Description
A 29-year-old man presented with a 10-year history of pain in his right ankle. The ankle was tender and swollen, and there was Achilles tendinitis. He had no complaints of buttock pain, abdominal pain, dysuria or a feeling of incomplete voiding. Skin examination was normal. Laboratory investigations revealed a leucocyte count of 6.0×109/L and a serum C reactive protein level of 5.21 mg/dL. Liver and renal function tests were normal. Rheumatoid factor, anticyclic citrullinated peptide antibody and antinuclear antibody were negative. Urinalysis was positive for occult blood, but there was no leucocyturia. Locus B human leukocyte antigen (HLA) typing was positive for B27. Plain radiography of the right ankle joint showed narrowing of the subtalar joint space and heel spurs on the plantar aspect of the calcaneus (figure 1). Contrast-enhanced CT scans demonstrated enhanced lesions in the peripheral zone of the prostate (figure 2). Culture of urine taken after prostate massage revealed Neisseria meningitidis. The diagnosis was reactive arthritis associated with prostatitis caused by N. meningitidis. He was successfully treated with antibiotics and low-dose prednisolone followed by methotrexate.
Figure 1.
Plain radiograph of the right ankle joint showing narrowing of the subtalar joint space (arrowhead) and heel spurs on the plantar aspect of the calcaneus (arrow).
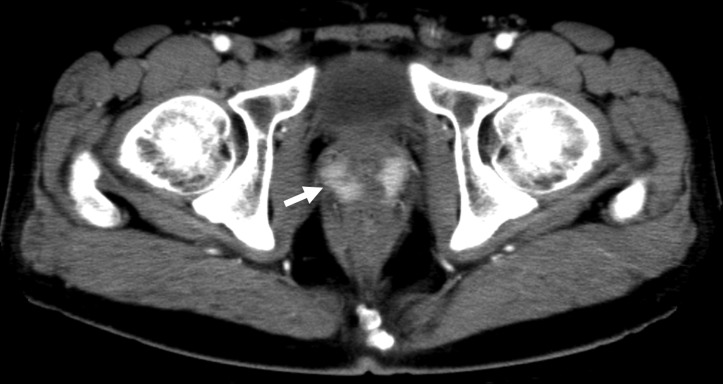
Figure 2.
Contrast-enhanced CT scans showing enhancing lesions (arrow) in the peripheral zone of the prostate.
Reactive arthritis is a form of HLA-B27-associated peripheral spondyloarthropathy that arises following infection, but the pathogens cannot be cultured from the affected joints.1 In most cases, a preceding enteric or genitourinary infection triggers the reactive arthritis. In our case, we could not confirm that the urinary infection preceded the onset of arthritis. However, the patient had several features of reactive arthritis, including positive HLA-B27 serology, asymmetric chronic arthritis in the lower extremities, enthesitis and persistent urinary tract infection. Therefore, it is reasonable to consider that the arthritis was associated with chronic asymptomatic prostatitis in this patient.
Organisms that induce reactive arthritis classically include Chlamydia, Yersinia, Salmonella, Shigella, Campylobacter and Clostridium spp.1 Our case is unique in that the patient developed chronic reactive arthritis associated with prostatitis attributable to N. meningitidis, which has not been previously described as a causative organism. Interestingly, in one report, PCR and sequencing analysis identified N. meningitidis DNA in synovial fluid samples from 1 of 15 patients with reactive arthritis, although the pathogenic role was unclear.2
The prognosis of reactive arthritis is generally good. Nevertheless, this type of arthritis can run a chronic course and may cause permanent joint damage. Our case further emphasises the importance of exploring possible sites of infection, even if the infection is asymptomatic, in a patient with asymmetric chronic arthritis of the lower extremities.
Learning points.
Reactive arthritis is a form of HLA-B27-associated peripheral spondyloarthropathy that arises following infection.
Organisms that trigger reactive arthritis include Chlamydia, Yersinia, Salmonella, Shigella, Campylobacter, Clostridium spp., and several other bacteria, including Neisseria.
In a patient with suspected reactive arthritis, it is important to look for possible sites of infection, even if the infection is asymptomatic.
Footnotes
Contributors: KK and YMo were involved in conception or design of the work. KK is responsible for acquisition of data. KK, TM, YMi and YMo are responsible for analysis and interpretation of the data. KK, TM and YMo drafted or revised the manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: KK, TM and YMo received scholarship donations from AbbVie, Actelion, Astellas, Bristol-Myers, Chugai, Daiichi Sankyo, Eisai, Eli Lilly, Japan Blood Products Organization, Mitsubishi-Tanabe, MSD, Pfizer, Shionogi, Takeda, Teijin and UCB. YMi received scholarship donations from Asahi Kasei, Astellas, Daiichi Sankyo, Kissei, Nippon Shinyaku, Ono, Pfizer and Takeda.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Girschick HJ, Guilherme L, Inman RD, et al. Bacterial triggers and autoimmune rheumatic diseases. Clin Exp Rheumatol 2008;26:S12–17. doi:10.1080/15563650802520675 [PubMed] [Google Scholar]
- 2.Cuchacovich R, Japa S, Huang WQ, et al. Detection of bacterial DNA in Latin American patients with reactive arthritis by polymerase chain reaction and sequencing analysis. J Rheumatol 2002;29:1426–9. doi:10.1080/15563650802520675 [PubMed] [Google Scholar]