Abstract
Background
Adolescent pregnancy has been persistently high in sub-Saharan Africa. The objective of this review is to identify factors influencing adolescent pregnancies in sub-Saharan Africa in order to design appropriate intervention program.
Methods
A search in MEDLINE, Scopus, Web of science, and Google Scholar databases with the following keywords: determinants, factors, reasons, sociocultural factors, adolescent pregnancy, unintended pregnancies, and sub- Saharan Africa. Qualitative and cross-sectional studies intended to assess factors influencing adolescent pregnancies as the primary outcome variable in sub- Saharan Africa were included. Our search was limited to, articles published from the year 2000 to 2017 in English. Twenty-four (24) original articles met the inclusion criteria.
Results
The study identified Sociocultural, environmental and Economic factors (Peer influence, unwanted sexual advances from adult males, coercive sexual relations, unequal gender power relations, poverty, religion, early marriage, lack of parental counseling and guidance, parental neglect, absence of affordable or free education, lack of comprehensive sexuality education, non-use of contraceptives, male’s responsibility to buy condoms, early sexual debut and inappropriate forms of recreation). Individual factors (excessive use of alcohol, substance abuse, educational status, low self-esteem, and inability to resist sexual temptation, curiosity, and cell phone usage). Health service-related factors (cost of contraceptives, Inadequate and unskilled health workers, long waiting time and lack of privacy at clinics, lack of comprehensive sexuality education, misconceptions about contraceptives, and non-friendly adolescent reproductive services,) as influencing adolescent pregnancies in Sub-Saharan Africa
Conclusion
High levels of adolescent pregnancies in Sub-Saharan Africa is attributable to multiple factors. Our study, however, categorized these factors into three major themes; sociocultural and economic, individual, and health service related factors as influencing adolescent pregnancies. Community sensitization, comprehensive sexuality education and ensuring girls enroll and stay in schools could reduce adolescent pregnancy rates. Also, provision of adolescent-friendly health services in schools and healthcare centers and initiating adolescent empowerment programs could have a positive impact.
Keywords: Adolescent pregnancy, Determinants, Sub-Saharan Africa
Plain English summary
Adolescent pregnancies have been persistently high in sub-Saharan Africa. This study seeks to identify factors influencing adolescent pregnancies in sub-Saharan Africa through a systematic review of published scientific articles.
A total of two hundred and twenty nine (229) original articles published between 2000 and 2017 were first identified from various data bases. Finally, twenty-four (24) original articles met the inclusion criteria and were included in the study. All articles were studies conducted in sub-Saharan Africa.
The study identified Sociocultural, environmental and Economic factors (Peer influence, unwanted sexual advances from adult males, coercive sexual relations, unequal gender power relations, poverty, religion, early marriage, lack of parental counseling and guidance, parental neglect, absence of affordable or free education, lack of comprehensive sexuality education, non-use of contraceptives, male’s responsibility to buy condoms, early sexual debut and inappropriate forms of recreation). Individual factors (excessive use of alcohol, substance abuse, educational status, low self-esteem, and inability to resist sexual temptation, curiosity, and cell phone usage). Health service-related factors (cost of contraceptives, Inadequate and unskilled health workers, long waiting time and lack of privacy at clinics, lack of comprehensive sexuality education, misconceptions about contraceptives, and non-friendly adolescent reproductive services,) as influencing adolescent pregnancies in Sub-Saharan Africa.
We believe that Community sensitization, sex education and ensuring girls enrol and stay in schools could reduce adolescent pregnancy rates. Also, provision of adolescent friendly health services at schools and initiating adolescent empowerment programs could have positive impact.
Background
The long-lived belief in the African society where females were not prioritized for education is fading out. With this, it expected that female education will increase in sub-Saharan Africa [1]. Unfortunately, adolescent pregnancy contributes to denying brilliant students education and has potential to retard their growth and development including that of their children.
According to WHO about 17 million adolescent girls give birth every year and most of these births occur in low- and middle-income countries [2]. Adolescent health and development are of global concern. The need to prevent early pregnancy among adolescent girls in Sub-Saharan Africa has been recognized increasingly over recent years [3]. African countries lead the world in teen pregnancies: With Niger on the top list of 203.604 births per 100,000 teenage women. Mali follows with 175.4438, Angola (166.6028), Mozambique (142.5334), Guinea (141.6722), Chad (137.173), Malawi (136.972), and Cote d’Ivoire (135.464) [4].
Adolescent girls continue to experience the disproportionately high burden of sexual and reproductive ill health, particularly in Sub-Saharan Africa [3]. High adolescent pregnancies with adverse health and social consequences are urgent problems facing low- and middle-income countries [2]. Adolescents are likely to have complications of pregnancy including unsafe abortion and more likely to become young mothers a second time [2, 5, 6]. Their infants are also more likely to be born premature and to die in the perinatal period [7]. Babies born to adolescent mothers face a substantially higher risk of dying than those born to women aged 20 to 24 [2, 5, 8]. They are at risk of malnutrition, low mental and physical development, inappropriate social connection with parents and poor education [5, 9].
Adolescents develop psychological problems from social stigma, suffer physical and domestic violence in their attempt to meet the demands of pregnancy and childbearing [9, 10]. Also, they most likely would drop out and may not get the chance to return to school [11]. The inadequate resources of low and middle-income countries would have to be channeled to cater for the health needs of pregnant and teen mothers including their children [5]. Economic opportunities are limited to adolescents who could not complete school because of unintended pregnancies. This could be the beginning of a poverty cycle in families, however, some are able to face the challenge and become productive later in life.
Factors associated with unintended pregnancies amongst adolescents are early marriages, culture, religion, gender [12], poor social and economic support [13, 14]. Curiosity and peer pressure [15, 16], lack of comprehensive sexuality education [17–19], poor reproductive health services provision [19, 20], poor attitude of health workers to providing contraceptive services for adolescents [15, 21]. Also, unmet need for contraceptives by adolescents [22] and fear of contraceptive side effects [16]. Barriers to contraceptive use among adolescents include inadequate sexual knowledge and risk perceptions. Also, lack of skills and power to negotiate safer sex options, ambivalence towards sex, and negative social norms around premarital sexual activity and pregnancy [23].
Policy makers in Sub-Saharan Africa need to understand the determinants of adolescent pregnancy in their context in order to design pragmatic interventional programs to reduce unintended pregnancies amongst adolescents. Since there has not been any review of literature on the determinants of adolescent pregnancy in Sub-Saharan Africa, this study aims to identify the determinants of high adolescent pregnancy in Sub-Saharan Africa.
Methods
Search strategy
MEDLINE, Scopus, web of science and Google Scholar databases were searched in July 2017 with the following keywords: determinants, factors, reasons, sociocultural factors, adolescent pregnancy, unintended pregnancies, and sub- Saharan Africa. Qualitative and cross-sectional studies intended to assess the factors influencing adolescent pregnancies either intended or unintended as the primary outcome variable in sub- Saharan Africa was included. Our search was limited to articles published in English from 2000 to 2017.
Inclusion and exclusion criteria
Qualitative and cross-sectional studies that assessed the factors associated with adolescent pregnancy, conducted in sub-Saharan Africa, whether the pregnancy was intended or not, from the year 2000 to 2017 were included. Studies that addressed factors associated with adolescent pregnancy, yet conducted outside Sub-Saharan Africa were excluded from the study.
Identification of reviews
A search framework was constructed and implemented through a broad scope and exhaustive search using Tehran University of Medical Sciences electronic library to identify applicable studies published in English. The search identified a total of 229 articles, which composed of 244 original research articles and 5 review articles. After the screening of titles and abstracts, 54 articles were excluded because they did not address adolescent pregnancy. Articles that addressed adolescent pregnancy were 170 and 5 reviews. All the review articles were excluded because 3 were conducted outside the study setting, and the other 2 did not assess the determinants of adolescent pregnancy. With the rest of the articles, 40 did not assess determinants of adolescent pregnancy, 16 were conducted before the year 2000, 56 were not full text and 34 were duplicated. Therefore, 24 research articles were sieved and included in the study. Figure 1 demonstrates articles selection criterion.
Fig. 1.
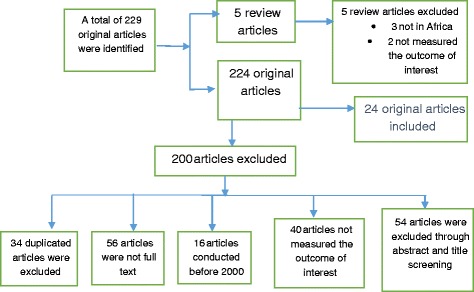
Inclusion and exclusion criteria
Variables assessed
The main variables assessed were age, lack of money, lack of family support, the culture of not talking about sex at home, peer influence, broken homes, early marriages, and religion. Service-related factors such as lack of adolescent-friendly services, inadequate comprehensive sexuality education, non-availability and cost of contraceptives, inadequate health personnel, judgmental attitude of service providers and inadequate counseling. Personal behavioral factors such as alcohol and tobacco use, fear of stigma and being judged by the service provider, low self-efficacy, low self-esteem, vulnerability and rape, curiosity, inadequate education and knowledge about contraceptives.
Articles appraisal
The Joanna Briggs appraisal tool [24] was used independently by the authors to appraise and certify for inclusion or exclusion of articles. Both authors, before inclusion, reached consensus. The tool consists of a checklist of ten questions for qualitative studies, eight for cross-sectional studies and 11 for systematic reviews and research syntheses.
Strengths of the study
The study has revealed, through a comprehensive search the determinants of adolescent pregnancy in Sub-Saharan Africa. The results of the study are similar to global reports [25]. In addition, the study revealed a gap in research regarding literature on determinants of adolescent pregnancy in the five sub-Saharan Africa countries with the highest rates [4].
Weaknesses of the study
Diverse disciplines deal with adolescents and adolescent pregnancies; this makes it possible to miss some articles during the search process since their findings may not be published in scientific based journals which were our main source of data. Secondly, grey literature, reports, and unpublished studies were not included in this review. In addition, some articles reported findings from small sample sizes.
Operational definition of concepts
Adolescent reproductive services
Healthcare services offered to assist adolescents access sexual and reproductive health information.
Comprehensive sexuality education
Teaching abstinence as the best method for avoiding unintended pregnancy, but also teaching about condoms and contraception to reduce the risk of unintended pregnancy. It also involves empowering adolescents to resist sexual temptations and peer pressure.
Curiosity
A strong desire to discover new things, especially about sex and relationships.
Early marriage
Union between two people in which one or both parties are younger than 18 years of age:
Early sexual debut
Having had first sexual intercourse at or before age 14.
Excessive use of alcohol
Uncontrolled and widespread alcohol usage.
Family dysfunction
Unhealthy interactions, conflict, misbehaviour, and child neglect of parents.
Gender power relations
The culturally determined social status of men and women in relationships.
Inability to resist sexual temptation
Inability to avoid or say no to sexual desires and pressure from both internal and external sources, and acting on it.
Inappropriate recreation
Recreational activities, which creates a risky sexual environment e.g. disco dances, clubbing etc.
Low self-esteem
Lacking self-confidence to turn down sexual advances from men.
Peer influence
Social pressure by members of one’s peer group to take a certain action, adopt certain values, or otherwise conform in order to be accepted.
Positive attitude towards early sexual relationships
Having a good feeling or emotion towards early sexual relationships.
Religion
A system of faith and worship.
Sexual advances
Purposeful visual, verbal or physical conduct of a sexual nature.
Substance abuse
Excessive and uncontrolled use of illicit and addictive substances such as tobacco, marijuana.
Results
Articles included in this review were studies conducted in Sub-Saharan African countries with a focus on adolescent pregnancies.
Out of 24 articles, eight (8) were qualitative research [19, 23, 26–31], 15 were cross-sectional studies [15, 32–45], and one article used mixed method [46] (Table 1).
Table 1.
Main determinants of unintended pregnancy amongst adolescents
| Title | Year/country | Study type | Determinants of adolescent pregnancy |
|---|---|---|---|
| Understanding sexual and reproductive health needs of adolescents: evidence from a formative evaluation in Wakiso district, Uganda | 2015 Uganda | Qualitative study | Sexual advances from adult males, rape, defilement, alcohol, marijuana, lack of youth counsellors, lack of sex education, inadequate education on family planning, cost of contraceptives, inadequate health workers and fear of stigma in seeking help form health workers. |
| Barriers to access reproductive healthcare for pregnant adolescent girls: a qualitative study in Tanzania | 2015 Tanzania | Qualitative study | They viewed condoms as ineffective for preventing STIs and pregnancies and unnecessary for those in committed relationships. Stigma and long waiting times. Lack of privacy in the clinics discouraged young females from seeking reproductive healthcare, lack of privacy, unkind health care workers |
| Relationship dynamics and teenage pregnancy in South Africa | 2001 south Africa | Exploratory study | Forced sexual initiation, unwillingness to confront unfaithful partner, partners of adolescents were older, unequal power relations, living in extended family, non-use of contraceptives, peer influence, and curiosity. |
| Who’s that girl? A qualitative analysis of adolescent girls’ views on factors associated with teenage pregnancies in Bolgatanga, Ghana | 2016 Ghana. | Qualitative study | Material gain, positive attitude towards relationship, early sexual debut, peer influence, most parents don’t talk about safe sex with their children, male should be responsible to buy condoms, fear of ridicule, misconceptions about family planning, inability to resist temptation, |
| Gendered norms, sexual exploitation and adolescent pregnancy in rural Tanzania | 2013, Tanzania | Qualitative study | Poverty, inability to exercise control over sexual decisions, adolescents sexual relationship with older men, early marriage, sexual expectations from men, rape, coerced sex |
| Adolescent pregnancy and associated factors in South African youth | 2012 south Africa | Cross sectional study | Unemployment, poverty, high sexual permissive attitude, contraceptive use, didn’t understand the risk of pregnancy, to prove their maturity, unequal power in relationship |
| Family and community support to adolescent mothers in Swaziland | 2003 Swaziland | Mixed method | Peer influence, lack of sexual and reproductive information from families and communities |
| Factors influencing the adolescent pregnancy rate in the Greater Giyani Municipality, Limpopo Province – South Africa | 2015 south Africa | Descriptive and explorative survey | Inconvenient health services, poor relationship with health workers, peer pressure, inadequate sexual knowledge, changing attitude toward sex. |
| Determinants of Sexual Activity and Pregnancy among Unmarried Young Women in Urban Kenya: A Cross-Sectional Study | 2015 Kenya | Cross-Sectional Study | Education level, religion, employment status, household size, family planning knowledge, misconceptions, and early sexual debut. |
| Unmet social needs and teenage pregnancy in Ogbomosho, South-western Nigeria | 2014 Nigeria | Cross-Sectional Study | The unmet material and financial supports expected from parents, the lack of free education from government up until secondary school level, the lack of sex education and knowledge needs for signs of maturity, and discouragement from friends not to have boyfriend. |
| Adolescent girls, illegal abortions and “sugar-daddies” in Dar es Salaam: vulnerable victims and active social agents | 2001 Tanzania | Qualitative study | Material benefits from men, high-risk sexual activity, lack of family planning information, sex education and poor health services. |
| Teenage pregnancy experiences in rural Kenya | 2003 Kenya | Community based survey | Sexual active adolescents, unmet reproductive health needs, education level of adolescents |
| Health workers’ attitudes toward sexual and reproductive health services for unmarried adolescents in Ethiopia | 2012 Ethiopia | descriptive cross-sectional survey | Negative attitude of health workers towards providing RH services to unmarried adolescents, low education of health workers, and lack of training on RH services. |
| Nurse-Midwives’ Attitudes towards Adolescent Sexual and Reproductive Health Needs in Kenya and Zambia | 2006 Kenyan and Zambia | cross-sectional survey | Negative attitudes of health workers towards adolescent sexual activity, contraceptive use and seeking reproductive health services. |
| Determinants of teenage pregnancies: The case of Busia District in Kenya | 2007 Kenya | Cross sectional survey | Level of education, sex education, peer pressure, inappropriate form of recreation, lack of parental guidance and counselling, poverty, knowledge of contraception. |
| Blood Blockages and Scolding Nurses: Barriers to Adolescent Contraceptive Use in South Africa | 2006 south Africa | Qualitative study | Pressure from male partners, fears about the effects of contraception, health workers attempt to stigmatize teenage sexuality, scolding and hash treatment of adolescents, unwillingness to acknowledge adolescent experience as contraceptive users. |
| A participatory action research approach to developing youth-friendly strategies for the prevention of teenage pregnancy | 2016 South Africa | participatory action research approach | Sexual curiosity, alcohol consumption, unprotected sex, peer influence, lack of family support, parental absence, low family socioeconomic status, gender power inequality, relationship with elder men, lack of youth-friendly clinics |
| Socio-Cultural Determinants of Contraceptives Use Among Adolescents in Northern Ghana | 2015 Ghana | Descriptive cross-sectional study | Early sexual debut, educational level, parental neglect, money, curiosity, peer pressure |
| Predictors of Sexual Debut Among Young Adolescents in Nairobi’s Informal Settlements | 2014 kenya | Descriptive cross-sectional study | School dropout, education, severe family dysfunction, lack of parental control. |
| Early Pregnancy of Junior High School Girls: Causes and Implications on Academic Progression in the Talensi District of the Upper East Region Of Ghana | 2015 Ghana | Cross-sectional study | Cell phone usage by teenagers, inadequate contraceptives, peer group influence, family neglect and poverty, peer group influence, lack of sex education. |
| Teenage Pregnancy in the Builsa District: A Focus Study in Fumbisi. | 2013 Ghana | Cross-sectional study | Poverty, prostitution, inadequate sex education, inadequate family support. |
| The cause and effect of teenage pregnancy: case of kontagora local government area in niger state, northern part of nigeria | 2013 Nigeria. | Cross-sectional study | Early sexual debut, socio-economic background, early marriage and traditional gender roles, peer pressure, lack of sex education and non-used of contraceptive during sexual intercourse. |
| Poverty the Cause of Teenage Pregnancy in Thulamela Municipality | 2015 south Africa | Cross-sectional study | Poverty, low socio-economic family status, lack of parental support, inadequate sex education from parents, peer influence. |
| The Effects of Teenage Pregnancy on the Educational Attainment of Girls at Chorkor, a Suburb of Accra | 2013 Ghana | Qualitative study | Poor parenting, poverty, peer influence and school dropout. |
Participants in this study were mostly adolescents. The study settings were both rural and urban, with an approximated total population of 11,651 participants. Participants per study varied from 10 as the least to 3122 as the highest. Refer to Table 2 for a detailed description of participant’s characteristics.
Table 2.
Participants Characteristics
| Author | Study setting/country | Number of participants | Gender % (n) | Age range (years) | Ethnicity | Socio-economic status | Marital status |
|---|---|---|---|---|---|---|---|
| Atuyambe et al. (2015) [19] | Wakiso district/Uganda | 156 | Females 50.6% (79), Males 49.4% (77) | 10--19 | not described | No employment status described | not indicated |
| Hokororo et al. (2015) [27] | Mwanza region/Tanzania | 49 | Females 100% (49) | 15-20 | Sukuma tribe | Non was employed | Legally married (2) Living with partner/boyfriend (40) Single or not living with partners (7) |
| R. Jewkes et al. (2001) [35] | Gugulethu and Khayelitsha, Cape Town/South Africa | 544 | Females 100% (544) | below 19 years | not described | No employment status described | not indicated |
| Krugu et al. (2016) [23] | Bolgatanga Municipality/Ghana | 20 | Females 100% (20) | 14-19 | not described | High school students | non was married |
| McCleary-Sills et al. (2013) [28] | Tanzania | 82 | Females 100% (82) | 12--17 | not described | No employment status described | not indicated |
| G. Mchunu et al. (2012) [38] | Eastern Cape, Gauteng, KwaZulu-Natal and Mpumalanga/ South Africa | 3123 | Female 45.4% (1418), Males 54.6% (1705) | 18-24 | not described | No employment status described | not indicated |
| P.T. Mngadi et al. (2003) [46] | Mbabane/Swaziland | 31 | Females 100% (31) | 15-19 | not described | Non was employed | not indicated |
| Mushwana et al. (2015) [15] | Greater Giyani Municipality/South Africa | 147 | Females 100% (147) | 10--19 | not described | No employment status described | Married (5), Single (136), Other (4) |
| Okigbo & Speizer (2015) [40] | Nairobi,Mombasa,Kisumu,Machakos, Kakamega/Kenya | 2020 | Female 100% (2020) | 15-24 | not described | Not employed 467, Student 658, Employed 895 | non has ever been married |
| Salami et al. (2014) [41] | Ogbomosho, Oyo State/Nigeria | participants 174, key informants 12 | Females 100% (174 + 12) | 10-20 and above | not described | Not employed 34, Student 62, Trading 45, Others 33 | not indicated |
| Silberschmidt & Rasch (2001) [29] | Dar es Salaam/Tanzania | 51 | Females 100% (51) | 15-19 | Not specific | Students 25, Employed 26 | non was married |
| Taffa et al. (2003) [42] | Nyanza region/Kenya | 1247 | Females 100% (1247) | 12--19 | Not specific | students 233, not in school 331 | married or co-habiting (253), not married (331) |
| Tilahun et al. (2012) [43] | Eastern Hararghe, Oromia region/Ethiopia | 394 | Females 301 (301), Males 23.6% (93) | 18-24 (219), 25-35 (143), 36 and above [32] | Oromiffa | Nurses (119), Health Extension Workers (236), Health Assistants [21] | Married (245), Single (149) |
| Warenius et al. (2006) [44] | Kenya and Zambia | 707 | Females 92% (651), Male 8% (56) | 22-60 | Not specific | Enrolled Nurses (502), Registred Nurses (200), Dispensary Techs [5] | not indicated |
| M. Were (2007) [45] | Busia District/Kenya | 258 | Females 78.7% (203), Male 21.3% (55) | 10--19 | not described | No employment status described | not indicated |
| K Wood & R Jewkes (2006) [30] | Limpopo Province/South Africa | 35 | Females 100% (35) | 14-20 | Not specific | No employment status described | non was married |
| L. Wooda & F. Hendricks (2016) [31] | South Africa | 24 | Females 58.3% (14) Males 41.7% (10) | Below 18 years | not described | grade 11 learners | not indicated |
| A. Yidana et al. (2015) [32] | Yendi Municipality /Ghana | 400 | Females 62.8% (251), Males 37.3% (149) | 14-19 | Dagomba | No employment status described | Cohabiting (19), Divorced (1), Married (76), Single (292), Widowed (12) |
| M. Marston et al. (2013) [37] | Korogocho and Viwandani/Kenya | 1754 | 12--16 | Swahili | No employment status described | not indicated | |
| E. Alhassan (2015) [34] | Talensi District/Ghana | 310 | Females 100% (310) | not specific | Telensi | Junior High School Students | not indicated |
| S. P. Adzitey et al. (2013) [33] | Fumbisi, Builsa District/Ghana | 20 | Females 100% (20) | 14-20 | Builsa (65%), Kasena (15%), Mamprusi (10%), Bimoba (5%) and Sisala (5%) | Students (95%), No education (5%) | Married (19), Single (1) |
| Ogori et al. (2013) [39] | Kontagora LocalGovernment Area, Niger State/Nigeria | 40 | Not specific | Not specific | Not specific | No employment status described | not indicated |
| Lambani M.N (2015) [36] | Limpopo Province/South Africa | 10 | Females 10% (10) | 17-18 | not described | Non was employed | not indicated |
| Gyan C. (2013) [26] | Chorkor, Greater Accra Region/Ghana | 55 | Females 100% (55) | not specific | Ga-Dangme and Akan | No employment status described | not indicated |
At least 12 key informants composed of parents, school teachers, health providers, and adolescent mothers/fathers were involved in some of the included studies. They provided information regarding some of the determinants of adolescent pregnancy.
It is interesting to note that there is no published data within this review years from the top five sub-Saharan African countries with adolescent pregnancy above 140 births per 100,000 adolescents [47].
The study revealed three major themes influencing adolescent pregnancy in sub-Saharan Africa: Sociocultural, environmental and Economic, Individual, and Health-Related Factors.
Sociocultural, environmental and economic factors
Peer influence was reported by 11 studies [15, 23, 26, 31, 34–36, 39, 41, 45, 46], Unwanted sexual advances from adult males which often led to coercive sexual relations [19, 28, 31, 35]. Also, unequal gender power relations [19, 27, 28, 30, 31, 35, 38, 39], poverty [19, 23, 26, 28, 31–34, 36, 38, 41, 45], religion and early marriage [28, 39, 40]. In addition, lack of parental counseling and guidance, severe family dysfunction with parental neglect [23, 26, 31, 33–37, 40, 41, 45, 46]. The absence of affordable or free education [41]. Lack of comprehensive sexuality education, both in schools and at home with family members [15, 19, 23, 26, 29, 31, 32, 34, 36, 37, 41, 45, 46]. Lack of knowledge, misconceptions, and non-use of contraceptives [19, 23, 29, 30, 35, 38, 40, 44, 45], male’s responsibility to buy condoms [23]. Positive attitude towards early sexual relationships, and early sexual debut [14, 22, 29, 31, 37–39, 41]. Inappropriate forms of recreation [45].
Individual factors
Excessive use of alcohol and substance abuse [19, 31], educational status [26, 32, 37, 42], low self-esteem and inability to resist sexual temptation [23, 28, 30, 31, 35, 38, 39], and curiosity [31, 32, 35]. Cell phone usage by teenagers [34].
Health service-related factors
Cost of contraceptives [19]. Inadequate and unskilled health workers [19, 27, 43]. Long waiting time and lack of privacy at clinics [27], lack of comprehensive sexuality education, and misconceptions about contraceptives [15, 19, 23, 27, 29, 30, 34, 35, 38, 40, 45, 46]. Also, non-friendly adolescent reproductive services, and negative attitude of health workers towards providing reproductive health services for adolescents [15, 19, 27, 29, 43, 44].
Discussion
Sociocultural, economic, individual and health service factors were identified as the main determinants of adolescent pregnancy. These factors were found to influence high rates of adolescent pregnancy in sub-Saharan Africa, similar to the developed world [25].
A study by Fearon et al. reported peers to be influential in romantic and sexual behaviors of adolescents [48]. Their finding is consistent with the findings of this review. Studies from Ghana, Nigeria, Swaziland, Kenya, Tanzania, and South Africa reported the influence of peers in adolescent pregnancy. Particularly mentioned in a study from Nigeria [41], peers encourage their friends to get boyfriends.
Low socioeconomic status of parents makes adolescents vulnerable to unintended pregnancies since the means to afford basic needs, and sometimes contraceptives is a challenge. Some adults take advantage of this situation to provide basic needs to unsuspecting adolescents and engage in sexual relationships with them. This creates a power difference between adolescents and their adult partners making them powerless to negotiate for safer sex. The effect of this is teenage pregnancy and the spread of sexually transmitted infections. Studies from Ghana [23], South Africa [31] and Tanzania [29] demonstrate how poverty leads adolescents to engage in sexual relations with elderly men in order to meet their basic needs. Lambani [36], reported that adolescents intentionally get pregnant to receive government support intended for teenage mothers to improve their economic condition not considering the consequence of their action.
Lack of parental counseling and guidance, severe family dysfunction with parental neglect were found as risk factors for adolescent pregnancies [26, 33, 35, 40, 45]. Parental counseling and guidance improves communication between parents and adolescents and enables parents to address challenges of adolescents. Improved family communication and parent involvement in adolescents pregnancy prevention programs could delay adolescent sexual activity and pregnancy [49].
Inadequate knowledge, misconceptions and non-use of contraceptives [15, 19, 23, 26, 29, 31, 32, 34, 36, 37, 41, 45, 46] were identified as determinants of adolescent pregnancy. As indicated by Wood and Hendricks [31], health practitioners don’t relate health education to sociocultural context of adolescents but rather on bio-medical facts and warn of negative consequences. They do not as well explore their fears regarding contraception; therefore, adolescents do not feel the impact of comprehensive sexuality education. Uninformed adolescents perceive contraceptives as a reserve for married couples [29].
Inappropriate modes of recreation in the form of unmonitored nightclubs or mixed-sex partying. These expose adolescents to early sex since they socialize easily with men [45].
We found the positive attitude towards early sexual relationship and early sexual debut as factors contributing to adolescent pregnancy, consistent with findings from some developed countries [50–52]. The participants mostly lived in a social environment where adolescents had free will to choose sexual partners at an early age without much criticism from parents, caregivers, and peers [23]. In other reports, adolescents intentionally became pregnant as proof of love and commitment to their sexual partners [30].
Religion and early marriages were also found to contribute to high reports of adolescent pregnancies, which is consistent with a study by Parsons et al. [53]. Adolescents affected by early marriages are deprived of economic empowerment and self-efficacy and are at risk of early pregnancies [3]. They are also prone to maternal morbidity and mortality [54]. WHO’s guidelines on prevention of unintended pregnancy stressed on policies to reduce early marriage [6]. Rape, coerced sex, sexual advances from adult men and unequal gender power in relationships identified in this review, undermines adolescents’ decision-making ability to either reject sex or negotiate the use of contraceptives [55].
Individual factors that influence adolescent pregnancies include excessive use of alcohol and substance abuse. This behavior makes adolescent girls vulnerable, and an easy target for sexual exploits. This is consistent with previous findings which reported an association between high-risk sexual behavior, adolescent pregnancy and substance abuse [56]. Cell phone usage promotes easy communication among peers and their partners and also gives them easy access to the internet which they use without regulation, to surf explicit content motivating early sex [34].
Health service-related factors include the cost of contraceptives [19], healthcare centers lacking the adequate and skilled staff to attend to adolescents who need reproductive health services [19, 27, 43]. Long waiting time and lack of privacy at clinics discourage adolescents from visiting the facilities for services [27]. Also, inadequate comprehensive sexuality education and misconceptions about contraceptives [15, 19, 23, 27, 29, 30, 34, 35, 38, 40, 45, 46] were identified. Similarly, lack of friendly adolescent reproductive services and negative attitude of health workers towards providing reproductive health services for adolescents [15, 19, 27, 29, 43, 44] were all associated with adolescent pregnancy.
Conclusion
High levels of adolescent pregnancies in Sub-Saharan Africa is attributable to multiple factors. Our study, however, categorized these factors into three major themes; Sociocultural, environmental and Economic factors (Peer influence, unwanted sexual advances from adult males, coercive sexual relations, unequal gender power relations, poverty, religion, early marriage. In addition, lack of parental counseling and guidance, parental neglect, the absence of affordable or free education, lack of comprehensive sexuality education, misconceptions, and non-use of contraceptives, male’s responsibility to buy condoms, positive attitude towards early sexual relationships, early sexual debut and inappropriate forms of recreation). Individual factors (excessive use of alcohol, substance abuse, educational status, low self-esteem, and inability to resist sexual temptation, curiosity, and cell phone usage). Health service-related factors (cost of contraceptives, Inadequate and unskilled health workers, long waiting time and lack of privacy at clinics, lack of comprehensive sexuality education, misconceptions about contraceptives, non-friendly adolescent reproductive services, and negative attitude of health workers towards providing reproductive health services for adolescents) as influencing adolescent pregnancies.
Seemingly unique to sub-Saharan Africa, our study found determinants of adolescent pregnancy to be associated with religious factors, early marriages, low level of education, and poverty. Also, cost of contraceptives, lack of adolescent-friendly health service provision, inadequate and unskilled health workers, and lack of comprehensive sexuality education.
Policymakers and opinion leaders should focus on community sensitization, comprehensive sexuality education and ensure girls enroll and stay in schools. Also, peers and significant others should be involved in designing interventional programs for adolescent pregnancy prevention. This could reduce adolescent pregnancy rates. Moreover, provision of adolescent-friendly health services at schools and healthcare centers, and initiating adolescent empowerment programs could have a positive impact on reducing adolescent pregnancy.
Further research is required on the determinants of adolescent pregnancy in the top five sub-Saharan African countries— Niger, Mali, Angola, Mozambique, and Guinea-- with rates of adolescent pregnancy above 140 births per 100,000 adolescent women.
Acknowledgments
We would like to thank the staff of Health Education and Health Promotion Department, School of Public Health, Tehran University of Medical Sciences for their support during this study. We also wish to express our appreciation to Tehran University of Medical Sciences for granting us the opportunity to have access to the school’s subscribed online databases and libraries during our data collection. Finally, our appreciation goes to the various authors of our included studies.
Funding
The authors received no funding for the study.
Availability of data and materials
The data set supporting the conclusions of this article is included in the article’s Table 1.
Authors’ contributions
YI conceptualized and wrote the original script. Both YI and WJS participated in data extraction and together determined the methodology, validated, reviewed and edited the final manuscript. Both authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Ibrahim Yakubu, Email: yaib85@gmail.com.
Waliu Jawula Salisu, Email: waliujawula@gmail.com.
References
- 1.Browne AW, Barrett HR. Female education in sub-Saharan Africa: the key to development? Comp Educ. 1991;27(3):275–285. [Google Scholar]
- 2.World Health Organization: Adolescent pregnancy Factsheet [Internet]. World Health Organization. 2014 [cited September 2014]. Available from: http://www.who.int/mediacentre/factsheets/fs364/en/.
- 3.Phillips SJ, Mbizvo MT. Empowering adolescent girls in sub-Saharan Africa to prevent unintended pregnancy and HIV: a critical research gap. Int J Gynaecol Obstet. 2016;132(1):1–3. doi: 10.1016/j.ijgo.2015.10.005. [DOI] [PubMed] [Google Scholar]
- 4.world atlas. World Facts: Highest Teen Pregnancy Rates Worldwide 2015 [updated April 25, 2017. Available from: http://www.worldatlas.com/articles/highest-teen-pregnancy-rates-worldwide.html.
- 5.Ganchimeg T, Ota E, Morisaki N, Laopaiboon M, Lumbiganon P, Zhang J, et al. Pregnancy and childbirth outcomes among adolescent mothers: a World Health Organization multi-country study. BJOG. 2014;121(Suppl 1):40–48. doi: 10.1111/1471-0528.12630. [DOI] [PubMed] [Google Scholar]
- 6.Chandra-Mouli V, Camacho AV, Michaud P-A. WHO guidelines on preventing early pregnancy and poor reproductive outcomes among adolescents in developing countries. J Adolesc Health. 2013;52(5):517–522. doi: 10.1016/j.jadohealth.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 7.Horgan RP, Kenny LC. Management of teenage pregnancy. Obstet Gynaecol. 2007;9(3):153–158. [Google Scholar]
- 8.Officials NAoCCH . Meeting the needs of pregnant and parenting teens. Washington: Local Health Department Programs and Services; 2009. [Google Scholar]
- 9.Hodgkinson S, Beers L, Southammakosane C, Lewin A. Addressing the mental health needs of pregnant and parenting adolescents. Pediatrics. 2014;133(1):114–122. doi: 10.1542/peds.2013-0927. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Atuyambe L, Mirembe F, Johansson A, Kirumira EK, Faxelid E. Experiences of pregnant adolescents--voices from Wakiso district, Uganda. Afr Health Sci. 2005;5(4):304–309. doi: 10.5555/afhs.2005.5.4.304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Aransiola JO, Asa S, Obinjuwa P, Olarewaju O, Ojo OO, Fatusi AO. Teachers' perspectives on sexual and reproductive health interventions for in-school adolescents in Nigeria. Afr J Reprod Health. 2013;17(4):84–92. [PubMed] [Google Scholar]
- 12.Warenius L, Pettersson KO, Nissen E, Höjer B, Chishimba P, Faxelid E. Vulnerability and sexual and reproductive health among Zambian secondary school students. Cult Health Sex. 2007;9(5):533–544. doi: 10.1080/13691050601106679. [DOI] [PubMed] [Google Scholar]
- 13.Ahorlu CK, Pfeiffer C, Obrist B. Socio-cultural and economic factors influencing adolescents' resilience against the threat of teenage pregnancy: a cross-sectional survey in Accra, Ghana. Reprod Health. 2015;12:117. doi: 10.1186/s12978-015-0113-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumi-Kyereme A, Awusabo-Asare K, Darteh EK. Attitudes of gatekeepers towards adolescent sexual and reproductive health in Ghana. Afr J Reprod Health. 2014;18(3):142–153. [PubMed] [Google Scholar]
- 15.Mushwana L, Monareng L, Richter S, Muller H. Factors influencing the adolescent pregnancy rate in the Greater Giyani municipality, Limpopo Province - South Africa. Int J Afr Nurs Sci. 2015;2:10–18. [Google Scholar]
- 16.A Yidana, SD Ziblim, TB Azongo, Abass YI. Socio-cultural determinants of contraceptives use among adolescents in northern Ghana. Public Health Res. 2015;5(4):83–89.
- 17.Adinma JI, Agbai AO, Okeke AO, Okaro JM. Contraception in teenage Nigerian school girls. Adv Contracept. 1999;15(4):283–291. doi: 10.1023/a:1006732222373. [DOI] [PubMed] [Google Scholar]
- 18.Ahlberg BM, Jylkas E, Krantz I. Gendered construction of sexual risks: implications for safer sex among young people in Kenya and Sweden. Reprod Health Matters. 2001;9(17):26–36. doi: 10.1016/s0968-8080(01)90005-9. [DOI] [PubMed] [Google Scholar]
- 19.Atuyambe LM, Kibira SP, Bukenya J, Muhumuza C, Apolot RR, Mulogo E. Understanding sexual and reproductive health needs of adolescents: evidence from a formative evaluation in Wakiso district, Uganda. Reprod Health. 2015;12:35. doi: 10.1186/s12978-015-0026-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Atuyambe L, Mirembe F, Annika J, Kirumira EK, Faxelid E. Seeking safety and empathy: adolescent health seeking behavior during pregnancy and early motherhood in central Uganda. J Adolesc. 2009;32(4):781–796. doi: 10.1016/j.adolescence.2008.10.012. [DOI] [PubMed] [Google Scholar]
- 21.Adekunle AO, Arowojolu AO, Adedimeji AA, Roberts OA. Adolescent contraception: survey of attitudes and practice of health professionals. Afr J Med Med Sci. 2000;29(3-4):247–252. [PubMed] [Google Scholar]
- 22.Abdul-Rahman L, Marrone G, Johansson A. Trends in contraceptive use among female adolescents in Ghana. Afr J Reprod Health. 2011;15(2):45–55. [PubMed] [Google Scholar]
- 23.Krugu JK, Mevissen FE, Prinsen A, Ruiter RA. Who's that girl? A qualitative analysis of adolescent girls' views on factors associated with teenage pregnancies in Bolgatanga, Ghana. Reprod Health. 2016;13:39. doi: 10.1186/s12978-016-0161-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The Joanna Briggs Institute . Joanna Briggs institute reviewers’ manual. 2011. [Google Scholar]
- 25.Sedgh G, Finer LB, Bankole A, Eilers MA, Singh S. Adolescent pregnancy, birth, and abortion rates across countries: levels and recent trends. J Adolesc Health. 2015;56(2):223–230. doi: 10.1016/j.jadohealth.2014.09.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gyan C. The effects of teenage pregnancy on the educational attainment of girls at Chorkor, a suburb of Accra. J Educ Soc Res. 2013;3(3):53. [Google Scholar]
- 27.Hokororo A, Kihunrwa AF, Kalluvya S, Changalucha J, Fitzgerald DW, Downs JA. Barriers to access reproductive health care for pregnant adolescent girls: a qualitative study in Tanzania. Acta Paediatrica (Oslo, Norway: 1992) 2015;104(12):1291–1297. doi: 10.1111/apa.12886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.McCleary-Sills J, Douglas Z, Rwehumbiza A, Hamisi A, Mabala R. Gendered norms, sexual exploitation and adolescent pregnancy in rural Tanzania. Reprod Health Matters. 2013;21(41):97–105. doi: 10.1016/S0968-8080(13)41682-8. [DOI] [PubMed] [Google Scholar]
- 29.Silberschmidt M, Rasch V. Adolescent girls, illegal abortions and "sugar-daddies" in Dar es salaam: vulnerable victims and active social agents. Soc Sci Med. 2001;52(12):1815–1826. doi: 10.1016/s0277-9536(00)00299-9. [DOI] [PubMed] [Google Scholar]
- 30.Wood K, Jewkes R. Blood blockages and scolding nurses: barriers to adolescent contraceptive use in South Africa. Reprod Health Matters. 2006;14(27):109–118. doi: 10.1016/S0968-8080(06)27231-8. [DOI] [PubMed] [Google Scholar]
- 31.Wood L, Hendricks F. A participatory action research approach to developing youth-friendly strategies for the prevention of teenage pregnancy. Educ Action Res. 2017;25(1):103–118. [Google Scholar]
- 32.Yidana A, Ziblim SD, Azongo TB, Abass YI. Socio-cultural determinants of contraceptives use among adolescents in northern Ghana. Public Health Res. 2015;5(4):83–89. [Google Scholar]
- 33.Adzitey SP, Adzitey F, Suuk L. Teenage pregnancy in the Builsa District: a focus study in Fumbisi. 2011. [Google Scholar]
- 34.Alhassan E. Early pregnancy of junior high school girls: causes and implications on academic progression in the Talensi District of the upper east region of Ghana. UDS Int J Dev. 2015;2(2):47–59.
- 35.Jewkes R, Vundule C, Maforah F, Jordaan E. Relationship dynamics and teenage pregnancy in South Africa. Soc Sci Med. 2001;52(5):733–744. doi: 10.1016/s0277-9536(00)00177-5. [DOI] [PubMed] [Google Scholar]
- 36.Lambani MN. Poverty the cause of teenage pregnancy in Thulamela municipality. 2015. [Google Scholar]
- 37.Marston M, Beguy D, Kabiru C, Cleland J. Predictors of sexual debut among young adolescents in Nairobi's informal settlements. Int Perspect Sex Reprod Health. 2013;39(1):22–31. doi: 10.1363/3902213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.McHunu G, Peltzer K, Tutshana B, Seutlwadi L. Adolescent pregnancy and associated factors in south African youth. Afr Health Sci. 2012;12(4):426–434. doi: 10.4314/ahs.v12i4.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ogori AF, Ajeya SHiTU fatima, Yunusa AR. The cause and effect of teenage pregnancy: case of Kontagora local government area in Niger state, northern part of Nigeria. J Educ Res 2013;Vol. 1,( No. 7): 01-15.
- 40.Okigbo CC, Speizer IS. Determinants of sexual activity and pregnancy among unmarried young women in urban Kenya: a cross-sectional study. PLoS One. 2015;10(6):e0129286. doi: 10.1371/journal.pone.0129286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Salami KK, Ayegboyin M, Adedeji IA. Unmet social needs and teenage pregnancy in Ogbomosho, South-western Nigeria. Afr Health Sci. 2014;14(4):959–966. doi: 10.4314/ahs.v14i4.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Taffa N, Omollo D, Matthews Z. Teenage pregnancy experiences in rural Kenya. Int J Adolesc Med Health. 2003;15(4):331–340. doi: 10.1515/ijamh.2003.15.4.331. [DOI] [PubMed] [Google Scholar]
- 43.Tilahun M, Mengistie B, Egata G, Reda AA. Health workers' attitudes toward sexual and reproductive health services for unmarried adolescents in Ethiopia. Reprod Health. 2012;9:19. doi: 10.1186/1742-4755-9-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Warenius LU, Faxelid EA, Chishimba PN, Musandu JO, Ong'any AA, Nissen EB. Nurse-midwives' attitudes towards adolescent sexual and reproductive health needs in Kenya and Zambia. Reprod Health Matters. 2006;14(27):119–128. doi: 10.1016/S0968-8080(06)27242-2. [DOI] [PubMed] [Google Scholar]
- 45.Were M. Determinants of teenage pregnancies: the case of Busia District in Kenya. Econ Hum Biol. 2007;5(2):322–339. doi: 10.1016/j.ehb.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 46.Mngadi PT, Zwane IT, Ahlberg BM, Ransjo-Arvidson AB. Family and community support to adolescent mothers in Swaziland. J Adv Nurs. 2003;43(2):137–144. doi: 10.1046/j.1365-2648.2003.02688.x. [DOI] [PubMed] [Google Scholar]
- 47.worldatlas. Highest Teen Pregnancy Rates Worldwide. In: Dillinger J, editor. 2017.
- 48.Fearon E, Wiggins RD, Pettifor AE, Hargreaves JR. Is the sexual behaviour of young people in sub-Saharan Africa influenced by their peers? A systematic review. Soc Sci Med. 2015;146:62–74. doi: 10.1016/j.socscimed.2015.09.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Silk J, Romero D. The role of parents and families in teen pregnancy prevention. J Fam Issues. 2014;35(10):1339–1362. [Google Scholar]
- 50.Cavazos-Rehg PA, Krauss MJ, Spitznagel EL, Schootman M, Bucholz KK, Peipert JF, et al. Age of sexual debut among US adolescents. Contraception. 2009;80(2):158–162. doi: 10.1016/j.contraception.2009.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lohman BJ, Billings A. Protective and risk factors associated with adolescent boys’ early sexual debut and risky sexual behaviors. J Youth Adolesc. 2008;37(6):723. [Google Scholar]
- 52.Mott FL, Fondell MM, Hu PN, Kowaleski-Jones L, Menaghan EG. The determinants of first sex by age 14 in a high-risk adolescent population. Fam Plan Perspect. 1996;28(1):13–18. [PubMed] [Google Scholar]
- 53.Parsons J, Edmeades J, Kes A, Petroni S, Sexton M, Wodon Q. Economic impacts of child marriage: a review of the literature. Review Faith Int Affairs. 2015;13(3):12–22. [Google Scholar]
- 54.Ebeigbe PN, Gharoro EP. Obstetric complications, intervention rates and maternofetal outcome in teenage nullipara in Benin City, Nigeria. Trop Dr. 2007;37(2):79–83. doi: 10.1177/004947550703700206. [DOI] [PubMed] [Google Scholar]
- 55.Leclerc-Madlala S. Age-disparate and intergenerational sex in southern Africa: the dynamics of hypervulnerability. AIDS. 2008;22:S17–S25. doi: 10.1097/01.aids.0000341774.86500.53. [DOI] [PubMed] [Google Scholar]
- 56.Homma Y, Wang N, Saewyc E, Kishor N. The relationship between sexual abuse and risky sexual behavior among adolescent boys: a meta-analysis. J Adolesc Health. 2012;51(1):18–24. doi: 10.1016/j.jadohealth.2011.12.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data set supporting the conclusions of this article is included in the article’s Table 1.


