy. Table 4 shows comparisons of the positive, mixed, and negative studies that enrolled samples with sleep disturbances. Average sample sizes were 36.4 ± 14.7, 108.0 ± 0, and 29.5 ± 7.5 for positive, mixed, and negative studies, respectively. Average probability of bias based on SASQI-CAM scoring appeared similar and high for studies reporting benefit of hypnosis on sleep and studies reporting no benefits of hypnosis on sleep outcomes (6 ± 3.2, and 6 ± 3.0, respectively). Treatment duration averaged 2.5 ± 2.5 for positive and 2.5 ± 0.5 for negative studies. Most of the studies enrolling samples with sleep problems assessed sleep with subjective assessments, except one study reporting positive outcomes of hypnosis on sleep.
Table 4.
Information about the subset of studies enrolling samples with sleep complaints.
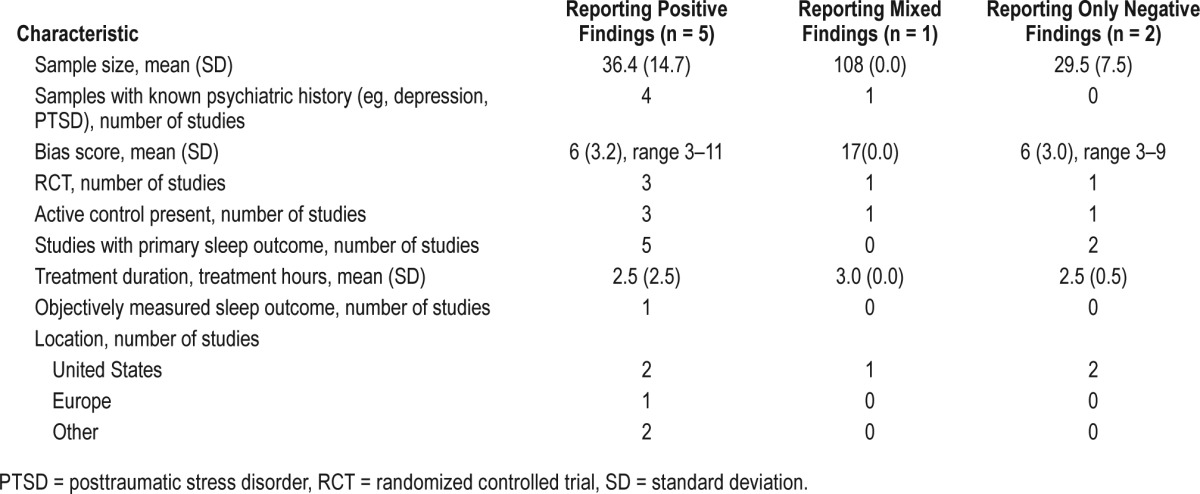
Eighty percent of the positive studies from this subset recruited samples with psychiatric comorbidities such as PTSD, anxiety, or depression; none of the studies reporting negative results indicated significant comorbidities in their participants. Sleep was the primary outcome in 62.5% of the studies showing benefits of hypnosis for sleep and in both of the studies showing no hypnosis effect on sleep.
Description of the Subset of Studies with SASQI-CAM Scores Indicating Lower Risk of Bias
Twelve of the included studies received a score higher than 9 on SASQI-CAM, indicating adequate study quality and lower risk of bias.22 The patterns observed for this subsample of the reviewed publications paralleled those observed for the full sample. Seven studies (58.3%) demonstrated an overall positive effect of the hypnosis intervention on the assessed sleep outcome. Two studies (16.7%) showed mixed results, indicating improvements in some but not all sleep outcomes. The remaining three studies (25%) demonstrated negative results, with no beneficial effects of hypnosis or comparable effects of hypnosis and control conditions on sleep outcomes.
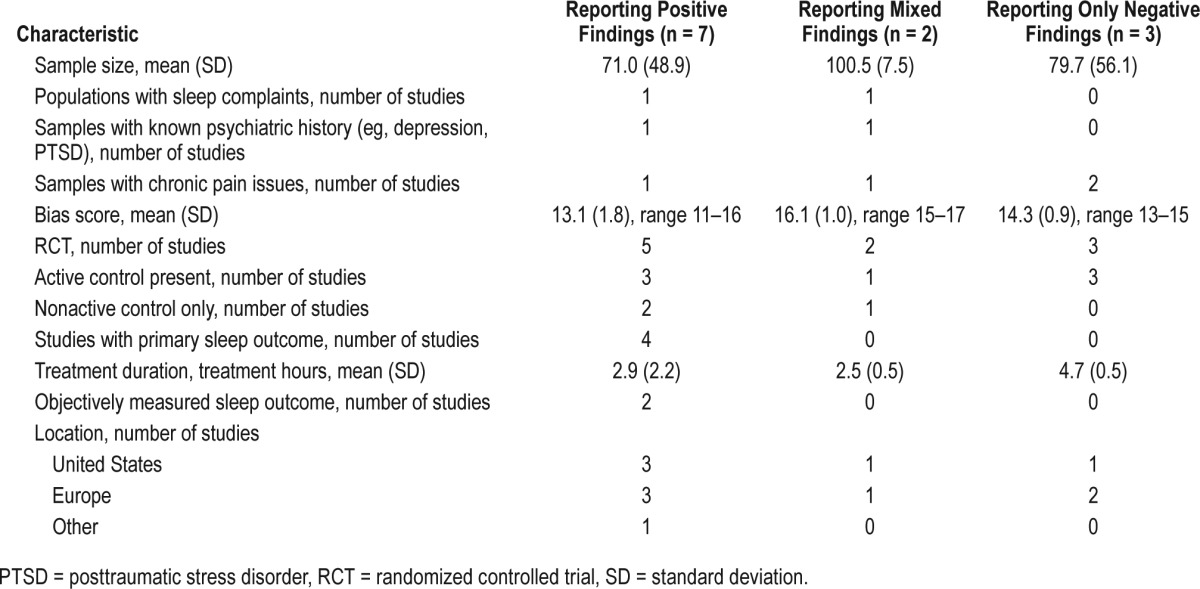
Table 5 presents comparisons of the positive, mixed, and negative studies scoring higher than 9 on SASQI-CAM on several variables. Positive and negative studies had similar average sample size (71.0 ± 48.9 and 79.7 ± 56.1, respectively), but average intervention duration was 2.9 ± 2.2 hours for positive studies and 4.7 ± 0.5 hours for negative studies. Except for two crossover placebo-controlled studies reporting positive results, the rest of the high-quality studies were RCTs. All high-quality studies used a control group, with most including active controls. Samples with sleep complaints were recruited in one of the studies reporting a positive effect of hypnosis on sleep and in none of the studies reporting negative hypnosis effects on sleep. Next, sleep was the primary outcome in 57.1% of the studies showing benefits of hypnosis for sleep and in none of the studies showing no hypnosis effect on sleep.
Table 5.
Information about the subset of studies with lower risk of bias (SASQI-CAM score higher than 9).
Hypnosis Intervention Procedures
Hypnosis is an approach that can be easily customized and adapted to a client with the choice of specific hypnosis techniques and individualized suggestions, and it also can be added to another therapy. This flexibility is one of the attractive features of this therapeutic approach. In most included studies (79.2%), hypnosis was used as a stand-alone intervention and the remaining studies combined hypnosis with another therapeutic intervention (eg, cognitive behavioral therapy, cognitive processing therapy). Few of the included studies (8.3%)25,43 reported using sleep hygiene instructions along with hypnosis training. The studies varied greatly in the lengths of hypnosis intervention: from 13-minute audio recordings with hypnosis for deep sleep to 8 sessions of hypnosis, each lasting 1 hour. Most of the studies (83.3%) used individual hypnosis sessions. Two of the included studies (8.3%) used group hypnosis sessions45,46 and the remaining 8.3% of the studies used an audio recording only.30,31 The number of sessions averaged 4 ± 1.2 (range, 1 to 8), with the total time spent in intervention averaging 3.6 ± 1.9 hours (0.23- to 8-hour range).
Home practice was encouraged in 54.2% of the included studies, with most of these studies offering audio recordings for such a practice. Adherence to the home practice instructions was not typically assessed.
One included study44 compared different hypnosis treatment packages and their effects on pain and sleep quality outcomes. The findings indicated no significant effect of hypnosis on sleep outcomes but showed that after hypnosis participants had a significantly greater reduction in the study primary outcome (pain intensity) than after control biofeedback treatment. Interestingly, there was no significant difference among the three hypnosis conditions (8 self-hypnosis group training sessions with audio recordings for home practice, 8 self-hypnosis group training sessions without recordings, or 2 self-hypnosis group training sessions with audio recordings for home practice and weekly reminder telephone calls). The authors concluded that two sessions of self-hypnosis with audio recordings for home practice may be as effective as 8 sessions of hypnosis treatment for pain management. It is of interest to assess the optimal number of sessions of sleep-focused hypnotherapy for individuals with sleep problems.
The hypnosis interventions described in the review targeted sleep disturbance (25%), pain symptoms (29.2%), and immune system (4.2%), focused on increase of relaxation and reduction stress (12.5%), symptoms associated with hot flashes (12.5%), and the remaining studies provided no specific intervention focus.
For studies specifically targeting insomnia symptoms, hypnosis approaches involved using a metaphor of a fish going deeper into the water for deeper sleep, using an age-regression technique prompting the participant to focus on his or her earlier memories of periods when restorative sleep could be easily achieved, providing directions for relaxation with visualizations including relaxing scenes, and delivering ego-strengthening suggestions.
In the studies targeting pain symptoms, suggestions included instructions for dissociating from pain, controlling pain perception, imagined analgesia, decreased pain unpleasantness, and managing breakthrough pain. Hypnoanalgesic techniques taught in the studies included age regression, dissociations, fantasy, changing pain image, glove anesthesia, and hypnoplasty. Hypnosis for reducing hot flashes symptoms incorporated suggestions for relaxation and coolness. Also commonly included were suggestions for relaxation, safe place imagery, coping with stress, and suggestions for effective hypnosis practice. Several studies (20.8%) specified that the sessions were individually tailored with customized suggestions.
Hypnotic susceptibility was assessed and reported in 37.5% of the included studies. In these studies, the assessment was completed with the Harvard Group Scale of Hypnotic Susceptibility54 (55.6%), Stanford Hypnotic Susceptibility Scale55,56 (33.3%), or the Hypnotic Induction Profile57 (11.1%). Some studies found that only highly susceptible participants benefitted from hypnotic suggestions for sleep improvement and those with low hypnotic susceptibility did not.30,31 The authors of one study indicated that participating in hypnotic susceptibility assessment prior to intervention might have influenced the participants' expectations for success in hypnosis.36 The other studies reported no effect of hypnotic susceptibility on sleep outcomes. Most of the studies assessed in this review did not include the assessment of hypnotic susceptibility or tested its relation to the study outcomes.
Adverse Event Reporting
One of the goals of this review was to assess adverse events in the published studies utilizing hypnosis. Hypnosis is typically described as the form of treatment with low or no associated side effects58; however, the practitioners of hypnosis are often cautioned that hypnosis may cause unpleasant side effects that may include dizziness, confusion, unpleasant somatic symptoms, false memories, or panic attacks in some people.59 The risk of moderate to severe after-effects of hypnosis was previously estimated to be 7% in research and clinical samples but it is believed that adverse events due to hypnosis may be underreported in clinical settings because these complications are typically short-lived.60 Therefore, the true incidence of such adverse events is not clear. The evidence from this review suggests that few studies utilizing hypnosis interventions report monitoring or assessing adverse experiences. Only two reviewed studies39,61 totaling 231 participants mentioned some form of monitoring of adverse events. All reported no adverse experiences associated with hypnosis. One study,36 though not specifically assessing adverse experiences, reported that some people in the hypnosis group showed general dissatisfaction with the procedure.
DISCUSSION
Overview of the Qualitative Analyses
Overall, more than half of the included studies indicated some positive effects of hypnosis on sleep outcomes. However, the body of evidence, in general, was of variable methodological quality. The studies reporting positive findings had a similar average methodological quality and sample sizes compared to those reporting negative hypnosis effects. However, on the one hand, more than 80% of the negative studies were controlled trials and a similar percentage had an active control group compared to only half of the positive studies having an RCT design and using an active control group. On the other hand, the studies reporting positive effects of hypnosis on sleep outcomes were more likely to have a sample with sleep problems and focus on a sleep outcome as a primary outcome measure. The results regarding outcomes were similar when only a subgroup of studies with samples experiencing sleep problems was considered. Furthermore, when only a subset of studies with higher SASQI-CAM scores indicating sufficient quality of the study was considered, the patterns were similar to those observed in the whole sample.
The hypnosis interventions were primarily delivered as separate treatment programs in several individual sessions with increasing interest in using tailored suggestions. Using sleep hygiene instructions along with hypnosis was reported in few hypnosis interventions for sleep improvement. For the studies targeting sleep and conditions affected by sleep (pain, stress, hot flashes) home practice was encouraged in most of the included studies, though adherence to such practice and its influence on the outcomes was rarely assessed. In studies that reported hypnosis provider, the interventions were delivered by a trained clinical professional with training and expertise in clinical hypnosis. The adverse event rate was very low given that more than 200 participants from two RCTs reported no adverse events; however, the information about adverse events was not reported in most studies.
Implications for Clinical Practice
A recent review assessing efficacy, safety, and applications of medical hypnosis did not list sleep problems among the suggested potential applications of medical hypnosis in daily clinical practice.58 The reason for this may be that, to date, rigorous research evaluating hypnosis interventions for sleep disturbances is lacking. Our review indicates that hypnosis may be a promising approach for sleep improvement that merits further investigation.
Several attractive features of hypnosis supported by the presented evidence should be highlighted. First, successful hypnosis interventions for sleep may be relatively short. Our review indicates that on average, 3 to 4 sessions were sufficient to obtain benefits for sleep outcomes in the studies reporting positive effects of hypnosis on sleep. The minimum number of sessions needed for an effective treatment remains open for debate and may depend on individual tailoring, with evidence leaning towards multiple (3 to 5) sessions with an individually tailored treatment plan. Though most of the studies reporting benefits of hypnosis on sleep were using individual sessions, benefits of hypnosis were also observed in studies utilizing group sessions and audio recording only, highlighting that sleep improvements can be achieved with more efficient interventions. The research also suggests that home practice supported by audio recordings of sessions may boost the efficacy of treatment and reduce the number of treatment sessions.
Second, hypnosis is a flexible approach with a big toolbox of techniques that can be tailored to the specific individual and their symptoms. Our review indicates that beneficial hypnosis for sleep improvement included sleep-specific suggestions, suggestions for relaxation and stress reduction, and age regressions. Another promising strategy for hypnosis treatment for sleep improvement may be an inclusion of ego-strengthening suggestions in the treatment sessions. These suggestions that are not focusing on specific sleep symptoms may be beneficial for improving therapeutic alliance, achieving heightened insight and better self-esteem in the patients and thus optimizing the treatment effects from hypnosis.62 Sleep hygiene instructions may also be included in a hypnosis treatment program for sleep improvement. Though inclusion of sleep hygiene instructions was not commonly reported in the studies included in the review, sleep hygiene may boost treatments targeting sleep.63
Next, though hypnotic susceptibility is believed to be important in how people respond to hypnosis, few included studies assessed it. The data are not conclusive about the role of hypnotic susceptibility in the success of the hypnotic interventions. Only some studies showed the importance of hypnotic susceptibility for the success of the intervention30,31 whereas others failed to show it or did not assess it. It was also suggested that patients in the midrange of hypnotic susceptibility may be the most appropriate clients for hypnosis treatments for some health conditions,25 but this aspect needs further investigation.
Further, hypnosis appears to be an approach with a low incidence of adverse effects. Though only a few studies reported adverse event monitoring in this review, those that included this information reported no adverse events. Additionally, a high rate of completion of the hypnosis interventions observed in the included studies (Table 1) suggests general acceptance of this modality by patients and study participants. Sleep problems are typically treated with sleep medications that have known unpleasant side effects and have an unknown efficacy for long-term use.2,7 These may be some of the reasons why those affected by sleep problems are likely to seek alternative approaches for management of insomnia.11 Empirical evidence from published research indicates either a beneficial effect of hypnosis interventions on sleep or hypnosis effects comparable to those of control interventions with a low rate of adverse experiences from hypnosis. Therefore, this approach may be important to explore further for its utility for treating sleep problems especially in populations in which using pharmacological treatments may be undesirable (eg, children, elderly, patients with multiple comorbidities, etc.)
Currently, a nonpharmacological approach of choice for treating insomnia is CBT-I.8,64 A recent systematic review and meta-analysis evaluating cognitive behavioral therapies for treatment of insomnia indicated that CBT-I is efficacious for some but not all dimensions of sleep problems.64 Though CBT-I has been considered a reliable treatment for chronic insomnia for the past 25 years, some limitations noted in the recent work include the need for 5 or more sessions of therapy to observe most optimal response and a shortage of trained therapists to provide the CBT-I.8,64 Hypnosis can be provided by any clinician (physician, nurse, psychologist) trained in hypnotherapy, and diverse patient populations can be trained to induce beneficial changes in health using self-hypnosis without the presence of a clinician as demonstrated in previous research assessing hypnosis for other health issues.33,65–69 Further, hypnosis is extremely flexible and can be performed in different settings (not just as individual, group, or on-line sessions similar to CBT-I but also as audio recorded sessions); the studies included in this review indicate that a beneficial effect can be obtained in four or fewer sessions with hypnosis; however, the optimal number of sessions for best results is yet to be determined. To date, the rigorous research directly comparing efficacy and cost-effectiveness of CBT-I and hypno-therapy for sleep is scarce. Of interest, few studies evaluating interventions combining cognitive therapy approaches with hypnosis indicate beneficial synergistic effects,29,39,70 suggesting that hypnosis might be a useful adjunct therapy for other psychotherapy approaches.
Our review indicates that research on using hypnosis for sleep problems is still in the early stages. Because of several attractive features of hypnosis previously described and promising research to date showing potential benefits of hypnosis in the absence of serious adverse events, hypnosis for sleep disorders deserves further evaluation.
Limitations
The review is limited in several respects. The included studies assessed relatively small samples of predominantly middle-aged female participants who may or may not have sleep complaints. Therefore, it is not clear how these results can be applied to the general population of individuals experiencing sleep problems.
Our selection procedures included filtering results based on language (English only). Furthermore, we allowed hypnosis interventions to focus on conditions other than sleep as long as sleep outcomes were included in the data. All of these issues may have affected the generalizability of these results to the general population with sleep problems.
Another limitation is the methodological diversity of the studies and the extent of bias of the included studies. Our review search strategy cast a broad net to include studies that reported at least one sleep-related outcome. Overall the quality of the included research was modest, with only half of the included studies receiving a score higher than 9, indicating lower risk of bias on SASQI-CAM. Only one-third of the studies included in this review recruited samples with sleep problems. Further, hypnosis intervention focused on sleep improvement in only a portion of the included studies; and several studies used interventions focused on pain, immune system, or hot flashes symptoms. We also included studies of different designs in addition to RCTs. Therefore, there was considerable heterogeneity in the included studies related to study samples, outcome measures, and clinical interventions, which complicates the qualitative analyses and interpretation of the results.
Additionally, though SASQI has been specifically designed for evaluating integrative medicine approaches and has been increasingly used in systematic reviews assessing efficacy of integrative approaches,18,22,71 its reliability and validity have yet to be formally assessed, thus potentially limiting objectivity of the study quality assessment.
Some limitations are specific to integrative medicine approaches such as hypnosis; for example, formal blinding of participants and clinicians to treatment arms is not always possible in trials assessing mind-body approaches. Thus, the extent to which the awareness of the group assignment affected the study outcomes is difficult to predict.
Recommendations for Future Research
Important future directions related to hypnosis include determining minimal effective dose (ie, the length of treatment) and delivery method (individual versus group versus recording), as well as the optimal combination of suggestions and techniques for sleep improvement hypnosis. Another important topic to explore is determining specific populations who would most likely benefit from hypnosis and specific populations for whom hypnosis is not an optimal intervention. Future studies must consider symptomatology, hypnotic susceptibility, expectancy, adherence to treatment, and other patient characteristics. Methodological quality of future research could be enhanced by careful selection of control conditions; assessment of participant expectancy of improvement; use of reliable sleep assessments; reporting adverse events; monitoring provider adherence to intervention protocols; reporting participant adherence to the intervention; providing detail on clinician qualifications in hypnosis; and use of longer follow-up periods to assess outcomes.
CONCLUSIONS
Despite the limitations associated with the current review and the overall state of research, hypnotherapy for sleep problems appears to be a promising treatment to explore with little evidence of any adverse events.
DISCLOSURE STATEMENT
Irina Chamine and Rachel Atchely were supported by the NIH-NCCIH T32 AT002688 grant. The authors have not entered any agreements with the funding organization that limited their ability to analyze data or publish this work. Barry Oken declares no financial support from any funding agency. The authors report no conflicts of interest. All authors have seen and approved the submitted manuscript.
ACKNOWLEDGMENTS
The authors thank Nathan Bodie for help with literature review and study selection, and Andy Fish for administrative support.
ABBREVIATIONS
- CAM
complementary and alternative medicine
- CBT
cognitive behavioral therapy
- CBT-I
cognitive behavioral therapy for insomnia
- CET
cerebral electrotherapy
- CPT
cognitive processing therapy
- IBS
irritable bowel syndrome
- ISI
Insomnia Sleep Index
- MOS
Medical Outcomes Survey
- PTSD
posttraumatic stress disorder
- PSG
polysomnography
- PSQI
Pittsburgh Sleep Quality Index
- QLQ-C30
Quality of Life Questionnaire for Cancer
- QOL
quality of life
- RCT
randomized controlled trial
- SASQI
Scale for Assessing Scientific Quality of Investigation
- SASQI-CAM
Scale for Assessing Scientific Quality of Investigation-Complementary and Alternative Medicine
- SD
standard deviation
- SSRI
selective serotonin reuptake inhibitor
- SWS
slow wave sleep
- VMWH
Valencia Model of Waking Hypnosis
REFERENCES
- 1.Hossain JL, Shapiro CM. The prevalence, cost implications, and management of sleep disorders: an overview. Sleep Breath. 2002;6(2):85–102. doi: 10.1007/s11325-002-0085-1. [DOI] [PubMed] [Google Scholar]
- 2.Morin CM, Benca R. Chronic insomnia. Lancet. 2012;379(9821):1129–1141. doi: 10.1016/S0140-6736(11)60750-2. [DOI] [PubMed] [Google Scholar]
- 3.National Institutes of Health NIH state-of-the-science conference statement on manifestations and management of chronic insomnia in adults. NIH Consens State Sci Statements. 2005;22(2):1–30. [PubMed] [Google Scholar]
- 4.Yaffe K, Laffan AM, Harrison SL, et al. Sleep-disordered breathing, hypoxia, and risk of mild cognitive impairment and dementia in older women. JAMA. 2011;306(6):613–619. doi: 10.1001/jama.2011.1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Budhiraja R, Roth T, Hudgel DW, Budhiraja P, Drake CL. Prevalence and polysomnographic correlates of insomnia comorbid with medical disorders. Sleep. 2011;34(7):859–867. doi: 10.5665/SLEEP.1114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Breslau N, Roth T, Rosenthal L, Andreski P. Sleep disturbance and psychiatric disorders: a longitudinal epidemiological study of young adults. Biol Psychiatry. 1996;39(6):411–418. doi: 10.1016/0006-3223(95)00188-3. [DOI] [PubMed] [Google Scholar]
- 7.Ford ES, Wheaton AG, Cunningham TJ, Giles WH, Chapman DP, Croft JB. Trends in outpatient visits for insomnia, sleep apnea, and prescriptions for sleep medications among US adults: findings from the National Ambulatory Medical Care survey 1999-2010. Sleep. 2014;37(8):1283–1293. doi: 10.5665/sleep.3914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.McCall WV. Cognitive behavioral therapy for insomnia (CBT-I): what is known, and advancing the science by avoiding the pitfalls of the placebo effect. Sleep Med Rev. 2017 May 5; doi: 10.1016/j.smrv.2017.05.001. [Epub ahead of print]. doi: 10.1016/j.smrv.2017.05.001. [DOI] [PubMed] [Google Scholar]
- 9.Barnes PM, Bloom B, Nahin R. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;(12):1–23. [PubMed] [Google Scholar]
- 10.Pearson NJ, Johnson LL, Nahin RL. Insomnia, trouble sleeping, and complementary and alternative medicine: analysis of the 2002 national health interview survey data. Arch Intern Med. 2006;166(16):1775–1782. doi: 10.1001/archinte.166.16.1775. [DOI] [PubMed] [Google Scholar]
- 11.Neuendorf R, Wahbeh H, Chamine I, Yu J, Hutchison K, Oken BS. The effects of mind-body interventions on sleep quality: a systematic review. Evid Based Complement Alternat Med. 2015;2015:902708. doi: 10.1155/2015/902708. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Elkins GR, Barabasz AF, Council JR, Spiegel D. Advancing research and practice: the revised APA division 30 definition of hypnosis. Am J Clin Hypn. 2015;57(4):378–385. doi: 10.1080/00029157.2015.1011465. [DOI] [PubMed] [Google Scholar]
- 13.Vanhaudenhuyse A, Gillet A, Malaise N, et al. Efficacy and cost-effectiveness: A study of different treatment approaches in a tertiary pain centre. Eur J Pain. 2015;19(10):1437–1446. doi: 10.1002/ejp.674. [DOI] [PubMed] [Google Scholar]
- 14.Adachi T, Fujino H, Nakae A, Mashimo T, Sasaki J. A meta-analysis of hypnosis for chronic pain problems: a comparison between hypnosis, standard care, and other psychological interventions. Int J Clin Exp Hypn. 2014;62(1):1–28. doi: 10.1080/00207144.2013.841471. [DOI] [PubMed] [Google Scholar]
- 15.Syrjala KL, Jensen MP, Mendoza ME, Yi JC, Fisher HM, Keefe FJ. Psychological and behavioral approaches to cancer pain management. J Clin Oncol. 2014;32(16):1703–1711. doi: 10.1200/JCO.2013.54.4825. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Park C. Mind-body CAM interventions: current status and considerations for integration into clinical health psychology. J Clin Psychol. 2013;69(1):45–63. doi: 10.1002/jclp.21910. [DOI] [PubMed] [Google Scholar]
- 17.Lam TH, Chung KF, Yeung WF, Yu BY, Yung KP, Ng TH. Hypnotherapy for insomnia: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Med. 2015;23(5):719–732. doi: 10.1016/j.ctim.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 18.Meeks TW, Wetherell JL, Irwin MR, Redwine LS, Jeste DV. Complementary and alternative treatments for late-life depression, anxiety, and sleep disturbance: a review of randomized controlled trials. J Clin Psychiatry. 2007;68(10):1461–1471. doi: 10.4088/jcp.v68n1001. [DOI] [PubMed] [Google Scholar]
- 19.Jeste DV, Dunn LB, Folsom DP, Zisook D. Multimedia educational aids for improving consumer knowledge about illness management and treatment decisions: a review of randomized controlled trials. J Psychiatr Res. 2008;42(1):1–21. doi: 10.1016/j.jpsychires.2006.10.004. [DOI] [PubMed] [Google Scholar]
- 20.Mason S, Tovey P, Long AF. Evaluating complementary medicine: methodological challenges of randomised controlled trials. BMJ. 2002;325(7368):832–834. doi: 10.1136/bmj.325.7368.832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Margolin A, Avants SK, Kleber HD. Investigating alternative medicine therapies in randomized controlled trials. JAMA. 1998;280(18):1626–1628. doi: 10.1001/jama.280.18.1626. [DOI] [PubMed] [Google Scholar]
- 22.D'Silva S, Poscablo C, Habousha R, Kogan M, Kligler B. Mind-body medicine therapies for a range of depression severity: a systematic review. Psychosomatics. 2012;53(5):407–423. doi: 10.1016/j.psym.2012.04.006. [DOI] [PubMed] [Google Scholar]
- 23.Abrahamsen R, Baad-Hansen L, Svensson P. Hypnosis in the management of persistent idiopathic orofacial pain--clinical and psychosocial findings. Pain. 2008;136(1-2):44–52. doi: 10.1016/j.pain.2007.06.013. [DOI] [PubMed] [Google Scholar]
- 24.Abrahamsen R, Zachariae R, Svensson P. Effect of hypnosis on oral function and psychological factors in temporomandibular disorders patients. J Oral Rehabil. 2009;36(8):556–570. doi: 10.1111/j.1365-2842.2009.01974.x. [DOI] [PubMed] [Google Scholar]
- 25.Abramowitz EG, Barak Y, Ben-Avi I, Knobler HY. Hypnotherapy in the treatment of chronic combat-related PTSD patients suffering from insomnia: a randomized, zolpidem-controlled clinical trial. Int J Clin Exp Hypn. 2008;56(3):270–280. doi: 10.1080/00207140802039672. [DOI] [PubMed] [Google Scholar]
- 26.Anderson JA, Dalton ER, Basker MA. Insomnia and hypnotherapy. J R Soc Med. 1979;72(10):734–739. doi: 10.1177/014107687907201007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barabasz AF. Treatment of insomnia in depressed patients by hypnosis and cerebral electrotherapy. Am J Clin Hypn. 1976;19(2):120–122. doi: 10.1080/00029157.1976.10403850. [DOI] [PubMed] [Google Scholar]
- 28.Borkovec TD, Fowles DC. Controlled investigation of the effects of progressive and hypnotic relaxation on insomnia. J Abnorm Psychol. 1973;82(1):153–158. doi: 10.1037/h0034970. [DOI] [PubMed] [Google Scholar]
- 29.Castel A, Cascon R, Padrol A, Sala J, Rull M. Multicomponent cognitive-behavioral group therapy with hypnosis for the treatment of fibromyalgia: long-term outcome. J Pain. 2012;13(3):255–265. doi: 10.1016/j.jpain.2011.11.005. [DOI] [PubMed] [Google Scholar]
- 30.Cordi MJ, Hirsiger S, Merillat S, Rasch B. Improving sleep and cognition by hypnotic suggestion in the elderly. Neuropsychologia. 2015;69:176–182. doi: 10.1016/j.neuropsychologia.2015.02.001. [DOI] [PubMed] [Google Scholar]
- 31.Cordi MJ, Schlarb AA, Rasch B. Deepening sleep by hypnotic suggestion. Sleep. 2014;37(6):1143–1152. doi: 10.5665/sleep.3778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Crawford HJ, Knebel T, Kaplan L, Vendemia JM, Xie M, Jamison S, Pribram KH. Hypnotic analgesia: 1. Somatosensory event-related potential changes to noxious stimuli and 2. Transfer learning to reduce chronic low back pain. Int J Clin Exp Hypn. 1998;46(1):92–132. doi: 10.1080/00207149808409992. [DOI] [PubMed] [Google Scholar]
- 33.Elkins G, Johnson A, Fisher W, Sliwinski J, Keith T. A pilot investigation of guided self-hypnosis in the treatment of hot flashes among postmenopausal women. Int J Clin Exp Hypn. 2013;61(3):342–350. doi: 10.1080/00207144.2013.784112. [DOI] [PubMed] [Google Scholar]
- 34.Elkins G, Marcus J, Stearns V, et al. Randomized trial of a hypnosis intervention for treatment of hot flashes among breast cancer survivors. J Clin Oncol. 2008;26(31):5022–5026. doi: 10.1200/JCO.2008.16.6389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Galovsky TE, Mott J, Blain LM, Elwood L, Gloth C. Augmenting CPT to improve sleep impairment in PTSD: a randomized clinical trial. J Consult Clin Psychol. 2016;84(2):167–177. doi: 10.1037/ccp0000059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Graham KR, Wright GW, Toman WJ, Mark CB. Relaxation and hypnosis in the treatment of insomnia. Am J Clin Hypn. 1975;18(1):39–42. doi: 10.1080/00029157.1975.10403769. [DOI] [PubMed] [Google Scholar]
- 37.Hurwitz TD, Mahowald MW, Schenck CH, Schluter JL, Bundlie SR. A retrospective outcome study and review of hypnosis as treatment of adults with sleepwalking and sleep terror. J Nerv Ment Dis. 1991;179(4):228–233. doi: 10.1097/00005053-199104000-00009. [DOI] [PubMed] [Google Scholar]
- 38.McCauley JD, Thelen MH, Frank RG, Willard RR, Callen KE. Hypnosis compared to relaxation in the outpatient management of chronic low back pain. Arch Phys Med Rehabil. 1983;64(11):548–552. [PubMed] [Google Scholar]
- 39.Mendoza ME, Capafons A, Gralow JR, et al. Randomized controlled trial of the Valencia model of waking hypnosis plus CBT for pain, fatigue, and sleep management in patients with cancer and cancer survivors. Psychooncology. 2016 Jul 28; doi: 10.1002/pon.4232. [Epub ahead of print]. doi: 10.1002/pon.4232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Picard P, Jusseaume C, Boutet M, Duale C, Mulliez A, Aublet-Cuvellier B. Hypnosis for management of fibromyalgia. Int J Clin Exp Hypn. 2013;61(1):111–123. doi: 10.1080/00207144.2013.729441. [DOI] [PubMed] [Google Scholar]
- 41.Plaskota M, Lucas C, Evans R, Cook K, Pizzoferro K, Saini T. A hypnotherapy intervention for the treatment of anxiety in patients with cancer receiving palliative care. Int J Palliat Nurs. 2012;18(2):69–75. doi: 10.12968/ijpn.2012.18.2.69. [DOI] [PubMed] [Google Scholar]
- 42.Smith GD. Effect of nurse-led gut-directed hypnotherapy upon health-related quality of life in patients with irritable bowel syndrome. J Clin Nurs. 2006;15(6):678–684. doi: 10.1111/j.1365-2702.2006.01356.x. [DOI] [PubMed] [Google Scholar]
- 43.Stanton HE. Hypnotic relaxation and the reduction of sleep onset insomnia. Int J Psychosom. 1989;36(1-4):64–68. [PubMed] [Google Scholar]
- 44.Tan G, Rintala DH, Jensen MP, Fukui T, Smith D, Williams W. A randomized controlled trial of hypnosis compared with biofeedback for adults with chronic low back pain. Eur J Pain. 2015;19(2):271–280. doi: 10.1002/ejp.545. [DOI] [PubMed] [Google Scholar]
- 45.Whitehouse WG, Dinges DF, Orne EC, et al. Psychosocial and immune effects of self-hypnosis training for stress management throughout the first semester of medical school. Psychosom Med. 1996;58(3):249–263. doi: 10.1097/00006842-199605000-00009. [DOI] [PubMed] [Google Scholar]
- 46.Younus J, Simpson I, Collins A, Wang X. Mind control of menopause. Womens Health Issues. 2003;13(2):74–78. doi: 10.1016/s1049-3867(02)00196-2. [DOI] [PubMed] [Google Scholar]
- 47.Buysse DJ, Reynolds CF, 3rd, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 48.Rejas J, Ribera MV, Ruiz M, Masrramon X. Psychometric properties of the MOS (Medical Outcomes Study) Sleep Scale in patients with neuropathic pain. Eur J Pain. 2007;11(3):329–340. doi: 10.1016/j.ejpain.2006.05.002. [DOI] [PubMed] [Google Scholar]
- 49.Allen RP, Kosinski M, Hill-Zabala CE, Calloway MO. Psychometric evaluation and tests of validity of the Medical Outcomes Study 12-item Sleep Scale (MOS sleep) Sleep Med. 2009;10(5):531–539. doi: 10.1016/j.sleep.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 50.Buysse DJ, Hall ML, Strollo PJ, et al. Relationships between the Pittsburgh Sleep Quality Index (PSQI), Epworth Sleepiness Scale (ESS), and clinical/polysomnographic measures in a community sample. J Clin Sleep Med. 2008;4(6):563–571. [PMC free article] [PubMed] [Google Scholar]
- 51.Buysse DJ, Reynolds CF, 3rd, Monk TH, Hoch CC, Yeager AL, Kupfer DJ. Quantification of subjective sleep quality in healthy elderly men and women using the Pittsburgh Sleep Quality Index (PSQI) Sleep. 1991;14(4):331–338. [PubMed] [Google Scholar]
- 52.Dietch JR, Taylor DJ, Sethi K, Kelly K, Bramoweth AD, Roane BM. Psychometric evaluation of the PSQI in U.S. college students. J Clin Sleep Med. 2016;12(8):1121–1129. doi: 10.5664/jcsm.6050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Viala-Danten M, Martin S, Guillemin I, Hays RD. Evaluation of the reliability and validity of the Medical Outcomes Study sleep scale in patients with painful diabetic peripheral neuropathy during an international clinical trial. Health Qual Life Outcomes. 2008;6:113. doi: 10.1186/1477-7525-6-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Angelini FJ, Kumar VK, Chandler L. The Harvard group scale of hypnotic susceptibility and related instruments: individual and group administrations. Int J Clin Exp Hypn. 1999;47(3):236–250. doi: 10.1080/00207149908410035. [DOI] [PubMed] [Google Scholar]
- 55.Orne MT, Hilgard ER, Spiegel H, et al. The relation between the hypnotic induction profile and the stanford hypnotic susceptibility scales, forms A and C. Int J Clin Exp Hypn. 1979;27(2):85–102. doi: 10.1080/00207147908407549. [DOI] [PubMed] [Google Scholar]
- 56.Hilgard JR, Hilgard ER. Assessing hypnotic responsiveness in a clinical setting: a multi-item clinical scale and its advantages over single-item scales. Int J Clin Exp Hypn. 1979;27(2):134–150. doi: 10.1080/00207147908407553. [DOI] [PubMed] [Google Scholar]
- 57.Spiegel H. The hypnotic induction profile (HIP): a review of its development. Ann N Y Acad Sci. 1977;296:129–142. doi: 10.1111/j.1749-6632.1977.tb38167.x. [DOI] [PubMed] [Google Scholar]
- 58.Hauser W, Hagl M, Schmierer A, Hansen E. The efficacy, safety and applications of medical hypnosis. Dtsch Ärztebl Int. 2016;113(17):289–296. doi: 10.3238/arztebl.2016.0289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Stanley RO, Burrows GD. International Handbook of Clinical Hypnosis. In: Burrows GD, Stanley RO, Bloom PB, editors. The Negative Consequences of Hypnosis Inappropriately or Ineptly Applied. Hoboken, NJ: John Wiley & Sons Ltd; 2001. [Google Scholar]
- 60.MacHovec F. Hypnosis complications, risk factors, and prevention. Am J Clin Hypn. 1988;31(1):40–49. doi: 10.1080/00029157.1988.10402766. [DOI] [PubMed] [Google Scholar]
- 61.Elkins GR, Fisher WI, Johnson AK, Carpenter JS, Keith TZ. Clinical hypnosis in the treatment of postmenopausal hot flashes: a randomized controlled trial. Menopause. 2013;20(3):291–298. doi: 10.1097/GME.0b013e31826ce3ed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.McNeal S, Frederick C. Inner strength and other techniques for ego strengthening. Am J Clin Hypn. 1993;35(3):170–178. doi: 10.1080/00029157.1993.10403001. [DOI] [PubMed] [Google Scholar]
- 63.Lyne J, Quinlivan L, Byrne CA, Malone K, Walsh C. Sleep hygiene use in a psychiatry outpatient setting. Ir Med J. 2011;104(2):49–50. [PubMed] [Google Scholar]
- 64.van Straten A, van der Zweerde T, Kleiboer A, Cuijpers P, Morin CM, Lancee J. Cognitive and behavioral therapies in the treatment of insomnia: a meta-analysis. Sleep Med Rev. 2017 Feb 9; doi: 10.1016/j.smrv.2017.02.001. [Epub ahead of print]. doi: 10.1016/j.smrv.2017.02.001. [DOI] [PubMed] [Google Scholar]
- 65.Bragard I, Etienne AM, Faymonville ME, et al. A nonrandomized comparison study of self-hypnosis, yoga, and cognitive-behavioral therapy to reduce emotional distress in breast cancer patients. Int J Clin Exp Hypn. 2017;65(2):189–209. doi: 10.1080/00207144.2017.1276363. [DOI] [PubMed] [Google Scholar]
- 66.Kohen DP. Chronic daily headache: helping adolescents help themselves with self-hypnosis. Am J Clin Hypn. 2011;54(1):32–46. doi: 10.1080/00029157.2011.566767. [DOI] [PubMed] [Google Scholar]
- 67.VandeVusse L, Hanson L, Berner MA, White Winters JM. Impact of self-hypnosis in women on select physiologic and psychological parameters. J Obstet Gynecol Neonatal Nurs. 2010;39(2):159–168. doi: 10.1111/j.1552-6909.2010.01103.x. [DOI] [PubMed] [Google Scholar]
- 68.Kohen DP. Long-term follow-up of self-hypnosis training for recurrent headaches: what the children say. Int J Clin Exp Hypn. 2010;58(4):417–432. doi: 10.1080/00207144.2010.499342. [DOI] [PubMed] [Google Scholar]
- 69.Dobbin A, Maxwell M, Elton R. A benchmarked feasibility study of a self-hypnosis treatment for depression in primary care. Int J Clin Exp Hypn. 2009;57(3):293–318. doi: 10.1080/00207140902881221. [DOI] [PubMed] [Google Scholar]
- 70.Bisson JI. Adding hypnosis to cognitive behavioural therapy may reduce some acute stress disorder symptoms. Evid Based Ment Health. 2005;8(4):109. doi: 10.1136/ebmh.8.4.109. [DOI] [PubMed] [Google Scholar]
- 71.Carim-Todd L, Mitchell SH, Oken BS. Mind-body practices: an alternative, drug-free treatment for smoking cessation? A systematic review of the literature. Drug Alcohol Depend. 2013;132(3):399–410. doi: 10.1016/j.drugalcdep.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]


