Abstract
In this article I examine the process by which low-income (mostly minority) women develop the skills to integrate diabetes self-management into daily life and the conditions that affect the process. I present and describe a multimethod approach, including semistructured interviews, photo elicitation, time geographic diaries, and a standardized assessment which were used to collect data from 10 low-income women with type 2 diabetes, ages 40 to 64 years, between July and December 2012. I describe the grounded theory approach to data analysis which facilitated the development of the Transactional Model of Diabetes Self-Management (DSM) Integration. The model depicts the theorized process whereby low-income women accept aspects of diabetes education and training as congruent with their circumstances, act on them, and practice with them until they become integrated into daily life. Inquiry and practice play key roles in assimilating DSM. I discuss the study’s implications for facilitating better health-management programs.
Keywords: behavior change, diabetes, diaries / journals, photography / photovoice, self-care, theory development
Type 2 diabetes (T2DM) is a chronic, progressive metabolic disorder that affects how the human body uses sugar (glucose) from food. Approximately 95% of the 25.8 million diabetes cases in the United States are type 2 (Centers for Disease Control and Prevention [CDC], 2011). As rates increase, researchers face a significant challenge understanding the processes inherent in diabetes self-management (DSM). Thus, an important goal of diabetes research is improved knowledge about how to facilitate the awareness, skills, and abilities necessary for self-management of this complex condition (Funnel et al., 2011). Nonetheless, without better conceptual understanding of the processes of DSM as experienced by those with the disorder, such knowledge will be incomplete and ineffective. In this article, I present an initial conceptual model of DSM integration based on in-depth qualitative research with women attempting DSM.
Research about DSM has identified the behaviors most significantly linked to successful metabolic control (Funnell et al., 2011; Mulcahy et al., 2003). These activities include: healthy eating, being physically active, taking medication, monitoring one’s condition, healthy coping, problem solving, and reducing risks (Peeples, Tomky, Mulcahy, Peyrot, & Siminerio, 2007). Historically, didactic education was the core of DSM intervention programs (Newman, Steed, & Mulligan, 2004); however, information presented didactically proved insufficient to produce lasting behavior change (Coster & Norman, 2009). Scholars have since moved beyond purely educational modes of behavior change and imported theories and constructs from psychology and the cognitive sciences to guide interventions (Newman et al., 2004). Current DSM education incorporates additional skills and strategies into interventions such as goal setting, and activities to increase self-efficacy and manage barriers (Peeples et al., 2007).
Despite the substantial body of intervention work that has been developed, DSM interventions still produce inconsistent results (Coster & Norman, 2009). Meta-analyses of DSM educational and behavioral interventions demonstrate that results vary depending on the outcomes being measured. For example, an intervention can produce a moderately significant decline in glycohemoglobin (GHb) while having little influence on participants’ weight and fasting blood glucose levels (Gary, Genkinger, Guallar, Peyrot, & Brancati, 2003). Similarly, psychological interventions can be effective in reducing stress but fail to produce significant changes in weight or blood glucose concentrations (Ismail, Winkley, & Rabe-Hesketh, 2004). In addition to inconsistent results, the positive results of DSM interventions attenuate after approximately 6 months (Norris, Lau, Smith, Schmid, & Engelgau, 2002).
DSM scholars are not alone in their inability to facilitate sustained engagement in healthy behaviors (Nilsen, Haverkos, Nebeling, & Taylor, 2010). Knowing core behaviors, behavioral determinants, mediators, and contextual influences is important in promoting more healthful lifestyles (Ory, Smith, Mier, & Wernicke, 2010). Nevertheless, to advance knowledge, researchers also need a clear understanding of how individuals sustain engagement in and eventually assimilate health-promoting behaviors in the context of constantly shifting personal, social, and environmental circumstances (Glasgow, Goldstein, Ockene, & Pronk, 2004). In the case of DSM, clients must change lifestyle behaviors and incorporate new tasks and activities (e.g., blood glucose monitoring and medication administration). To be successful, they must learn how to reconfigure aspects of their daily context and life patterns and negotiate a variety of barriers and supports to self-management (Audulv, Asplund, & Gustaf-Norbergh, 2012). This is a particularly difficult task for low-income and minority women in the United States (CDC, 2011).
Although being a woman, of minority status, or low income does not in itself determine a person’s ability to engage in DSM, the compounding of these factors creates conditions that make it very difficult for persons in such populations to attain their DSM goals (Hills-Briggs et al., 2011). Women are more likely to live in poverty than men, have less formal education, and receive less pay for the same level of work (American Psychological Association, n.d.; Agency for Healthcare Research and Quality, 2011). The situation is even more problematic for low-income and minority women, who often act as caregivers in multigenerational households (often referred to as the sandwich generation) and experience additional restrictions on time, energy, and resources available to balance both the competing demands of the caretaker role and performing their own health management (Riley, 2005).
Evidence demonstrates that knowing what people should do, identifying possible barriers to their engagement, and understanding important mediators in behavior change processes is not enough. Scholars still know very little about how individuals with T2DM act to reconfigure daily life contexts; that is, how they negotiate the assimilation of DSM activities. Understanding how people integrate DSM into daily life, even in the face of multiple challenges, could provide new insights into strategies and subprocesses that ensure continued participation in self-management behaviors. Such knowledge is necessary to move the field forward. The purpose of the study presented here was to address this gap by exploring the process by which low-income women integrate DSM behaviors into daily life, and the conditions that influence this process.
Methods
In this study I used a multiple-case, multiple-method design to understand different layers of the integration experience (i.e., temporal, social, personal, contextual). Data were analyzed using a grounded theory approach (Charmaz, 2006).
Recruitment Procedures
The study design was approved by the University of North Carolina at Chapel Hill. I used a purposive sampling strategy to identify low-income Black and White (self-identified) women ages 40 to 64 years who self-identified as being diagnosed with type 2 diabetes. For the purpose of the study, low income was defined as having a total household income at or below 200% of the federal poverty guidelines (U.S. Department of Health and Human Services, 2012). For example, in 2012 the 200% household income limit for a household of two people was at or below $30,020USD. Participants were recruited from a nonprofit primary care clinic in an urban location in the southeastern United States. I was involved with DSM educational classes being offered at the clinic, and with permission from the medical director, had access to population of low-income women with type 2 diabetes from which to recruit a sample.1 The diabetes class coordinator allotted time at the end of the classes during which I explained the study, distributed recruitment flyers, and obtained the contact information of interested potential participants.
Potential participants who expressed interest in the study received a follow-up phone call and were screened for eligibility. If they were eligible I made an appointment to meet with them. During the appointment I review the study consent forms, answered any additional questions potential participants had, and obtained their informed consent. I made them aware that participation was voluntary, that they could withdraw from the study at any time, and that their confidentiality and anonymity in data collection, analysis, and presentation of the findings was guaranteed.
Study Participants
Ten women completed all of the study activities. The sample (7 Black, 3 White) included individuals with varying levels of DSM experience. All of the participants had previously participated in formal DSM classes (range: 2 to 4 previous classes) within the previous 2 to 18 years. As befits a qualitative approach in which I sought to understand a range of individual experiences, I intentionally recruited participants with a broad range of demographic characteristics. The women ranged in age from 45 to 63 years, with the time of managing diabetes ranging from 3 to 30 years. Half of the women were married, and family size ranged across the sample from 1 to 7 persons in the household. Five of the participants had some college education (one semester class, and 1 participant had an associate degree; the other 4 participants had either a high school diploma or a general education degree (GED). Employments characteristics were as follows: employed (n = 6), retired (n = 1), on disability (n = 1), and unemployed (n = 2). Income range for the sample was < $5,000USD to $29,000USD.
Data Collection
On average, it took each study participant 7 weeks to complete all study-related activities (range = 5 to 16 weeks). I conducted participant interviews in a private office at the nonprofit clinic. With participants’ permission I audio recorded interviews. I wrote field notes during interviews and after each participant contact. I used multiple methods of data collection, in the following order, to more fully capture the complexity of how the women integrated DSM into daily life: (a) the Diabetes Care Profile (DCP; Fitzgerald et al., 1996), followed by a semistructured interview; (b) participant-generated photography, followed by participation in a photo-elicitation interview; and (c) 2 days of data collection using a time geographic diary (TGD; Michelson, 2005) and a follow-up TGD interview. Each data collection activity is discussed in more detail below.
Diabetes Care Profile and Semistructured Interview
During the initial phase of the study, I met study participants at the clinic to complete the DCP (Fitzgerald et al., 1996) and the semistructured interview. Participants were first asked to complete the DCP. The DCP is a standardized patient self-report assessment of their demographic data, DSM practices, diabetes knowledge, and perception of supports and barriers. After participants completed the DCP (during the same meeting) they participated in a semistructured interview. The interview guide was designed to elicit data on the following aspects of the DSM-integration process: (a) experience of DSM through time, specifically from diagnosis onward; (b) past and current process of integrating DSM tasks into daily life; (c) facilitators and inhibitors of DSM from the participant’s perspective; and (d) aspects of decisional processes, such as negotiating competing activities/circumstances, handling contingencies, and creating/modifying routines.
Participant Photography and Photo-Elicitation Interview
Photo elicitation was the second data collection activity. Photo elicitation involves inserting photographic material (participant- or researcher-generated) into a research interview (Harper, 2002). Research has demonstrated that using photographic data in conjunction with research interviews produces a more focused, detailed, and reflective report of a phenomenon (Collier, 1957; Pink, 2001; Lorenz, 2011). In addition, the method has been shown to be an effective way to collect data on participants’ contexts, subjective experiences, and tacit processes across a variety of settings, populations, and problems (Collier, 1957; Harper, 2002; Lal, Jarus, & Suto, 2012; Pink, 2001), making it an effective tool for collecting data on participants’ perceptions of their DSM in their particular context.
The photo-elicitation component began with providing participants a 27-exposure disposable camera and a prepaid mailer for returning the camera. I instructed participants to “take photographs of the things you associate with diabetes self-management.” I asked participants to take their photographs throughout the following 2 weeks to facilitate timely data collection and prevent the possible loss of cameras. To maintain anonymity, I instructed participants not to take pictures of their own or others’ faces.
I took the film to a local commercial photo developer. Next, I reviewed the photographs and made notes on my initial impressions before meeting each participant and engaging together in the photo-elicitation interview. This step allowed me to document my assumptions about participants’ lives and later compare them to their explanations of the photographs. At the beginning of the photo-elicitation interviews I instructed participants to select the photographs they wanted to discuss, to present each photograph individually, and to described the content of the photo: why a photo was taken (e.g., its meaning, value, or representation), where it was taken, and if applicable, with whom the photo was taken. Finally, I asked participants to reflect and elaborate on anything they had wanted to take a picture of but did not because of not having the opportunity or access.
Time Geographic Diary
Following the photo-elicitation phase, participants were asked to complete a time geographic diary (TGDs; Michelson, 2005). Time geographic diaries provide a unique method for eliciting information about daily life patterns, including activities completed, time use, and social contacts. This type of diary method asks participants to log their daily activities in a specific way and in small increments of time. Diary studies are used to ensure a higher level of data quality and are often used in situations in which recall bias is a concern (Pentland & Harvey, 1999). Time-use research illustrates that the difference in data quality when 2 days are recorded vs. 3 days or more is minimal (Michelson; Pentland & Harvey). Therefore, to lessen participant burden, TGDs were completed for 2 days of their choosing, including one weekend day and one weekday (Pentland & Harvey).
Rather than focus explicitly on DSM behaviors, participants were asked to simply record all of their daily activities, with the assumption that DSM would emerge as part of daily life patterns. The TGD packet included (a) the leave-behind TGD formatted in 15-minute intervals; (b) an example of how to complete the diary; (c) my contact information (in case participants needed additional guidance); and (d) a prepaid mailer for returning the TGD. The TGD was created using Microsoft Excel. The matrix consisted of seven columns labeled time, activity, location of activity, person present, secondary (cooccurring) activity, forfeited activity, and miscellaneous comments. The columns were formatted for a 24-hour day divided into 15-minute intervals, resulting in a total of 96 rows. I met with each participant to discuss how to complete the TGD and illustrated its use. I left the TGDs with participants when they felt confident that they could complete it independently.
On receiving the participants’ diaries, I transferred the data to a spreadsheet and reviewed it prior to each TGD interview. This step informed the interviews by suggesting avenues of additional questioning (e.g., why certain activities always occurred at specified locations). During the interviews, I asked participants to discuss the influence of time use and daily life patterns on their DSM and how/if they had changed through time. Questions included (a) why certain activities co-occurred, (b) how and why their DSM activities were performed in different locations or in different social contexts, and (c) how they negotiated DSM in the face of competing daily demands. Participants received a $100 gift card for completing all of the study activities.
Data Analysis
Data analyzed included 10 completed diabetes care profiles, transcripts of 30 in-depth interviews, typed field notes from all data collection activities, 182 photographs, and the completed TGDs. I used peer debriefing (during biweekly meetings) with other researchers at my institution throughout data collection and analysis to ensure trustworthiness and to explore alternative interpretations of the data. I coded all interview transcripts and field notes in the Atlas.ti software package (Scientific Software Company, 2012) using a grounded theory approach (Charmaz, 2006). Key features of grounded theory, which includes theoretical sampling, constant comparison, and the use of a coding paradigm, make it particularly useful for capturing the complexity of social processes (Charmaz), such as the integration of DSM into daily life.
I began data analysis with open coding (coding small segments of text line-by-line) of all text sources of data. Because participants were enrolled sequentially, I was able to open code initial interview transcripts and analyze emerging themes before continuing with subsequent interviews. Themes that emerged early in data analysis were theoretically sampled for in later interviews. For example, during the third semistructured interview, destabilizing life events emerged as an important influence on the integration process; this theme was therefore incorporated into subsequent interviews. Following the open-coding step, data were focus-coded, which involved taking initial analytical directions developed from the line-by-line coding and applying them more selectively to larger chunks of text (Charmaz, 2006). Finally, I axial coded2 the data to facilitate reassembling it into a coherent developing theory.
Finally, all of the data collected were considered together and integrated through constant comparisons across cases and data types. I compared the diabetes care profile data to the data provided by participants during the interviews to explore issues of convergence or divergence in participants’ reports. Participants’ photographs were analyzed in conjunction with the photo-elicitation interview transcripts. Specifically, participants’ photographs often illuminated contradictions among data sources. For example, narratives of strong adherence to a diabetes-friendly diet were often coupled with photographs of family meals which depicted unhealthy dietary choices. I actively discussed discrepancies with participants, which led to a deeper and more nuanced understanding of DSM integration.
In addition, I made notes on the backs of the photographs while reading the transcripts to indicate what each photo represented to the participants. I analyzed the photographs by their objective content and by the participants’ explanations of the photo (significance). I analyzed the TGDs in conjunction with the TGD interview transcripts at several levels to yield different perspectives on how the sequence of daily activities affected engaging in DSM. These included the types of primary and secondary activities that each participant engaged in during a typical day (defined by participants as their normal and usual daily routine), the total time allotted to activities, the types and frequencies of co-occurring activities, and the structure of their daily routines. Figure 1 illustrates how I developed inferences from the integration of multiple data sources.
Figure 1.
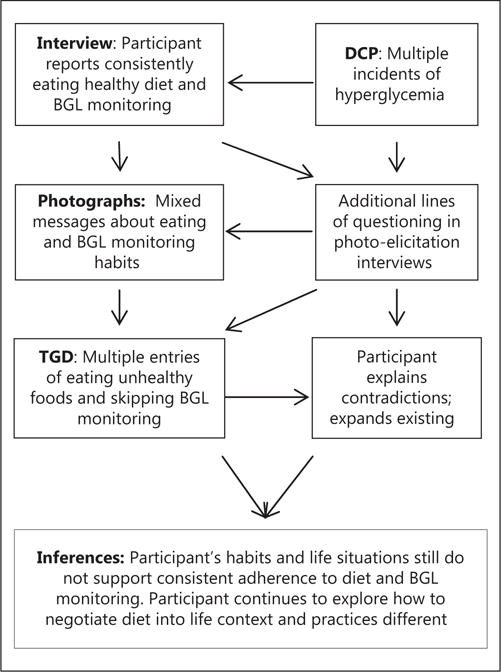
The process of integrating multiple data sources during data analysis.
Note. BGL = Blood Glucose Level; DCP = diabetes care profile; TGD = time geographic diary.
As data sources were integrated, memos and diagrams of hypothesized linkages were either supported or rejected as data from additional cases were added. The addition of subsequent cases also increased the depth of emerging themes and allowed me to explore alternative interpretations of the data. I followed this process until data saturation was reached at 10 participants. Data were considered saturated when the addition of new cases no longer resulted in additional codes or analytical directions. This process led to refinements of the analysis and the generation of findings.
Findings
The grounded theory process resulted in the development of the Transactional Model of Diabetes Self-Management Integration (TMDSMI), which depicts the theorized integration process. Participants defined DSM as the ability to do “almost everything you have to do almost all of the time.” They depicted integration as the point where habits and contexts supported seamless engagement in DSM components. They characterized the process leading to integration as a process of becoming able to do better.
The TMDSMI depicts the process whereby participants accepted aspects of diabetes education and training as congruent with their circumstances, applied them to their own context, and practiced with them until they became integrated into daily life. The primary domains of the model include potential uptake, inquiry, practice, integration, and reconfiguration. The full model also depicts the conditions that influence the process. A detailed explanation of the conditional influences is beyond the scope of this article; however, they are briefly discussed below to provide additional context. Figure 2 depicts the primary domains of the TMDSMI.
Figure 2.
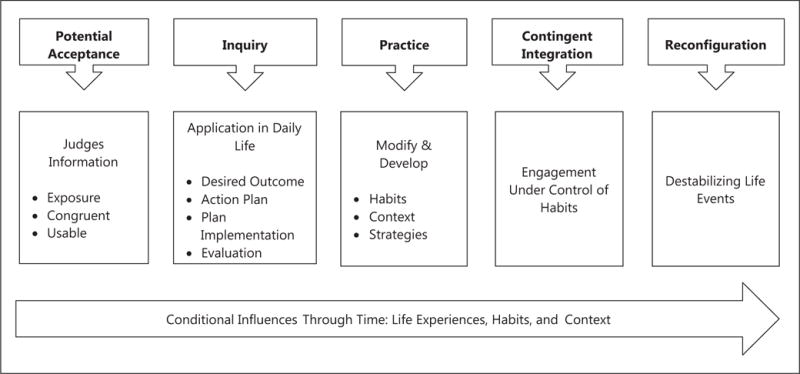
The Transactional Model of Diabetes Self-Management Integration.
Conditional Influences: Experience Frame and Time
Habits and life contexts constituted the experience frame that surrounded the process of DSM integration and influenced participants’ integration efforts from diagnosis onward. Participants’ habits developed and operated in conjunction with their particular situational context. The existing habit–context relationship operated largely beneath participants’ conscious awareness and served a valuable function in the context of general daily life management. Nevertheless, established habits and life context made it difficult for participants to integrate DSM into daily life and had to be modified to better support DSM integration. Participants became able to modify aspects of their habits and situation through the process described below. Time flows through the model because integration is a temporally contiguous process because past and current experiences contribute to future action.
Potential Uptake
Prior to diagnosis, participants did not have a priori knowledge about how to manage a complex condition such as diabetes; instead, they needed guidance and information to get started. Potentials were the raw materials of DSM integration and represented the DSM-relevant information that could potentially be integrated into daily life. The term potentials was derived from the language a participant used to describe the power inherent in DSM information: “There is a lot of potential there; there is always potential. For me, I just had to figure out how to make it work in my own situation.” Participants were exposed to potentials through their health care providers and their social networks. The likelihood that participants would accept, act on, and integrate a potential into daily life depended on how they were introduced to the information. Participants were more likely to act on information that came from a supportive provider. This was because they felt their provider knew their life situation and would not suggest that they engage in something they were incapable of. One participant said, “She [provider] knows my situation, so she knows what I can do.” The trust participants had in supportive care providers increased the likelihood that their recommendations would be acted on.
Participants also valued being introduced to potentials through their personal networks. The information participants received from friends and family was typically different from the information they received from their primary care providers. In addition, information from friends and family was perceived as being more congruent with their life because it had been tried out by others with similar life situations before being passed along. For example, one participant noted that the most usable suggestions she acted on came from older women in her community who also had diabetes. Another participant stated that she got her most valued DSM “tips and tricks” from her brother and spouse (both of whom had T2DM). The participant also shared a photograph that showed grapefruit cooking in a pot (see Figure 3). She decided to try this approach to making a healthful beverage after her spouse introduced her to the idea.
Figure 3.
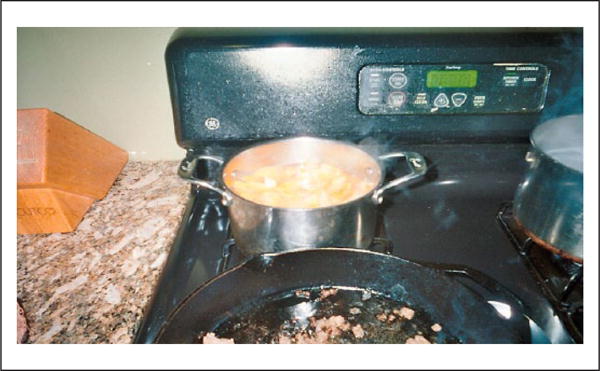
An example of acting on a new idea.
The congruency and usability of DSM information also influenced whether or not participants would decide to act on it. They judged potentials as acceptable (or not) depending on how congruent they were with their habits, values, beliefs, time constraints, and personal situation. Similar to Bourdieu’s (1998) concept of habitus, participants demonstrated a sense of whether or not a potential was “for them” or not, and this tacit sense of fit influenced which potentials they accepted or ignored. In one of the most poignant examples, a participant stated,
We [African American people] don’t mess with stuff like quinoa, or however you call it. Couscous? Please! I mean, a whole grain to me is wheat bread. I can’t see messing with some of that other stuff. I mean, I can’t even say what it’s called [pronounce it].
The participant’s perception was that such foodstuffs were not congruent with what people ‘like her’ would eat. The perception of foreignness dissuaded her from wanting to try such new ingredients.
Participants were more likely to accept potentials that were seen as more usable (i.e., providing greater detail, suggestions, examples, and intermediate steps toward a goal). The importance of congruence and usability was expressed in terms of the effort (both cognitive and behavioral) and resources needed to act on certain recommendations. It took more resources and effort to adopt behavioral recommendations that were perceived as vague and incongruent with their lifestyle. One participant stated, “I mean, they tell you what to do, and you nod and say, ‘Yeah, that’s good.’ but you know that if it doesn’t fit with what you’re doing, you’re not going to really do it.”
Inquiry
Inquiry constituted participants’ initial engagement with an accepted potential. The term inquiry was used to reflect that although inquiry is similar in form to problem solving, inquiry was neutral and could be used to solve problems or to simply fulfill the desire to improve already functional DSM regimens. The inquiry experience was novel and characterized by increased reflective awareness. One participant noted, “Yeah, I mean, you think more about it, especially the first couple times, because it’s like, hey, I’m exercising [laughter].” During inquiry participants determined the desired outcome of their efforts and then constructed a tentative action plan to achieve the outcome. Next participants enacted their plan, making modifications as necessary, and evaluated the outcome of their efforts.
To construct a reasonable action plan participants had to be able to assess the qualities of their unique situation and determine what they could work with or what might need to be changed. For example, acting on a new recipe required participants to assess micro contexts (task-specific circumstances) to determine what products they already had and could continue to use, while also deciding on what items they still needed or could be substituted. In addition, as one participant stated, “You also have to assess your own skills, like, ‘Can I actually do that, or it is just going to end up as one big mess?’” Action plans had to account for both context and self-assessment.
Participants often deviated from their action plan and made minor adjustments in response to problems. During the evaluation phase, participants appraised the outcomes of their efforts. The evaluation process included not only a valuation of their own performance, but a feasibility assessment of how the process fit into their daily life (e.g., whether it was cost effective, time effective, and was supported by established routines). One participant noted,
It’s not just about me, I mean it’s, “Can I afford it? Do I have the time? Do they [father and grandchildren] like it?” I mean, I have to look at how I’m really gonna make it work in the whole scheme of things, because you can make anything work once.
Effective inquiry promoted informed decisions regarding if and how new tasks could be integrated or behaviors modified successfully. Inquiry, therefore, prepared participants for future success. Faulty inquiry, however, could lead to maladaptive approaches to DSM, and the inquiry process was fraught with pitfalls. Although participants could readily identify tentative outcomes, they often struggled with assessing their context for supports or hindrances—an essential step in constructing action plans. In addition, some participants failed to critically evaluate the outcomes of their efforts, which led to incorrect assumptions about how easy it would be to integrate behaviors into daily life long term. Moreover, although inquiry was described as a reflective process, participants’ reflective approaches to inquiry were also influenced by their habits.
Participants’ habitual ways of doing and thinking were often imperceptible to them. At times, the negative impact their habits had on the inquiry process went unexamined. For example, by assessing one participant’s time geographic diary and discussing it and her decisions in our interviews, it became clear that she habitually approached problems and change in a stark, all-or-nothing manner. In addition, although it was not the intention of the study, discussing participants’ photographs and TGDS often facilitated their reflective awareness of some of these problematic habits. For example, when discussing her TGD and photographs of herself exercising, one participant stated,
When I plan something out [exercising], you know, if I was smart I would make a plan that works, but sitting here talking about this, I see that one problem I have is always making plans that make everyone else happy rather than what I really need to do.
Socially learned tendencies to respond to situations in particular ways (Bourdieu, 1998; Dewey, 1922/1957), though useful in daily life, were problematic for DSM and were often imperceptible to participants.
In addition, participants repeatedly came in contact with certain persons and places within daily routines that negatively influenced integration efforts. Because such person/place interactions became habitual, it was difficult for participants to identify problematic aspects of their routines until drastic changes occurred that brought them into reflective awareness. For example, one participant stopped at the same fast food restaurant every morning for 11 years on her way to her office. It was not until she lost her job and stopped driving to work that she was able to reflect on the how the location of the fast food restaurant (next to her office), in the context of her daily routine, influenced poor dietary behaviors for years. She stated,
You know, I would not cook that way in my own home, because I was aware. It [fast food breakfast] just became a part of my day because I was busy in the morning, so eventually I never gave it any thought.
These examples provide a glimpse into how operating in habitual ways made it more difficult to integrate and apply DSM knowledge.
Practice Phase
Participants initiated new tasks and behavioral changes in the inquiry phase, and their performance resulted in a plausible “rough draft” of an integrated potential. Through inquiry, participants formulated preliminary ideas about how to reconfigure personal habits and contextual features to support new behaviors. Practice was how the dynamics of daily life were reconfigured. Practice was the engagement in numerous mini-inquiry phases that occurred through time and across situations. One participant made a drawing (see Figure 4) to illustrate how small changes (x’s) accumulated through time via repeated engagement in DSM components.
Figure 4.
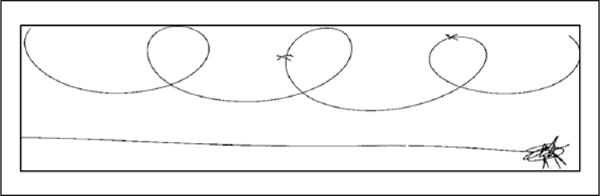
An example of small changes made through time during repeated practice.
Practice linked participants’ initial experiences with potentials to their finished, integrated products. During practice, participants experienced an increased awareness of their habits and contexts. Moreover, through repeated practice participants continued to develop their inquiry skills, especially contextual and self-assessment skills and how to anticipate necessary adjustments. A participant noted, “They say practice makes perfect, right? Well in my case it really has taught me a lot about myself and how what I do affects my diabetes.” This process however, occurred serially rather than suddenly. Participants made incremental changes to their habits and life situation with each engagement. The accumulation of such modifications resulted in enduring behavior changes. One participant described the process:
It didn’t happen overnight [changing cooking habits]. No, I started off, “Well, let’s change this, okay? No butter.” Next, “Lower my salt. Okay.” Then what else? “Oh, let’s try some of those sugar-free substitutes.” Don’t get me wrong, you don’t do it all at once; you gotta keep at it.
During practice, participants also developed strategies to facilitate consistent engagement in DSM components. The more practice the women had with DSM, the more numerous and varied the strategies they developed. Although participants acquired some of their strategies from other individuals (e.g., family, friends, and health care providers), they derived the majority through practice. For example, while in the hospital a participant was served a heart-healthy baked pork chop. Once home, she continued to practice the method repeatedly and refined it to the point that she was able to use the same method with other proteins. Through practice she developed multiple strategies to make the dish healthy, pleasing to her family, and convenient. She explained it this way:
I don’t need to use butter so I substitute with olive oil, and if I don’t have that I use just a touch of that Pam cooking spray. See, I substitute. That’s a strategy I use a lot. I don’t fry it, neither. What I do is I bread it, but then I also started using the wheat breadcrumbs, and then I bake it. And see, to get my family to eat the vegetables I layer them underneath so that they taste like the pork, so they taste better. I also cook ahead; that’s another strategy I do. I just do a whole big thing of it and then portion it out into servings so it’s quick and easy during the week. The last thing I do, another strategy I use is these [holding photograph of small plates], I eat off of that plate. That’s a strategy I use to make sure I watch my portion size.
Through practice participants developed strategies that allowed them to integrate more health-promoting behaviors into their life in ways that were cost-effective, time-effective, and amenable to other family members.
Contingent Integration and Reconfiguration
Practice begins as a reflective process, resulting in the modification of habits and context and the development of strategies. An integrated DSM component can be thought of as the most congruent, refined version of a potential that participants were capable of constructing given their habits, situation, and developed strategies. Although practice began as a reflective process, engagement became less reflective as components were mastered. Integration was achieved when engagement with a potential no longer elicited reflective awareness, and instead simply became a habitual part of daily life. In fact, participants rarely addressed integrated potentials in their photographs, although they noted their completion in the TGDs. Integration was desired because it signified the point where engagement in a DSM component was less burdensome, being relegated to habitual thought and action. One participant stated, “Now I just do it, it’s automatic. I don’t really think about how I do it; it’s just like clockwork.”
Furthermore, integration was contingent because destabilizing life events could derail established DSM regimens. Destabilizing events were defined as events that changed participants’ life situations so significantly that the functional habit/situational quality relationship no longer supported established DSM regimens. Participants provided examples of the many life events that could be destabilizing, and emphasized that not all destabilizing events were negative, but that they interfered with their DSM efforts (e.g., acute illness, divorce, birth of a child, or employment change).
Many of the participants were either experiencing or had just recovered from a major destabilizing life event, and they often depicted these events through their photographs. For example, a participant presented a photograph of her weekly schedule. She had recently enrolled in school to advance her education. Because her spouse had been underemployed, she had also recently made the decision to work a second job. She was thankful for the job and the opportunity to continue her studies, but noted that she would suddenly have to rethink her entire DSM regimen and how to make it function because of these events.
Reconfiguration involved participants going through aspects of the integration process again. For some participants, repeated instability made it virtually impossible to even get started developing self-management skills. As one participant stated when discussing her own experience with destabilizing life events, “You basically have to start over.” For low-income women faced with social and financial instability, destabilizing events often necessitated reconfiguration.
Discussion
The five phases of the model depict how participants accepted aspects of diabetes education and training as congruent with their circumstances, acted on them, and practiced with them until they became a more integrated part of their daily life. Although scholars have previously explored facets of DSM (e.g., Schulman-Green et al., 2012), to my knowledge this is the first theoretical model derived from participants’ experiences that depicts the process of how DSM is integrated into daily life.
The Transactional Model of Diabetes Self-Management Integration (TMDSMI) shares some similarities with health behavior theories commonly applied to the problem of DSM. For instance, processes similar to those described in Problem Solving Theory (Hills-Briggs, 2011) are at work during inquiry and practice. In addition, the influence of prior experience on current action is similar to Social Cognitive Theory’s emphasis on experience as a means of developing self-efficacy (Bandura, 1997). The TMDSMI, however, also differs from health-behavior theories commonly used in DSM research, and therefore suggests important avenues of inquiry that remain underexplored.
One significant difference is the perspective of human agency. Psychological and cognitive-based theories of health behavior (commonly used to inform DSM research) presume human action to be reflective and under conscious control (Churchill & Jessop, 2011; Crosby & Noar, 2010). Although people do engage in reflective thought and action, emerging literature suggests that the majority of human thought and action is actually the product of habitual rather than purposeful processes (Churchill & Jessop; Lindbladh & Lyttkens, 2002; Neal, Wood, Wu, & Kurlander, 2011; Orbell & Verplanken, 2010). The TMDSMI accounts for the role of reflective and habitual thought and action in the integration process.
For example, inquiry is a highly reflective phase, yet even during reflective inquiry habitual ways of being in the world impeded participants’ abilities to effectively assess their self and their context. Participants were aware of what they should do to manage their condition; they were less aware of what they habitually did and how it affected the process. Findings draw attention to why change is so difficult: because it is so difficult to see aspects of daily life as problematic to begin with. Telling people what to do is different than facilitating their understanding of what they already do.
Another important finding is the interlocking nature of the inquiry and practice phases of DSM integration, which extends current understandings of initiating behavior vs. sustaining it. Within the model, inquiry represents the initiation of a behavior, the purpose of which is to determine the feasibility of continued participation. Assessments and conclusions drawn from inquiry inform how potentials could best be incorporated into one’s unique situation. Participants initiated DSM components in inquiry, but integrated them through practice. Participants who inquired yet did not practice were unable to develop DSM regimens that could be sustained for very long. The findings contribute new understandings regarding why some people might initiate components of DSM yet fail to truly incorporate them into their daily life.
The inquiry–practice relationship also raises questions regarding the dose of DSM programs. It is a logistical necessity that interventionists maximize effectiveness while reducing participant burden; however, findings from this study demonstrate that changes to habits and situations are made incrementally via repeated engagements through time; much longer time frames, then, are typically feasible for DSM programs. It is possible that outcome measures occurring at shorter durations, such as 3 or 6 months, capture successful inquiry and the beginning of practice, but not integration. This might contribute to why DSM intervention effects deteriorate after approximately 6 months (Norris et al., 2002). Perhaps programs are terminated before participants have sufficiently practiced and actually integrated DSM components.
How then can researchers design programs to incorporate the inquiry and practice needs of behavior-change initiation and its continual evolution? Regularly scheduled boosters are becoming increasingly incorporated into DSM programs, and might provide the means for facilitating much-needed practice and supporting individuals as they reconfigure their DSM regimens. Additionally, more practice-oriented DSM programing could provide a platform whereby clients are afforded opportunities to practice fundamental DSM skills, an opportunity that could be especially important for low-income women with complicated life situations (Hills-Briggs et al., 2011).
Charmaz (2006) argued that it is impossible to enter the grounded theory process as a blank slate, and that the outcomes of the grounded theory process should be viewed as the coconstructed product of both the researcher’s and participants’ experiences and knowledge. My experience as a clinician and my social science training influenced how I viewed the data. During contact with participants, my emerging ideas and hypothesis were shared with participants, and the resultant model is a reflection of this process.
This study’s readily identifiable limitations are its relatively small sample and geographically limited urban context. Moreover, all participants were taking part in additional DSM education as part of another research project while enrolled in this study. Therefore, the sample might not be representative of middle-aged, low-income urban women faced with DSM. Because of their previous DSM educational experiences, it is likely that this group of women were better able to reflect on certain aspects of their DSM.
In addition, the study included women only; whether aspects of the model would be as relevant to men remains uncertain. For example, the amount of time and effort participants dedicated to practicing diet-related DSM activities could be an artifact of gender-associated roles. It is possible that, for example, a similar cohort of men would dedicate more time to exercise, but this is purely speculative. Because habits and situations affect the prioritization of DSM activities, it would be realistic to expect that habits associated with the enactment of gender roles would influence the DSM integration process.
Despite these limitations, it should be noted that the socioeconomic similarities of participants was a strength. Their financial homogeneity resulted in a depth of data in this area that permitted more comprehensive investigation of the effects of economic vulnerability on DSM. The women in this study were low-income, and many lived in a state of near-personal or -financial crisis. Had the study included a different group of individuals it is quite possible that their more widely ranging experiences and stories would not have revealed the highly contingent nature of DSM integration practices in a context of ever-changing vulnerability.
The study’s findings suggest several lines of future investigation. For example, it is unclear how long individuals must engage in practice before integration occurs. Participants provided retrospective accounts of their practice time for some DSM behaviors; however, more data are needed. Understanding the optimum practice:integration ratio could assist researchers in designing intervention programs with an appropriate dose and scheduled follow up. Evidence suggests that coaching clients in their illness self-management can improve outcomes (Two Feathers et al., 2005; Whittemore, Melkus, Sullivan, & Grey, 2004). Such an approach could be particularly useful for DSM integration, yet more research needs to be done to understand how to best coach clients through inquiry and practice.
DSM integration involves negotiating a place for a multitude of DSM tasks into daily life while also modifying health habits. The TMDSMI presented here offers new insights into how individuals achieve integration in the face of dynamic daily life context, and into where it breaks down. As the incidence and prevalence of diabetes continues to rise in the United States, facilitating DSM will continue to be an important goal. Future studies need to be conducted to continue to develop and test key aspects of the model.
Acknowledgments
I acknowledge Malcolm Cutchin and Cathy Lysack for their valuable feedback on previous versions of this article.
Funding
The author disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The University of North Carolina at Chapel Hill School of Nursing Interventions for Preventing and Managing Chronic Illness grant 2T32NR007091-16 from the National Institute of Nursing Research.
Biography
Heather Fritz, PhD, OTR/L, is a postdoctoral fellow at the Wayne State University Institute of Gerontology in Detroit, Michigan, USA.
Footnotes
Portions of this article were presented at the 12th Annual Society for the Study of Occupation: USA, October 19, 2013, in Lexington, KY.
Declaration of Conflicting Interests
The author declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
DSM education classes were offered as part of another research project being conducted at the clinic. The groups met once every 3 months at the clinic. Class topics included information on diet, nutrition, physical activity, eye health, blood pressure, and cholesterol. The principal investigator in the other research project volunteered time to assist with recording participants’ weight, served snacks, and contributed to the group discussions. Group classes consisted of predominantly Black, low-income women with type 2 diabetes.
Although Charmaz (2006) does not consider axial coding as essential to grounded theory analysis, the extra step of axial coding is not outside of her constructivist interpretation of process, and provides a useful frame.
References
- Agency for Healthcare Research and Quality. National healthcare quality report. 2011 doi: 10.1080/15360280802537332. Retrieved from http://www.innovations.ahrq.gov/content.aspx?id=736. [DOI] [PubMed]
- American Psychological Association. Fact sheet: Wo-men and socioeconomic status. (n.d.) Retrieved from www.apa.org/pi/ses/resources/publications/factsheet-women.aspx.
- Audulv A, Asplund K, Gustaf-Norbergh K. The integration of chronic illness self-management. Qualitative Health Research. 2012;22:332–345. doi: 10.1177/104973231-1430497. [DOI] [PubMed] [Google Scholar]
- Bandura A. Self-efficacy: The exercise of control. New York: W. H. Freeman; 1997. [Google Scholar]
- Bourdieu P. Practical reason. Stanford, CA: Stanford University Press; 1998. [Google Scholar]
- Centers for Disease Control and Prevention. National diabetes fact sheet: National estimates and general information on diabetes and prediabetes in the United States 2011. Atlanta: Author; 2011. [Google Scholar]
- Charmaz K. Constructing grounded theory: A practical guide through qualitative analysis. Thousand Oaks, CA: Sage; 2006. [Google Scholar]
- Churchill S, Jessop D. Reflective and non-reflective antecedents of health-related behaviour: Exploring the relative contributions of impulsivity and implicit self-control to the prediction of dietary behavior. British Journal of Health Psychology. 2011;16:257–271. doi: 10.1348/135910710X498688. [DOI] [PubMed] [Google Scholar]
- Collier J. Photography in anthropology: A report on two experiments. American Anthropologist. 1957;59:843–859. [Google Scholar]
- Crosby R, Noar SM. Theory development in public health promotion: Are we there yet? Journal of Behavioral Medicine. 2010;33:259–263. doi: 10.1007/s10865-010-9260-1. [DOI] [PubMed] [Google Scholar]
- Coster S, Norman I. Cochrane reviews of educational and self-management interventions to guide nursing practice: A review. International Journal of Nursing Studies. 2009;46(4):508–28. doi: 10.1016/j.ijnurstu.2008.09.009.. [DOI] [PubMed] [Google Scholar]
- Dewey J. Human nature and conduct. New York: Modern Library; 1922/1957. [Google Scholar]
- Fitzgerald DT, Davis JY, Connell WK, Hess CM, Funnell MM, Hiss RG. Diabetes Care Profile [survey instrument] 1996 doi: 10.1177/016327879601900205. Retrieved from www.med.umich.edu/mdrtc/profs/survey.html#dcp. [DOI] [PubMed]
- Funnell M, Brown T, Childs B, Haas L, Jensen B, Maryniuk M, Weiss M. National standards for diabetes self-management education. Diabetes Care. 2011;34(1):S89–S96. doi: 10.2337/dc11-S089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gary TL, Genkinger JM, Guallar E, Peyrot M, Brancati FL. Meta-analysis of randomized educational and behavioral interventions in type 2 diabetes. Diabetes Educator. 2003;29(3):488–501. doi: 10.1177/014572170302900313. [DOI] [PubMed] [Google Scholar]
- Glasgow RE, Goldstein MG, Ockene JK, Pronk NP. Translating what we have learned into practice: Principles and hypotheses for interventions addressing multiple behaviors in primary care. American Journal of Preventive Medicine. 2004;27(Suppl. 2):88–101. doi: 10.1016/j.amepre.2004.04.019. Retrieved from www.sciencedirect.com/science/article/pii/S074937-9704000996. [DOI] [PubMed] [Google Scholar]
- Harper D. Talking about pictures: A case for photo elicitation. Visual Studies. 2002;17(1):13–26. doi: 10.1080/14-725860220137345. [DOI] [Google Scholar]
- Hills-Briggs F, Lazo M, Peyrot M, Doswell A, Chang Y, Hill M, Brancati F. Effect of problem solving based diabetes self-management training on diabetes control in a low income patient sample. Journal of General Internal Medicine. 2011;26:972–978. doi: 10.1007/s11606-011-1689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ismail K, Winkley K, Rabe-Hesketh S. Systematic review and meta-analysis of randomized controlled trials of psychological interventions to improve glycaemic control in patients with type 2 diabetes. Lancet. 2004;363(9421):1589–1597. doi: 10.1016/S0140-6736(04)162-02-8. [DOI] [PubMed] [Google Scholar]
- Lal S, Jarus T, Suto M. A scoping review of the photovoice method: Implications for occupational therapy research. Canadian Journal of Occupational Therapy. 2012;79:181–188. doi: 10.2182/cjot.2012.79.3.8. [DOI] [PubMed] [Google Scholar]
- Lindbladh E, Lyttkens CH. Habit versus choice: The process of decision-making in health-related behavior. Social Science & Medicine. 2002;55(3):451–465. doi: 10.1016/S0277-9536(01)00180-0. [DOI] [PubMed] [Google Scholar]
- Lorenz L. A way into empathy: A case of photo-elicitation in illness research. Health. 2011;15:259–275. doi: 10.1177/1363459310397976. [DOI] [PubMed] [Google Scholar]
- Michelson W. Time use: Expanding the explanatory power of the social sciences. Boulder, CO: Paradigm; 2005. [Google Scholar]
- Mulcahy K, Maryniuk M, Peeples M, Peyrot M, Tomky D, Weaver T, Yarborough P. Diabetes self-management education core outcomes measures. Diabetes Educator. 2003;29:768–770. doi: 10.1177/0145721703029005-09. [DOI] [PubMed] [Google Scholar]
- Neal DT, Wood W, Wu M, Kurlander D. The pull of the past: When do habits persist despite conflict with motives? Personality and Social Psychology Bulletin. 2011;37:1428–1437. doi: 10.1177/0146167211419863. [DOI] [PubMed] [Google Scholar]
- Newman S, Steed L, Mulligan K. Self-management interventions for chronic illness. Lancet. 2004;364:1523–1537. doi: 10.1016/S0140-6736(04)17277-2. [DOI] [PubMed] [Google Scholar]
- Nilsen W, Haverkos L, Nebeling L, Taylor V. Maintenance of long term behavior change. American Journal of Health Behavior. 2010;34:643–646. doi: 10.5993/ajhb.34.6.1. Retrieved from http://ehis.ebscohost.com/eds/pdfviewer/pdfviewer?sid=d8d1a9db-cae1-412f-ba01-49cdd989d729%40sessionmgr115&vid=21&hid=101. [DOI] [PubMed] [Google Scholar]
- Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: A meta-analysis of the effect on glycemic control. Diabetes Care. 2002;25:1159–1171. doi: 10.2337/dia-care.25.7.1159. [DOI] [PubMed] [Google Scholar]
- Orbell S, Verplanken B. The automatic component of habit in health behavior: Habit as cue-contingent automaticity. Health Psychology. 2010;29:374–383. doi: 10.1037/a0019596. [DOI] [PubMed] [Google Scholar]
- Ory M, Smith M, Mier N, Wernicke M. The science of sustaining health behavior change: The Health Maintenance Consortium. American Journal or Health Behavior. 2010;34:647–659. doi: 10.5993/ajhb.34.6.2. Retrieved from www.scopus.com/record/display.url?eid=2-s2.0-77957966998&origin=inward&txGid=28C689BDCAC0087B7EA99BB2DB969711.aXczxbyuHHiXgaIW6Ho7g%3a11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peeples M, Tomky D, Mulcahy K, Peyrot M, Siminerio L. Evolution of the American Association of Diabetes Educators’ Diabetes Education Outcomes Project. Diabetes Educator. 2007;33:794–817. doi: 10.1177/0145721707307615. [DOI] [PubMed] [Google Scholar]
- Pentland W, Harvey AS. Future directions. In: Pentland W, Lawton MP, Harvey AS, McColl MA, editors. Time use research in the social sciences. New York: Plenum; 1999. pp. 259–261. [Google Scholar]
- Pink S. Doing visual ethnography: Images, media, and representations in research. London: Sage; 2001. [Google Scholar]
- Riley L. The sandwich generation: Challenges and coping strategies of multigenerational families. Family Journal. 2005;13(1):52–58. doi: 10.1177/1066480704270099. [DOI] [Google Scholar]
- Schulman-Green D, Jaser S, Martin F, Alonzo A, Grey M, McCorkle R, Whittemore R. Processes of self-management in chronic illness. Journal of Nursing Scholarship. 2012;44:136–144. doi: 10.1111/j.1547-5069.2012.01444.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Scientific Software Company. Atlas.ti [software] 2012. [Google Scholar]
- Two Feathers J, Kieffer EC, Palmisano G, Anderson M, Sinco B, Janz M, James SA. Racial and ethnic approaches to community health (REACH) Detroit partnership: Improving diabetes-related outcomes among African American and Latino adults. American Journal of Public Health. 2005;95:1552–1560. doi: 10.2105/AJPH.2005.066134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. 2012 HHS poverty guidelines. 2012 Retrieved from http://aspe.hhs.gov/poverty/12poverty.shtml.
- Whittemore R, Melkus GD, Sullivan A, Grey M. A nurse-coaching intervention for women with type 2 diabetes. Diabetes Educator. 2004;30:795–804. doi: 10.1177/014572170403000515. Retrieved from http://tde.sagepub.com/content/30/5/795.full.pdf+html. [DOI] [PubMed] [Google Scholar]


