Abstract
Objective:
To determine the epidemiological aspects of patients with traumatic brain injury (TBI) in a regional trauma center.
Methods:
A cross-sectional study was conducted on patients with TBI during 2013 to 2016 in a single center in Hamedan, central Iran. The distribution and relationships of TBI was assessed with gender, age, type of trauma, traumatic cause, exiting status and Length of Hospitalization (LOH). Data were analyzed by Stata V11 statistical software.
Results:
In general, 9426 patients with TBI were enrolled in analyses. The mean ± SD age of patients was 29.70 (± 21.46) years. Multivariate logistic regression indicated that being male [OR: 1.29; 95% CI (2.92-4.73), P ≤0.001], 41-50 to 71-80 and 90+ years old' age groups (1.32<OR<3.12, 0.029<p≤0.001), having surgery [OR: 5.58; 95% CI (4.89-6.37), p≤0.001], and different types of trauma (p≤0.001) were significantly related to LOH. Moreover, odds ratio of mortality was 1.52 times greater in males than females (p≤0.001). As the age increases, the odds ratio of mortality was also rising. However, having surgery [OR: 3.72; 95% CI (2.92-4.73), p≤0.001], LOH >5 days [OR: 2.01; 95% CI (1.60-2.52), p≤0.001] and different types of trauma were significantly related to mortality.
Conclusion:
TBI is one of the main causes of mortality and LOH of the young population. By providing preventive measures and a traumatic care system, the burden of trauma can be greatly reduced, the implementation of the trauma care system in Hamedan province is a necessity.
Key Words: Epidemiology, Trend, Trauma, Injury, Head injury, Head trauma, Brain injury, Trauma care, Iran
Introduction
Traumatic brain injury (TBI) is a common reason for an emergency room visit. Traumatic events and loss are common in people's lives, from every 10 deaths in the world, one of them is due to trauma [1-3]and in developing countries, most of DALYs (Disability Adjusted Life-Years), economic losses and the main cause of death are accounted for the trauma in the ages of 1 to 29 years [4, 5].
In physical medicine, major trauma is injury or damage to a biological organism caused by physical harm from an external source and the internal source or disease in the body is not cause of injury [6, 7]. The World Health Organization (WHO) estimates that the burden of disease from trauma will increase from 14% to 20% by 2020 [7, 8]. Intracranial hemorrhages are one of the most serious and unfortunate consequences of injuries and this may occur in four form (Epidural, Subdural, Subarachnoid and Intracerebral) hemorrhages [9]. The consequences of head injuries are serious, which mainly are occurred due to the neglect of motorists, cyclists, construction workers and industrial workers in observing safety precautions. In Iran, studies have shown that head and neck injury were one of the most common traumas and the most traumatic mechanism was road accidents. Accidents are the most important causes of death, disability, hospital costs and economic damage to the community, which the WHO has chosen them as the main topic of research [10-12]. Death in road accidents in elderly is twice that of other age groups [7, 9, 13].
Patients suffering from trauma, especially TBI have an emergency condition. Cause and type of traumas vary according to socioeconomic and other demographic characters in different societies. Finding patterns and distribution of lethal traumas, such as head injury, is necessary in each geographic region and counties for policy-making in the health sector, and preventive measures are needed [14].
This study attempts to investigate all causes of head trauma, considering that few studies have been carried out specifically for patients with TBI in Hamadan, Iran. Therefore, it is necessary to identify risk factors for TBI patients and attempted to identify the high-risk groups in order to improve the quality of services and to establish a trauma care system [15] for patients with head trauma.
Materials and Methods
Study Design / Population
This study was carried out using cross-sectional method on patients with head injuries in one of the largest and provincial reference university hospitals in the north west of the Iran. Due to lack of trauma ward in other hospitals of the province cities, these trauma patients are referred to this hospital. Therefore, it can be said that Be'sat Hospital covers all cases of trauma, except for those who go to hospitals in other provinces, including Tehran, before going to Be'sat Hospital.
Data collection
Data were collected from the hospital registry database. Patients included those who had head or neck injuries, refereed to Be'sat hospital, Hamadan, admitted to the hospital from March 2013 to December 2016, data entered into the Excel 2013 program (Microsoft Office Professional Plus 2013). A total of 424 patients were not eligible to enter the analyses so excluded. So to extract data a checklist was developed based on the objectives of the study (gender, age, type of trauma, mechanism of trauma, Length of Hospitalization (LOH) and final outcome). The LOH was calculated by subtracting the patient's discharge time from the time of admission. So the required information was extracted, then entered by the trained personnel in the Stata software version 11.0 (Stata Corp, College Station, TX).
All appropriate ethical and regulatory permissions were obtained. Study registration number is 95-05-11-4625 in Deputy of Research, Hamedan University of Medical Sciences.Types of trauma were categorized according to ICD-10 codes as follows: Fracture of base of skull (S02.10), Fracture of neck, part unspecified (S12.90), Diffuse brain injury (S06.20), Epidural hemorrhage (S06.40), Unspecified injury of head (face, ear, nose) (S09.9), Other intracranial injuries (S06.80), Intracranial injury, unspecified (Brain injury) (S06.90), Fracture of vault of skull (S02.00), Fracture of skull and facial bones, part unspecified (S02.90), Injury of spinal cord, level unspecified (T09.3), Traumatic subarachnoid hemorrhage (S06.60), Other and unspecified injuries of head (S09), Traumatic subdural hemorrhage (S06.50).
Since the causes of the head injury were over 100 types, so we extracted cases with 1% frequency and above .
As well as external causes of TBI were determined according to proprietary codes of ICD-10 .Pedestrian injured in collision with two- or three-wheeled motor vehicle (V02.0), Pedestrian injured in collision with car, pick-up truck or van (V03.0), Motorcycle rider injured in collision with car, pick-up truck or van/ Driver injured/ (V23.0), Motorcycle rider injured in collision with car, pick-up truck or van/ Passenger injured/ (V23.1), Motorcycle rider injured in non-collision transport accident/Driver injured/ (V28.0), Motorcycle rider injured in non-collision transport accident /Passenger injured (V28.1), Motorcycle rider injured in non-collision transport accident /Unspecified motorcycle rider injured/ (V28.9), Motorcycle rider [any] injured in unspecified traffic accident (V29.9), Car occupant injured in collision with car, pick-up truck or van /Driver injured/ (V43.0), Car occupant injured in collision with car, pick-up truck or van /Passenger injured/ (V43.1), Car occupant injured in collision with heavy transport vehicle or bus/Passenger injured/ (V44.1), Car occupant injured in non-collision transport accident/Driver injured/ (V48.0), Car occupant injured in non-collision transport accident/Passenger injured/ (48.1), Car occupant injured in non-collision transport accident/Unspecified car occupant injured/ (48.9), Car occupant [any] injured in unspecified traffic accident (V49.9), Person injured in unspecified vehicle accident (V89.9), Fall on and from stairs and steps (W10.9), Other fall from one level to another (W17.9), Other fall on same level (W18.9), Struck by thrown, projected or falling object (W20.9), Striking against or struck by other objects (W22.9), Assault by bodily force (Y04.9).
Inclusion criteria
The eligibility criteria were determined based on the definition of patients with TBI and the tenth edition of the International Classification of Diseases (ICD-10) and the codes for head and neck injuries [16].
Exclusion criteria
Totally, 9841 patients with head injury were extracted from Be'sat hospital registry database. Of these, 361 patients with non-traumatic head and neck codes were excluded . Therefore, in 63 cases, more than 30% of the information was incomplete and they were excluded. Finally, 9426 patients entered the study protocol.
Analysis
Initially, descriptive factors of the TBI were assessed by using frequency and standard division. Normality was checked using one sample Kolmogorov-Smirnov test. So the relationships between qualitative variables were analyzed by Chi-square test, the analytical relationships between variables and for control the confounding effects, a full model including all independent variables was initially estimated and then using a backward stepwise selection procedure.
Furthermore, adjusted multivariable logistic regression model on 5% level of significance was used. Eventually, a final model including only those variables that had a statistically significant association with LOH or Mortality was developed. Data analysis was performed using the Stata V11 (Stata Corp, College Station, TX) software . In all analysis, a p-value of <0.05 was considered statistically significant.
Results
Descriptive Factors
In this study, the mean ± SD age of patients was 29.70 (± 21.46) years. By increasing age (changes range: 0 to 110 years) the frequency of TBI was reduced. So that 73% of cases were in the 0 to 40 age group and 90% of cases were in the age group of 0 up to 60 years old, of which the two groups (zero up to 10 and 21 to 30 years old) have the highest frequency. The frequency of TBI in males was twice as females . Therefore, in all age groups, the men were more likely to suffer from TBI (Table 1). Moreover, the number of 349 patients did not have one of the admission or discharge dates, so the hospital admissions days were not calculated for them. According to the Table 1, four types of head injuries with the highest mean (± SD) of LOH were as follows:
Table 1.
Descriptive factors of the traumatic brain injury in Hamadan province, Iran
| Age Groups | 0-10 | 11-20 | 21-30 | 31-40 | 41-50 | 51-60 | 61-70 | 71-80 | 81-90 | 91-100 | 101-110 | Total | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Male | 1309 | 896 | 1493 | 961 | 573 | 447 | 263 | 199 | 95 | 21 | 1 | 6258 | |||||||
| Female | 877 | 309 | 575 | 451 | 307 | 268 | 176 | 135 | 62 | 8 | 0 | 3168 | |||||||
| Genders in died patients | |||||||||||||||||||
| Male | 20 | 30 | 64 | 45 | 40 | 45 | 33 | 44 | 28 | 6 | 1 | 356 | |||||||
| Female | 10 | 6 | 10 | 13 | 10 | 12 | 11 | 17 | 5 | 1 | 0 | 95 | |||||||
| Hospitalization Days | |||||||||||||||||||
| ICD-10 | Mean | SD | |||||||||||||||||
| S02.10 | 13.66 | 17.41 | 16 | 9 | 14 | 10 | 8 | 5 | 6 | 3 | 0 | 0 | 0 | ||||||
| S12.90 | 13.87 | 41.37 | 1 | 8 | 18 | 23 | 21 | 12 | 8 | 4 | 1 | 0 | 0 | ||||||
| S06.20 | 18.08 | 34.33 | 18 | 17 | 28 | 22 | 13 | 15 | 11 | 6 | 5 | 1 | 0 | ||||||
| S06.40 | 11.96 | 15.51 | 29 | 27 | 42 | 31 | 20 | 14 | 3 | 5 | 3 | 0 | 0 | ||||||
| S09.9 | 2.40 | 12.77 | 1884 | 1018 | 1736 | 1133 | 722 | 543 | 336 | 234 | 114 | 17 | 1 | ||||||
| S06.80 | 15.01 | 18.75 | 13 | 3 | 13 | 7 | 11 | 9 | 9 | 12 | 5 | 0 | 0 | ||||||
| S06.90 | 11.62 | 11.22 | 0 | 4 | 1 | 1 | 2 | 0 | 1 | 0 | 0 | 0 | 0 | ||||||
| S02.00 | 6.39 | 7.31 | 30 | 10 | 7 | 11 | 10 | 8 | 2 | 2 | 0 | 0 | 0 | ||||||
| S02.90 | 12.48 | 18.73 | 36 | 14 | 26 | 23 | 3 | 11 | 3 | 2 | 0 | 0 | 0 | ||||||
| T09.3 | 3.29 | 5.53 | 7 | 13 | 23 | 22 | 15 | 13 | 2 | 2 | 2 | 0 | 0 | ||||||
| S06.60 | 17.63 | 34.30 | 12 | 15 | 32 | 29 | 13 | 26 | 14 | 14 | 5 | 2 | 0 | ||||||
| S06.50 | 13.46 | 26.14 | 31 | 15 | 29 | 34 | 16 | 29 | 26 | 35 | 19 | 6 | 0 | ||||||
| S09 | 1.78 | 6.62 | 109 | 52 | 99 | 66 | 26 | 30 | 18 | 15 | 3 | 3 | 0 | ||||||
| Total Percent's | 10.89- | -- | 2186(23.19) | 1205(12.78) | 2068(21.94) | 1412(14.98) | 880(9.34) | 715(7.59) | 439(4.66) | 334(3.54) | 157(1.67) | 29(0.31) | 1(0.01) | ||||||
| Cum | - | - | 23.19 | 35.97 | 57.91 | 72.89 | 82.23 | 89.82 | 94.47 | 98.2 | 99.68 | 99.99 | 100 | ||||||
Diffuse brain injury 18.08(±34.33) days, Traumatic subarachnoid hemorrhage 17.63 (±34.30) days, other intracranial injuries 15.01(± 18.75) days and Fracture of neck, part unspecified 13.87(±41.37) days (Table 1).
LOH and Mortality
In overall, 451 (4.79%) patients died . The number of 25 patients had no discharge date and three male and five female patients had no discharge status, so were not in analyses. Therefore, the numbers of 9077 patients were selected with 66.01% males. LOH was less than five days in 7714 (84.9%) patients. Results showed that the more than five days' LOH frequency ratio in males than in females was 17.17 vs 10.83. According to the results, with the increase in age the more than five days' hospital stay has also increased However as the age increases the number of TBI patient's decreases. Moreover, the frequency ratio of patients that has more than Five days' LOH and surgery than in patients who not surgery was 31.36% vs 6.84%.
In addition, most of the victims were males (5.69%), older patients (rang: 1.37% in ≤10 to 26.67% in 91+ patients), having surgery (11%), patients with more than five days hospitalization. The descriptive characteristics of the TBI are presented in Table 2.
Table 2.
Mortality and Hospitalization of patient with head trauma by the dempgrapic factors
|
LOH
|
Mortality
|
|||||
|---|---|---|---|---|---|---|
| Total (9077) N(%) | ≤5 days (n=7714) | >5 days (n=1363) | Total (n=9418) | Non-survived (n=451) | Survived (n=8967) | |
| Gender(n=9426) | ||||||
| Female | 3085(33.99) | 2751(89.17) | 334(10.83) | 3163 (33.58) | 95(3) | 3.068 |
| Male | 5992(66.01) | 4963(82.83) | 1029(17.17) | 6255(66.42) | 356(5.69) | 5899 |
| Age (year)(n=9426) | ||||||
| 11 | 2113(23.28) | 1922 | 91(9.04) | 2183(23.19) | 30(1.37) | 2153 |
| 11-20 | 1176(12.96) | (90.96) | 165(14.03) | 1203(12.77) | 36(3) | 1167 |
| 21-30 | 1982(21.84) | 1011(85.97) | 265(13.37) | 2067(21.95) | 74(3.58) | 1993 |
| 31-40 | 1348(14.85) | 1717(86.63) | 223(16.54) | 1412(14.99) | 58(4.11) | 1354 |
| 41-50 | 840(9.25) | 1125(83.46) | 142(16.9) | 880(9.34) | 50(5.68) | 830658 |
| 51-60 | 689(7.59) | 698(83.10) | 158(22.93) | 715(7.59) | 57(7.97) | 395 |
| 61-70 | 427(4.7) | 531(77.07) | 92(21.55) | 439(4.66) | 44(10.02) | 272 |
| 71-80 | 321(3.54) | 335(78.45) | 83(25.86) | 333(3.54) | 61(18.32) | 123 |
| 81-90 | 151(1.66) | 238(74.14) | 33(21.85) | 156(1.66) | 33(21.15) | 22 |
| 91+ | 30(0. 39) | 118(78.15) | 11(34.48) | 30(0.32) | 8(26.67) | 2153 |
| Surgery(n=9426) | ||||||
|
Yes
No |
3026 (33.34) 6051(66.66) |
2077(68.64) 5637(93.16) |
949(31.36) 414(6.84) |
3149(33.44) 6269(66.56) |
336(11) 115(2) |
2813 6154 |
| LOH | ||||||
|
≤5
>5 |
-- | -- | -- | 7714(84.98) 1363(15.02) |
249(3.23) 177(12.99) |
7465 1186 |
Mechanism of trauma
Table 3 presents the causes of head injury that have a frequency more than 1%, of all causes of trauma mechanism. This includes 84.46% of the all patients (422 cases were without mechanism of trauma codes, so they were not in the analysis). Totally, 41.75% of head injuries were due to vehicle accidents, 30.01% were due to various types of falls, and 7.93% were due to assault by bodily force.
Table 3.
Most frequentet of external causes of traumatic brain injury, Hamadan province, Iran
| External Code | N | percent |
|---|---|---|
| V02.0 | 185 | 2.05 |
| V03.0 | 565 | 6.27 |
| V23.0 | 344 | 3.82 |
| V23.1 | 99 | 1.10 |
| V28.0 | 224 | 2.49 |
| V28.1 | 110 | 1.22 |
| V28.9 | 94 | 1.04 |
| V29.9 | 113 | 1.25 |
| V43.0 | 147 | 1.63 |
| V43.1 | 381 | 4.23 |
| V44.1 | 113 | 1.25 |
| V48.0 | 254 | 2.82 |
| V48.1 | 656 | 7.29 |
| V48.9 | 137 | 1.52 |
| V49.9 | 176 | 1.95 |
| V89.9 | 161 | 1.79 |
| W10.9 | 585 | 6.50 |
| W17.9 | 1061 | 11.78 |
| W18.9 | 1056 | 11.73 |
| W20.9 | 189 | 2.10 |
| W22.9 | 243 | 2.70 |
| Y04.9 | 714 | 7.93 |
| Total | 7.607 | 84.46 |
| All Cases | 9.004 | - |
Analytical reviews The results of multivariate logistic regression analysis for the variables associated with LOH and mortality of TBI patient is presented in Table 4. These results showed that being male [OR: 1.29; 95% CI(2.92-4.73), p≤0.001], 41-50 to 71-80 and 90+ years old' age groups (1.32<OR<3.12, 0.029<p≤0.001), having surgery [OR: 5.58; 95% CI(4.89-6.37), p≤0.001], and type of trauma (p≤0.001) were significantly related to LOH. The results also showed that, odds ratio of mortality was 1.52 times greater in males than females (p≤0.001). As the age increases, the odds ratio of mortality was also rising, so the odds ratio of mortality in 51-60 years old patients was 3.23 times greater than the ≤10 age group. However, surgery [OR: 3.72; 95% CI(2.92-4.73), p≤0.001], LOH >5 days [OR: 2.01; 95% CI(1.60-2.52), p≤0.001] and different types of trauma were significantly related to mortality. The results of multiple logistic regression analysis for the variables associated with mortality and LOH is presented in Table 4.
Table 4.
Adjusted Odds Ratio (OR) estimating the factors associated with mortality and Hospitalization in patient with traumatic brain injury
|
LOH
|
Mortality
|
|||||
|---|---|---|---|---|---|---|
| Oods Ratio | 95% CI | P -value | Oods Ratio | 95% CI | P -value | |
| Gender | ||||||
| Female | Reference | - | - | Reference | - | - |
| Male | 1.29 | 1.12-1.49 | 0.000 | 1.52 | 1.18-1.96 | 0.001 |
| Age Graups | ||||||
| ≥10 | Reference | - | - | Reference | - | - |
|
11-20
21-30 31-40 41-50 51-60 61-70 71-80 81-90 90+ |
1.05 0.95 1.08 1.32 1.77 1.55 1.92 1.32 3.12 |
0.83-1.33 0.77-1.18 0.87-1.35 1.03-1.69 1.39-2.28 1.16-2.09 1.4-2.63 0.85-2.06 1.34-7.25 |
0.70 0.65 0.47 0.029 0.000 0.003 0.000 0.22 0.008 |
1.42 1.54 1.59 2.66 3.23 3.93 8.39 9.74 10.42 |
0.86-2.34 0.99-2.41 0.99-2.53 1.64-4.30 2.01-5.18 2.38-6.53 5.18-13.58 5.52-17.17 3.88-28.01 |
0.17 0.06 0.051 0.000 0.000 0.000 0.000 0.000 0.000 |
| Surgery | ||||||
| No Yes |
Reference 5.58 |
- 4.89-6.37 |
- 0.000 |
Reference 3.72 |
- 2.92-4.73 |
- 0.000 |
| LOH | ||||||
|
≤5
>5 |
- | - | - | Reference 2.01 |
- 1.60-2.52 |
- 0.000 |
| Trauma Type | 1.09 | 1.06-1.11 | 0.000 | 1.14 | 1.11-1.17 | 0.000 |
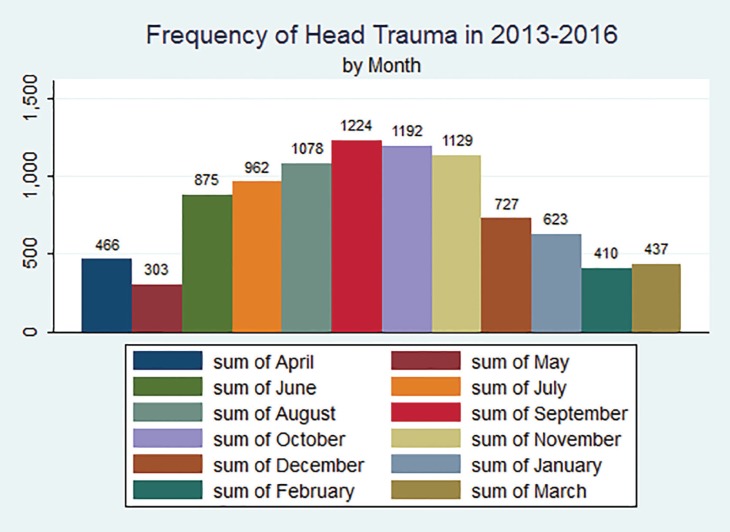
Trend of head injury
Frequency of TBI show an increasing trend during the 2013 to 2016, the highest frequencies were in the middle months of the year in Persian date (khordad to Azar, June to December in Latin date), as the number of TBI patients increases from June to September and this decreased from July to march (Figure1).
Fig. 1.
Frequency of traumatic brain injury in 2013-2016 in Hamedan, Iran.
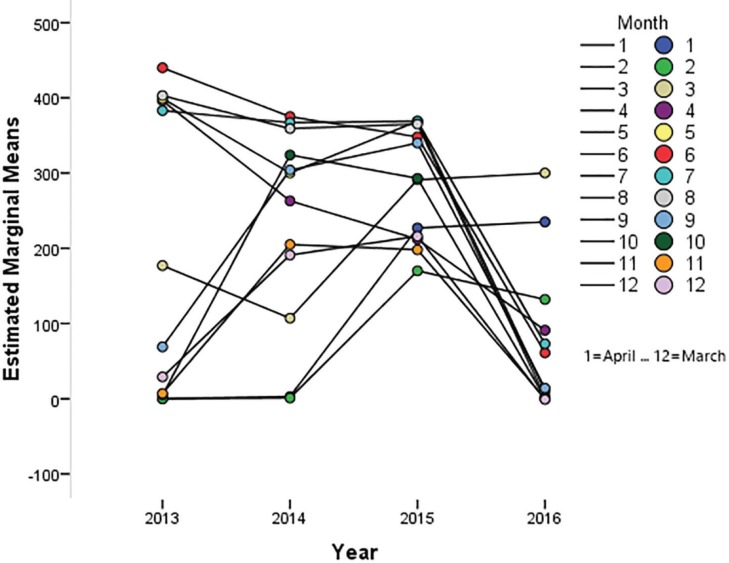
The trend of head trauma's frequency is presented in the Figure 2, in average the frequency of head traumas was increased during 2013 to 2015, although the data of 2016 were not accessible completely in the hospital registry system however, it's expected that distribution of head injury was an incremental trend compared to the previous years.
Fig. 2.
Trend of traumatic brain injury during 2013-2016 in Hamedan, Iran
Discussion
Studies on the epidemiology of traumas, risk factors and the distribution of their outcomes are very widespread. However, the head injury causes a wide range of effects, from memory problems, depression, confusion, anger to fatigue, disability and death. Researchers have been less studied the epidemiology of head traumas exclusively. Therefore, we found that such an investigation is necessary.
In this study, the high-risk cases were under-aged and active groups of the population. Among them, the two groups were the most frequent in the age range of 0 to 10 years old and 21 to 30 years old, so that 73% of patients were under age of 40 years old and the prevalence of TBI in males were about twice as much as females. Some studies in Iran and other countries have reported similar results to the present study [17-20].
Given that the sex ratio in the Iranian population there is not much difference [21], it seems that men to be more at risk than women. Due to the difference in the population ratio in different societies however, it seems men and young/ middle-aged people were more likely to be at risk than women and older age groups .
Various types of vehicles collision, types of falls, strife/ physical quarrel had the first to third ranks among the causes of head injuries. The results of the study by Saadat et al., [22], Rasouli [23], Chardoli et al., [24], Moini et al., [17] were in line with the results of the present study. The causes of trauma in studies carried out in other countries were almost the same as those obtained in Iran [25]. In a prospective cohort study of Janssens et al., [26] the highest incidence of falls and injuries due to cycling has been in the 1 to 9 and 10 to 18 years old age groups. In addition, Gowing and colleagues [18] reported that motor crashes, assaults and falls are three main causes of trauma in last 10 years in Australia. Therefore, considering that in most studies, at risk age groups are young/ active people, it seems that the control or reduction of road accidents and injuries caused by falling into occupations or workplace and high-risk groups is urgency.
In current study, LOH was longer in males than in females and by increase the age, LOH was also increased, which these are agreed to results of the previous studies [27-29]. Length of hospital stay is multifactorial and can be reduced by review of the care protocol to effect incremental changes that have a significant impact on reducing stay [30, 31]. This is wrong to compare LOH between countries, due to differences in the trauma care system and the variations in patterns of trauma and a comparison of our results with previous studies indicate conflicting results.
Furthermore, mortality was higher in male gender and older patients. Researchers discovered significant differences in the type of accident between young women and men and found that young females were 66% more likely to use safety belt than the young males. Therefore, there are studies that indicated that mortality was associated with increase age, these are agreeing about the results of the previous studies. [29, 32, 33].
the study by Hu et al., [34] was in line with our results, so that with increasing age, the rate of death and the number of hospital stay days has increased.
Guidelines and protocols aimed at reducing disability and mortality caused by injuries [31]. Emergency care can play an important role in reducing avoidable mortality and disability in developing countries. However, it's needs to be planned well and supported at all levels. In Iran, Trauma care systems have been implemented in some provinces, however, as it needs the executive infrastructure and costs that have not yet been created in our trauma care system and trauma organizations do not have the proper coordination [35, 36]. Although recently clinical treatment of patients with trauma has improved, but reducing the burden of injuries requires an organizational approach (prehospital care, hospital clinical care, and hospital administrative care) to prevent and treat injuries.
TBI, especially acute head and neck traumas is one of the major causes of death and LOH in Hamadan province. Therefore, attention to the identification and establish trauma care system in this province is urgency. The results of this study and similar studies can provide a suitable field for identifying target groups and provide a solution for policy makers and emergency/ health department officials to take cost-effective measures.
Limitations
This study was performed on hospital data from 2013 to 2016, and since the trauma data were not completely recorded in 2016, it is likely to affect the outcomes of the study. However, we evaluated changes in TBI during the entire period, and comparisons were not made between years
Acknowledgments
The medical records Center of the Be'sat Hospital provide this database. The Institutional Review Board of the Modeling of Non-Communicable Diseases Research Center of Hamedan University of Medical Sciences approved the project.
Funding Support
The Modeling of Non-Communicable Diseases Research Center of Hamedan University of Medical Sciences has supported this study.
Conflict of interest:
The authors has no conflict of interest.
References
- 1.Mahran DG, Farouk O, Qayed MH, Berraud A. Pattern and Trend of Injuries Among Trauma Unit Attendants in Upper Egypt. Trauma Mon. 2016;21(2):e20967. doi: 10.5812/traumamon.20967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rangarajan V, Mavani SB, Nadkarni TD, Goel AH. Traumatic cervical epidural hematoma in an infant. J Craniovertebr Junction Spine. 2013;4(1):37–9. doi: 10.4103/0974-8237.121624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bae JY, Groen RS, Kushner AL. Surgery as a public health intervention: common misconceptions versus the truth. Bull World Health Organ. 2011;89(6):394. doi: 10.2471/BLT.11.088229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Epstein D, Chaib F World Health Organization. WHO releases guidance on mental health care after trauma. (6 August 2013) [cited 25 March 2016]. Available from: http://www.who.int/mediacentre/news/releases/2013/trauma_mental_health_20130806/en.
- 5.Pant PR, Towner E, Pilkington P, Ellis M, Manandhar D. Community perceptions of unintentional child injuries in Makwanpur district of Nepal: a qualitative study. BMC Public Health. 2014;14:476. doi: 10.1186/1471-2458-14-476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sina Trauma and Surgery Research Center. The database deal with the injury (Trauma) [25 March 2016]. Available from: http://traumainfo.ir/Pages.aspx?pgID=1007.
- 7.World Health Organization. Emergency and trauma care. 2016. [cited 25 March 2016]. Available from: http://www.who.int/emergencycare/activities/en.
- 8.World Health Organization. Disability-Adjusted Life Year (DALY) 2016 . [cited 25 March 2016]. Available from: http://www.who.int/healthinfo/global_burden_disease/estimates/en/index2.html.
- 9.Qubty WF, Mrelashvili A, Patterson MC. Epidural hematoma in a patient on pegylated-L-asparginase therapy. J Child Neurol. 2015;30(5):636. doi: 10.1177/0883073813512900. [DOI] [PubMed] [Google Scholar]
- 10.Kim YS, Moon KS, Lee KH, Jung TY, Jang WY, Kim IY, et al. Spontaneous acute epidural hematoma developed due to skull metastasis of hepatocelluar carcinoma: A case report and review of the literature. Oncol Lett. 2016;11(1):741–4. doi: 10.3892/ol.2015.3947. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jalalvandi F, Arasteh P, Safari Faramani R, Esmaeilivand M. Epidemiology of Pediatric Trauma and Its Patterns in Western Iran: A Hospital Based Experience. Glob J Health Sci. 2015;8(6):139–46. doi: 10.5539/gjhs.v8n6p139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Zamani M, Esmailian M, Mirazimi MS, Ebrahimian M, Golshani K. Cause and final outcome of trauma in patients referred to the emergency department: a cross sectional study. Iranian journal of emergency medicine. 2014;1(1):22–7. [Google Scholar]
- 13.Asadi P, Asadi K, Monsef-Kasmaei V, Zohrevandi B, Kazemnejad-leili E, Kouchakinejad Eramsadati L, et al. Evaluation of Frequency of Cervical Spine Injuries in Patients with Blunt Trauma. Journal of Guilan University of Medical Sciences. 2015;23(92):31–6. [Google Scholar]
- 14.Zolotor AJ, Runyan DK, Shanahan M, Durrance CP, Nocera M, Sullivan K, et al. Effectiveness of a Statewide Abusive Head Trauma Prevention Program in North Carolina. JAMA Pediatr. 2015;169(12):1126–31. doi: 10.1001/jamapediatrics.2015.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O'Reilly GM, Gabbe B, Cameron PA. Trauma registry methodology: a survey of trauma registry custodians to determine current approaches. Injury. 2015;46(2):201–6. doi: 10.1016/j.injury.2014.09.010. [DOI] [PubMed] [Google Scholar]
- 16.World Health Organization. ICD-10 online versions. 2016 . [cited 30 March 2016]. Available from: http://www.who.int/classifications/icd/icdonlineversions/en.
- 17.Moini M, Rezaishiraz H, Zafarghandi MR. Characteristics and outcome of injured patients treated in urban trauma centers in Iran. J Trauma. 2000;48(3):503–7. doi: 10.1097/00005373-200003000-00023. [DOI] [PubMed] [Google Scholar]
- 18.Gowing CJ, McDermott KM, Ward LM, Martin BL. Ten years of trauma in the 'top end' of the Northern Territory, Australia: a retrospective analysis. Int Emerg Nurs. 2015;23(1):17–21. doi: 10.1016/j.ienj.2014.09.006. [DOI] [PubMed] [Google Scholar]
- 19.Mehmood A, Allen KA, Al-Maniri A, Al-Kashmiri A, Al-Yazidi M, Hyder AA. Trauma care in Oman: A call for action. Surgery. 2017;162(6s):S107–s16. doi: 10.1016/j.surg.2017.01.028. [DOI] [PubMed] [Google Scholar]
- 20.Consunji R, Ameratunga S, Hyder AA. Trauma care in the developing world: Introduction to special issue. Surgery. 2017;162(6s):S2–s3. doi: 10.1016/j.surg.2017.06.011. [DOI] [PubMed] [Google Scholar]
- 21.Statistical Center of Iran. Statistical information Tehran: Instituto Nacional de Estadística. 1390. [cited 1 February 2017]. Available from: https://www.amar.org.ir.
- 22.Saadat S, Rashidi-Ranjbar N, Rasouli MR, Rahimi-Movaghar V. Pattern of skull fracture in Iran: report of the Iran National Trauma Project. Ulus Travma Acil Cerrahi Derg. 2011;17(2):149–51. doi: 10.5505/tjtes.2011.26043. [DOI] [PubMed] [Google Scholar]
- 23.Rasouli MR, Nouri M, Zarei MR, Saadat S, Rahimi-Movaghar V. Comparison of road traffic fatalities and injuries in Iran with other countries. Chin J Traumatol. 2008;11(3):131–4. doi: 10.1016/s1008-1275(08)60028-0. [DOI] [PubMed] [Google Scholar]
- 24.Chardoli M, Rahimi-Movaghar V. Analysis of trauma outcome at a university hospital in Zahedan, Iran using the TRISS method. East Afr Med J. 2006;83(8):440–2. doi: 10.4314/eamj.v83i8.9458. [DOI] [PubMed] [Google Scholar]
- 25.Magnone S, Ghirardi A, Ceresoli M, Ansaloni L. Trauma patients centralization for the mechanism of trauma: old questions without answers. 2017. [DOI] [PubMed] [Google Scholar]
- 26.Janssens L, Holtslag HR, Leenen LP, Lindeman E, Looman CW, van Beeck EF. Trends in moderate to severe paediatric trauma in Central Netherlands. Injury. 2014;45(8):1190–5. doi: 10.1016/j.injury.2014.04.027. [DOI] [PubMed] [Google Scholar]
- 27.Ghaem H, Soltani M, Yadollahi M, ValadBeigi T, Fakherpour A. Epidemiology and Outcome Determinants of Pedestrian Injuries in a Level I Trauma Center in Southern Iran; A Cross-Sectional Study. Bull Emerg Trauma. 2017;5(4):273–9. doi: 10.18869/acadpub.beat.5.4.508.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Mohtasham-Amiri Z, Dastgiri S, Davoudi-Kiakalyeh A, Imani A, Mollarahimi K. An Epidemiological Study of Road Traffic Accidents in Guilan Province, Northern Iran in 2012. Bull Emerg Trauma. 2016;4(4):230–5. [PMC free article] [PubMed] [Google Scholar]
- 29.Haghparast-Bidgoli H, Saadat S, Bogg L, Yarmohammadian MH, Hasselberg M. Factors affecting hospital length of stay and hospital charges associated with road traffic-related injuries in Iran. BMC Health Serv Res. 2013;13:281. doi: 10.1186/1472-6963-13-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C, Joshipura M. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–31. [PMC free article] [PubMed] [Google Scholar]
- 31.Carney N, Totten AM, O'Reilly C, Ullman JS, Hawryluk GW, Bell MJ, et al. Guidelines for the Management of Severe Traumatic Brain Injury, Fourth Edition. Neurosurgery. 2017;80(1):6–15. doi: 10.1227/NEU.0000000000001432. [DOI] [PubMed] [Google Scholar]
- 32.Bhat G, Beck L, Bergen G, Kresnow MJ. Predictors of rear seat belt use among US adults, 2012. J Safety Res. 2015;53:103–6. doi: 10.1016/j.jsr.2015.03.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lukasiewicz AM, Grant RA, Basques BA, Webb ML, Samuel AM, Grauer JN. Patient factors associated with 30-day morbidity, mortality, and length of stay after surgery for subdural hematoma: a study of the American College of Surgeons National Surgical Quality Improvement Program. J Neurosurg. 2016;124(3):760–6. doi: 10.3171/2015.2.JNS142721. [DOI] [PubMed] [Google Scholar]
- 34.Hu J, Ugiliweneza B, Meyer K, Lad SP, Boakye M. Trend and geographic analysis for traumatic brain injury mortality and cost based on MarketScan database. J Neurotrauma. 2013;30(20):1755–61. doi: 10.1089/neu.2013.2857. [DOI] [PubMed] [Google Scholar]
- 35.Zargar M, Kalantar Motamedi SM, Karbakhsh M, Ghodsi SM, Rahimi-Movaghar V, Panahi F, et al. Trauma care system in Iran. Chin J Traumatol. 2011;14(3):131–6. [PubMed] [Google Scholar]
- 36.Kobusingye OC, Hyder AA, Bishai D, Hicks ER, Mock C, Joshipura M. Emergency medical systems in low- and middle-income countries: recommendations for action. Bull World Health Organ. 2005;83(8):626–31. [PMC free article] [PubMed] [Google Scholar]