Abstract
Introduction
Plasma factor VIII (FVIII) and von Willebrand factor (VWF) levels have been associated with the rate and severity of arterial thrombus formation and have been linked to outcomes following thrombolytic therapy in acute myocardial infarction patients. Here, we aimed to investigate FVIII and VWF levels during the course of thrombolysis in acute ischemic stroke (AIS) patients and to find out whether they predict long-term outcomes.
Materials and methods
Study population included 131 consecutive AIS patients (median age: 69 years, 60.3% men) who underwent i.v. thrombolysis with recombinant tissue plasminogen activator (rt-PA). Blood samples were taken on admission, 1 and 24 h after rt-PA administration to measure FVIII activity and VWF antigen levels. Neurological deficit of patients was determined according to the National Institutes of Health Stroke Scale (NIHSS). ASPECT scores were assessed using computer tomography images taken before and 24 h after thrombolysis. Intracranial hemorrhage was classified according to the European Cooperative Acute Stroke Study (ECASS) II criteria. Long-term functional outcome was determined at 90 days after the event by the modified Rankin scale (mRS).
Results
VWF levels on admission were significantly elevated in case of more severe AIS [median and IQR values: NIHSS <6:189.6% (151.9–233.2%); NIHSS 6–16: 199.6% (176.4–250.8%); NIHSS >16: 247.8% (199.9–353.8%), p = 0.013]; similar, but non-significant trend was observed for FVIII levels. FVIII and VWF levels correlated well on admission (r = 0.748, p < 0.001) but no significant correlation was found immediately after thrombolysis (r = 0.093, p = 0.299), most probably due to plasmin-mediated FVIII degradation. VWF levels at all investigated occasions and FVIII activity before and 24 h after thrombolysis were associated with worse 24 h post-lysis ASPECT scores. In a binary backward logistic regression analysis including age, gender, high-sensitivity C-reactive protein, active smoking, diabetes, and NIHSS >5 on admission, elevated FVIII and VWF levels after thrombolysis were independently associated with poor functional outcomes (mRS ≥ 3) at 90 days (immediately after thrombolysis: FVIII: OR: 7.10, 95% CI: 1.77–28.38, p = 0.006, VWF: OR: 6.31, 95% CI: 1.83–21.73, p = 0.003; 24 h after thrombolysis: FVIII: OR: 4.67, 95% CI: 1.42–15.38, p = 0.011, VWF: OR: 19.02, 95% CI: 1.94–186.99, p = 0.012).
Conclusion
Elevated FVIII activity and VWF antigen levels immediately after lysis and at 24 h post-therapy were shown to have independent prognostic values regarding poor functional outcomes at 90 days.
Keywords: acute ischemic stroke, intracerebral hemorrhage, factor VIII, therapy outcome, thrombolysis, von Willebrand factor
Introduction
Stroke is the second leading cause of death worldwide and the most common cause of disability (1). Currently, intravenous administration of recombinant tissue plasminogen activator (rt-PA), initiated within 4.5 h after symptom onset, is the standard therapy for the treatment of acute ischemic stroke (AIS). Although thrombolysis using rt-PA treatment has been proven to be safe and effective by a number of clinical trials and systematic reviews (2, 3), only approximately half of treated patients achieve functional independence with complete or nearly complete neurological recovery at 3 months (4). Of all thrombolysis-related complications, the most feared is symptomatic intracerebral hemorrhage, which occurs in approximately 7% of patients causing significant morbidity and mortality (5, 6). Several factors have been associated with a potentially increased risk of poor outcome after rt-PA treatment (e.g., advanced age, male gender, stroke severity, diabetes, baseline hyperglycemia, etc.) (5), still, clinical outcomes are not easily foreseen at the initiation of the therapy as most of the current clinical–radiological risk scores are non-specific and have modest predictive value (6). In order to improve patient care in the near future, new risk prediction models incorporating the use of specific biomarkers might be helpful. A potentially useful biomarker in this case is expected to be involved in the underlying pathophysiological pathway and must confer significant predictive value regarding therapy outcomes.
A growing body of research has demonstrated a role for coagulation factor VIII (FVIII) and von Willebrand factor (VWF) in the pathophysiology of AIS (7, 8). FVIII is stabilized in the circulation by VWF: the linear relationship between the levels of FVIII and VWF has been described (9). The FVIII–VWF complex plays an important role in the propagation of thrombus formation as it mediates platelet attachment to the damaged subendothelium and supports the activation of coagulation cascade at the site of the growing thrombus (7). Plasma FVIII/VWF levels have been directly linked to the rate and severity of arterial thrombus formation (10). Elevated levels of FVIII/VWF have been associated with the risk of stroke (8, 11, 12); however, less evidence is available on the prognostic value of both markers in stroke outcomes (12, 13). Only few papers, including relatively small cohort of patients describe a potential relationship between FVIII and/or VWF levels and thrombolysis outcomes (14). Elevated levels of VWF during thrombolysis in acute myocardial infarction (AMI) patients have been associated with poor recanalization and worse outcomes (15). Less is known about the levels of FVIII and VWF during the course of thrombolysis in AIS patients—even though it has been speculated based on animal studies that the degradation of FVIII during thrombolysis treatment could be a potential causative factor for bleeding complications occurring in treated patients (16).
In the past decades, inhibition of the action of VWF has become an attractive new antithrombotic strategy in ischemic stroke management (7, 17). When used in combination with rt-PA, VWF antagonists could promote the rapid dissolution of the occluding thrombus and limit subsequent thrombo-inflammatory ischemia/reperfusion injury (17). As most of these studies were performed in animal models, data regarding the changes of VWF/FVIII levels during thrombolysis in humans could be of particular interest.
Here, we hypothesized that levels of FVIII and VWF are related to stroke severity and/or patient outcome following thrombolysis treatment. In this observational study, we investigated the levels of FVIII and VWF in a cohort of consecutive AIS patients using blood samples taken on three occasions during the course of i.v. thrombolysis and assessed the potential prognostic value of the measured parameters on functional outcomes at 90 days post-event.
Materials and Methods
Patients
Consecutive AIS patients aged 18 years or more, eligible for thrombolysis, admitted to a single Stroke Center (Department of Neurology, Faculty of Medicine, University of Debrecen, Hungary) were enrolled in the study. All patients were within 4.5 h of their symptom onset at the time of admission. Patient enrollment lasted for 22 months starting in March 2011. Intravenous thrombolytic therapy was applied according to the European Stroke Organization (ESO) guidelines using rt-PA (Alteplase, Boehringer Ingelheim, Germany) (18). Inclusion and exclusion criteria of patients were identical to that of thrombolysis eligibility as described in the ESO 2008 guideline (18). The diagnosis of IS was based on clinical symptoms and brain imaging using computer tomography (CT) scan and CT angiography (CTA). Admission CTA was used to identify the level of vessel occlusion in every patient. A control CT was performed for every patient 24 h after thrombolysis. All CT images were analyzed by four different investigators blinded to the clinical state of the patients and the Alberta Stroke Program Early CT Scores (ASPECTS) were calculated (19). Neurological deficit of patients was determined by the NIHSS (20) at various time points: on admission and at 2 h, 24 h, and 7 days post-lysis. Stroke etiology was determined according to the Trial of ORG 10172 in Acute Stroke Treatment (TOAST) criteria (21). Hemorrhagic events were classified as symptomatic or asymptomatic intracranial hemorrhage (SICH or aSICH, respectively) according to the European Cooperative Acute Stroke Study (ECASS) II criteria (22). For each patient a detailed list of clinical parameters was recorded including demographic characteristics, neurological status, time of symptom onset, cardiovascular risk factors (arterial hypertension, atrial fibrillation, hyperlipidemia, diabetes mellitus, smoking status), history of previous cardiovascular events, and medications. Patients were followed and long-term functional outcomes were determined at 90 days post-event using the modified Rankin Scale (mRS) (23).
The following outcomes were investigated: (1) short-term functional outcome at 7 days post-event: favorable outcome was defined as a decrease in NIHSS score by at least 4 points or to 0 by day 7, unfavorable outcome was defined as an increase in NIHSS score by at least 4 points by day 7. (2) The presence of therapy-associated SICH or aSICH was defined according to ECASS II criteria. (3) Long-term functional outcome at 90 days post-event: poor long-term outcome was specified as an mRS greater than 2.
The study was approved by the Ethics Committee of the University of Debrecen, Hungary. All patients or their relatives provided written informed consent.
Blood Sampling and Laboratory Measurements
Peripheral blood samples were drawn from patients into vacutainer tubes on three different occasions: upon hospital admission (before thrombolysis), immediately after the administration of rt-PA infusion (~1 h after the initiation of thrombolysis) and approximately 24 h after the administration of thrombolytic therapy. Routine laboratory tests were performed from blood samples taken before thrombolysis and included the measurements of complete blood count, serum ions, glucose levels, basic kidney function tests, liver function test, high-sensitivity C-reactive protein (hsCRP), and screening tests of coagulation (prothrombin time, activated partial thromboplastin time and thrombin time). Blood samples anticoagulated with sodium citrate, theophylline, adenosine and dipyridamole (Vacuette CTAD Tubes, Greiner Bio-One, Austria) were centrifuged at 1,220 g, room temperature for 15 min. Plasma aliquots were labeled with a code and stored at −70°C until further analysis of FVIII activity and VWF antigen levels. FVIII activity, determined by chromogenic method and VWF antigen level, determined by immunoturbidimetric assay were measured from coded plasma samples on a BCS coagulometer by standard methods (Siemens Healthcare Diagnostic Products, Marburg, Germany), by an investigator blinded to patient identification and clinical information. Batches of plasma samples (approximately 20 samples) were thawed for 10 min at 37°C followed by immediate analysis. According to the manufacturer, precision of the assays are the following: coefficient of variation within run (intra-assay precision) for FVIII activity assay: 4–9%, for VWF antigen level test: 1.4–4.2%; between run (inter-assay precision) for FVIII activity assay: 4–10%, for VWF antigen level test: 0.9–2.6%.
Statistical Analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (SPSS, Release 22.0, Chicago, IL, USA) and GraphPad Prism 5.0 (GraphPad Prism Inc., La Jolla, CA, USA) softwares. Normality of the data was evaluated by the Shapiro–Wilk test. As FVIII activity and VWF antigen levels were not normally distributed at any time points measured, the Mann–Whitney U test was applied for all two-group analyses and the Kruskal–Wallis analysis with Dunn–Bonferroni post hoc test was used for multiple comparisons. Differences between categorical variables were assessed by the Fisher’s exact or χ2 test. Friedman’s two-way ANOVA with Dunn–Bonferroni post hoc test was applied to investigate the effect of thrombolysis on FVIII activity and VWF levels. Strength of association between FVIII activity and VWF antigen levels was tested using Spearman’s correlation test. In order to test for differences between adjusted means, univariate analysis incorporating covariate testing (one-way ANCOVA) was performed after logarithmic transformation of data. Positive predictive values (PPVs) and negative predictive values (NPVs) of the studied parameters were assessed using contingency tables and the Fisher’s exact test. A binary backward logistic regression model was used to determine whether elevated FVIII and VWF levels of different time points are independent predictors of poor functional outcomes at 90 days post-event. Adjustment of the models were based on the results of previous statistical analyses (Mann–Whitney U test, Fisher’s exact, or χ2 test), previous literature and methodological principles (dichotomized variables wherever possible). Results of the logistic regression analysis were expressed as odds ratio (OR) and 95% confidence interval (CI). A p-value of <0.05 was considered statistically significant.
Results
Study Population
During the study period, 131 consecutive AIS patients receiving intravenous rt-PA treatment were enrolled. Baseline demographic variables, main stroke characteristics and details of thrombolysis treatment are listed in Tables 1 and 2. In case of six patients, intravenous thrombolytic therapy was supplemented with intra-arterial thrombolysis using rt-PA according to standard protocol; the duration of thrombolysis and the final dose of rt-PA applied did not significantly differ for these patients. Median age of the patient cohort was 69 (IQR: 59–79) years, 60.3% were men. The most common cerebrovascular risk factor was arterial hypertension in this patient cohort (n = 100, 76.3%). Median time from symptom onset to treatment was 155 (IQR: 125–180) min. Median NIHSS before stroke treatment was 8 (IQR: 5–14). According to the TOAST criteria, etiology of stroke was most commonly large vessel disease (n = 49, 37.4%), followed by 27 (20.6%) patients with cardioembolic stroke. As detected by CTA on admission, 70 patients (53.4%) had a vessel occlusion, and 27 patients (20.6%) stenosis. Poor functional outcome at 7 days post-event was observed in 20 cases (15.3%), while poor outcome at 90 days (mRS ≥ 3) was observed in case of 51 (38.9%) patients. Therapy-associated intracranial hemorrhage was detected in 13 cases, of which 6 cases (4.6%) were symptomatic according to ECASS II. Mortality rates by day 7, 14, and day 90 post-event were 3.8, 6.1, and 22.1%, respectively.
Table 1.
Study population.
| Variable | |
|---|---|
| Patients, n | 131 |
| Age, median (IQR) | 69.0 (59.0–79.0) |
| Male, n (%) | 79 (60.3) |
| Cerebrovascular risk factors, n (%) | |
| Arterial hypertension | 100 (76.3) |
| Atrial fibrillation | 35 (26.7) |
| Hyperlipidemia | 81 (61.8) |
| Diabetes mellitus | 39 (29.8) |
| Smoking | |
| Non-smoker | 69 (52.7) |
| Previous smoker | 16 (12.2) |
| Current smoker | 31 (23.7) |
| Undetermined | 15 (11.5) |
| Previous stroke or TIA, n (%) | 42 (32.1) |
| Thrombolysis treatment, median (IQR) | |
| Time from symptom onset to treatment (min) | 155 (125.0–180.0) |
| Duration of thrombolysis (min) | 60 (60.0–65.0) |
| rt-PA dose (mg) | 67.0 (58.0–80.8) |
| Medication at enrollment, n (%) | |
| Antihypertensive therapy | 93 (71.0) |
| Angiotensin-converting enzyme inhibitor | 60 (45.8) |
| Alpha blocker | 7 (5.3) |
| Beta blocker | 56 (42.8) |
| Calcium channel blocker | 30 (22.9) |
| Diuretics | 39 (29.8) |
| Antiplatelet druga | 58 (44.3) |
| Anticoagulant drug | 7 (5.3) |
| Lipid lowering therapy | 38 (29.0) |
| Antidiabetic therapyb | 16 (12.2) |
| Laboratory measurements, median (IQR) | |
| INR | 0.98 (0.94–1.03) |
| APTT (s) | 28.5 (26.1–32.1) |
| WBC (G/L) | 7.59 (6.12–9.0) |
| Platelets (G/L) | 207.5 (169.0–254.3) |
| Serum glucose (mmol/L) | 6.5 (5.5–7.9) |
| hsCRP (mg/L) | 3.06 (1.7–5.9) |
| Creatinine (μmol/L) | 78.0 (64.0–97.0) |
IQR, interquartile range; TIA, transient ischemic attack; rt-PA, recombinant tissue plasminogen activator; INR, international normalized ratio; APTT, activated partial thromboplastin time; WBC, white blood cell; hsCRP, high sensitivity CRP.
aAspirin or P2Y12 inhibitor treatment or both.
bInsulin therapy or oral antidiabetic drug therapy.
Table 2.
Stroke characteristics.
| Variable | |
|---|---|
| Stroke severity on admission, n (%) | |
| NIHSS 0–5 | 36 (27.5) |
| NIHSS 6–10 | 46 (35.1) |
| NIHSS 11–16 | 29 (22.1) |
| NIHSS >16 | 17 (13.0) |
| Undetermined | 3 (2.3) |
| Stroke etiology (TOAST), n (%) | |
| Large artery atherosclerosis | 49 (37.4) |
| Small vessel occlusion | 13 (9.9) |
| Cardioembolic | 27 (20.6) |
| Other/undetermined | 42 (32.1) |
| Imaging data | |
| ASPECTS, median (IQR) | |
| On admission | 10 (9–10) |
| 24 h after thrombolysis | 9 (5–10) |
| Affected vessel territory, n (%) | |
| MCA | 82 (62.6) |
| ICA | 11 (8.4) |
| MCA + ICA | 10 (7.6) |
| VB | 28 (21.4) |
| Level of occlusion, n (%) | |
| No stenosis/occlusion | 34 (26.0) |
| Stenosis | 27 (20.6) |
| Occlusion | 70 (53.4) |
| Outcomes, n (%) | |
| Functional outcome at 7 days | |
| Favorable outcome | 49 (37.4) |
| No change | 42 (32.1) |
| Unfavorable outcome | 20 (15.3) |
| Functional outcome at 90 days | |
| mRS 0–2 | 57 (43.5) |
| mRS 3–6 | 51 (38.9) |
| Undetermined | 23 (17.6) |
| Intracranial hemorrhage (ECASS II) | |
| aSICH | 7 (5.3) |
| SICH | 6 (4.6) |
n, number of patients; IQR, interquartile range, NIHSS, National Institutes of Health Stroke Scale; TOAST, Trial of ORG 10172 in Acute Stroke Treatment; ASPECTS, Alberta Stroke Program Early Computed Tomography Score; MCA, middle cerebral artery; ICA, internal carotid artery; VB, vertebrobasilar territory; mRS, modified Rankin Scale; ECASS II, European Cooperative Acute Stroke Study II; aSICH, asymptomatic intracerebral hemorrhage; SICH, symptomatic intracerebral hemorrhage.
The Effect of Thrombolysis on FVIII Activity and VWF Antigen Levels
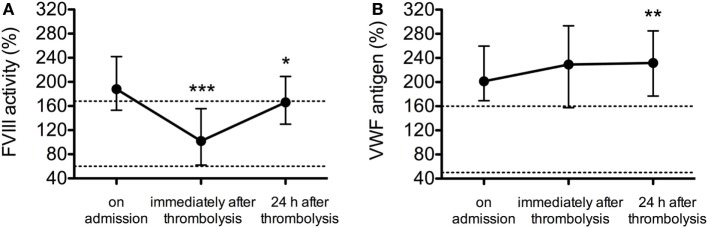
The median and IQR values of FVIII activity and VWF antigen levels are shown at all investigated time points in Figures 1A,B, respectively. In the samples taken on admission, the median values of both hemostasis parameters were above the upper limit of the respective reference interval in the whole patient cohort (FVIII activity median: 188.0%, IQR: 153.0–242.0%, VWF antigen level median: 201.3%, IQR: 169.1–259.6%). FVIII activity dropped significantly in the samples obtained immediately after thrombolysis as compared to the initial values (median: 102.0%, IQR: 62.0–155.5%, p < 0.001) and showed an increase 24 h after the event (median: 166%, IQR: 130.0–209.0%, p = 0.014) (Figure 1A). On the contrary, VWF levels increased steadily post-lysis (median VWF levels immediately after lysis: 229.1%, IQR: 157.6–293.3%, at 24 h post-lysis: 231.6%, IQR: 176.8–284.8%, Friedman’s two-way ANOVA p = 0.002). Notably, VWF median and IQR values were above the upper limit of the reference interval at all investigated time points in the study cohort (Figure 1B).
Figure 1.
The effect of thrombolytic therapy on factor VIII (FVIII) activity (A) and von Willebrand factor (VWF) antigen levels (B). Results are expressed as median values and interquartile ranges (whiskers) as measured from samples taken on admission, immediately after thrombolysis and 24 h after thrombolysis. Upper and lower limits of respective reference intervals are indicated with dashed lines (FVIII activity: 60–168%, VWF antigen levels: 50–160%). Statistical significance was assessed using Friedman’s two-way ANOVA with Dunn–Bonferroni post hoc test. *p < 0.05, **p < 0.01, ***p < 0.001 as compared to values on admission.
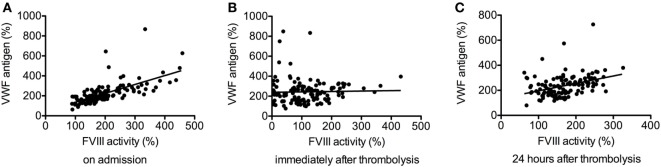
Factor VIII activity and VWF antigen levels showed good correlation on admission (r = 0.748, p < 0.001) (Figure 2A), but no significant correlation was found immediately after thrombolysis (r = 0.093, p = 0.299, Figure 2B), most probably due to plasmin-mediated FVIII degradation. Fair correlation was observed between the two parameters in the samples obtained 24 h after thrombolysis (r = 0.420, p < 0.001, Figure 2C).
Figure 2.
Correlation between factor VIII (FVIII) activity and von Willebrand factor (VWF) antigen levels before thrombolysis (r = 0.748, p < 0.001) (A), immediately after thrombolysis (r = 0.093, p = 0.299) (B), and 24 h after thrombolysis (r = 0.420, p < 0.001) (C).
The Association of FVIII Activity and VWF Antigen Levels with Stroke Severity
von Willebrand factor antigen levels were gradually and significantly elevated in case of more severe AIS (NIHSS 6–16 and NIHSS >16) at all investigated time points, but no such significant association was observed for FVIII activity levels (Table 3). The association between VWF antigen levels and stroke severity remained significant after adjustments for confounders (current smoking, hsCRP, age) in the statistical model.
Table 3.
FVIII activity and VWF antigen levels according to stroke severity on admission.
| Stroke severity on admission | |||||
|---|---|---|---|---|---|
| NIHSS 0–5 (n = 36) | NIHSS 6–16 (n = 75) | NIHSS > 16 (n = 17) | p-Value | p-Value* | |
| FVIII activity (%) | |||||
| On admission | 175.5 (145.0–209.3) | 186.0 (155.0–238.0) | 212.0 (165.5–352.0) | 0.162 | 0.046 |
| Immediately after thrombolysis | 108.0 (47.0–148.0) | 92.0 (70.0–152.0) | 114.0 (51.5–201.0) | 0.571 | 0.400 |
| 24 h after thrombolysis | 159.0 (115.5–188.5) | 162.0 (134.0–208.0) | 172.0 (134.0–234.0) | 0.292 | 0.163 |
| VWF antigen (%) | |||||
| On admission | 189.6 (151.9–233.2) | 199.6 (176.4–250.8) | 247.8 (199.9–353.8) | 0.013 | 0.013 |
| Immediately after thrombolysis | 172.2 (141.2–257.0) | 229.2 (166.6–293.6) | 276.8 (219.1–375.5) | 0.008 | 0.011 |
| 24 h after thrombolysis | 181.4 (156.9–246.8) | 235.9 (188.3–292.7) | 261.7 (192.4–366.8) | 0.003 | 0.001 |
NIHSS, National Institutes of Health Stroke Scale; FVIII, factor VIII; VWF, von Willebrand factor.
Data are presented as median and interquartile range. Stroke severity of patients was classified according to previous literature (24, 25). p-Value: statistical significance assessed using the Kruskal–Wallis test. p-Value*: statistical significance assessed after adjustments for covariates (active smoking, hsCRP, age) in the statistical model (ANCOVA after logarithmic transformation of variables).
The association of elevated VWF levels and more severe AIS was also proved as significantly higher VWF levels were found at all investigated time points in patients presenting with worse 24 h post-lysis CT scans (ASPECTS score 7–0) (Table 4). Similar association was observed for FVIII levels, except for the samples investigated immediately after lysis. Associations for VWF levels and FVIII activity remained significant after adjustments for confounders (current smoking, hsCRP, age) in the statistical model (Table 4). As CT scans on admission are not indicative of stroke severity and have less predictive values as the ASPECTS at 24 h post-lysis, it was not surprising that no significant association was found between the investigated hemostasis parameters and the ASPECTS on admission (Table 4). No association was found between FVIII activity and VWF antigen levels at any time points and stroke subtypes according to TOAST criteria (data not shown). FVIII activity at 24 h post-lysis was significantly elevated in patients with vessel occlusion (median: 175.0%, IQR: 151.5–227.0%) as compared to those with stenosis only (median: 137.0%, IQR: 98.5–175.0%) or without occlusion/stenosis (median: 142.0%, IQR: 115.0–177.0%) (p = 0.001) (Table S1 in Supplementary Material), while such association was not observed for VWF levels.
Table 4.
FVIII activity and VWF antigen levels according to ASPECTS on admission and at 24 h after thrombolysis.
| ASPECTS on admission |
ASPECTS 24 h after thrombolysis |
|||||||
|---|---|---|---|---|---|---|---|---|
| 10 (n = 59) | 9–0 (n = 34) | p-Value | p-Value* | 10–8 (n = 55) | 7–0 (n = 38) | p-Value | p-Value* | |
| FVIII activity (%) | ||||||||
| On admission | 171.0 (139.0–206.0) | 188.0 (168.5–262.3) | 0.072 | 0.046 | 171.0 (135.0–192.0) | 194.0 (168.0–299.5) | 0.002 | 0.001 |
| Immediately after thrombolysis | 90.0 (38.8–147.3) | 125.0 (79.0–165.0) | 0.056 | 0.041 | 92.0 (55.5–147.5) | 114.0 (66.0–177.0) | 0.141 | 0.256 |
| 24 h after thrombolysis | 166.0 (135.0–198.0) | 178.0 (134.0–234.0) | 0.290 | 0.171 | 156.0 (121.0–182.0) | 198.0 (158.0–246.0) | 0.001 | <0.001 |
| VWF antigen (%) | ||||||||
| On admission | 193.1 (161.6–246.2) | 199.4 (173.4–257.1) | 0.236 | 0.182 | 191.5 (161.6–231.7) | 223.2 (175.1–268.6) | 0.012 | 0.018 |
| Immediately after thrombolysis | 224.7 (152.9–284.4) | 224.5 (171.7–295.9) | 0.505 | 0.270 | 199.2 (146.3–261.8) | 255.2 (200.6–326.3) | 0.004 | 0.002 |
| 24 h after thrombolysis | 225.5 (180.0–295.9) | 242.8 (180.8–270.2) | 0.816 | 0.783 | 197.8 (174.2–259.6) | 257.4 (205.1–320.1) | 0.003 | 0.017 |
ASPECTS, Alberta Stroke Program Early Computed Tomography Score; FVIII, factor VIII; VWF, von Willebrand factor.
Data are presented as median and interquartile range. Patients on admission were dichotomized as having none (ASPECTS = 10) vs. any (ASPECTS = 9–0) early ischemic signs, while patients at 24 h after thrombolysis were dichotomized as having mild/none (ASPECTS 10–8) vs. moderate/severe (ASPECTS 7–0) ischemic signs according to previous literature (26, 27). p-Value: statistical significance assessed using the Mann–Whitney U test. p-Value*: statistical significance assessed after adjustments for covariates (active smoking, hsCRP, age) in the statistical model (ANCOVA after logarithmic transformation of variables).
Elevated FVIII Activity and VWF Antigen Levels As Predictors of Thrombolysis Outcomes
Factor VIII activity and VWF antigen levels were not associated at any investigated time points with short-term therapy outcomes as assessed by the changes in NIHSS score by day 7 post-lysis (data not shown).
No association was found between FVIII activity or VWF antigen levels at any investigated time points and therapy-associated ICH, except for higher VWF at 24 h post-lysis in patients presenting with SICH (median: 226.8%, IQR: 176.5–279.4% vs. median: 347.5%, IQR: 263.3–372.1% for no bleeding or aSICH vs. SICH, p = 0.017) (Figure S1 in Supplementary Material).
Poor functional outcome (mRS ≥3) at 90 days post-event was associated with traditional risk factors including advanced age, increased NIHSS on admission, elevated hsCRP, and the presence of diabetes/diabetes treatment (Table 5). Moreover, as expected, ASPECTS at 24 h post-lysis and the level of vessel occlusion as detected by CTA was also indicative of the long-term outcome. Among the hemostasis parameters investigated at various time points, elevated FVIII activity 24 h post-lysis and elevated VWF antigen level measured immediately after lysis and 24 h after therapy showed significant association with poor outcomes (Table 5). Both parameters, as measured immediately post-lysis and 24 h post-lysis conferred a significant PPV and NPV for poor functional outcomes (highest PPV: VWF 24 after thrombolysis: 0.83; 95% CI: 0.59–0.96, p = 0.009 and highest NPV: FVIII immediately after thrombolysis: 0.73; 95% CI: 0.50–0.89, p = 0.009).
Table 5.
Characteristics of patients according to functional outcomes at 90 days following thrombolysis.
| Variables | mRS 0–2 (n = 57) | mRS 3–6 (n = 51) | p-Value |
|---|---|---|---|
| Age, median (IQR) | 67.0 (58.0–76.0) | 76.0 (62.0–83.0) | 0.011 |
| Male, n (%) | 39 (68.4) | 27 (52.9) | 0.116 |
| Cerebrovascular risk factors, n (%) | |||
| Arterial hypertension | 44 (77.2) | 39 (76.5) | 1.000 |
| Atrial fibrillation | 16 (28.1) | 14 (27.5) | 1.000 |
| Hyperlipidemia | 39 (68.4) | 26 (51.0) | 0.078 |
| Diabetes mellitus | 12 (21.1) | 20 (39.2) | 0.057 |
| Previous stroke | 21 (36.8) | 14 (28.5) | 0.412 |
| Current smoker | 12 (21.1) | 13 (25.5) | 0.817 |
| Stroke etiology, n (%) | |||
| Small vessel disease | 8 (14.0) | 3 (5.9) | |
| Large vessel disease | 17 (29.8) | 21 (41.2) | 0.238 |
| Cardioembolic | 13 (22.8) | 10 (19.6) | |
| NIHSS on admission, median (IQR) | 6 (4–9) | 14 (8–19) | <0.001 |
| Imaging data | |||
| ASPECTS, median (IQR) | |||
| on admission | 10 (9–10) | 10 (9–10) | 0.482 |
| 24 h after thrombolysis | 9 (8–10) | 7 (2–9) | 0.001 |
| Affected vessel territory, n (%) | |||
| MCA | 33 (57.9) | 33 (64.7) | |
| ICA | 4 (7.0) | 3 (5.9) | 0.093 |
| MCA + ICA | 2 (3.5) | 7 (13.7) | |
| VB | 18 (31.6) | 8 (15.7) | |
| Level of occlusion, n (%) | |||
| No stenosis/occlusion | 22 (38.6) | 7 (13.7) | |
| Stenosis | 13 (22.8) | 9 (17.6) | 0.004 |
| Occlusion | 22 (38.6) | 35 (68.6) | |
| Current drug use, n (%) | |||
| Antihypertensive therapy | 43 (75.4) | 36 (70.6) | 0.821 |
| Antiplatelet druga | 26 (45.6) | 25 (49.0) | 0.846 |
| Anticoagulant drug | 2 (3.5) | 4 (7.8) | 0.425 |
| Lipid lowering therapy | 17 (29.8) | 15 (29.4) | 1.000 |
| Antidiabetic therapyb | 3 (5.3) | 10 (19.61) | 0.037 |
| Laboratory measurements, median (IQR) | |||
| INR | 0.97 (0.94–1.02) | 0.99 (0.96–1.06) | 0.082 |
| APTT (s) | 27.9 (25.9–31.2) | 28.6 (26.8–32.2) | 0.117 |
| WBC (G/L) | 7.56 (6.21–8.87) | 7.1 (6.06–9.03) | 0.545 |
| Platelets (G/L) | 209.0 (179.5–240.7) | 198.0 (162.0–261.0) | 0.562 |
| Serum glucose (mmol/L) | 6.5 (5.45–7.40) | 6.5 (5.5–8.03) | 0.737 |
| hsCRP (mg/L) | 2.34 (1.02–4.12) | 4.72 (1.80–10.11) | 0.002 |
| Creatinine (μmol/L) | 77.0 (65.0–90.5) | 81.0 (61.0–101.0) | 0.735 |
| FVIII activity (%), median (IQR) | |||
| On admission | 175.0 (142.0–218.5) | 191.0 (161.0–274.0) | 0.092 |
| Immediately after thrombolysis | 88.0 (44.5–149.0) | 110.0 (66.0–185.0) | 0.102 |
| 24 h after thrombolysis | 153.0 (120.5–174.0) | 176.0 (134.0–237.0) | 0.018 |
| VWF antigen (%), median (IQR) | |||
| On admission | 193.1 (162.1–255.2) | 214.0 (176.8–262.2) | 0.092 |
| Immediately after thrombolysis | 204.1 (141.8–265.8) | 254.8 (176.8–323.2) | 0.011 |
| 24 h after thrombolysis | 212.5 (160.0–251.6) | 259.2 (191.0–315.1) | 0.002 |
mRS, modified Rankin Scale; IQR, interquartile range; NIHSS, National Institutes of Health Stroke Scale; ASPECTS, Alberta Stroke Program Early Computed Tomography Score; MCA, middle cerebral artery; ICA, internal carotid artery; VB, vertebrobasilar territory; INR, international normalized ratio; APTT, activated partial thromboplastin time; WBC, white blood cell; hsCRP, high sensitivity CRP; FVIII, factor VIII; VWF, von Willebrand factor.
aAspirin or P2Y12 inhibitor treatment or both.
bInsulin therapy or oral antidiabetic drug therapy.
A binary backward logistic regression model including age, gender, elevated hsCRP, active smoking, diabetes mellitus, and NIHSS >5 on admission revealed that a FVIII activity and VWF antigen level above the upper limit of the reference interval (168 and 160%, respectively) as measured immediately after lysis and 24 h after thrombolysis significantly and independently increase the risk of unfavorable functional outcomes at 90 days (Table 6). In this model, FVIII activity and VWF antigen levels on admission did not prove to have an independent prognostic value regarding poor functional outcomes at 90 days, while elevated FVIII and VWF levels immediately after thrombolysis conferred an independent OR: 7.09 (IQR: 1.77–28.38, p = 0.006) and OR: 6.31 (IQR: 1.83–21.7, p = 0.003), respectively. Elevated levels of both factors 24 h after lysis were also found to have a significant predictive value (OR: 4.67, IQR: 1.42–15.38, p = 0.011 for FVIII activity and OR: 19.02, IQR: 1.39–187.0, p = 0.012 for VWF antigen level). Besides these hemostasis parameters, only hsCRP >5.2 mg/L and NIHSS >5 on admission remained in the stepwise backwards regression analysis model as independent risk factors for poor outcomes at 90 days (OR: 4.85, 95% CI: 1.64–14.33, p = 0.004 and OR: 3.51, 95% CI: 1.17–10.57, p = 0.026, respectively).
Table 6.
Association of FVIII activity and VWF antigen levels with poor functional outcome (mRS ≥ 3) at 90 days.
| Odds ratio | 95% confidence interval | p-Value | |
|---|---|---|---|
| FVIII activity >168%a | |||
| On admission | 2.24 | 0.81–6.21 | 0.122 |
| Immediately after thrombolysis | 7.10 | 1.77–28.38 | 0.006 |
| 24 h after thrombolysis | 4.67 | 1.42–15.38 | 0.011 |
| VWF antigen >160%a | |||
| On admission | 2.52 | 0.65–9.73 | 0.180 |
| Immediately after thrombolysis | 6.31 | 1.83–21.73 | 0.003 |
| 24 h after thrombolysis | 19.02 | 1.94–186.99 | 0.012 |
mRS, modified Rankin Scale.
Backward multiple logistic regression model included age >75 years, gender, hsCRP >5.2 mg/L, active smoking, diabetes mellitus, NIHSS >5 on admission.
aThe upper limit of reference interval.
Discussion
In this study, we examined the levels of FVIII and VWF during thrombolysis in 131 consecutive AIS patients and studied the relationship between the hemostasis factor levels and stroke characteristics and therapy outcomes. Only few papers are found in the literature studying the changes of certain hemostasis factors during the course of thrombolysis following ischemic stroke (28–31) and up to our knowledge, none of them studied the levels of FVIII and VWF comprehensively in this respect. It has been known for almost 40 years that in vitro plasmin degrades and inactivates FVIII (32). Studies in animal models also suggested such effect of plasmin on FVIII (33); however, the in vivo effect of plasmin on FVIII in humans during the course of rt-PA-induced thrombolysis, has not yet been characterized. Here, we showed that FVIII activity drops significantly immediately after thrombolysis as compared to levels measured on admission of patients. However, as the vast majority of patients had elevated FVIII levels on admission, this reduction, most probably due to plasmin-mediated degradation, did not reach a level that would suggest a potential risk for intracerebral hemorrhage. In fact, FVIII levels measured at any time points in this study were not associated with bleeding complications, which is in line with the results of studies in animal models (16). Opposite to FVIII activity, VWF antigen levels showed a rising tendency during the course of thrombolysis in our study. This, in theory might be due to two reasons. The first apparent reason is VWF degradation by plasmin, which has been shown before in vitro (34, 35). As the test we used for measuring VWF antigen levels contains polyclonal antibody against VWF, the degradation of the protein leads to an increased antigen level. In an early paper describing the time course of certain hemostasis factors in a few patients (n = 7) with AMI treated by rt-PA induced thrombolysis, it was shown that thrombolysis treatment resulted in the elevation of VWF antigen levels, most probably due to the proteolysis of VWF multimers. The degradation of VWF multimers has been speculated to be a potential causative factor for hemorrhagic complications in AMI patients treated with thrombolysis (11, 35). In our study, VWF antigen levels were found to be significantly higher at 24 h post-lysis in patients with SICH as compared to the rest of the cohort, but due to the relatively low number of patients with SICH in this population (n = 6), this association should be confirmed by other studies. As for a second reason for the elevation of VWF antigen levels post-lysis, it is plausible that the increase is due to endothelial damage caused by ischemic damage. Studies in AMI patients suggested that thrombolysis induced by streptokinase is associated with an increase of VWF antigen levels due to endothelial damage as a result of oxidative stress caused by the thrombolytic agent (11, 15). Interestingly, in our study, VWF antigen levels showed an increase after thrombolysis only in patients with more severe stroke (NIHSS 6–16 and NIHSS >16 on admission), while in the group of patients with less severe stroke (NIHSS 0–5) this elevation was not seen, suggesting that at least in part endothelial dysfunction is likely to contribute to this finding.
Many studies have investigated the association between FVIII and/or VWF levels and the risk of cardiovascular or cerebrovascular events (8, 9, 12, 36). Despite few conflicting results, it has been well established that elevated FVIII and/or VWF levels predispose patients to AIS (8, 12). In line with our findings, most studies revealed that in the majority of tested patients with AIS, high FVIII and VWF levels were found; moreover, baseline stroke severity, as measured by the NIHSS score was associated with elevated FVIII and/or VWF levels (13, 37, 38). Furthermore, beyond these previously known results, here we describe a strong association between elevated FVIII/VWF levels during the course of thrombolysis and the ASPECT score in patients as assessed 24 h post-lysis. The only non-significant association in this respect was for FVIII activity tested immediately after lysis, which was most probably due to plasmin-mediated degradation of the protein. The finding that the ASPECT score the day after stroke shows a strong association with the tested hemostasis parameters is of considerable interest, as it indicates a link between the investigated factors and stroke severity as verified by not only the NIHSS functional score but by imaging analysis as well. Similar findings on the relation of any hemostasis factors and the results of such imaging analysis is practically lacking in the literature as yet. Limited evidence is available on the possible association of FVIII/VWF levels with the etiology of stroke; moreover, reports are often discordant in this respect (8, 12, 39). Here, we could not find any association of FVIII/VWF levels with the subtype of stroke as classified by the TOAST criteria.
While the association between VWF levels and thrombolysis outcome following AMI has been studied before (15), surprisingly, similar data regarding ischemic stroke are much more limited. Here, we show that a FVIII activity and VWF antigen level above the upper limit of the reference interval, as measured immediately after or 24 h post-lysis, confer a significant, independent risk for poor functional outcomes at 90 days post-event. Our results indicate that both factors could be useful biomarkers having significant prognostic values on long-term outcomes, which might help with patient selection requiring alternative treatment post-lysis. At the same time, at least according to results of this cohort, pretreatment FVIII and VWF levels were not indicative of thrombolysis outcomes.
Although here we propose that our results have prognostic value in the studied patient cohort; nevertheless, we consider the relevance of our findings as potentially useful descriptive data, which might provide basis for future research, while its clinical relevance remains to be fully elucidated. In the era of mechanical thrombectomy, the management of AIS faces new types of decision-making questions in the clinical practice. Useful biomarkers with predictive values regarding poor outcomes might be incorporated into algorithms designed to select candidates for alternative approaches rather than rt-PA alone, e.g., mechanical thrombectomy or other pharmacological approaches (40–42). Moreover, studies on VWF in particular might prove even more useful in the future, as preclinical and clinical studies on inhibitors of VWF are promising and show a safe antithrombotic potential. When used in combination with tPA, VWF antagonists were able to prevent ongoing microvascular thrombus formation reducing stroke progression (7, 17). These findings are particularly interesting in the light of our observations showing that VWF median and IQR values were constantly above the upper limit of the reference interval in the studied AIS population. Although drugs that target the inhibition of the action of VWF have not yet reached approval for the market (17), studies on FVIII/VWF levels during stroke and thrombolysis might provide useful descriptive data to understand the pathophysiology relevant to the potential clinical application of these inhibitors in the future in humans.
Limitations
Our study has limitations. The sample size is limited, but in the light of other studies on AIS patients treated by thrombolysis it is considered representative. Due to the limited number of patients with SICH and with poor outcomes in this cohort, despite the significant associations found, results presented here need to be verified by larger studies.
We did not investigate AIS patients who were not suitable for rt-PA therapy. In theory, measuring FVIII/VWF levels of patients receiving and not receiving rt-PA and comparing the results with outcomes might seem useful. However, due to the important baseline differences between the two groups (e.g., the group not receiving rt-PA might be highly heterogeneous regarding time window from symptom onset, baseline coagulation screening tests, effective anticoagulation, age, etc.), which may significantly affect the results, such comparison might fail to support relevant conclusions.
The lack of advanced neuro-imaging (e.g., perfusion and collateral circulation imaging) limits the application of this study.
Finally, as the study was designed to find potential biomarkers with predictive values for long-term outcomes following thrombolysis, we did not perform any functional characterization studies on the plasmin-mediated effect of FVIII and VWF proteins. In case of FVIII activity, we assumed, based on previous studies, that the reduction in activity levels as detected immediately after thrombolysis is due to plasmin-mediated degradation and did not perform any biochemical tests to prove this hypothesis. In case of VWF, functional activity tests, including ristocetin-induced activity tests, collagen-binding assay, multimer testing, etc. were not measured in the patient population. Future studies are required to elucidate whether the qualitative changes of both proteins following stroke and thrombolysis would have any pathophysiological relevance and prognostic value.
Conclusion
Here, we report the changes in FVIII activity levels and VWF antigen levels during the course of thrombolysis in a cohort of consecutive AIS patients. Elevated FVIII activity and VWF antigen levels immediately after lysis and 24 h post-therapy were shown to have independent prognostic values regarding poor functional outcomes at 90 days.
Ethics Statement
The study was approved by the Ethics Committee of the University of Debrecen, Hungary. All patients or their relatives provided written informed consent.
Author Contributions
LC and ZB designed the study. ES, KC-K, FS, EB, KF, and IF were involved in sample collection and source data preparation. NT and ON performed the measurements. NT and ZB analyzed the data, designed and performed the statistical analysis, and wrote the paper. All authors agreed to the final version of the manuscript.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors would like to thank Prof. László Muszbek for helpful discussions. They thank all co-workers of the Department of Laboratory Medicine, Debrecen, Hungary, who participated in the blood collection and analysis of routine blood samples.
Footnotes
Funding. This work was supported by grants from the National Research, Development and Innovation Fund (K109712, K120042, PD111929), by GINOP-2.3.2-15-2016-00043, and by the Hungarian Academy of Sciences (MTA-DE Cerebrovascular and Neurodegenerative Research Group). Supported by the ÚNKP-17-4-III-DE-381 New National Excellence Program of The Ministry of Human Capacities. ZB is the recipient of János Bólyai fellowship and Lajos Szodoray Prize.
Supplementary Material
The Supplementary Material for this article can be found online at http://www.frontiersin.org/articles/10.3389/fneur.2017.00721/full#supplementary-material.
von Willebrand factor (VWF) antigen levels during the course of thrombolysis in patients with or without therapy-associated symptomatic intracranial hemorrhage (SICH). Results are expressed as median values (circles) and interquartile ranges (whiskers) as measured from samples taken on admission, immediately after thrombolysis and 24 h after thrombolysis. Open circles represent patients with SICH, solid circles represent patients with no bleeding or with asymptomatic intracranial hemorrhage (aSICH). Upper and lower limits of VWF reference interval (50–160%) are indicated with dashed lines. Statistical significance was assessed using Mann–Whitney’s U test. *p < 0.05 for SICH vs. no bleeding/aSICH.
References
- 1.Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation (2016) 133:e38–360. 10.1161/CIR.0000000000000366 [DOI] [PubMed] [Google Scholar]
- 2.Fugate JE, Giraldo EA, Rabinstein AA. Thrombolysis for cerebral ischemia. Front Neurol (2010) 1:139. 10.3389/fneur.2010.00139 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tsivgoulis G, Kargiotis O, Alexandrov AV. Intravenous thrombolysis for acute ischemic stroke: a bridge between two centuries. Expert Rev Neurother (2017) 17:819–37. 10.1080/14737175.2017.1347039 [DOI] [PubMed] [Google Scholar]
- 4.Lees KR, Emberson J, Blackwell L, Bluhmki E, Davis SM, Donnan GA, et al. Effects of alteplase for acute stroke on the distribution of functional outcomes: a pooled analysis of 9 trials. Stroke (2016) 47:2373–9. 10.1161/STROKEAHA.116.013644 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miller DJ, Simpson JR, Silver B. Safety of thrombolysis in acute ischemic stroke: a review of complications, risk factors, and newer technologies. Neurohospitalist (2011) 1:138–47. 10.1177/1941875211408731 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karaszewski B, Houlden H, Smith EE, Markus HS, Charidimou A, Levi C, et al. What causes intracerebral bleeding after thrombolysis for acute ischaemic stroke? Recent insights into mechanisms and potential biomarkers. J Neurol Neurosurg Psychiatry (2015) 86:1127–36. 10.1136/jnnp-2014-309705 [DOI] [PubMed] [Google Scholar]
- 7.De Meyer SF, Stoll G, Wagner DD, Kleinschnitz C. von Willebrand factor: an emerging target in stroke therapy. Stroke (2012) 43:599–606. 10.1161/STROKEAHA.111.628867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Siegler JE, Samai A, Albright KC, Boehme AK, Martin-Schild S. Factoring in factor VIII with acute ischemic stroke. Clin Appl Thromb Hemost (2015) 21:597–602. 10.1177/1076029615571630 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conlan MG, Folsom AR, Finch A, Davis CE, Sorlie P, Marcucci G, et al. Associations of factor VIII and von Willebrand factor with age, race, sex, and risk factors for atherosclerosis. The Atherosclerosis Risk in Communities (ARIC) Study. Thromb Haemost (1993) 70:380–5. [PubMed] [Google Scholar]
- 10.Vischer UM. von Willebrand factor, endothelial dysfunction, and cardiovascular disease. J Thromb Haemost (2006) 4:1186–93. 10.1111/j.1538-7836.2006.01949.x [DOI] [PubMed] [Google Scholar]
- 11.Paulinska P, Spiel A, Jilma B. Role of von Willebrand factor in vascular disease. Hamostaseologie (2009) 29:32–8. [PubMed] [Google Scholar]
- 12.Sonneveld MA, de Maat MP, Leebeek FW. Von Willebrand factor and ADAMTS13 in arterial thrombosis: a systematic review and meta-analysis. Blood Rev (2014) 28:167–78. 10.1016/j.blre.2014.04.003 [DOI] [PubMed] [Google Scholar]
- 13.Chang TR, Albright KC, Boehme AK, Dorsey A, Sartor EA, Kruse-Jarres R, et al. Factor VIII in the setting of acute ischemic stroke among patients with suspected hypercoagulable state. Clin Appl Thromb Hemost (2014) 20:124–8. 10.1177/1076029613488936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Faille D, Labreuche J, Meseguer E, Huisse MG, Ajzenberg N, Mazighi M. Endothelial markers are associated with thrombolysis resistance in acute stroke patients. Eur J Neurol (2014) 21:643–7. 10.1111/ene.12369 [DOI] [PubMed] [Google Scholar]
- 15.Lip GY, Lydakis C, Nuttall SL, Landray MJ, Watson RD, Blann AD. A pilot study of streptokinase-induced endothelial injury and platelet activation following acute myocardial infarction. J Intern Med (2000) 248:316–8. 10.1046/j.1365-2796.2000.00738.x [DOI] [PubMed] [Google Scholar]
- 16.Stewart D, Kong M, Novokhatny V, Jesmok G, Marder VJ. Distinct dose-dependent effects of plasmin and TPA on coagulation and hemorrhage. Blood (2003) 101:3002–7. 10.1182/blood-2002-08-2546 [DOI] [PubMed] [Google Scholar]
- 17.Denorme F, De Meyer SF. The VWF-GPIb axis in ischaemic stroke: lessons from animal models. Thromb Haemost (2016) 116:597–604. 10.1160/TH16-01-0036 [DOI] [PubMed] [Google Scholar]
- 18.European Stroke Organisation (ESO) Executive Committee, ESO Writing Committee. Guidelines for management of ischaemic stroke and transient ischaemic attack 2008. Cerebrovasc Dis (2008) 25:457–507. 10.1159/000131083 [DOI] [PubMed] [Google Scholar]
- 19.Aviv RI, Mandelcorn J, Chakraborty S, Gladstone D, Malham S, Tomlinson G, et al. Alberta Stroke Program Early CT Scoring of CT perfusion in early stroke visualization and assessment. AJNR Am J Neuroradiol (2007) 28:1975–80. 10.3174/ajnr.A0689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Brott T, Adams HP, Jr, Olinger CP, Marled JR, Barman WAG, Biller J, et al. Measurements of acute cerebral infarction: a clinical examination scale. Stroke (1989) 20:864–70. 10.1161/01.STR.20.7.864 [DOI] [PubMed] [Google Scholar]
- 21.Adams HP, Jr, Bendixen BH, Kappelle LJ, Biller J, Love BB, Gordon DL, et al. Classification of subtype of acute ischemic stroke. Definitions for use in a multicenter clinical trial. TOAST. Trial of ORG 10172 in Acute Stroke Treatment. Stroke (1993) 24:35–41. 10.1161/01.STR.24.1.35 [DOI] [PubMed] [Google Scholar]
- 22.Larrue V, von Kummer RR, Muller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke (2001) 32:438–41. 10.1161/01.STR.32.2.438 [DOI] [PubMed] [Google Scholar]
- 23.van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J. Interobserver agreement for the assessment of handicap in stroke patients. Stroke (1988) 19:604–7. 10.1161/01.STR.19.5.604 [DOI] [PubMed] [Google Scholar]
- 24.Jovin TG, Chamorro A, Cobo E, de Miquel MA, Molina CA, Rovira A, et al. Thrombectomy within 8 hours after symptom onset in ischemic stroke. N Engl J Med (2015) 372:2296–306. 10.1056/NEJMoa1503780 [DOI] [PubMed] [Google Scholar]
- 25.Logallo N, Kvistad CE, Naess H, Waje-Andreassen U, Thomassen L. Mild stroke: safety and outcome in patients receiving thrombolysis. Acta Neurol Scand Suppl (2014) 129:37–40. 10.1111/ane.12235 [DOI] [PubMed] [Google Scholar]
- 26.Weir NU, Pexman JH, Hill MD, Buchan AM, CASES Investigators . How well does ASPECTS predict the outcome of acute stroke treated with IV tPA? Neurology (2006) 67:516–8. 10.1212/01.wnl.0000228221.44334.73 [DOI] [PubMed] [Google Scholar]
- 27.Schroder J, Thomalla G. A critical review of Alberta Stroke Program Early CT Score for evaluation of acute stroke imaging. Front Neurol (2017) 7:245. 10.3389/fneur.2016.00245 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sun X, Berthiller J, Derex L, Trouillas P, Diallo L, Hanss M. Post-thrombolysis haemostasis changes after rt-PA treatment in acute cerebral infarct. Correlations with cardioembolic aetiology and outcome. J Neurol Sci (2015) 349:77–83. 10.1016/j.jns.2014.12.029 [DOI] [PubMed] [Google Scholar]
- 29.Fassbender K, Dempfle CE, Mielke O, Schwartz A, Daffertshofer M, Eschenfelder C, et al. Changes in coagulation and fibrinolysis markers in acute ischemic stroke treated with recombinant tissue plasminogen activator. Stroke (1999) 30:2101–4. 10.1161/01.STR.30.10.2101 [DOI] [PubMed] [Google Scholar]
- 30.Alessi MC, Gaudin C, Grosjean P, Martin V, Timsit S, Mahagne MH, et al. Changes in activated thrombin-activatable fibrinolysis inhibitor levels following thrombolytic therapy in ischemic stroke patients correlate with clinical outcome. Cerebrovasc Dis (2016) 42:404–14. 10.1159/000447722 [DOI] [PubMed] [Google Scholar]
- 31.Sun X, Berthiller J, Trouillas P, Derex L, Diallo L, Hanss M. Early fibrinogen degradation coagulopathy: a predictive factor of parenchymal hematomas in cerebral rt-PA thrombolysis. J Neurol Sci (2015) 351:109–14. 10.1016/j.jns.2015.02.048 [DOI] [PubMed] [Google Scholar]
- 32.Atichartakarn V, Marder VJ, Kirby EP, Budzynski AZ. Effects of enzymatic degradation on the subunit composition and biologic properties of human factor VIII. Blood (1978) 51:281–97. [PubMed] [Google Scholar]
- 33.Hoover-Plow J. Does plasmin have anticoagulant activity? Vasc Health Risk Manag (2011) 6:199–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hamilton KK, Fretto LJ, Grierson DS, McKee PA. Effects of plasmin on von Willebrand factor multimers. Degradation in vitro and stimulation of release in vivo. J Clin Invest (1985) 76:261–70. 10.1172/JCI111956 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Federici AB, Berkowitz SD, Zimmerman TS, Mannucci PM. Proteolysis of von Willebrand factor after thrombolytic therapy in patients with acute myocardial infarction. Blood (1992) 79:38–44. [PubMed] [Google Scholar]
- 36.Samai AA, Boehme AK, Shaban A, George AJ, Dowell L, Monlezun DJ, et al. A model for predicting persistent elevation of factor VIII among patients with acute ischemic stroke. J Stroke Cerebrovasc Dis (2016) 25:428–35. 10.1016/j.jstrokecerebrovasdis.2015.10.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Menih M, Krizmaric M, Hojs Fabjan T. Clinical role of von Willebrand factor in acute ischemic stroke. Wien Klin Wochenschr (2017) 129:491–6. 10.1007/s00508-017-1200-4 [DOI] [PubMed] [Google Scholar]
- 38.Kraft P, Drechsler C, Gunreben I, Nieswandt B, Stoll G, Heuschmann PU, et al. Von Willebrand factor regulation in patients with acute and chronic cerebrovascular disease: a pilot, case-control study. PLoS One (2014) 9:e99851. 10.1371/journal.pone.0099851 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bath PM, Blann A, Smith N, Butterworth RJ. Von Willebrand factor, P-selectin and fibrinogen levels in patients with acute ischaemic and haemorrhagic stroke, and their relationship with stroke sub-type and functional outcome. Platelets (1998) 9:155–9. 10.1080/09537109876618 [DOI] [PubMed] [Google Scholar]
- 40.Jayaraman MV, McTaggart RA, Goyal M. Unresolved issues in thrombectomy. Curr Neurol Neurosci Rep (2017) 17:69. 10.1007/s11910-017-0776-4 [DOI] [PubMed] [Google Scholar]
- 41.Evans MRB, White P, Cowley P, Werring DJ. Revolution in acute ischaemic stroke care: a practical guide to mechanical thrombectomy. Pract Neurol (2017) 17:252–65. 10.1136/practneurol-2017-001685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Christophe BR, Mehta SH, Garton AL, Sisti J, Connolly ES, Jr. Current and future perspectives on the treatment of cerebral ischemia. Expert Opin Pharmacother (2017) 18:573–80. 10.1080/14656566.2017.1309022 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
von Willebrand factor (VWF) antigen levels during the course of thrombolysis in patients with or without therapy-associated symptomatic intracranial hemorrhage (SICH). Results are expressed as median values (circles) and interquartile ranges (whiskers) as measured from samples taken on admission, immediately after thrombolysis and 24 h after thrombolysis. Open circles represent patients with SICH, solid circles represent patients with no bleeding or with asymptomatic intracranial hemorrhage (aSICH). Upper and lower limits of VWF reference interval (50–160%) are indicated with dashed lines. Statistical significance was assessed using Mann–Whitney’s U test. *p < 0.05 for SICH vs. no bleeding/aSICH.