Abstract
Background
The quality of nursing homes (NHs) has attracted a lot of interest in recent years and is one of the most challenging issues for policy-makers. Nutritional care should be considered an important variable to be measured from the perspective of quality management. The aim of this systematic review is to describe the use of structural, process, and outcome indicators of nutritional care in NHs and the relationship among them.
Methods
The literature search was carried out in Pubmed, Embase, Scopus, and Web of Science. A temporal filter was applied in order to select papers published in the last 10 years. All types of studies were included, with the exception of reviews, conference proceedings, editorials, and letters to the editor. Papers published in languages other than English, Italian, and Spanish were excluded.
Results
From the database search, 1063 potentially relevant studies were obtained. Of these, 19 full-text articles were considered eligible for the final synthesis. Most of the studies adopted an observational cross-sectional design. They generally assessed the quality of nutritional care using several indicators, usually including a mixture of many different structural, process, and outcome indicators. Only one of the 19 studies described the quality of care by comparing the results with the threshold values. Nine papers assessed the relationship between indicators and six of them described some significant associations—in the NHs that have a policy related to nutritional risk assessment or a suitable scale to weigh the residents, the prevalence or risk of malnutrition is lower. Finally, only four papers of these nine included risk adjustment. This could limit the comparability of the results.
Conclusion
Our findings show that a consensus must be reached for defining a set of indicators and standards to improve quality in NHs. Establishing the relationship between structural, process, and outcome indicators is a challenge. There are grounds for investigating this theme by means of prospective longitudinal studies that take the risk adjustment into account.
Keywords: Malnutrition, Nutritional care, Structural indicators, Process indicators, Nursing homes
Background
With the increase in life expectancy and the prevalence of disabilities and comorbidity related to aging, nursing homes (NHs) now play an increasingly important role.
The quality of NHs has attracted a lot of interest in recent years and is one of the most challenging issues for policy-makers. In the NH sector, poor quality represents an issue of public concern and discussions are taking place to address it [1–4]. The quality of care in NHs is a multidimensional construct that is difficult to define and assess. According to Donabedian’s framework [5], quality is a function of three domains: structure, process, and outcome. Structure is defined by the attributes of the settings in which care is provided, process by the activities of the care-giving practitioners, and outcome by the change in the health status of the patient. Within these three domains, the quality of care can be measured by using the structure, process, and outcome quality indicators.
The use of structural and process indicators for quality management offers several advantages — they are generally easy to measure and interpret and the collected data are often routinely available. However, they might not reflect the level of the quality of care; structural and process indicators indicate the attributes of the NH and what is being done (or is supposed to be done), but they do not automatically translate into a higher quality of care or better outcomes. Therefore, they are ‘necessary but not sufficient’ characteristics and do not necessarily indicate the appropriateness of what is being done [6, 7]. Moreover, the NH context is complex and very little knowledge translation has been carried out to date [8–10]. Outcome indicators overcome these limitations and are considered to be more closely related to quality. However, they are influenced by the risk level of elderly patients—primarily due to their health status—as well as by the quality of the care process. For these reasons, outcome indicators have to be risk-adjusted [7, 11].
Moreover, in order for structural and process indicators to be valid for NHs in terms of other care settings, they must first demonstrate the ability to generate a better outcome [6]. Specifically, they should be associated with and influence the outcome indicator, for example in terms of variation over time.
These unresolved issues and limitations in the use and interpretation of quality indicators have led to difficulties in assessing the real influence of the structural and process indicators on the prediction of the outcome indicators. Difficulties have also arisen, in general, in the evaluation of the effectiveness of quality indicators and quality systems for improving the quality of care, health status, and quality of life in NHs [12–15].
Malnutrition and unintentional weight loss in the NHs are major issues because of their high prevalence, serious health consequences, and related healthcare costs [16–20]. Recent studies estimate that 20% of NH residents suffer from some form of malnutrition, the prevalence of which ranges between 1.5 and 66.5%, depending on the definition [17]. Moreover, malnutrition can influence the health status, leading to clinical complications such as impaired immune response, depression, pressure ulcers, falls, and even death [18].
The causes of malnutrition and weight loss in elderly people living in long-term care facilities can be classified as either individual (age, comorbidity) or organizational [21, 22]. For many elderly adults in NHs, aging is accompanied by a progressive physiological and medical decline, which leads to nutritional vulnerability. This in turn can create a progressive feeding dependency. Many organizational factors can negatively affect the assumption of nutritionally adequate diet for such people, thus increasing the likelihood of malnutrition and weight loss. Therefore, nutritional care (i.e. the substances, procedures, and setting involved in ensuring the proper intake and assimilation of nutrients) must be considered an important variable that should be measured from the perspective of quality management by using the related structural, process, and outcome indicators [12, 22–26].
The aim of this review is to describe the state of the art with regard to:
the use of quality indicators of nutritional care in NHs;
the relationship between structural, process, and outcome indicators of nutritional care in NHs.
Methods
The literature search was carried out in four databases—Pubmed, Embase, Scopus, and Web of Science—and was completed with a manual search on the basis of the references given in the selected papers.
While performing the research, a temporal filter was applied in order to select papers published in the last 10 years. Databases were last accessed on 18 February 2016.
The search strategies used in each database are reported in Table 1.
Table 1.
Search strategies of systematic review
| DATABASE | Search strategy |
|---|---|
| Pubmed | ((((((“Quality Assurance, Health Care”[Mesh]) OR “Quality Improvement”[Mesh]) OR “Quality Indicators, Health Care”[Mesh]) OR “Health Care Quality, Access, and Evaluation”[Mesh])) AND “last 10 years”[PDat]) AND ((“Malnutrition”[Mesh] OR “nutritional care” OR “weight loss”) AND “last 10 years”[PDat]) AND ((“Nursing Homes”[Mesh] OR “Long-Term Care”[Mesh]) AND “last 10 years”[PDat]) |
| Embase | quality OR indicator* OR assurance OR ‘health care’/exp. AND (‘malnutrition’/exp. OR ‘nutritional care’ OR ‘weight loss’/exp) AND ‘nursing home* |
| Scopus | (((quality OR indicator* OR assurance OR “health care”) AND (malnutrition OR “nutritional care” OR “weight loss”) AND (nursing home*))) |
| Web of Science | (((quality OR indicator* OR assurance OR “health care”) AND (malnutrition OR “nutritional care” OR “weight loss”) AND (nursing home*))) |
Two reviewers independently selected papers based on the inclusion criteria. Disagreements were resolved through a consensus meeting in the presence of a third reviewer.
In order to be included, papers had to examine both care quality and nutritional care in the specific setting of NHs; moreover, they had to respond to the aims of this study, namely to describe the use of quality indicators of nutritional care in NHs and/or to assess the relationship between structural, process, and outcome indicators of nutritional care in NHs. All types of studies were included, with the exception of reviews, conference proceedings, editorials, and letters to the editor.
Papers published in languages other than English, Italian and Spanish were excluded.
Figure 1 summarizes the selection process of the articles.
Fig. 1.
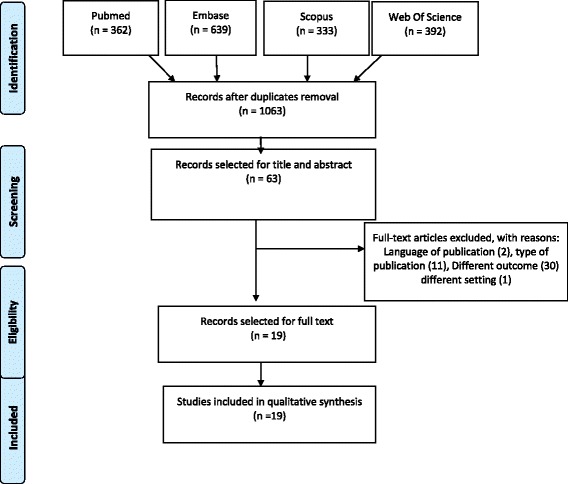
Flow diagram of the study selection [58]
Results
From the database search, 1063 potentially relevant studies were obtained and screened for the presence of all inclusion criteria. Of the 63 studies selected on the basis of title and abstract, 44 were excluded: two because of language of publication, 11 for type of publication (four conference proceedings, three narrative reviews, three editorials, and one letter to the editor), 30 for outcomes (24 not concerning quality aspects, four not reporting quality indicators, and two not concerning nutritional aspects), and one for setting. Ultimately, 19 full-text articles were considered eligible for the final synthesis (Fig. 1).
Table 2 shows the main characteristics of each of the selected papers, including year of publication, country, setting, number of participants, type, and aim of the study. Most of the studies were conducted in the USA or Europe and adopted an observational cross-sectional design. One study [27] combined the Delphi method with an observational design. In two papers, the authors conducted a before/after analysis [28, 29].
Table 2.
Main characteristics of selected studies
| 1st Author, Year of publication | Country | Setting/ n. participants | Type of study | Aim of the study |
|---|---|---|---|---|
| Bonaccorsi, 2015 [35] | Italy | 67 NHs; 2395 participants | Cross-sectional survey | To describe the quality indicators of nutritional care in older residents in a sample of NHs in Tuscany, Italy, and to evaluate the predictors of protein-energy malnutrition risk. |
| Dyck, 2007 [39] | USA | 2948 NHs for malnutrition; 364,339 residents | Cross-sectional analysis of two data sets | To examine the relationships between nursing staffing and the nursing home resident outcome on weight loss and dehydratation . |
| Halfens, 2013 [30] | The Netherlands, Austria, Switzerland | 211 hospitals (20,232 patients); 165 NHs (6969 residents) | Cross-sectional multicentre study. | To measure care problems (including malnutrition) in terms of prevalence rates, prevention, treatment, and quality indicators in healthcare organizations in the Netherlands, Austria, and Switzerland. |
| Hjaltadottir, 2012 [27] | Iceland | Panel for Delphi method: 12 experts; 47 NHs (2247 participants) | Two rounds Delphi study and observational study | To determine upper and lower thresholds of Minimum Data Set quality indicators for Icelandic NHs. |
| Hurtado, 2016 [40] | USA | 30 NHs | Prospective ecological study | To examine whether quality of care in NHs was predicted by schedule control (workers’ ability to decide work hours), independent of other staffing characteristics. |
| Lee, 2014 [41] | USA | 195 NHs | Cross-sectional analysis of five data sets | To examine the association of registered nurse staffing hours and five quality indicators, including process and outcome measures. |
| Meijers, 2009 [59] | The Netherlands | 50 hospitals, 90 NHs, 16 care homes, and 20,255 participants | Cross-sectional multicentre study | To investigate screening, treatment, and other quality indicators of nutritional care in Dutch healthcare organizations. |
| Meijers, 2014 [36] | The Netherlands | 74 Care homes (41 participated four times,33 five times); 26,046 participants (2007–2011) | Cross-sectional study | To analyse the trend of malnutrition prevalence rates between 2007 and 2011 in Dutch care homes and the effect of process and structural indicators on malnutrition prevalence rates. |
| Moore, 2014 [31] | Australia | Four Residential Aged Care (RAC) | Cross-sectional study | To explore relationships among the Victorian Public Sector RAC Services quality indicators and other demographic and health-related issues. |
| Rantz, 2009 [29] | USA | 492 NHs | Before-after observational study | To present and discuss the evaluation of the Quality Improvement Program of Missouri in 2006, using some outcome indicators. |
| Schönherr, 2012 [32] | Austria | 18 NHs (1487 participants); 18 hospitals (2326 participants) | Multicentre cross-sectional study | To describe and compare structural and process indicators of nutritional care in Austrian hospitals and NHs. |
| Shin, 2015 [42] | Korea | 150 NHs | Cross-sectional study | To investigate the relationship between nurse staffing and quality of care in NHs in Korea. |
| Simmons, 2006 [28] | USA | 1 NHs (48 beds) | Before-after observational study | To train long-term care staff in conducting continuous quality improvement (CQI) related to nutritional care. |
| Simmons, 2007 [44] | USA | 7 NHs | Cross-sectional study | To assess the impact of Paid Feeding Assistant (PFA) programmes on feeding assistance care process quality. |
| Van Nie, 2014 [37] | The Netherlands, Germany and Austria | 214 NHs 19,876 residents | Multicentre cross-sectional study | To identify structural quality indicators of nutritional care that influence the outcome of quality of care in terms of prevalence of malnutrition and effect of possible differences between malnutrition prevalence in Dutch, German, and Austrian NHs. |
| van Nie-Visser, 2011 [33] | The Netherlands and Germany | 151 NHs, 10,771 participants | Multicentre cross-sectional study | To investigate possible differences in malnutrition prevalence rates in Dutch and German NHs, as well as in structural and process indicators for nutritional care |
| van Nie-Visser, 2014 [34] | The Netherlands, Germany and Austria | 214 NHs; 19,876 residents | Multicentre cross-sectional study | To investigate possible differences in malnutrition prevalence rates in Austrian, Dutch, and German NHs, as well as in structural and process indicators for nutritional care; to investigate whether resident characteristics influence possible differences in malnutrition prevalence between countries. |
| van Nie-Visser, 2015 [38] | The Netherlands, Germany and Austria | 214 NH; 22,886 participants, | Multicentre cross-sectional study | To explore whether structural quality indicators for nutritional care influence malnutrition prevalence in Dutch, German, and Austrian NHs |
| Werner, 2013 [43] | USA | 16,623 NHs | Cross- sectional study using 2 data sets | To test how changes in NH processes improve outcomes of care. |
Seven studies only aimed to measure the prevalence of malnutrition/weight loss (as outcome indicator) and the use of structural or process indicators [20, 27, 30–34]. Four others tried to assess both the prevalence of malnutrition and the relationship among the quality indicators [35–38]. Five only assessed the relationship between indicators (without describing their prevalence/use) [39–43], and three examined the effect of nutritional care interventions on outcome indicators [28, 29, 44].
With regard to the collection of information, the most commonly used instruments were the standardized Landelijke Prevalentiemeting Zorgproblemen (LPZ) questionnaire, the Minimum Data Set (MDS), and the Online Survey, Certification, and Reporting (OSCAR). LPZ is more widely used in European countries and aims to assess malnutrition prevalence. MDS and OSCAR are more common in the American context—the former predicts unplanned weight loss while the latter includes facility-reported data on residents’ characteristics. In some other studies [28, 35, 42, 44], ad hoc instruments were used. In one of them, the ad hoc instrument was improved on the basis of a literature analysis [35]. Hurtado et al. [41] used both standardized instruments and ad hoc questionnaire.
The selected papers show heterogeneity in the considered quality indicators, particularly the structural and process indicators. As regards the outcome indicators, the authors considered the risk of malnutrition (according to Malnutrition Universal Screening Tool), weight loss (according either to MDS or VPSRAC - Victorian Public Sector Residential Aged Care Services - definition), and malnutrition prevalence (according to LPZ questionnaire) (Table 3).
Table 3.
Quality indicators of nutritional care reported in the selected papers
| 1st Author, Year of publication | Instruments for collecting data on quality indicators | Structural/process indicators | Outcome indicators |
|---|---|---|---|
| Bonaccorsi, 2015 [35] | Ad hoc instruments (questionnaire/direct observation) | Structural indicators | Prevalence of subjects with medium to high risk of malnutrition, according to MUST. |
| Type of scales used to weigh residents | |||
| Employment of dietitians and type of consultation | |||
| Number of operators assigned to manage the administration of meals in a specific day | |||
| Process indicators | |||
| Use of a nutrition screening tool | |||
| Presence of protocols/guidelines for weight assessment | |||
| Presence of protocols or guidelines for administration of food | |||
| Assessment of dysphagia | |||
| Dyck, 2007 [39] | MDS; OSCAR | Staffing hours: | Weight lossa |
| - RN hours per resident per day | |||
| - LPN hours per resident per day | |||
| Halfens, 2013 [30] | LPZ | Not described | Malnutrition prevalenceb |
| Hjaltadottir, 2012 [27] | MDS | – | Weight lossa |
| Hurtado, 2016 [40] | Nursing Home Compare/MDS; ad hoc questionnaire | Schedule control (from ad hoc questionnaire): | Weight lossa |
| - to choose when to take day off or vacation | |||
| - to choose when to start/end each work day | |||
| - to choose when to take a few hours of break | |||
| - to decide how many hours to work each day | |||
| Lee, 2014 [41] | MDS; the Colorado state inspections | RN staffing hours (from the Colorado state inspections data) | Weight lossa |
| Meijers, 2009 [59] | LPZ | Institutional level | Malnutrition prevalenceb |
| Availability of an up-to-date protocol/guideline on malnutrition prevention and treatment | |||
| Auditing of protocol/guideline for malnutrition prevention and treatment | |||
| Availability of malnutrition advisory teams | |||
| Multiple dietitians available in the institution | |||
| Malnutrition education (prevention and treatment) given by malnutrition specialist within the last two years | |||
| Ward level | |||
| Trained malnutrition specialist working on the ward | |||
| Control of use of prevention and treatment guidelines | |||
| Policy to measure weight at admission | |||
| Documentation of malnutrition interventions | |||
| Correct mealtime ambience | |||
| Meijers, 2014 [36] | LPZ | Structural indicators | Malnutrition prevalenceb |
| Institutional level | |||
| There is an agreed protocol/guideline for the prevention and/or treatment of malnutrition within the institution. | |||
| There is an advisory committee for malnutrition at the institution or department level. | |||
| There is someone within the institution who is responsible for updating and ensuring that the necessary attention is devoted to the malnutrition protocol. | |||
| Over the last two years, a refresher course and/or a meeting was organized for caregivers, which was/were specifically devoted to the prevention and treatment of malnutrition within the institution. | |||
| Ward level | |||
| There is at least one person/specialist in the department/basic care unit/team who is specialized in the area of malnutrition. | |||
| Work in the department/basic care unit/team is done in a controlled fashion or in accordance with the malnutrition protocol/guideline. | |||
| Upon admission, every resident is weighed as a part of standard procedure. | |||
| The nutritional status is screened upon admission. | |||
| The care file/care plan specifies the activities that must be implemented for residents who are at risk of malnutrition. | |||
| The department has a policy on when and how to measure weight. | |||
| Process indicators | |||
| Assessment of the nutritional status by a validated screening instrument | |||
| Weight monitoring in a controlled fashion | |||
| Dietitian consultation | |||
| Use of nutritional treatment | |||
| Moore, 2014 [31] | VPSRACS; data routinely collected in the facilities included in the study | – | Weight lossc |
| Rantz, 2009 [29] | MDS | Not described (QIPMO—nurse site visits to suggest how to improve quality of care) | Weight lossa |
| Schönherr, 2012 [32] | LPZ | Structural indicators: | Malnutrition prevalenceb |
| Guideline for prevention and treatment | |||
| Auditing of guideline | |||
| Advisory committee for malnutrition | |||
| Updating of guideline | |||
| Criteria for determining malnutrition | |||
| Employment of dietitians | |||
| Refresher course for caregivers | |||
| Information brochure | |||
| Standard policy for handover | |||
| Process indicators | |||
| Assessment of weight | |||
| Use of nutritional screening tool | |||
| Assessment of weight over time | |||
| Use of clinical view | |||
| Use of biochemical parameters | |||
| Dietitian consulted | |||
| Energy- and protein-enriched diet | |||
| Energy-enriched snack | |||
| Oral nutritional support | |||
| Enteral nutrition | |||
| Parenteral nutrition | |||
| Texture-modified diet | |||
| Fluid 1–1.5 L/d | |||
| No interventions owing to palliative policy | |||
| Shin, 2015 [42] | Ad hoc instruments (questionnaire-interviews) | Nurse staffing, by type (RN, CNA, qualified care workers): | Weight lossa |
| - hours per resident per day | |||
| - skill-mix hours per resident per day | |||
| - staff turnover | |||
| Simmons, 2006 [28] | Ah hoc instruments (direct observation) | Feeding Assistance Care Process Measure: | – |
| -% of residents who eat less than 50% of meal and receive less than one min of assistance. | |||
| -% of residents who eat less than 50% of meal and are not offered a substitute. | |||
| -% of residents who receive less than five min of assistance and a supplement. | |||
| -% of residents who are independent but receive physical assistance. | |||
| - % of residents who receive physical assistance without verbal cue. | |||
| Simmons, 2007 [44] | Ah hoc instruments (direct observation) | Feeding Assistance Care Process Measure, by type of staff (CNAs, PFAs, no assistance from either type of staff): | – |
| -% of residents who eat less than 50% of meal and receive less than one min of assistance. | |||
| -% of residents who eat less than 50% of meal and are not offered a substitute. | |||
| -% of residents who receive less than five min of assistance and a supplement. | |||
| -% of residents who are independent but receive physical assistance. | |||
| - % of residents who receive physical assistance without verbal cue. | |||
| Van Nie, 2014 [37] | LPZ | Structural indicators | Malnutrition prevalenceb |
| Institutional level | |||
| There is an agreed protocol/guideline for the prevention and/or treatment of malnutrition within the institution. | |||
| Malnutrition-related work within the institution is carried out in a controlled fashion or in accordance with a malnutrition protocol/guideline. | |||
| There is a multidisciplinary advisory committee for malnutrition at the institutional or ward level. | |||
| There is someone within the institution who is responsible for updating and ensuring that the necessary attention is devoted to the malnutrition protocol. | |||
| Within the institution, criteria have been defined for determining malnutrition. | |||
| There are dietitians employed at the institution. | |||
| Over the past two years, a refresher course and/or a meeting has been organized for caregivers, which was specifically devoted to the prevention and treatment of malnutrition within the institution. | |||
| An information brochure about malnutrition is available at the institution for clients and/or family members. | |||
| Ward level | |||
| There is at least one nurse in the ward who is specialized in the area of malnutrition | |||
| Clients who are at risk of malnourishment or who are malnourished are discussed on the ward during multidisciplinary work consultations. | |||
| Work in the ward is conducted in a controlled fashion or in accordance with a malnutrition protocol/guideline. | |||
| At admission, every client is weighed as a part of standard procedure. | |||
| At admission, the height of each client is determined as a part of standard procedure. | |||
| The nutritional status is assessed at admission. | |||
| The care file includes an assessment as to each patient’s risk of malnutrition. | |||
| The care file/care plan specifies the activities that must be implemented for clients who are at risk of malnutrition. | |||
| In case of (expected) malnutrition, a protein- and energy-enriched diet is provided in the ward as a part of standard procedure. | |||
| Every client who is malnourished (or is at risk for becoming so) and his or her family receive an informational brochure about malnutrition. | |||
| The ambience at mealtimes is taken into account within the ward. | |||
| The care file includes the intake for each client. | |||
| The ward has a weight policy. | |||
| van Nie-Visser, 2011 [33] | LPZ | Structural indicators | Malnutrition prevalenceb and prevalence of subjects with risk of malnutrition. |
| Institution level | |||
| Prevention and treatment protocol/guideline | ‘At risk of malnutrition is defined as meeting one or more of the following criteria: (1) BMI 21–23.9 kg/m2, (2) not eaten or hardly eaten anything for three days or not eaten normally for more than a week. | ||
| Malnutrition advisory team | |||
| Auditing of protocol/guideline | |||
| Dietitians employed in institution | |||
| Education on malnutrition prevention and treatment in last 2 years | |||
| Information brochure available for client or family | |||
| Ward level | |||
| Person specialized in malnutrition on unit | |||
| Control of use of prevention/treatment guideline | |||
| Measurement of weight at admission | |||
| Interventions on malnutrition stated in patient file | |||
| Optimal mealtime ambience provided at dinner | |||
| Process indicators | |||
| Assessment of weight | |||
| Use of nutritional screening tool | |||
| Weight history | |||
| Use of clinical view | |||
| Use of biochemical parameters | |||
| Energy- and protein-enriched diet | |||
| Energy-enriched snacks between meals | |||
| Oral nutritional supplements | |||
| Tube feeding | |||
| Parenteral feeding | |||
| Fluid 1–1.5 L/d | |||
| No interventions | |||
| Palliative policy | |||
| van Nie-Visser, 2015 [38] | LPZ | See above (….) | Malnutrition prevalenceb |
| van Nie-Visser, 2014 [34] | LPZ | – | Malnutrition prevalenceb |
| Werner, 2013 [43] | MDS/Nursing Home Compare; OSCAR | -% of residents receiving tube feeds | Weight lossa |
| -% of residents receiving mechanically altered diets | |||
| -% of residents with assisted eating devices |
MUST Malnutrition Universal Screening Tool
MDS Minimum Data Set
LPZ Landelijke Prevalentiemeting Zorgproblemen (In Dutch)
VPSRACS Victorian Public Sector Residential Aged Care Services
OSCAR Online Survey, Certification, and Reporting
ARF Area Resource File
RN Registered Nurse
LPN Licensed Practical Nurse
CNA certified nursing assistant
QIPMO Quality Improvement Program of Missouri
PFA Paid Feeding Assistant
aloss of 5% or more in the last months or loss of 10% or more in the past six months, as defined in MDS
b(1) BMI ≤ 18.5 kg/m2(age 18–65 years) or BMI ≤ 20 kg/m2 (age > 65 years), and/or (2) unintentional weight loss (more than 6 kg in the previous six month or more than 3 kg in the last month) and/or (3) no nutritional intake for three days or reduced intake for more than 10 days combined with a BMI between 18.5–20 kg/m2 (age18–65 years) or between 20 and 23.9 kg/m2(age > 65 years)
closs of ≥3 kg over three months, or any unplanned weight loss for each consecutive month of the quarter
Of the19 selected papers, nine studies [29, 35–40, 42, 44] examined the influence of structural and process indicators on the outcome indicators (Table 4).
Table 4.
Relationship between structural, process and outcome indicators of nutritional care
| 1st Author, Year of publication | Risk adjustment | Main results |
|---|---|---|
| Bonaccorsi, 2015 [35] | Age, gender, the Barthel Index score, the Pfeiffer test score, the EBS score, where the subject consumed lunch on the day of the survey | Among the process and structural indicators included in the study, the only one with a role in predicting malnutrition was the availability of a scale suitable for weighing residents even in the case of mobility restriction (chair or platform scale). |
| Dyck, 2007 [39] | Residents’ case-mix: end of life, depression, swallowing problem, renal failure, diabetes mellitus | Staffing hours affect weight loss: residents receiving at least three hours/day of nursing assistant care had a 17% decreased likelihood of weight loss. |
| Hurtado, 2016 [40] | High-risk residents’ adjustment at facility level (not described). | Schedule control was not associated with weight loss. |
| Meijers, 2014 [36] | NO | Only the interacted process indicators nutritional screening and oral nutritional supplementation were significant in influencing malnutrition prevalence rates over time. Structural indicators had no impact on the malnutrition prevalence over time. |
| Rantz, 2009 [29] | NO | ‘At risk’ facilities (defined using quality indicators derived from MDS) accepting one or more visits improved weight loss quality indicators by 4%. |
| Shin, 2015 [42] | NO | Hours per resident per day, skill-mix hours per resident per day, and staff turnover are not statistically associated with weight loss. |
| Van Nie, 2014 [37] | NO | Five structural quality indicators influenced malnutrition prevalence in NH residents at the ward level: presence of at least one nurse in the ward specialized in the area of malnutrition; nutrition assessment upon admission; inclusion in the care file of the assessment as to the risk of malnutrition for each client; provision of a protein- and energy-enriched diet in case of (expected) malnutrition, in accordance with a standard procedure; inclusion in the care file of the intake for each client. |
| van Nie-Visser, 2015 [38] | NO | Two structural quality indicators of nutritional care at ward level influence malnutrition prevalence in NH residents: the policy that a care file should include the nutritional intake for each resident and the policy for ward having a weight measurement. |
| Werner, 2013 [43] | Data controlled for case-mix and for facility-level characteristics related to residents’ case-mix: • Age • Activity of Daily Living • Cognitive performance scale • % of residents who needs radiation therapy, chemotherapy, dialysis, intravenous therapy, respiratory treatments, tracheostomy care, ostomy care, suctioning, injections |
The statistically significant improvement in weight loss indicator could not be explained by changes in the investigated measures of process of care (% of residents receiving tube feeds; % of residents receiving mechanically altered diets; % of residents with assisted eating devices). |
EBS Eating Behaviour Scale, MDS Minimum Data Set, OSCAR Online Survey, Certification, and Reporting
In four of the studies [35, 39, 40, 43], an individual risk adjustment procedure was applied by using different variables and determining heterogeneity among the different studies. While five studies [29, 35–38] showed a significant association between some structural or process indicators and the outcome indicators, said association was found for different structural and process indicators.
Discussion
In this review, we selected 19 papers in the aim of investigating the use of quality indicators of nutritional care in NHs. The selected papers assessed the quality of nutritional care in NHs in general by using several indicators, normally including a mixture of several structural, process, and outcome indicators. Most of the studies used standardized questionnaires or instruments to collect data on quality indicators, either routinely applied at a state level for mandatory reasons (MDS, Victorian Public Sector Residential Aged Care Services [VPSRACS]), or implemented as an annual measurement of malnutrition prevalence and structural quality indicators of nutritional care in the NHs that voluntarily decided to participate to the study (LPZ). As for the outcomes, different indicators were taken into account. However, weight loss was always included, although different combinations of time periods and cut-offs were considered for each instrument. It was evident that no consensus exists on the sets of indicators to be used, especially outcome indicators, even though only a few instruments were used to collect data. Nevertheless, according to our findings, the presence of nutritional screening and its inclusion in the care file, the availability and use of protocols on malnutrition prevention and treatment, mealtime assistance, and the use of nutritional treatment/supplements, all appear to be relevant indicators for nutritional care quality assessment. In any case, studies aimed at testing the reliability and validity of these indicators, as well as the outcome indicators, need to be developed in order to identify the best set of indicators for describing the quality of nutritional care in NHs. This is also in agreement with statements of other authors [45, 46].
Most of the papers aimed to describe the quality of nutritional care in NHs, at times also to compare the data in different geographical areas, settings, or time periods. However, they do not discuss the collected data in terms of good or poor quality with respect to a standard, with the exception of the paper by Hjaltadòttir et al. [27], in which the quality of care in Icelandic NHs was compared with the threshold values that had been determined in the same study. Thresholds for quality indicators could help guide and facilitate progress in the NHs’ quality of care, indicating the potentially poor or good quality of care and improvement goals [27]. Criteria and standards specify the expected outcome, and encourage the performer to progress towards fulfilling them. However, no internationally recognized comprehensive standards are available, although the laws and reforms of long-term care systems in many countries have also included aspects of quality assurance and improvement, such as the setting of minimum requirements as preconditions of licensing and contractual decisions for providers [2, 3]. The lack of internationally recognized standards can be attributed to the complexity of the context of long-term care and the fact that context and residents often differ considerably in the different NHs. Research on threshold values and standards for nutritional care should be encouraged, taking into account the specificity of the setting and the residents as well as the knowledge translation aspects [8].
The prevalence or risk of malnutrition is associated with aspects such as having a policy related to nutritional risk assessment (i.e. screening the subjects for malnutrition, weighing them, assessing and recording nutritional intake) or having suitable scales to weight the residents; when these aspects are present or used in NHs, the prevalence or risk of malnutrition is lower.
In two [36, 37] out of three [36–38] articles that investigated the provision of a protein- and energy-enriched diet, or the use of oral nutritional supplementation in case of (expected) malnutrition, this factor was found to be related to malnutrition. Malnutrition is more prevalent in institutions implementing this indicator. Therefore, providing an enriched diet or oral nutritional supplementation seems to be more of an intervention treatment than a preventive one. This hypothesis and the role of screening for malnutrition are both confirmed by the results of the study by Meijers et al. [36]—the only one in which a trend evaluation of the outcome indicator is carried out. In fact, according to the authors, structural screening is the most important indicator of a decrease in the prevalence of malnutrition. In NHs with a higher prevalence of malnutrition, more residents receive oral nutritional supplementation. While the provision of oral nutritional supplementation is associated with a gradual decrease in the prevalence of malnutrition, this drop is more pronounced if the use is lower, probably due to the fact that the group receiving less oral nutritional supplementation is probably in better health [36].
On the other hand, quality indicators related to the staff (i.e. employment of dieticians, malnutrition specialists, person in charge of the malnutrition protocol, or a multidisciplinary malnutrition advisory team, the organization of courses on malnutrition, and staff turnover) do not seem to affect the outcome indicators, with the exception of the ‘presence of at least one nurse in the ward specialized in the area of malnutrition’ in one of the papers by Van Nie et al. [37] and ‘receiving at least [three] hours/day of nursing assistant care’ in the study by Dyck et al. [39]. Consequently, the presence of a staff member with competencies in nutritional aspects and specific education or training is related to malnutrition risk in just one study, where it only concerns the presence of nurses with specific competencies in the area of malnutrition. This result is in line with the results of two reviews regarding staffing and the various aspects of the quality of care in NHs [13, 47].
Regarding the relationship between indicators, we have also included risk adjustment to control individual risk in our assessment, in order to generalize the results for residents with different levels of disabilities and comorbidities. The need for individual risk adjustment in the assessment of quality of care in NHs has emerged simultaneously with the growing attention to quality in healthcare, but only a few authors have considered this factor to avoid a biased use of quality indicators [11, 48]. Individual risk adjustment has yielded better results in terms of validity and comparability, since NH residents are quite dissimilar [3, 7, 49–54]. In our review, only four papers [35, 39, 40, 43] out of nine included risk adjustment, which could limit the comparability of the results. Risk adjustment should also be taken into account when identifying the thresholds for quality indicators in order to control the cut-off levels for individual risk.
Eight [35–40, 42, 43] of the nine articles describe the results obtained through a cross-sectional or ecological approach. One cross-sectional study includes a sample at the time of ascertainment, selected without any reference to exposure or health outcome (disease status or other condition of interest, such as risk of a disease). Exposure is determined simultaneously with the health condition, and different exposure subpopulations are compared with respect to their health status to assess correlation or association between exposure and outcome. Such studies have difficulty determining the chronological order of events (i.e. the beginning of the exposure and the onset of a health condition). Due to this limitation, it is not possible to work out whether an association between exposure and outcome demonstrated in a cross-sectional study underlies a cause-effect relationship. The same issue occurs for ecological studies in which the association or the correlation between exposure and health outcome is assessed using groups rather than individuals (the unit of analysis is the group, and the analysis is conducted without considering the individual level) [55]. Cross-sectional, ecological and other descriptive studies are often the initial tentative approaches to new events or conditions for generating a hypothesis for causation (‘hypothesis-generating’ studies). The etiologic hypothesis has to be tested through cohort, case-control, or experimental studies [56, 57]. Therefore, considering the study design of almost all articles included in this review, it is not possible to fully understand the type of relationship (i.e. etiologic or not) between process or structural indicators and outcome indicators.
One article [29] in the sample includes a before-after observational study aimed at evaluating a quality improvement programme that is not described in detail. As a result, when reading the paper it is not possible to understand whether the implemented measures would be able to foresee aspects concerning specific structural or process indicators.
Conclusions
Our findings show that there is an open debate regarding the indicators that could be used to describe the quality of nutritional care in NHs. A consensus must be reached to define a set of indicators and a standard to improve the quality in NHs. For this purpose, studies aimed at testing the reliability and validity of the indicators are encouraged. Moreover, the relationships among structural, process, and outcome indicators are a matter of challenge. According to our results, while the prevalence or risk of malnutrition is associated with aspects such as having a policy related to nutritional risk assessment or having suitable scales to weigh the residents, these findings need to be confirmed. In conclusion, there are grounds for investigating this new theme by means of prospective longitudinal studies that also take the risk adjustment into account.
Acknowledgements
Not applicable.
Funding
The review has been conducted using the founding of the University of Florence. No external founding has been used.
Availability of data and materials
Not applicable.
Abbreviations
- ARF
Area Resource File
- BMI
Body Mass Index
- CNA
Certified nursing assistant
- EBS
Eating Behaviour Scale
- LPN
Licensed Practical Nurse
- LPZ
Landelijke Prevalentiemeting Zorgproblemen (In Dutch)
- MDS
Minimum Data Set
- MUST
Malnutrition Universal Screening Tool
- NH
nursing home
- OSCAR
Online Survey, Certification, and Reporting
- PFA
Paid Feeding Assistant
- QIPMO
Quality Improvement Program of Missouri
- RN
Registered Nurse
- VPSRACS
Victorian Public Sector Residential Aged Care Services
Authors’ contributions
CL: study design, analysis of the selected papers, interpretation of the results, drafting of the manuscript, final approval of the manuscript. BRP: study design, literature search, selection of the papers, analysis of the selected papers, interpretation of the results, drafting of the manuscript, final approval of the manuscript. FP: study design, literature search, selection of the papers, analysis of the selected papers, interpretation of the results, drafting of the manuscript, final approval of the manuscript. GB: study design, interpretation of the results, drafting of the manuscript, final approval of the manuscript.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Chiara Lorini, Phone: +390552751065, Email: chiara.lorini@unifi.it.
Barbara Rita Porchia, Email: babibell83@gmail.com.
Francesca Pieralli, Email: f.pieralli@gmail.com.
Gugliemo Bonaccorsi, Email: guglielmo.bonaccorsi@unifi.it.
References
- 1.Di Giorgio L, Filippini M, Masiero G. Is higher nursing home quality more costly? Eur J Health Econ. 2015:1–16. 10.1007/s10198-015-0743-4. [DOI] [PubMed]
- 2.OECD/European Commission. A good life in old age? Monitoring and improving quality in long-term care: OECD Health Policy Studies, OECD Publishing; 2013.
- 3.Riedel M, Kraus M. The organisation of formal long-term care for the elderly: results from the 21 European country studies in the ANCIEN project: Social Welfare Policies, ENEPRI Research report; 2011.
- 4.Carter MW, Porell FW. Nursing home performance on selected publicity reported quality indicators and resident risk of hospitalization: grappling with policy implications. J Aging Soc Policy. 2006;18(1):17–39. doi: 10.1300/J031v18n01_02. [DOI] [PubMed] [Google Scholar]
- 5.Donabedian A. The quality of care. How can it be assessed? JAMA. 1988;260(12):1743–1748. doi: 10.1001/jama.1988.03410120089033. [DOI] [PubMed] [Google Scholar]
- 6.Mainz J. Defining and classifying clinical indicators for quality improvement. Int J Qual Health Care. 2003;15(6):523–530. doi: 10.1093/intqhc/mzg081. [DOI] [PubMed] [Google Scholar]
- 7.Castle NG, Ferguson JC. What is nursing home quality and how is it measured? Gerontologist. 2010;50(4):426–442. doi: 10.1093/geront/gnq052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cammer A, Morgan D, Stewart N, McGilton K, Rycroft-Malone J, Dopson S, et al. The Hidden Complexity of Long-Term Care: how context mediates knowledge translation and use of best practices. Gerontologist. 2014;54(6):1013–1023. doi: 10.1093/geront/gnt068. [DOI] [PubMed] [Google Scholar]
- 9.Boström AM, Slaughter SE, Chojecki D, Estabrooks CA. What do we know about knowledge translation in the care of older adults? A scoping review. J Am Med Dir Assoc. 2012;13(3):210–219. doi: 10.1016/j.jamda.2010.12.004. [DOI] [PubMed] [Google Scholar]
- 10.Berta W, Teare GF, Gilbart E, Ginsburg LS, Lemieux-Charles L, Davis D, et al. Spanning the know-do gap: understanding knowledge application and capacity in long-term care homes. Soc Sci Med. 2010;70(9):1326–1334. doi: 10.1016/j.socscimed.2009.11.028. [DOI] [PubMed] [Google Scholar]
- 11.Jones RN, Hirdes JP, Poss JW, Kelly M, Berg K, Fries KB, et al. Adjustment of nursing home quality indicators. BMC Health Serv Res. 2010;10:96. doi: 10.1186/1472-6963-10-96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wagner C, van der Wal G, Groenewegen PP, de Bakker DH. The effectiveness of quality systems in nursing homes: a review. Qual Health Care. 2001;10(4):211–217. doi: 10.1136/qhc.0100211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Spilsbury K, Hewitt C, Stirk L, Bowman C. The relationship between nurse staffing and quality of care in nursing homes: a systematic review. Int J Nurs Stud. 2011;48(6):732–750. doi: 10.1016/j.ijnurstu.2011.02.014. [DOI] [PubMed] [Google Scholar]
- 14.Netten A, Trukeschitz B, Beadle-Brown J, Forder J, Towers AM, Welch E. Quality of life outcomes for residents and quality ratings of care homes: is there a relationship? Age Ageing. 2012;41(4):512–517. doi: 10.1093/ageing/afs050. [DOI] [PubMed] [Google Scholar]
- 15.Gladman JR, Bowman CE. Quality of care and the quality of life in care homes. Age Ageing. 2012;41(4):426–427. doi: 10.1093/ageing/afs080. [DOI] [PubMed] [Google Scholar]
- 16.Elia M, Zellipour L, Stratton RJ. To screen or not to screen for adult malnutrition? Clin Nutr. 2005;24(6):867–884. doi: 10.1016/j.clnu.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 17.Bell CL, Lee AS, Tamura BK. Malnutrition in the nursing home. Curr Opin Clin Nutr Metab Care. 2015;18(1):17–23. doi: 10.1097/MCO.0000000000000130. [DOI] [PubMed] [Google Scholar]
- 18.Arvanitakis M, Coppens P, Doughan L, Van Gossum A. Nutrition in care homes and home care: recommendations - a summary based on the report approved by the Council of Europe. Clin Nutr. 2009;28(5):492–496. doi: 10.1016/j.clnu.2009.07.011. [DOI] [PubMed] [Google Scholar]
- 19.Brotherton A, Simmonds N, Stroud M. Malnutrition Matters Meeting Quality Standards in Nutritional Care. British Association for Parenteral and Enteral Nutrition (BAPEN). 2010;
- 20.Meijers JM, Halfens RJ, Wilson L, Schols JM. Estimating the costs associated with malnutrition in Dutch nursing homes. Clin Nutr. 2012;31(1):65–68. doi: 10.1016/j.clnu.2011.08.009. [DOI] [PubMed] [Google Scholar]
- 21.Porter Starr KN, McDonald SR, Bales CW. Nutritional Vulnerability in Older Adults: A Continuum of Concerns. Curr Nutr Rep. 2015;4(2):176–184. doi: 10.1007/s13668-015-0118-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tamura BK, Bell CL, Masaki KH, Amella EJ. Factors associated with weight loss, low BMI, and malnutrition among nursing home patients: a systematic review of the literature. J Am Med Dir Assoc. 2013;14(9):649–655. doi: 10.1016/j.jamda.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 23.Wagner C, Ikkink K, van der Wal G, Spreeuwenberg P, de Bakker DH, Groenewegen PP. Quality management systems and clinical outcomes in Dutch nursing homes. Health Policy. 2006;75(2):230–240. doi: 10.1016/j.healthpol.2005.03.010. [DOI] [PubMed] [Google Scholar]
- 24.Simmons SF, Garcia ET, Cadogan MP, Al-Samarrai NR, Levy-Storms LF, Osterweil D, et al. The minimum data set weight-loss quality indicator: does it reflect differences in care processes related to weight loss? J Am Geriatr Soc. 2003;51(10):1410–1418. doi: 10.1046/j.1532-5415.2003.51459.x. [DOI] [PubMed] [Google Scholar]
- 25.Schulz E. Quality Assurance Policies and Indicators for Long-Term Care in the European Union Country Report: Germany. ENEPRI Research Report No. 104, Work Package 5, 2012.
- 26.Cefalu C. Nursing home quality measures: do they accurately reflect quality? Annals of Long Term Care. 2011;19(9):33–36. [Google Scholar]
- 27.Hjaltadóttir I, Ekwall AK, Nyberg P, Hallberg IR. Quality of care in Icelandic nursing homes measured with Minimum Data Set quality indicators: retrospective analysis of nursing home data over 7 years. Int J Nurs Stud. 2012;49(11):1342–1353. doi: 10.1016/j.ijnurstu.2012.06.004. [DOI] [PubMed] [Google Scholar]
- 28.Simmons SF, Schnelle JF. A continuous quality improvement pilot study: impact on nutritional care quality. J Am Med Dir Assoc. 2006;7(8):480–485. doi: 10.1016/j.jamda.2006.03.002. [DOI] [PubMed] [Google Scholar]
- 29.Rantz MJ, Cheshire D, Flesner M, Petroski GF, Hicks L, Alexander G, et al. Helping nursing homes “at risk” for quality problems: a statewide evaluation. Geriatr Nurs. 2009;30(4):238–249. doi: 10.1016/j.gerinurse.2008.09.003. [DOI] [PubMed] [Google Scholar]
- 30.Moore KJ, Doyle CJ, Dunning TL, Hague AT, Lloyd LA, Bourke J, et al. Public sector residential aged care: identifying novel associations between quality indicators and other demographic and health-related factors. Aust Health Rev. 2014;38(3):325–331. doi: 10.1071/AH13184. [DOI] [PubMed] [Google Scholar]
- 31.Schönherr S, Halfens RJ, Meijers JM, Schols JM, Lohrmann C. Structural and process indicators of nutritional care: a comparison between Austrian hospitals and nursing homes. Nutrition. 2012;28(9):868–873. doi: 10.1016/j.nut.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 32.van Nie-Visser NC, Meijers JM, Schols JM, Lohrmann C, Bartholomeyczik S, Halfens RJ. Comparing quality of nutritional care in Dutch and German nursing homes. J Clin Nurs. 2011;20(17-18):2501–2508. doi: 10.1111/j.1365-2702.2011.03761.x. [DOI] [PubMed] [Google Scholar]
- 33.van Nie-Visser NC, Meijers J, Schols J, Lohrmann C, Bartholomeyczik S, Spreeuwenberg M, et al. Which characteristics of nursing home residents influence differences in malnutrition prevalence? An international comparison of The Netherlands, Germany and Austria. Br J Nutr. 2014;111(6):1129–1136. doi: 10.1017/S0007114513003541. [DOI] [PubMed] [Google Scholar]
- 34.Bonaccorsi G, Collini F, Castagnoli M, Di Bari M, Cavallini MC, Zaffarana N, et al. A cross-sectional survey to investigate the quality of care in Tuscan (Italy) nursing homes: the structural, process and outcome indicators of nutritional care. BMC Health Serv Res. 2015;15:223. doi: 10.1186/s12913-015-0881-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Meijers JM, Tan F, Schols JM, Halfens RJ. Nutritional care; do process and structure indicators influence malnutrition prevalence over time? Clin Nutr. 2014;33(3):459–465. doi: 10.1016/j.clnu.2013.06.015. [DOI] [PubMed] [Google Scholar]
- 36.van Nie NC, Meijers JM, Schols JM, Lohrmann C, Spreeuwenberg M, Halfens RJ. Do structural quality indicators of nutritional care influence malnutrition prevalence in Dutch, German, and Austrian nursing homes? Nutrition. 2014;30(11-12):1384–1390. doi: 10.1016/j.nut.2014.04.015. [DOI] [PubMed] [Google Scholar]
- 37.van Nie-Visser NC, Meijers JM, Schols JM, Lohrmann C, Spreeuwenberg M, Halfens RJ. To what extend do structural quality indicators of (nutritional) care influence malnutrition prevalence in nursing homes? Clin Nutr. 2015;34(6):1172–1176. doi: 10.1016/j.clnu.2014.12.003. [DOI] [PubMed] [Google Scholar]
- 38.Dyck MJ. Nursing staffing and resident outcomes in nursing homes: weight loss and dehydration. J Nurs Care Qual. 2007;22(1):59–65. doi: 10.1097/00001786-200701000-00012. [DOI] [PubMed] [Google Scholar]
- 39.Hurtado DA, Berkman LF, Buxton OM, Okechukwu CA. Schedule Control and Nursing Home Quality: Exploratory Evidence of a Psychosocial Predictor of Resident Care. J Appl Gerontol. 2016;35(2):244–253. doi: 10.1177/0733464814546895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lee HY, Blegen MA, Harrington C. The effects of RN staffing hours on nursing home quality: a two-stage model. Int J Nurs Stud. 2014;51(3):409–417. doi: 10.1016/j.ijnurstu.2013.10.007. [DOI] [PubMed] [Google Scholar]
- 41.Shin JH, Hyun TK. Nurse Staffing and Quality of Care of Nursing Home Residents in Korea. J Nurs Scholarsh. 2015;47(6):555–564. doi: 10.1111/jnu.12166. [DOI] [PubMed] [Google Scholar]
- 42.Werner RM, Konetzka RT, Kim MM. Quality improvement under nursing home compare: the association between changes in process and outcome measures. Med Care. 2013;51(7):582–588. doi: 10.1097/MLR.0b013e31828dbae4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Simmons SF, Bertrand R, Shier V, Sweetland R, Moore TJ, Hurd DT, et al. A preliminary evaluation of the paid feeding assistant regulation: impact on feeding assistance care process quality in nursing homes. Gerontologist. 2007;47(2):184–192. doi: 10.1093/geront/47.2.184. [DOI] [PubMed] [Google Scholar]
- 44.Arling G, Kane RL, Lewis T, Mueller C. Future development of nursing home quality indicators. Gerontologist. 2005;45(2):147–156. doi: 10.1093/geront/45.2.147. [DOI] [PubMed] [Google Scholar]
- 45.Hutchinson AM, Milke DL, Maisey S, Johnson C, Squires JE, Teare G, Estabrooks CA. The Resident Assessment Instrument-Minimum Data Set 2.0 quality indicators: a systematic review. BMC Health Serv Res. 2010;10:166. doi: 10.1186/1472-6963-10-166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Shin JH, Bae SH. Nurse staffing, quality of care, and quality of life in US nursing homes, 1996–2011: an integrative review. J Gerontol Nurs. 2012;38(12):46–53. doi: 10.3928/00989134-20121106-04. [DOI] [PubMed] [Google Scholar]
- 47.Arling G, Karon SL, Sainfort F, Zimmerman DR, Ross R. Risk adjustment of nursing home quality indicators. Gerontologist. 1997;37(6):757–766. doi: 10.1093/geront/37.6.757. [DOI] [PubMed] [Google Scholar]
- 48.Moty C, Barberger-Gateau P, De Sarasqueta AM, Teare GF, Henrard JC. Risk adjustment of quality indicators in French long term care facilities for elderly people. A preliminary study. Rev Epidemiol Sante Publique. 2003;51(3):327–338. [PubMed] [Google Scholar]
- 49.Mukamel DB, Glance LG, Li Y, Weimer DL, Spector WD, Zinn JS, et al. Does risk adjustment of the CMS quality measures for nursing homes matter? Med Care. 2008;46(5):532–541. doi: 10.1097/MLR.0b013e31816099c5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Arling G, Lewis T, Kane RL, Mueller C, Flood S. Improving quality assessment through multilevel modeling: the case of nursing home compare. Health Serv Res. 2007;42(3 Pt 1):1177–1199. doi: 10.1111/j.1475-6773.2006.00647.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Li Y, Cai X, Glance LG, Spector WD, Mukamel DB. National release of the nursing home quality report cards: implications of statistical methodology for risk adjustment. Health Serv Res. 2009;44(1):79–102. doi: 10.1111/j.1475-6773.2008.00910.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li Y, Schnelle J, Spector WD, Glance LG, Mukamel DB. The “Nursing Home Compare” measure of urinary/fecal incontinence: cross-sectional variation, stability over time, and the impact of case mix. Health Serv Res. 2010;45(1):79–97. doi: 10.1111/j.1475-6773.2009.01061.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Harris Y, Clauser SB. Achieving improvement through nursing home quality measurement. Health Care Financ Rev. 2002;23(4):5–18. [PMC free article] [PubMed] [Google Scholar]
- 54.Rothman KJ, Greenland S, Lash T. Modern Epidemiology. 3. Philadelphia: Lippincott Williams & Wilkins; 2008. [Google Scholar]
- 55.Grimes DA, Schulz KF. Descriptive studies: what they can and cannot do. Lancet. 2002;359:145–149. doi: 10.1016/S0140-6736(02)07373-7. [DOI] [PubMed] [Google Scholar]
- 56.Rothman KJ. Six persistent research misconceptions. J Gen Intern Med. 2014;29(7):1060–1064. doi: 10.1007/s11606-013-2755-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Meijers JM, Halfens RJ, van Bokhorst-de van der Schueren MA, Dassen T, Schols JM. Malnutrition in Dutch health care: prevalence, prevention, treatment, and quality indicators. Nutrition. 2009;25(5):512–519. doi: 10.1016/j.nut.2008.11.004. [DOI] [PubMed] [Google Scholar]
- 58.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009;6(6):e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Halfens RJ, Meesterberends E, van Nie-Visser NC, Lohrmann C, Schönherr S, Meijers JM, et al. International prevalence measurement of care problems: results. J Adv Nurs. 2013;69(9):e5–17. doi: 10.1111/jan.12189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not applicable.


