Abstract
Background
Cancer incidence and mortality rates in the US are declining, but this decrease may not be observed in rural areas where residents are more likely to live in poverty, smoke, and forego cancer screening. However, there is limited research exploring national rural-urban differences in cancer incidence and trends.
Methods
We analyzed data from the North American Association of Central Cancer Registries' public use dataset, which includes population-based cancer incidence data from 46 states. We calculated age-adjusted incidence rates, rate ratios, and annual percentage change (APC) for: all cancers combined; selected individual cancers; and cancers associated with tobacco use and human papillomavirus (HPV). Rural-urban comparisons were made by demographic, geographic, and socioeconomic characteristics for 2009 to 2013. Trends were analyzed for 1995 to 2013.
Results
Combined cancers incidence rates were generally higher in urban populations, except for the South, though the urban decline in incidence rate was greater than in rural populations (10.2% vs. 4.8%, respectively). Rural cancer disparities included higher rates of tobacco associated, HPV associated, lung and bronchus, cervical , and colorectal cancers across most population groups. Further, HPV-associated cancer incidence rates increased in rural areas (APC=0.724, p<0.05) while temporal trends remained stable in urban areas.
Conclusions
Cancer rates associated with modifiable risks - tobacco, HPV, and some preventive screening modalities (e.g. colorectal and cervical cancers) - were higher in rural compared to urban populations.
Impact
Population-based, clinical, and/or policy strategies and interventions that address these modifiable risk factors could help reduce cancer disparities experienced in rural populations.
Keywords: rural health, neoplasms, epidemiology, incidence
Introduction
Cancer mortality rates across the nation have been decreasing, but this decline has not been experienced equally across demographic groups. For some racial/ethnic minorities, incidence and mortality rates have declined more slowly than for whites, which is also the case for rural areas (1). For many rural populations, cancer mortality is not decreasing; it is steady and, in some cases, rising. Several studies have documented persistently elevated cancer incidence and mortality in rural communities compared to urban areas (2-5). As nearly 1 in 5 Americans lives in a rural area, disparities among this population can have a broad impact on the nation's health (6).
The reasons for these cancer health disparities are complex. In 2010-2012, the highest rates of poverty and uninsured status in the nation were found in small rural counties and in large inner cities (7). While the Affordable Care Act increased insurance coverage, many states with large rural populations did not expand Medicaid, leaving millions of people still without health insurance (8). Furthermore, there are documented barriers to health care access in rural communities. Many rural residents live in health care provider shortage areas, may have fewer choices in care, and may need to travel long distances just to see a primary care physician. Thus, it is not surprising that studies have found that rural residents have lower rates of cancer screening and experience lower quality cancer care (2,3). Further, numerous studies have identified higher rates of cancer-risk behaviors among rural residents, which can contribute to the elevated incidence rates. Higher rates of tobacco use and obesity in rural populations are consistently reported (9-13). Additionally, human papillomavirus (HPV) vaccination rates are lagging in rural areas, with lower rates associated with increasing rurality (14).
The preponderance of evidence shows that rural residents may be at greater risk for cancer, and there has been an increasing call for further research efforts and funding investments in cancer control based upon geographic location, broadly, and rural locations, specifically (15,16). However, there is a paucity of research that has comprehensively characterized the rural cancer burden. Previous investigations have been limited to examining specific rural regions (e.g. Appalachia), data from only Surveillance, Epidemiology, and End Results (SEER) registries, or national data of single or limited cancer types (5,17-26). Therefore, our objective is to describe the national rural cancer burden by assessing rural-urban differences in incidence rates and trends by overall cancer, individual cancers, and by sub-groups of cancers (tobacco- and HPV-associated).
Materials and Methods
We analyzed data from the North American Association of Central Cancer Registries (NAACCR) Cancer in North America public use data set, which contains data from population-based cancer registries in the United States and Canada who authorized inclusion in the dataset and whose registry was certified as meeting gold or silver data quality standards by NAACCR (27). Gold and silver quality standards are based on level of data completeness (95+% for gold certification and 90+% for silver certification), accuracy, and timeliness of submission of data to NAACCR (28).This dataset included 46 states in the United States and the District of Columbia, representing 93% of the United States population. Four states (Kansas, Maryland, Minnesota, and Vermont) did not consent for their data to be included. The dataset includes variables on demographics, registry, county level characteristics (i.e. rural and poverty status), and tumor characteristics (e.g. site, histology, stage).
Rural and urban were defined using the 2013 Beale codes (also known as Rural-Urban Continuum Codes or RUCCs), which categorize counties based upon their population size and proximity to metropolitan areas. A Beale code or RUCC of 1-3 indicates a metro (urban) county while a code of 4-9 indicates a non-metro (rural) county as outlined in the map in Supplemental Figure 1 (29).
Changes in cancer case reporting requirements occurred in 2001 in response to the shift from International Classification of Disease Oncology-2 (ICD-O-2) to ICD-O-3 histology and behavior codes. Our analysis only included cases that were malignant in both ICD-O-2 and ICD-O-3 to allow for congruency in analysis over time. Primary site of cancer diagnosis was defined by the ICD-O-3 classification. We also categorized cancer groups associated with two different carcinogenic exposures-- tobacco and HPV. Tobacco-associated cancers were those identified by the 2014 Surgeon General's Report, including oral cavity and pharynx, larynx, esophagus, trachea, lung and bronchus, acute myeloid leukemia, stomach, liver, pancreas, kidney and ureter, cervix, bladder, and colorectal (30). HPV-associated cancers were determined by ICD-O-3 code for primary site and relevant histology, i.e. cervical carcinomas and squamous cell carcinomas of the oropharynx, vagina, vulva, penis, anus, and rectum (31).
We used SEER*Stat 8.3.2 to calculate age-adjusted incidence rates and rate ratios utilizing Tiwari modifications and to determine annual percentage change (APC) for selected individual cancer sites and groups (32). Rate ratios with p-values less than 0.05 indicated statistically significant rural-urban differences in rates. Rural-urban incidence rate comparisons were made by sex, race/ethnicity, U.S. census division, and county-level poverty rate for 2009 to 2013. Race/ethnic groups were defined as Non-Hispanic (NH) white, NH black, and Hispanic. U.S. Census Division include the Northeast, South, Midwest, and West as outlined in the map in Supplemental Figure 1. APC and overall percentage change in cancer rates were analyzed for 1995 to 2013. APCs with p-values less than 0.05 indicated a statistically significant percentage change in rates. This study was determined to be non-human subjects research by the Springfield Committee for Research Involving Human Subjects.
Results
Between 2009 and 2013, 1,215,260 invasive cancer cases were diagnosed in rural populations comprising 16.7% of all cancer cases (Table 1). More than three-fourths (75.8%) of rural cancer cases were diagnosed in the Midwest and the South. Most cases in rural areas were NH white (87.8%), compared to 75.3%. of urban cases. More than half of both rural and urban cancer cases were diagnosed in individuals 65 years of age or older (57.1% and 53.2%, respectively). One third of rural cancer cases were diagnosed in counties with greater than 20% of the population living in poverty compared to 10.7% of urban cases.
Table 1. Demographic Characteristics of Invasive Cancer Cases in Rural and Urban Areas, 2009-2013.
| Rural | Urban | |
|---|---|---|
| N (%) | N (%) | |
|
| ||
| Total Cases | 1,215,260 (16.7%) | 6,073,283 (83.3%) |
|
| ||
| U.S. Census Region | ||
| Northeast | 134,197 (11.0%) | 1,411,055 (23.2%) |
| Midwest | 373,953 (30.8%) | 1,157,272 (19.1%) |
| South | 546,632 (45.0%) | 2,130,224 (35.1%) |
| West | 160,478 (13.2%) | 1,374,732 (22.6%) |
|
| ||
| Sex | ||
| Male | 646,302 (53.1%) | 3,069,294 (50.5%) |
| Female | 568,866 (46.9%) | 3,003,288 (49.5%) |
|
| ||
| Race/Ethnicity | ||
| Non Hispanic White | 1,066,639 (87.8%) | 4,571,767 (75.3%) |
| Non Hispanic Black | 84,207 (6.9%) | 688,268 (11.3%) |
| Hispanic | 31,675 (2.6%) | 507,150 (8.4%) |
| Other | 22,784 (1.9%) | 223,674 (3.7%) |
| Unknown | 9,955 (0.8%) | 82,424 (1.4%) |
|
| ||
| Age | ||
| 0-19 | 9,384 (0.8%) | 59,312 (1.0%) |
| 20-44 | 70,405 (5.8%) | 464,105 (7.6%) |
| 45-64 | 441,423 (36.3%) | 2,316,831 (38.1%) |
| 65+ | 694,048 (57.1%) | 3,233,035 (53.2%) |
|
| ||
| County Poverty Level | ||
| 0-9.99% | 69,566 (5.7%) | 1,019,614 (16.8%) |
| 10-19.99% | 744,946 (61.3%) | 4,403,852 (72.5%) |
| 20+% | 400,748 (33.0%) | 649,817 (10.7%) |
Primary Site by Sex
The incidence rates for all sites combined were higher in urban populations for both sexes combined and for females (Table 2). The all sites combined incidence rate in rural and urban populations was 446.4 and 448.7 per 100,000, respectively. The rate of tobacco-associated cancers were higher in both sexes combined and individually, with a rural rate in both sexes combined of 205.8 per 100,000 compared to a rate of 192.0 in urban populations. Rates of HPV-associated cancer were higher in rural females compared to urban (15.2 vs. 13.4 per 100,000, respectively). Additionally, for both sexes combined and for males and females analyzed separately, oral and pharynx, esophagus, colon and rectum, lung and bronchus, larynx, and kidney and renal pelvis cancers each were higher in rural populations compared to urban. Urban populations had higher rates of breast (female), prostate, stomach, liver and intrahepatic duct, pancreas, melanoma, thyroid, Non-Hodgkin lymphoma, and endometrial cancer.
Table 2. Invasive cancer incidence rates by primary site, rural and urban, all races, 2009-2013.
| Rural | Urban | |||||
|---|---|---|---|---|---|---|
| All Rates | Male Rates | Female Rates | All Rates | Male Rates | Female Rates | |
| All sites | 446.4b | 502.1 | 405.4b | 448.7 | 501.1 | 412.5 |
| Tobacco-associated | 205.8b | 266.0b | 155.8b | 192.0 | 248.3 | 147.9 |
| HPV-associated | 12.6b | 9.9 | 15.2b | 11.7 | 10.0 | 13.4 |
| Oral cavity and pharynx | 12.2b | 18.3b | 6.7b | 11.2 | 16.9 | 6.2 |
| Esophagus | 5.1b | 8.9b | 1.7b | 4.6 | 8.0 | 1.8 |
| Stomach | 5.8b | 8.1b | 3.8b | 6.9 | 9.5 | 4.8 |
| Colon and rectum | 43.9b | 50.5b | 38.2b | 40.1 | 46.2 | 35.1 |
| Liver and intrahepatic duct | 6.3b | 9.6b | 3.4b | 7.9 | 12.3 | 4.2 |
| Pancreas | 11.9b | 13.7b | 10.4b | 12.5 | 14.2 | 11.0 |
| Larynx | 4.4b | 7.3b | 1.8b | 3.4 | 6.0 | 1.3 |
| Lung and bronchus | 70.2b | 86.7b | 57.1b | 61.2 | 72.5 | 52.8 |
| Melanoma | 19.9b | 24.1b | 16.9b | 20.1 | 26.1 | 15.9 |
| Breast | -- | -- | 113.4b | -- | -- | 124.8 |
| Cervical | -- | -- | 8.4b | -- | -- | 7.6 |
| Endometrial | -- | -- | 25.0b | -- | -- | 25.7 |
| Ovary | -- | -- | 11.3b | -- | -- | 11.7 |
| Prostate | -- | 114.1b | -- | -- | 124.5 | -- |
| Testis | -- | 5.5 | -- | -- | 5.5 | -- |
| Urinary bladder | 20.9b | 36.0 | 8.8 | 20.6 | 36.1 | 8.9 |
| Kidney and renal pelvis | 16.9b | 21.9b | 12.3b | 15.9 | 21.6 | 11.1 |
| Brain and other nervous system | 6.7b | 7.8 | 5.6 | 6.6 | 7.7 | 5.6 |
| Thyroid | 12.0b | 5.8b | 18.2b | 14.4 | 7.2 | 21.2 |
| Hodgkin lymphoma | 2.6 | 3.0 | 2.3 | 2.7 | 3.1 | 2.4 |
| Non-Hodgkin lymphoma | 18.2b | 21.8b | 15.3b | 19.2 | 23.2 | 16.0 |
| Myeloma | 5.9b | 7.4b | 4.8b | 6.5 | 8.1 | 5.3 |
| Leukemia | 13.5b | 17.1 | 10.5 | 13.3 | 17.1 | 10.4 |
Rates are expressed per 100,000 people and age-adjusted to the 2000 US standard population.
The rate ratio indicates that the rural rate is statistically significantly different than the urban rate (p<0.05).
Race/Ethnicity
Urban populations had higher all cancer combined incidence rates across sexes and racial/ethnic groups with the exception of NH black males, where there was no rural-urban difference (Table 3). Tobacco-associated cancer rates were higher in rural males across NH racial groups. For women, rates were higher in rural NH whites and Hispanics, but no rural-urban differences in rates among NH blacks. Elevated HPV-associated cancers were found in rural areas amongst all sex and race/ethnic groupings except NH black males and Hispanic females where there were no rural-urban differences. Lung and bronchus cancer rates were higher in rural areas for all sex and race/ethnic groupings except for NH black women amongst whom rates are higher in urban populations. Colorectal cancer rates were higher in rural NH white and black men and women, but there was no rural-urban difference in rates among Hispanics. Cervical cancer rates were higher among rural NH whites and blacks than their urban peers, but there was no difference in Hispanics. Higher rates of breast, prostate, and thyroid cancers were seen in urban populations across sex and racial/ethnic groupings.
Table 3. Cancer incidence rates by primary site by race/ethnicity.
| Rural | Urban | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| All Rates | Male Rates | Female Rates | All Rates | Male Rates | Female Rates | |
|
| ||||||
| All Cancers | ||||||
|
| ||||||
| NH White | 449.5c | 501.5c | 410.8c | 464.4 | 510.1 | 433.1 |
| NH Black | 458.7c | 567.8 | 384.6c | 471.4 | 570.7 | 404.9 |
| Hispanic | 322.7c | 349.5c | 306.3c | 350.9 | 393.5 | 325.2 |
|
| ||||||
| Tobacco-Associated Cancers | ||||||
|
| ||||||
| NH White | 206.6c | 266.8c | 156.3c | 197 | 253.7 | 151.5 |
| NH Black | 216.1c | 292.3c | 159.5c | 209.9 | 276.8 | 163.7 |
| Hispanic | 152.4 | 189.2c | 119.6c | 150 | 195.5 | 116 |
|
| ||||||
| HPV-Associated Cancers | ||||||
|
| ||||||
| NH White | 12.8c | 10.3c | 15.2c | 12.3 | 11 | 13.6 |
| NH Black | 13.1c | 10.2 | 16.0c | 12.4 | 9.6 | 14.7 |
| Hispanic | 8.9c | 5.2c | 13.1 | 10.1 | 6.3 | 13.7 |
|
| ||||||
| Selected Individual Cancers | ||||||
|
| ||||||
| Prostate | ||||||
| NH White | --- | 108.1c | --- | --- | 116.2 | --- |
| NH Black | --- | 190.5c | --- | --- | 199 | --- |
| Hispanic | --- | 78.1c | --- | --- | 106.7 | --- |
|
| ||||||
| Breast | ||||||
| NH White | --- | --- | 114.3c | --- | --- | 131.4 |
| NH Black | --- | --- | 118.2c | --- | --- | 125.6 |
| Hispanic | --- | --- | 81.6c | --- | --- | 92.5 |
|
| ||||||
| Lung and Bronchus | ||||||
| NH White | 71.7c | 87.3c | 59.2c | 65.4 | 75.4 | 58 |
| NH Black | 70.1c | 104.5c | 45.0c | 67 | 89.7 | 51.9 |
| Hispanic | 36.7c | 45.7c | 29.2c | 32.3 | 41.9 | 25.4 |
|
| ||||||
| Colorectal | ||||||
| NH White | 43.2c | 49.7c | 37.6c | 39.5 | 45.2 | 34.7 |
| NH Black | 53.8c | 63.7c | 46.8c | 48.8 | 58 | 42.5 |
| Hispanic | 36.6 | 42.5 | 31.1 | 35.6 | 43 | 29.9 |
|
| ||||||
| Urinary Bladder | ||||||
| NH White | 22.1c | 38.0c | 9.2c | 23.3 | 40.5 | 10 |
| NH Black | 10.5c | 16.9c | 6.1c | 12.1 | 20.2 | 6.8 |
| Hispanic | 10.3c | 16.8c | 4.7 | 11.4 | 20.1 | 5.2 |
|
| ||||||
| Melanoma | ||||||
| NH White | 22.1c | 26.5c | 18.9c | 26.2 | 33 | 21.3 |
| NH Black | 1.3c | 1.3 | 1.3c | 1 | 1.1 | 0.9 |
| Hispanic | 5.5c | 6.1c | 5.3c | 4.5 | 5 | 4.2 |
|
| ||||||
| Kidney and Renal Pelvis | ||||||
| NH White | 16.8c | 21.9 | 12.2c | 16.1 | 21.9 | 11.1 |
| NH Black | 17.5 | 22.4c | 13.5 | 18 | 24.7 | 12.9 |
| Hispanic | 16.6 | 20.2 | 13.2c | 15.8 | 20.7 | 11.9 |
|
| ||||||
| Non-Hodgkin Lymphoma | ||||||
| NH White | 18.7c | 22.4c | 15.6c | 20.1 | 24.3 | 16.7 |
| NH Black | 12.5c | 14.5c | 10.7c | 14.6 | 17.7 | 12.2 |
| Hispanic | 14.9 | 16.8c | 13.3 | 17.4 | 20.1 | 15.2 |
|
| ||||||
| Leukemia | ||||||
| NH White | 13.8c | 17.4c | 10.7 | 14 | 18 | 10.8 |
| NH Black | 10.1 | 13 | 8.1 | 10.5 | 13.3 | 8.6 |
| Hispanic | 10.0c | 12 | 8.1c | 10.7 | 13.1 | 8.9 |
|
| ||||||
| Oral Cavity and Pharynx | ||||||
| NH White | 12.5c | 18.7c | 6.8 | 12.2 | 18.4 | 6.7 |
| NH Black | 11.3c | 17.7c | 5.8c | 9.3 | 14.7 | 5.2 |
| Hispanic | 6.6c | 9.3c | 3.9 | 7.2 | 10.9 | 4.1 |
|
| ||||||
| Endometrial | ||||||
| NH White | --- | --- | 25.3c | --- | --- | 26.5 |
| NH Black | --- | --- | 23.3c | --- | --- | 25.2 |
| Hispanic | --- | --- | 19.0c | --- | --- | 21.8 |
|
| ||||||
| Thyroid | ||||||
| NH White | 12.8c | 6.3c | 19.3c | 15.7 | 8.2 | 23 |
| NH Black | 6.7c | 2.7c | 10.7c | 9.2 | 3.8 | 13.6 |
| Hispanic | 9.0c | 4.2c | 14.7c | 12.8 | 5.3 | 20 |
|
| ||||||
| Pancreas | ||||||
| NH White | 11.8c | 13.6c | 10.1c | 12.4 | 14.2 | 10.8 |
| NH Black | 15.1c | 16.5 | 13.8 | 15.8 | 17.3 | 14.6 |
| Hispanic | 10.7 | 11.1 | 10.3 | 11.2 | 12.2 | 10.3 |
|
| ||||||
| Esophagus | ||||||
| NH White | 5.1c | 9.0c | 1.7c | 5 | 8.7 | 1.9 |
| NH Black | 5.9c | 10.1c | 2.4 | 4.5 | 7.3 | 2.4 |
| Hispanic | 3 | 4.9 | 1.1 | 2.8 | 5 | 1.1 |
|
| ||||||
| Larynx | ||||||
| NH White | 4.3c | 7.2c | 1.8c | 3.5 | 6 | 1.4 |
| NH Black | 5.8c | 11.5c | 1.9 | 4.5 | 8.6 | 1.8 |
| Hispanic | 2.6 | 4.4 | 0.8 | 2.6 | 5.1 | 0.7 |
|
| ||||||
| Brain and Other Nervous System | ||||||
| NH White | 7.2c | 8.4c | 6.0c | 7.5 | 8.8 | 6.4 |
| NH Black | 3.8 | 4.4c | 3.3 | 4.2 | 4.9 | 3.7 |
| Hispanic | 4.7c | 5.2c | 4 | 5.2 | 6 | 4.5 |
|
| ||||||
| Cervix | ||||||
| NH White | --- | --- | 8.0c | --- | --- | 6.9 |
| NH Black | --- | --- | 10.8c | --- | --- | 9.8 |
| Hispanic | --- | --- | 9.4 | --- | --- | 9.9 |
Rates are expressed per 100,000 people and age-adjusted to the 2000 US standard population.
NH=Non-Hispanic
The rate ratio indicates that the rural rate is statistically significantly different than the urban rate (p<0.05).
Geographic Census Region
All cancer combined incidence rates were higher in urban populations across census regions, except the South where rates were higher in rural areas (449.1 vs. 440.9 per 100,000 in rural and urban areas, respectively) (Table 4). Tobacco-associated, HPV-associated, and lung and bronchus cancers were highest in rural areas across regions, except for the Midwest where there were no rural-urban differences. Colorectal cancer incidence rates were higher in rural areas, except for the West where there was no rural-urban difference. Oral cavity and pharynx, esophagus, and larynx cancers were higher in rural areas across regions. Cervical cancer rates were higher in rural areas of the Midwest and South, but no differences were seen in other regions. Breast, prostate, and thyroid cancers incidence rates were higher in urban areas across all regions. Stratifications by race/ethnicity showed some different dynamics for colorectal cancer. Rates were higher in urban blacks in the Northeast, Midwest, and West compared to their rural peers, but the rate in the black South was higher in rural populations (Supplementary Table 1). Hispanics in the rural West also had a higher colorectal cancer rate than their urban peers.
Table 4. Cancer Incidence Rates by U.S. Census Region.
| Northeast | Midwest | South | West | |||||
|---|---|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | Rural | Urban | Rural | Urban | |
| All Cancers | 476.6b | 482.9 | 447.0b | 462.4 | 449.1b | 440.9 | 415.7b | 419.8 |
| Tobacco- Associated | 208.5b | 201.8 | 204.5 | 203.6 | 215.8b | 194.3 | 175.3b | 170.4 |
| HPV-Associated | 12.3b | 11.5 | 11.9 | 11.8 | 13.7b | 12.7 | 10.9b | 10.5 |
| Prostate | 121.3b | 136.9 | 110.3b | 125.4 | 116.1b | 122.5 | 111.4b | 116.3 |
| Breast (female) | 122.0b | 131.5 | 114.8b | 127.1 | 110.6b | 121.0 | 113.6b | 122.8 |
| Lung and Bronchus | 69.1b | 63.1 | 68.9 | 68.5 | 77.0b | 64.6 | 53.0b | 48.7 |
| Colorectal | 43.2b | 41.8 | 44.6b | 41.9 | 45.5b | 39.7 | 37.7 | 37.4 |
| Urinary Bladder | 27.1b | 24.3 | 22.0b | 21.6 | 18.8 | 18.9 | 20.6b | 18.8 |
| Melanoma | 22.6b | 20.2 | 20.1b | 19.0 | 18.2b | 19.5 | 23.3b | 21.9 |
| Kidney and Renal Pelvis | 16.1 | 16.0 | 17.2 | 16.9 | 17.5b | 16.3 | 14.7 | 14.5 |
| Non-Hodgkin Lymphoma | 20.6b | 21.3 | 19.5 | 19.7 | 17.1 | 18.1 | 17.3b | 18.6 |
| Leukemia | 15.5b | 14.6 | 13.8b | 13.4 | 12.9 | 12.8 | 13.3b | 12.9 |
| Oral Cavity and Pharynx | 11.5b | 11.0 | 11.9b | 11.4 | 13.0b | 11.8 | 11.1b | 10.3 |
| Endometrial | 31.2 | 30.8 | 27.8 | 28.3 | 22.1 | 22.1 | 23.7 | 24.2 |
| Thyroid | 16.1b | 19.6 | 12.4b | 13.6 | 10.7b | 12.2 | 12.2b | 13.7 |
| Pancreas | 12.7b | 13.4 | 11.7b | 13.0 | 12.2 | 12.1 | 11.0b | 11.7 |
| Esophagus | 5.9b | 4.9 | 5.4b | 5.2 | 4.7b | 4.4 | 4.9b | 4.1 |
| Larynx | 4.0b | 3.5 | 4.2b | 3.9 | 5.1b | 3.9 | 2.7b | 2.3 |
| Brain and Other Nervous System | 7.4b | 6.8 | 6.9 | 6.7 | 6.4 | 6.5 | 6.7b | 6.3 |
| Cervix | 7.3 | 7.2 | 7.7b | 7.2 | 9.4b | 8.3 | 7.3 | 7.0 |
Rates are expressed per 100,000 people and age-adjusted to the 2000 US standard population.
The rate ratio indicates that the rural rate is statistically significantly different than the urban rate (p<0.05).
County Poverty Level
Amongst populations where less than 10% live in poverty, colorectal cancer rates were higher in rural populations, but rates for all cancers combined, tobacco-associated, prostate, breast and five other cancers were higher in urban populations (Table 5). In populations where the county poverty rate was 10-19.99%19.99%, the all cancer combined rate was higher in rural populations (447.6 vs. 445.6 per 100,000 respectively). Tobacco-associated, HPV-associated, lung and bronchus, colorectal, and six other cancers were higher in rural areas with between 10-19.99% of the population living below poverty. In populations where 20+% of the population lives in poverty, the all cancer combined rate was higher in urban areas, but the tobacco-associated, HPV-associated, lung and bronchus, colorectal, and five other cancers had higher rates in rural areas.
Table 5. Cancer Incidence Rates by County Level Poverty Rates.
| 0-9.99% Below Poverty | 10-19.99% Below Poverty | 20+% Below Poverty | ||||
|---|---|---|---|---|---|---|
| Rural | Urban | Rural | Urban | Rural | Urban | |
| All Cancers | 441.7b | 463.7 | 447.6b | 445.6 | 445.2b | 448.2 |
| Tobacco- Associated | 183.5b | 188.8 | 203.2b | 191.6 | 214.4b | 200.5 |
| HPV-Associated | 10.2 | 10.4 | 12.3b | 11.9 | 13.5b | 12.7 |
| Prostate | 120.9b | 127.7 | 112.9b | 122.6 | 115.3b | 132.7 |
| Breast (female) | 120.4b | 134.6 | 114.8b | 123.6 | 109.8b | 117.6 |
| Lung and Bronchus | 55.5b | 58.9 | 68.5b | 61.2 | 76.0b | 64.6 |
| Colorectal | 41.7b | 39.2 | 43.1b | 40.0 | 45.8b | 41.9 |
| Urinary Bladder | 23.0 | 23.0 | 22.0b | 20.4 | 18.4b | 17.9 |
| Melanoma | 25.2b | 23.7 | 21.0b | 20.2 | 17.0b | 14.1 |
| Kidney and Renal Pelvis | 15.6 | 15.8 | 16.7b | 15.8 | 17.4b | 17.0 |
| Non-Hodgkin Lymphoma | 18.8b | 20.6 | 18.9 | 19.0 | 16.9b | 18.2 |
| Leukemia | 14.7 | 14.2 | 13.7b | 13.2 | 12.8 | 12.8 |
| Oral Cavity and Pharynx | 10.8 | 10.9 | 12.2b | 11.3 | 12.5b | 11.2 |
| Endometrial | 26.6b | 27.9 | 26.2b | 25.2 | 22.4b | 25.0 |
| Thyroid | 14.0b | 17.8 | 12.5b | 13.8 | 10.6b | 13.0 |
| Pancreas | 11.6b | 12.9 | 11.8b | 12.3 | 12.2b | 13.0 |
| Esophagus | 5.0 | 4.6 | 5.2b | 4.5 | 4.9 | 4.8 |
| Larynx | 3.0 | 2.9 | 4.1b | 3.4 | 5.0b | 4.1 |
| Brain and Central Nervous | 7.0 | 7.1 | 6.9b | 6.5 | 6.3 | 6.0 |
| Cervix | 5.9 | 6.1 | 8.0b | 7.7 | 9.4 | 9.2 |
Rates are expressed per 100,000 people and age-adjusted to the 2000 US standard population.
The rate ratio indicates that the rural rate is statistically significantly different than the urban rate (p<0.05).
Trends
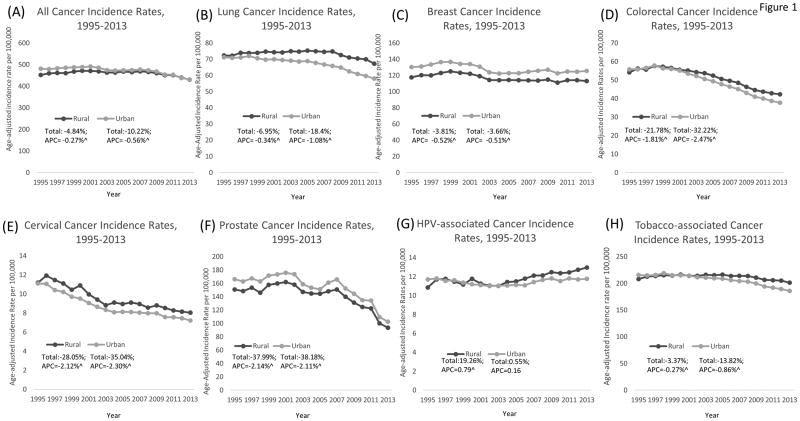
Between 1995 and 2013, the all cancers combined incidence rate decreased for both rural and urban populations (a decrease of 4.84% and 10.22% respectively), with average annual decreases of 0.27% and 0.56% (Figure 1A). Lung cancer incidence rates decreased by 7.0% and 18.4% in rural and urban populations, respectively, corresponding to -0.34% and-1.08% APCs (Figure 1B). Breast cancer rates in rural and urban areas decreased at nearly equal rates, with APCs of -0.52% and -0.51%, respectively (Figure 1C). Colorectal cancer rates decreased 21.78% and 32.22% in rural and urban areas, respectively Figure 1D). Rural and urban populations experienced 28.05% and 35.04% decreases in cervical cancer incidence rates between 1995 and 2013 (Figure 1E). Trends in prostate cancer incidence rates were similar between rural and urban populations; 37.99% and 38.18% decreases, respectively (Figure1F). Rural populations experienced a statistically significant 0.79% APC increase in HPV-associated cancers between 1995 and 2013, while rates remained stable in urban areas (Figure 1G). The decrease in tobacco-associated cancer incidence rates were steeper in urban compared to rural populations, with decreases of 13.8% and 3.4%, respectively (Figure 1H).
Figure 1.
Temporal Trends in Rural and Urban Cancer Incidence, 1995-2013; Rates are per 100,000 and age-adjusted to the 2000 US standard population. “Total” indicates the percent change in incidence between 1995 and 2013, and “APC” indicates the annual percentage change in rates during this interval. ∧ notes an APC that is statistically significantly different than zero (P<0.05).
Figure 1 contains multiple panels displaying the trends, total percent change, and annual percentage change (1995-20130 for eight cancer groups: (A): All cancer; (B): Lung cancer; (C): Breast cancer; (D): Colorectal cancer; (E): Cervical cancer; (F):Prostate cancer; (G): HPV-associated cancer; (H): Tobacco-associated cancer.
Discussion
We evaluated rural-urban differences in cancer incidence rates and trends in the United States. In general, urban populations had higher all sites combined incidence rates regardless of sex or race/ethnic groupings. However, rural populations often had higher rates of tobacco-associated and HPV-associated cancer rates. For individual cancers, rural populations had higher rates of lung and bronchus, colorectal, oral and pharynx, larynx, and cervical cancers than their urban peers, while urban populations had higher rates of breast (female), prostate, and thyroid cancers. For most regions, cancer incidence rates were higher in urban populations, except for the South. Lung and bronchus, colorectal, and oral cavity and pharynx cancers tended to be higher in rural areas across most regions. The rate of all cancers combined was higher in rural populations in areas with 10-19.99% of the population living in poverty. Higher rates of lung and bronchus, colorectal, kidney and renal pelvis, and oral cavity and pharynx cancers were found in rural areas with at least 10% of the population living in poverty compared to urban areas. Rates of lung, breast, and colorectal, cervical, prostate, and tobacco-associated cancers decreased in both rural and urban populations, but the rate of decrease was more pronounced in urban population. The rate of HPV-associated cancers increased in rural population, but remained stable in urban populations.
As many individual cancer rates are higher in rural areas, the higher combined cancer rate in urban areas may be largely driven by higher rates of breast and prostate cancer, the two most common cancers. Of particular note, however, is the dynamic of rural incidence rates and trends relative to mortality rates and trends. We found that incidence rates for all cancers combined are decreasing in rural areas, but other studies have shown that the rural mortality rates are not decreasing at such rates. In 1999, cancer mortality rates for those residing in urban and rural were similar, but by 2014 there was a marked disparity with higher cancer mortality in rural populations (33). Less access to cancer screening and oncology care in rural areas due to poorer spatial access to care, cost burdens, and greater uninsured rates among rural populations may contribute to this incidence/mortality dynamic (34,35). These access barriers may mean that rural residents are diagnosed at a more advanced stage of disease which can affect prognosis and treatment options (36, 37). Social and behavioral factors like higher poverty, greater social isolation, and higher levels of smoking, obesity and physical inactivity may also contribute to poorer cancer outcomes (38,39). Future research should examine this dynamic by assessing rural-urban differences in cancer stage at diagnosis and treatment to elucidate the contributing factors to higher mortality in rural areas despite lower incidence rates.
HPV-associated cancers were significantly higher among NH white rural females and NH black rural males, amongst rural individuals in the Northeast, South and West regions, and among communities where 10% or more of the population lived below the poverty level. These findings complement a recent study that showed elevated oral pharyngeal cancer rates among males and those living in rural areas (40). Further, other studies have shown that STD risk is associated with lower income and that rural males engage in more risky sexual behaviors (41-42). Identifying patterns of HPV-associated cancer is important as there are vaccines for HPV subtypes most commonly associated with cancer (i.e. 16 and 18). A multi-state survey found no rural-urban difference in HPV vaccination initiations overall, but some rural subgroups were less likely than their urban counterparts to initiate vaccination, including girls whose mothers indicated cost as a barrier (43). A statewide analysis of clinic visits among adolescents in Utah found that rural adolescents were less likely to receive a HPV vaccination when receiving other adolescent vaccinations compared to their urban counterparts (44). As HPV-associated cancers are the only cancer type where rates are increasing in rural areas, there is an opportunity to reduce and change the trending trajectory of these rates through HPV vaccination interventions.
We also found a decreasing trend in cervical cancer incidence rates for both rural and urban women, though the decrease was greater in urban. However, incidence rates were higher for rural compared to urban women particularly in the South. Further, incidence rates were higher for both rural NH white and NH black women. These findings are consistent with studies indicating higher rates in rural women, especially among Southern black women (45,46). Rural women are less likely than their urban counterparts to have had a pap smear, which paradoxically may contribute to higher rates in rural areas due to lack of detection at a precancerous stage and may underestimate already high rates due to lack of detection (17,47,48). Our findings of rural-urban and geographic disparities in incidence among both white and black women in the rural South correspond with elevated mortality rates in these populations as well (46, 49, 50).
Our analysis found that tobacco-associated cancers were significantly higher among rural males (NH White and NH Black) and females (NH White and Hispanic), among rural populations in the Northeast, South and West, and among rural populations experiencing greater poverty. The rate of tobacco associated cancers was especially high in the rural South, likely the key contributor to the higher overall cancer incidence rates in rural vs. urban south. A 2006 study indicated that smoking rates in the rural areas of 10 states (including the southern states of Alabama, Georgia, Mississippi, Oklahoma, South Carolina, and Texas) increased between the mid-1990s and the early 2000s, which may latently contribute to higher tobacco associated cancer rates in the rural South (51). Further, while tobacco-associated cancer incidence rates have decreased in both rural and urban populations, the decrease has been more pronounced in urban areas. These findings complement studies consistently indicating higher smoking rates and higher rates of smokeless tobacco in rural areas (10-12,52,53). Doogan and colleagues suggest that rural-urban differences in smoking in past studies were due to demographic or psychosocial differences, while more recent differences may be due to the disproportionately positive effects of tobacco control policies in urban areas (11). There are opportunities to ensure that policies are broadly relevant and enforceable. Further, while our findings mirror differences in smoking prevalence, they also might suggest population groups among whom tobacco cessation interventions might best be implemented and may inform the development for more context-specific (e.g. rural Hispanic females) programs. Our findings also underscore the importance of interventions aimed at preventing smoking initiation in rural adolescents, among whom tobacco use is more pervasive (53,54). In addition to rurally relevant tobacco initiatives, continued efforts could address policies and interventions that promote healthy lifestyles more broadly (13,55,56).
Our results indicated rural-urban differences in lung cancer incidence across most racial/ethnic groups and regions, with these disparities widening in recent years. This corroborate previous studies showing higher rates in rural areas, which may be due in part to higher poverty and smoking rates in rural areas (19). Primary and secondary prevention strategies can help reduce the lung cancer disparity in rural areas. The continued rural disparity for lung cancer specifically provides an opportunity to implement low-dose computed tomography (LDCT) screening to reduce lung cancer mortality in high risk, rural areas. While radiologist capacity for LDCT is a concern in rural areas, efforts to increase knowledge and awareness of LDCT in rural areas like Appalachian Kentucky have shown preliminary success (57,58). Similar campaigns could be implemented in other rural areas to reach high risk populations as implementation of LDCT screening programs continues to expand.
Most rural populations had higher colorectal cancer incidence rates than urban populations across sexes, race/ethnic groups, regions, and poverty levels. Additionally, while colorectal cancer rates have decreased in both rural and urban populations, rates in rural populations have decreased more slowly. The increased incidence in rural areas is consistent with studies indicating lower colorectal cancer screening rates in rural populations, with disparities seen also between rural and urban minorities (59-61). Other studies have shown that high rates of colorectal cancer mortality have clustered in largely rural areas of the United States, like the Lower Mississippi Delta Region and Appalachia (49,62). The confluence of high incidence and mortality and low colorectal cancer screening rates make rural populations important areas for preventive and screening interventions.
While most cancer incidence rates are higher in rural areas, there are a few notable exceptions, namely breast, prostate, and thyroid cancers. These high urban rates persist regardless of race, ethnicity and region. For breast cancer, our findings corroborate previous studies showing higher incidence rates in urban areas, which may be due to increased early detection and utilization of mammography services (63-67). Our findings also corroborate previous studies showing higher rates of prostate cancer in urban areas (63,68,69). Even when stratifying by racial/ethnic groupings (NH whites, NH blacks, or Hispanics), rates were higher in urban populations across all groups. As with breast cancer, elevated incidence of prostate cancer among urban men may be due to higher screening rates and greater availability of healthcare services, especially as the majority of our study period was prior to the 2012 United States Preventive Services Task Force (USPSTF) discontinuation of recommending prostate specific antigen testing (70). Higher rates of thyroid cancer in urban areas is consistent with previous studies (71). Likewise, this may be due to greater access to healthcare services utilization of imaging services among urban residents, especially as previous studies show urban residents have higher and increasing incidence of small tumors that may be indicative of incidentally detected cancers (71). Despite the elevated incidence rates of these cancers in urban areas, studies have either shown no rural-urban differences in mortality or elevated mortality in rural areas. While there continues to be debate regarding over-diagnosis of both breast and thyroid cancers and as the USPSTF recently re-visited prostate cancer screening recommendations, it is important for rural populations to have adequate access and utilization of screening services and cancer treatment to reduce rural mortality disparities.
Strengths and Limitations
Our study is the first, to our knowledge, to comprehensively describe rural-urban differences in cancer incidence across sexes, racial/ethnic groups, regions, and poverty levels and to assess trends. Previous studies were limited to single state cancer registries, multi-registry data sources like SEER, mortality data or only considered one or a few cancer types. Assessing rural-urban differences across demographic and geographic designations and categorizing cancers by associations with carcinogenic agents like tobacco and HPV provides useful information to better understand disparities and inform population-based interventions. Further, our assessment of rural-urban incidence trends will be useful for future research and interventions.
Our study was not without limitation. The only rural-urban metric available in the dataset was a dichotomous rural-urban measure, which limits how we could make comparisons. Analyses that use different measures and/or categorizations of rural-urban status may yield different results. Further, the NAACCR dataset categorized counties into a small number of poverty groupings with the most impoverished grouping being 20+%. However, because poverty is more pervasive in rural areas (e.g. 21.7% of the entire rural South lives below poverty), residual confounding may have occurred when stratifying by only a small number of pre-defined poverty levels (72). The dataset did not include data from 4 states. This may particularly have affected analysis performed by U.S. Census Region, as one state in the Northeast region (Vermont) and South region (Maryland) and two states in the Midwest region (Minnesota and Kansas) were not included. Additionally, a few states were not certified for the entirety of the study period, thus their data were only included for years when they achieved silver or gold certification (73). This year-to-year variability may minimally impact findings, but to fully utilize the robustness of this dataset, we included all registries that were certified for each given year in our analysis.
Conclusions
We found that overall cancer incidence rates were higher in urban areas, but there were some areas where rural populations experience cancer disparity. Cancers associated with modifiable factors (i.e. tobacco and HPV) were higher in rural areas, as were cancers with either new or established screening modalities like lung, cervical, and colorectal cancers. Thus, these cancers, are ready for population-based, clinical, and/or policy strategies and interventions that will reduce risk and ultimately reduce incidence (and mortality). Our findings further underscore the importance of greater research investment in rural cancer control. Additionally, as more geographically precise data become more readily available, more specific analysis could consider cancer incidence differences along a rural-urban gradient, beyond the dichotomous rural-urban designations used in our study and could look more finely at differences across census regions. This will be important for identifying areas and populations who would benefit the most from interventions known to be effective at reducing smoking, increasing HPV vaccination, and increasing access to and utilization of cancer screening tests. Future research should explore differences in cancer stage distribution, receipt of treatment, and survival to help further characterize rural-urban cancer disparities and to subsequently develop population and clinically based strategies and interventions to close gaps in rural-urban cancer outcomes.
Supplementary Material
Acknowledgments
The authors acknowledge the efforts of cancer registrars and state cancer registries in collecting and maintaining the data used in this study. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health, the North American Association of Central Cancer Registries, nor any individual cancer registry
References
- 1.DeSantis CE, Siegel RL, Sauer AG, Miller KD, Fedewa SA, Alcaraz KI, et al. Cancer statistics for African Americans, 2016: Progress and opportunities in reducing racial disparities. CA Cancer J Clin. 2016 doi: 10.3322/caac.21340. [DOI] [PubMed] [Google Scholar]
- 2.Meilleur A, Subramanian SV, Plascak JJ, Fisher JL, Paskett ED, Lamont EB. Rural residence and cancer outcomes in the United States: issues and challenges. Cancer Epidemiol Biomarkers Prev. 2013;22(10):1657–67. doi: 10.1158/1055-9965.epi-13-0404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chow CJ, Al-Refaie WB, Abraham A, Markin A, Zhong W, Rothenberger DA, et al. Does patient rurality predict quality colon cancer care?: A population-based study. Dis Colon Rectum. 2015;58(4):415–22. doi: 10.1097/DCR.0000000000000173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kinney AY, Harrell J, Slattery M, Martin C, Sandler RS. Rural-urban differences in colon cancer risk in blacks and whites: the North Carolina Colon Cancer Study. Journal of Rural Health. 2006;22(2):124–30. doi: 10.1111/j.1748-0361.2006.00020.x. doi:JRH20. [pii] 10.1111/j.1748-0361.2006.00020.x. [DOI] [PubMed] [Google Scholar]
- 5.Singh GK, Williams SD, Siahpush M, Mulhollen A. Socioeconomic, Rural-Urban, and Racial Inequalities in US Cancer Mortality: Part I-All Cancers and Lung Cancer and Part II-Colorectal, Prostate, Breast, and Cervical Cancers. J Cancer Epidemiol. 2011;2011:107497 d. doi: 10.1155/2011/107497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.United States Census Bureau. 2010 Census Urban and Rural Classification and Urban Area Criteria. [Accessed 2017 April 23];2012 Apr 23; https://www.census.gov/geo/reference/ua/urban-rural-2010.html.
- 7.National Center for Health Statistics. Health US, 2015: With, Special Feature on Racial and Ethnic Health Disparities. Hyattsville, MD: 2016. [PubMed] [Google Scholar]
- 8.Foutz JAS, Garfield R. The Role of Medicaid in Rural America. [Avvessed 2017 May 17]; http://kff.org/medicaid/issue-brief/the-role-of-medicaid-in-rural-america/
- 9.Roberts ME, Doogan NJ, Kurti AN, Redner R, Gaalema DE, Stanton CA, et al. Rural tobacco use across the United States: How rural and urban areas differ, broken down by census regions and divisions. Health Place. 2016;39:153–9. doi: 10.1016/j.healthplace.2016.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Doescher MP, Jackson JE, Jerant A, Gary Hart L. Prevalence and trends in smoking: a national rural study. J Rural Health. 2006;22(2):112–8. doi: 10.1111/j.1748-0361.2006.00018.x. [DOI] [PubMed] [Google Scholar]
- 11.Doogan NJ, Roberts ME, Wewers ME, Stanton CA, Keith DR, Gaalema DE, et al. A growing geographic disparity: Rural and urban cigarette smoking trends in the United States. Prev Med. 2017 doi: 10.1016/j.ypmed.2017.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chang JT, Levy DT, Meza R. Trends and Factors Related to Smokeless Tobacco Use in the United States. Nicotine Tob Res. 2016;18(8):1740–8. doi: 10.1093/ntr/ntw090. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Befort CA, Nazir N, Perri MG. Prevalence of obesity among adults from rural and urban areas of the United States: findings from NHANES (2005-2008) J Rural Health. 2012;28(4):392–7. doi: 10.1111/j.1748-0361.2012.00411.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henry KA, Stroup AM, Warner EL, Kepka D. Geographic Factors and Human Papillomavirus (HPV) Vaccination Initiation among Adolescent Girls in the United States. Cancer Epidemiol Biomarkers Prev. 2016;25(2):309–17. doi: 10.1158/1055-9965.epi-15-0658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Martin DN, Lam TK, Brignole K, Ashing KT, Blot WJ, Burhansstipanov L, et al. Recommendations for Cancer Epidemiologic Research in Understudied Populations and Implications for Future Needs. Cancer Epidemiol Biomarkers Prev. 2016;25(4):573–80. doi: 10.1158/1055-9965.EPI-15-1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Blake KD, Moss JL, Gaysynsky A, Srinivasan S, Croyle RT. Making the Case for Investment in Rural Cancer Control: An Analysis of Rural Cancer Incidence, Mortality, and Funding Trends. Cancer Epidemiol Biomarkers Prev. 2017 Jun 9; doi: 10.1158/1055-9965.EPI-17-0092. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wilson RJ, Ryerson AB, Singh SD, King JB. Cancer Incidence in Appalachia, 2004-2011. Cancer Epidemiol Biomarkers Prev. 2016;25(2):250–8. doi: 10.1158/1055-9965.epi-15-0946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Singh GK. Rural-urban trends and patterns in cervical cancer mortality, incidence, stage, and survival in the United States, 1950-2008. J Community Health. 2012;37(1):217–23. doi: 10.1007/s10900-011-9439-6. [DOI] [PubMed] [Google Scholar]
- 19.Atkins GT, Kim T, Munson J. Residence in Rural Areas of the United States and Lung Cancer Mortality. Disease Incidence, Treatment Disparities, and Stage-Specific Survival Ann Am Thorac Soc. 2017;14(3):403–11. doi: 10.1513/AnnalsATS.201606-469OC. [DOI] [PubMed] [Google Scholar]
- 20.Wang Z, Goodman M, Saba N, El-Rayes BF. Incidence and prognosis of gastroesophageal cancer in rural, urban, and metropolitan areas of the United States. Cancer. 2013;119(22):4020–4027. doi: 10.1002/cncr.28313. [DOI] [PubMed] [Google Scholar]
- 21.Coughlin SS, Richards TB, Thompson T, Miller BA, VanEenwyk J, Goodman MT, Sherman RL. Rural/nonrural differences in colorectal cancer incidence in the United States, 1998-2001. Cancer. 2006;107(5 Suppl):1181–1188. doi: 10.1002/cncr.22015. [DOI] [PubMed] [Google Scholar]
- 22.Yao N, Alcala HE, Anderson R, Balkrishnan R. Cancer Disparities in Rural Appalachia: Incidence, Early Detection, and Survivorship. J Rural Health. 2016 Sep 7; doi: 10.1111/jrh.12213. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 23.Lengerich EJ, Tucker TC, Powell RK, Colsher P, Lehman E, Ward AJ, Siedlecki JC, Wyatt SW. Cancer incidence in Kentucky, Pennsylvania, and West Virginia: disparities in Appalachia. J Rural Health. 2005;21(1):39–47. doi: 10.1111/j.1748-0361.2005.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 24.Liang PS, Mayer JD, Wakefield J, Ko CW. Temporal Trends in Geographic and Sociodemographic Disparities in Colorectal Cancer Among Medicare Patients, 1973-2010. J Rural Health. 2016 Aug 31; doi: 10.1111/jrh.12209. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Fitzgerald TL, Lea CS, Brinkley J, Zervos EE. Colorectal cancer outcome inequalities: association between population density, race, and socioeconomic status. Rural Remote Health. 2014;14(3):2668. Epub 2014 Jul 22. [PubMed] [Google Scholar]
- 26.Singh GK, Siahpush M. Widening rural-urban disparities in all-cause mortality and mortality from major causes of death in the USA, 1969-2009. J Urban Health. 2014 Apr 9;91(2):272–92. doi: 10.1007/s11524-013-9847-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.SEER*Stat Database: NAACCR Incidence Data - CiNA Analytic File -, Public Use (which includes data from CDC's National Program of Cancer Registries (NPCR), CCCR's Provincial and Territorial Registries, and the NCI's Surveillance, Epidemiology and End Results (SEER) Registries), certified by the North American Association of Central Cancer Registries (NAACCR) as meeting high-quality incidence data standards for the specified time periods, submitted December 2015.
- 28.North American Association of Central Cancer Registries. [Accessed 9 June 2017];Certification Critieria. Available at https://www.naaccr.org/certification-criteria/
- 29.United States Department of Agriculture. Rural Urban Continuum Codes. [Accessed 17 April 2017]; Available at http://www.ers.usda.gov/data-products/rural-urban-continuum-codes.aspx.
- 30.National Center for Chronic Disease Prevention and Health Promotion Office on Smoking and H. Reports of the Surgeon General. The Health Consequences of Smoking-50 Years of Progress: A Report of the Surgeon General. Atlanta (GA): Centers for Disease Control and Prevention (US); 2014. [Google Scholar]
- 31.Viens LJ, Henley SJ, Watson M, Markowitz LE, Thomas CC, Thompson TD, et al. Human Papillomavirus-Associated Cancers - United States, 2008-2012. MMWR Morb Mortal Wkly Rep. 2016;65(26):661–6. doi: 10.15585/mmwr.mm6526a1. [DOI] [PubMed] [Google Scholar]
- 32.Tiwari RC, Clegg LX, Zou Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15(6):547–69. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 33.Moy E, Garcia MC, Bastian B, Rossen LM, Ingram DD, Faul M, et al. Leading Causes of Death in Nonmetropolitan and Metropolitan Areas- United States, 1999-2014. MMWR Surveill Summ. 2017;66(1):1–8. doi: 10.15585/mmwr.ss6601a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Palmer NR, Geiger AM, Lu L, Case LD, Weaver KE. Impact of rural residence on forgoing healthcare after cancer because of cost. Cancer Epidemiol Biomarkers Prev. 2013;22(10):1668–76. doi: 10.1158/1055-9965.epi-13-0421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sadowski DJ, Geiger SW, Mueller GS, Zahnd WE, Alanee SR, McVary KT. Kidney Cancer in Rural Illinois: Lower Incidence Yet Higher Mortality Rates. Urology. 2016;94:90–5. doi: 10.1016/j.urology.2016.05.022. [DOI] [PubMed] [Google Scholar]
- 36.Williams F, Jeanetta S, James AS. Geographical Location and Stage of Breast Cancer Diagnosis: A Systematic Review of the Literature. J Health Care Poor Underserved. 2016;27(3):1357–83. doi: 10.1353/hpu.2016.0102. [DOI] [PubMed] [Google Scholar]
- 37.Stitzenberg KB, Thomas NE, Dalton K, Brier SE, Ollila DW, Berwick M, et al. Distance to diagnosing provider as a measure of access for patients with melanoma. Arch Dermatol. 2007;143(8):991–998. doi: 10.1001/archderm.143.8.991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Fleisch Marcus A, Illescas AH, Hohl BC, Llanos AA. Relationships between social isolation, neighborhood poverty, and cancer mortality in a population-based study of US adults. PLoS One. 2017;12(3):e0173370. doi: 10.1371/journal.pone.0173370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Meit M, Knudson A, Gilbert T, Tzy-Chyi Yu A, Tanenbaum Eea. The 2014 Update of the Rural-Urban Chartbook. 2014 https://ruralhealth.und.edu/projects/health-reform-policy-research-center/pdf/2014-rural-urban-chartbook-update.pdf.
- 40.Javadi P, Sharma A, Zahnd WE, Jenkins WD. Evolving disparities in the epidemiology of oral cavity and oropharyngeal cancers. Cancer Causes Control. 2017 Jun;28(6):635–645. doi: 10.1007/s10552-017-0889-8. [DOI] [PubMed] [Google Scholar]
- 41.Harling G, Subramanian S, Barnighausen T, Kawachi I. Socioeconomic disparities in sexually transmitted infections among young adults in the United States: examining the interaction between income and race/ethnicity. Sex Transm Dis. 2013;40(7):575–81. doi: 10.1097/OLQ.0b013e31829529cf. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Crosby R, Yarber W, Ding K, DiClemente R. Rural and nonrural adolescents HIV/STD sexual risk, behavior; a comparison from a national sample. Health Education Monograph Series. 2000;18:45–50. [Google Scholar]
- 43.Monnat SM, Rhubart DC, Wallington SF. Differences in Human Papillomavirus Vaccination Among Adolescent Girls in Metropolitan Versus Non-metropolitan Areas: Considering the Moderating Roles of Maternal Socioeconomic Status and Health Care Access. Matern Child Health J. 2016;20(2):315–25. doi: 10.1007/s10995-015-1831-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kepka D, Spigarelli MG, Warner EL, Yoneoka Y, McConnell N, Balch A. Statewide analysis of missed opportunities for human papillomavirus vaccination using vaccine registry data. Papillomavirus Res. 2016;2:128–32. doi: 10.1016/j.pvr.2016.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benard VB, Johnson CJ, Thompson TD, Roland KB, Lai SM, Cokkinides V, et al. Examining the association between socioeconomic status and potential human papillomavirus-associated cancers. Cancer. 2008;113(10 Suppl):2910–8. doi: 10.1002/cncr.23742. [DOI] [PubMed] [Google Scholar]
- 46.Yoo W, Kim S, Huh WK, Dilley S, Coughlin SS, Partridge EE, et al. Recent trends in racial and regional disparities in cervical cancer incidence and mortality in United States. PLoS One. 2017;12(2):e0172548. doi: 10.1371/journal.pone.0172548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bennett KJ, Probst JC, Bellinger JD. Receipt of cancer screening services: surprising results for some rural minorities. J Rural Health. 2012;28(1):63–72. doi: 10.1111/j.1748-0361.2011.00365.x. [DOI] [PubMed] [Google Scholar]
- 48.Horner MJ, Altekruse SF, Zou Z, Wideroff L, Katki HA, Stinchcomb DG. U.S. geographic distribution of prevaccine era cervical cancer screening, incidence, stage, and mortality. Cancer Epidemiol Biomarkers Prev. 2011;20(4):591–9. doi: 10.1158/1055-9965.epi-10-1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zahnd WE, Jenkins WD, Mueller-Luckey GS. Cancer Mortality in the Mississippi Delta Region: Descriptive Epidemiology and Needed Future Research and Interventions. J Health Care Poor Underserved. 2017;28(1):315–28. doi: 10.1353/hpu.2017.0025. [DOI] [PubMed] [Google Scholar]
- 50.Eberhardt MSID, Makuc DM, et al. Health US. Hyattsville, Maryland: National; 2001. 2001. Urban and Rural, Health Chartbook. CfHS. [Google Scholar]
- 51.Doescher MP, Jackson JE, Jerant A, Gary Hart L. Prevalence and trends in smoking: a national rural study. J Rural Health. 2006;22(2):112–118. doi: 10.1111/j.1748-0361.2006.00018.x. [DOI] [PubMed] [Google Scholar]
- 52.Vander Weg MW, Cunningham CL, Howren MB, Cai X. Tobacco use and exposure in rural areas: Findings from the Behavioral Risk Factor Surveillance System. Addict Behav. 2011;36(3):231–6. doi: 10.1016/j.addbeh.2010.11.005. [DOI] [PubMed] [Google Scholar]
- 53.Lutfiyya MN, Shah KK, Johnson M, Bales RW, Cha I, McGrath C, et al. Adolescent daily cigarette smoking: is rural residency a risk factor? Rural Remote Health. 2008;8(1):875. [PubMed] [Google Scholar]
- 54.American Lung Association. Cutting Tobacco's Rural Roots: Tobacco Use in Rural Communities. [Accessed on 2017 May 17]; Available at http://www.lung.org/assets/documents/research/cutting-tobaccos-rural-roots.pdf.
- 55.Cohen SA, Cook SK, Kelley L, Foutz JD, Sando TA. A Closer Look at Rural-Urban Health Disparities: Associations Between Obesity and Rurality Vary by Geospatial and Sociodemographic Factors. J Rural Health. 2016 doi: 10.1111/jrh.12207. [DOI] [PubMed] [Google Scholar]
- 56.Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, et al. Health-Related Behaviors by Urban-Rural County Classification - United States, 2013. MMWR Surveill Summ. 2017;66(5):1–8. doi: 10.15585/mmwr.ss6605a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Smieliauskas F, MacMahon H, Salgia R, Shih YC. Geographic variation in radiologist capacity and widespread implementation of lung cancer CT screening. J Med Screen. 2014;21(4):207–15. doi: 10.1177/0969141314548055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Cardarelli R, Reese D, Roper KL, Cardarelli K, Feltner FJ, Studts JL, et al. Terminate lung cancer (TLC) study-A mixed-methods population approach to increase lung cancer screening awareness and low-dose computed tomography in Eastern Kentucky. Cancer Epidemiol. 2017;46:1–8. doi: 10.1016/j.canep.2016.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Coughlin SS ea. Breast, cervical, and colorectal carcinoma screening in a demographically defined region of the southern U.S. Cancer. 2002;95(10):2211–2222. doi: 10.1002/cncr.10933. [DOI] [PubMed] [Google Scholar]
- 60.Cole AM, Jackson JE, Doescher M. Urban-rural disparities in colorectal cancer screening: cross-sectional analysis of 1998-2005 data from the Centers for Disease Control's Behavioral Risk Factor Surveillance Study. Cancer Med. 2012;1(3):350–6. doi: 10.1002/cam4.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Cole AM, Jackson JE, Doescher M. Colorectal cancer screening disparities for rural minorities in the United States. J Prim Care Community Health. 2013;4(2):106–11. doi: 10.1177/2150131912463244. [DOI] [PubMed] [Google Scholar]
- 62.Siegel RL, Sahar L, Robbins A, Jemal A. Where can colorectal cancer screening interventions have the most impact? Cancer Epidemiol Biomarkers Prev. 2015;24(8):1151–6. doi: 10.1158/1055-9965.EPI-15-0082. [DOI] [PubMed] [Google Scholar]
- 63.Fogleman AJ, Mueller GS, Jenkins WD. Does where you live play an important role in cancer incidence in the U.S.? Am J Cancer Res. 2015;5(7):2314–9. [PMC free article] [PubMed] [Google Scholar]
- 64.Akinyemiju TF, Genkinger JM, Farhat M, Wilson A, Gary-Webb TL, Tehranifar P. Residential environment and breast cancer incidence and mortality: a systematic review and meta-analysis. BMC Cancer. 2015 Mar;15:191. doi: 10.1186/s12885-015-1098-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Onega T, Hubbard R, Hill D, Lee CI, Haas JS, Carlos HA, et al. Geographic access to breast imaging for US women. J Am Coll Radiol. 2014;11(9):874–82. doi: 10.1016/j.jacr.2014.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Doescher MP, Jackson JE. Trends in cervical and breast cancer screening practices among women in rural and urban areas of the United States. J Public Health Manag Pract. 2009;15(3):200–9. doi: 10.1097/PHH.0b013e3181a117da. [DOI] [PubMed] [Google Scholar]
- 67.Leung J, McKenzie S, Martin J, McLaughlin D. Effect of rurality on screening for breast cancer: a systematic review and meta-analysis comparing mammography. Rural Remote Health. 2014;14(2):2730. [PubMed] [Google Scholar]
- 68.Oliver MN, Smith E, Siadaty M, Hauck FR, Pickle LW. Spatial analysis of prostate cancer incidence and race in Virginia, 1990-1999. Am J Prev Med. 2006;30(2 Suppl):S67–76. doi: 10.1016/j.amepre.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 69.Altekruse SF, Huang L, Cucinelli JE, McNeel TS, Wells KM, Oliver MN. Spatial patterns of localized-stage prostate cancer incidence among white and Black men in the southeastern United States, 1999–2001. Cancer Epidemiol Biomarkers Prev. 2010;19(6):1460–7. doi: 10.1158/1055-9965.epi-09-1310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Moyer VA. Screening for prostate cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2012;157(2):120–134. doi: 10.7326/0003-4819-157-2-201207170-00459. [DOI] [PubMed] [Google Scholar]
- 71.Li N, Du XL, Reitzel LR, Xu L, Sturgis EM. Impact of Enhanced Detection on the Increase in Thyroid Cancer Incidence in the United States: Review of Incidence Trends by Socioeconomic Status Within the Surveillance, Epidemiology, and End Results Registry, 1980-2008. Thyroid. 2013;23:103–10. doi: 10.1089/thy.2012.0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.United States Department of Agriculture. Geography of Poverty. [Accessed 11 June 2017]; Available at https://www.ers.usda.gov/topics/rural-economy-population/rural-poverty-well-being/geography-of-poverty.aspx.
- 73.North American Association of Central Cancer Registries. Certified Registries. [Accessed 11 June 2017]; Available at https://www.naaccr.org/certified-registries/#CertificationHistory.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.