Abstract
Hydatid disease of long bone is a rare presentation. Chemotherapy and surgery constitute the standard treatment of choice. Non-union of a pathological fracture of femur particularly due to hydatid disease has been known to be resistant to treatment. These resistant cases require combination drug chemotherapy and excision of the lesion. Reconstruction of a large skeletal defect following resection of the lesion poses a challenge to the orthopaedic surgeons. We discuss the staged treatment of hydatid disease of shaft of femur with resection and cement spacer application followed by reconstruction using massive skeletal allograft under cover of combination drug chemotherapy.
Keywords: infections, musculoskeletal and joint disorders, orthopaedic and trauma surgery
Background
Hydatid disease is a parasitic zoonotic disease, endemic in several areas of the world. The causative organism is Echinococcus granulosus and occasionally, E. multilocularis.1 Visceral organs especially liver, lungs and kidneys have been reported to be the most common sites of involvement. Skeletal involvement accounts for 0.5%–2.5% of all human hydatidosis of which spine is the most common site followed by the pelvis and the long bones, especially femur.1–3 Clinical presentation is mostly asymptomatic. Radiological features are inconclusive. When symptomatic, it is characterised by pain and most commonly pathological fracture at presentation. Although, chemotherapy and surgery are the recommended treatment of choice, resistant cases are difficult to treat. Single-drug therapy may not be sufficient for disease control; hence, a combination drug therapy may be required. Curettage alone may not be adequate, and hence, an excision of the lesion may be necessary.
Case presentation
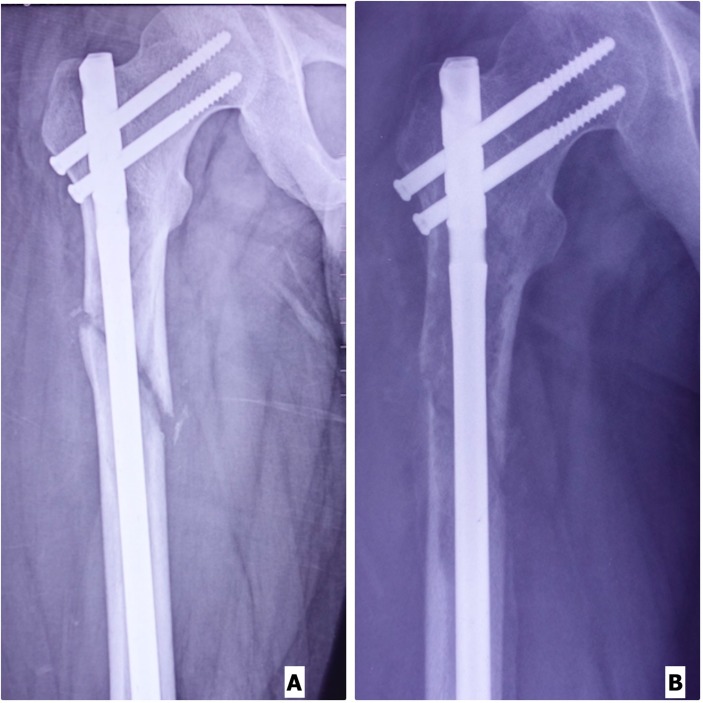
A 25-year-old male sustained subtrochanteric fracture shaft of right femur (figure 1) due to fall from a height. There was no history of pain before the injury. Femoral interlocking nail (figure 2A) was done elsewhere. The follow-up X rays showed non-union of the fracture. In addition, there was progressive lytic lesion around the fracture site which was initially not appreciable in the X-ray (figure 2B). The patient was referred to our institute.
Figure 1.
X-ray of right hip with thigh showing fracture at the subtrochanteric region.
Figure 2.
(A) Immediate postoperative X-ray of right hip with thigh showing reduced fracture with intramedullary nail in situ. (B) Follow-up X-ray of right hip with thigh showing non-union of fracture. Note the expansible lytic lesion around the non-union site.
Investigations
MRI showed elongated cystic lytic lesion involving the upper one-third of the shaft of femur with hyperintense signal in the soft tissue over the anterolateral aspect of the thigh. As the MRI findings was not conclusive, a bone biopsy was done. The histopathological examination revealed hydatid disease of the bone (figure 3).
Figure 3.
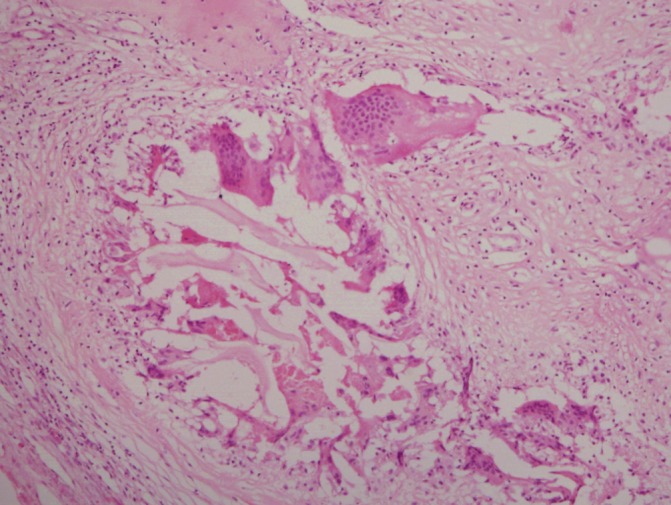
Histopathology showing acellular lamellated membrane of Echinoccocus with dense foreign body type giant cell reaction around them (H&E stain, ×40).
Differential diagnosis
Malignant lesion like sarcoma
Benign cystic lesion like myxoma
Infection
Lymphatic malformation with superadded infection
Cystic metastasis.
Treatment
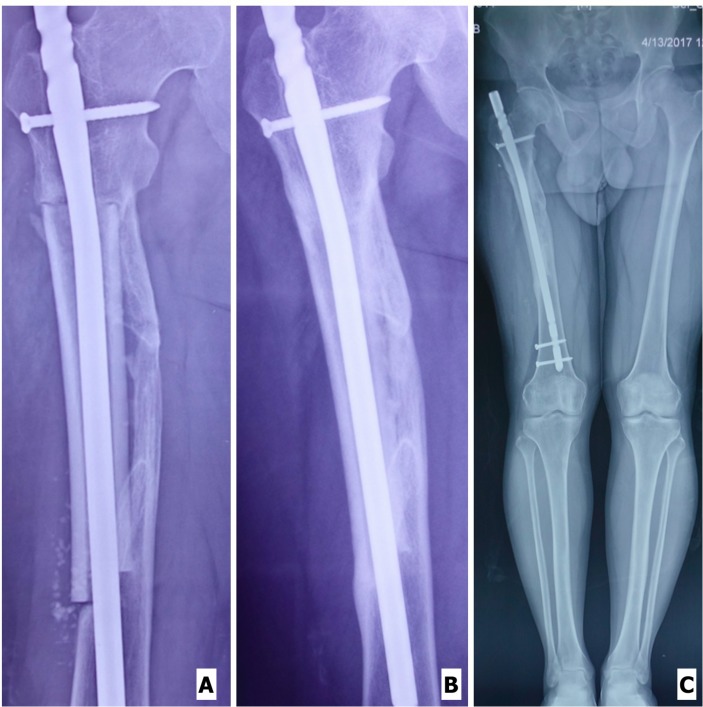
The patient was started on tab. albendazole 400 mg twice daily. Curettage and debridement with hydrogen peroxide, betadine solution and hypertonic saline followed by exchange nailing and cement spacer application were done. At 3 months, MRI was done which showed persistence of infestation. He was then put on combination drug chemotherapy (tab. praziquantel 300 mg once daily in addition to Tab. Albendazole 400 mg twice daily). In view of persistence of disease, excision of the lesion was carried out followed by cement spacer application (figure 4). Intraoperatively, care was taken to keep the margins grossly clear and no hydatid membrane be left behind. The bone marrow from either ends of the native bone was also sent separately for frozen section, which was reported negative. The excised mass was sent for histopathology which was consistent with hydatid disease of bone.
Figure 4.

X-ray of right hip with thigh showing an intramedullary nail with cement spacer in situ.
Reconstruction procedure
After a combination drug chemotherapy of 6 months, the patient was declared disease-free from radiological point of view as revealed by the MRI. In view of severe loss of bone segment, a reconstruction plan was made using a massive femoral shaft allograft. Combined spinal epidural anaesthesia was given and the patient was placed in a left lateral position. A 2.5 cm incision was given in the supra trochanteric region to remove the intramedullary nail. Lateral incision about 18 cm long was given over previous scar mark to remove the cement spacer. Thorough wash was done using betadine solution, hydrogen peroxide and hypertonic saline. A step-cut osteotomy was made over the proximal and distal fragments of the host femur. A freeze-dried irradiated femoral shaft allograft was selected from the bone bank and prepared using betadine solution, hydrogen peroxide, normal saline and absolute alcohol. Femoral shaft allograft of about 14 cm was prepared and matching step cut osteotomy was made corresponding to the step cuts in the host femur. The prepared allograft was placed bridging the host bone matching the step cuts. Fixation was done using an intramedullary nail. As the femoral nail could not be pushed more distally in the host bone even with the smallest available diameter nail (probably due to mismatch in the femoral bow), a proud nail was accepted and locking done both proximally and distally (figure 5A). Wound closed in layers over a drain which was removed after 48 hours. Postoperatively, the patient was continued with combined drug chemotherapy for 6 months.
Figure 5.
(A) X-ray of right hip with thigh with an allograft fixed with an intramedullary nail in situ. (B) X-ray of right hip with thigh showing full incorporation of the allograft into the host bone. (C) Standing scanogram of bilateral limbs with incorporated allograft in right thigh. There is no apparent limb length discrepancy.
Outcome and follow-up
At 6 months, the patient was declared disease-free as revealed from the MRI. At the latest follow-up of 2 years, the patient is doing well. There is complete incorporation of the allograft with the host bone (figure 5B). There is no apparent limb length discrepancy and the patient is doing well (figure 5C).
Discussion
The symptoms of bone hydatid cyst are non-specific and often misguiding. Diagnosis of skeletal hydatid disease is challenging. Imaging studies are not very specific for diagnosis and often the diagnosis is suspected when the patient presents with pathological fracture. The eight-test battery for immunodiagnosis, though proved to be most sensitive and specific for alveolar and hepatic echinococcosis,4 is not commonly done for skeletal cysts because the disease in the bone induces less antibody response and is more difficult to detect by the common serological methods.1 Accurate diagnosis is often made histologically only. Although, in cases with suspected echinococcosis, diagnostic biopsy or aspiration is contraindicated,5 in this case, it was carried as our first possibility was neoplasm and we were lucky enough not to have any hypersensitivity reaction. Hydatid disease of the bone is difficult to treat, often is recurrent and progressive despite treatment.6 7 Surgery is usually the treatment of choice combined with chemotherapy. Surgery involves debridement of the cyst, which may be intralesional, that is, curettage, or extralesional, that is, wide resection. Curettage is supplemented with application of scolicidal agents like hypertonic saline, hydrogen peroxide, betadine, etc. Curettage often leaves some residual disease which is responsible for recurrence. In this case, there was recurrence despite curettage, hence, wide resection was necessary to achieve local control. Even after surgical resection, the disease cannot be completely cured; hence, effective chemotherapy is of great benefit. Albendazole alone has been found ineffective in the treatment of hydatid cyst who are surgical candidates especially in cases where intraoperative spillage is expected. Hence, praziquantel was added. The combination chemotherapy has been found to be safe and effective in treating human hydatidosis.8 There is no clear consensus regarding the duration of chemotherapy before and after the surgery in case of bony hydatidosis. Although, there have been reports of no chemotherapy to monotherapy and/or combination chemotherapy ranging from few days to few months, we decided to go for prolong combination chemotherapy in view of recurrence. Further, the surgery was also planned in stages to reduce the recurrence rate and prevent the failure of reconstruction. Resection left a massive bone defect which was filled up with cement spacer in first stage. Reconstruction of such massive defect was another challenge as the autograft would be insufficient to bridge the large defect. In addition, the multiple graft site comorbidities were of concern, as the patient would require the fibula as well as both the iliac crest autografts to fill up the defect. Furthermore, the strength of the graft would significantly delay the weight bearing in the patient. Hence, the reconstruction was carried out with massive skeletal allograft. Although, the use of allograft has its own potential risk of infection and disease transmission, and, complications like non-union and fracture of the allograft, the size of the defect and age of the patient suited the use of skeletal allograft. There are very few reports of the use of massive skeletal allograft for reconstruction of bone defects after wide resection for hydatid disease of the femur which are summarised in table 1.9–11 Current case report further strengthens and supports the use of a massive skeletal allograft as a reliable reconstructive procedure after extensive bone resection for osseous hydatid disease.
Table 1.
Reported cases of hydatid cyst of femur treated by massive allograft
| Authors | Disease location | Chemotherapy | Duration of chemotherapy | Surgical intervention | Follow-up | Result |
| Neogi et al 9 | Femoral shaft | Albendazole | Twice daily for 4 weeks followed by a gap of 2 weeks and cycle repeated | Resection+femoral allograft | 26 months | Full incorporation of the allograft |
| Jain et al 10 | Iliac blade | Albendzole monotherapy | One month | Resection+allograft+ autograft (Rib) | 6 months | No abnormality in radiology |
| Domingo et al
11
(two cases) |
1. Femoral diaphysis 2. Femoral metaphysis |
No chemotherapy Albendazole |
Preoperatively for 1 month and 6 months postoperatively | Femoral shaft allograft Allograft prosthesis composite of proximal femur |
9 years 5 years |
Excellent outcome Excellent result |
| Current case | Femoral shaft | Albendazole+praziquantel | 6 months preoperatively+6 months postoperatively | Femoral shaft allograft | 2 years | Excellent result |
Learning points.
Hydatid disease of bone is rare and difficult to treat.
Combination drug chemotherapy is preferred to monotherapy if the response is not seen early, that is, in resistant cases.
Excision of the mass is preferable to curettage to eliminate the disease in accessible sites.
Large skeletal defect can be managed with massive allograft.
The authors recommend aggressive approach for hydatid disease of bone in the form of combination drug chemotherapy along with excision of the mass.
Footnotes
Contributors: DG prepared the manuscript. RM is the chief surgeon and provided valuable inputs in drafting the manuscript. SD was responsible for the collection of data and preparation of draft.
Funding: Wellcome Trust DBT/India Alliance. Grant number: IA/RTF/15/1/1003.
Competing interests: DG is the recipient of grant from Wellcome Trust DBT/India Alliance.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Eckert J, Gemmell MA, Meslin FX, et al. WHO/OIE manual on echinococcosis in humans and animals: a public health problem of global concern. Paris: World Organisation for Animal Health, 2002:20–72. [Google Scholar]
- 2. Arik HO, Arican M, Cetin NK, et al. Primary intraosseous hydatid cyst of femur. Iran Red Crescent Med J 2015;17:e21070 10.5812/ircmj.21070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Zlitni M, Ezzaouia K, Lebib H, et al. Hydatid cyst of bone: diagnosis and treatment. World J Surg 2001;25:75–82. 10.1007/s002680020010 [DOI] [PubMed] [Google Scholar]
- 4. Song XH, Ding LW, Wen H. Bone hydatid disease. Postgrad Med J 2007;83:536–42. 10.1136/pgmj.2007.057166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Tatari H, Baran O, Sanlidağ T, et al. Primary intramuscular hydatidosis of supraspinatus muscle. Arch Orthop Trauma Surg 2001;121:93–4. 10.1007/PL00013775 [DOI] [PubMed] [Google Scholar]
- 6. Arazi M, Erikoglu M, Odev K, et al. Primary echinococcus infestation of the bone and muscles. Clin Orthop Relat Res 2005;432:234–41. 10.1097/01.blo.0000149816.86222.2d [DOI] [PubMed] [Google Scholar]
- 7. Salamone G, Licari L, Randisi B, et al. Uncommon localizations of hydatid cyst. Review of the literature. G Chir 2016;37:180–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Alvela-Suárez L, Velasco-Tirado V, Belhassen-Garcia M, et al. Safety of the combined use of praziquantel and albendazole in the treatment of human hydatid disease. Am J Trop Med Hyg 2014;90:819–22. 10.4269/ajtmh.13-0059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Neogi DS, Kumar V, Malhotra R. Femoral allograft in the management of osseous hydatidosis presenting as femoral shaft non-union. Arch Orthop Trauma Surg 2009;129:1627–32. 10.1007/s00402-008-0797-1 [DOI] [PubMed] [Google Scholar]
- 10. Jain S, Chopra P. Cystic echinococcosis of the pelvic bone with recurrences: a case report. Korean J Parasitol 2011;49:277–9. 10.3347/kjp.2011.49.3.277 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Muscolo DL, Zaidenberg EE, Farfalli GL, et al. Use of massive allografts to manage hydatid bone disease of the femur. Orthopedics 2015;38:e943–6. 10.3928/01477447-20151002-92 [DOI] [PubMed] [Google Scholar]