Abstract
After the World War II, fecal diversion became the standard of care for colon injuries, although medical, logistic, and technical advancements have challenged this approach. Damage control surgery serves to temporize immediately life-threatening conditions, and definitive management of destructive colon injuries is delayed until after appropriate resuscitation. The bowel can be left in discontinuity for up to 3 days before edema ensues, but the optimal repair window remains within 12 to 48 hours. Delayed anastomosis performed at the take-back operation or stoma formation has been reported with variable results. Studies have revealed good outcomes in those undergoing anastomosis after damage control surgery; however, they point to a subgroup of trauma patients considered to be “high risk” that may benefit from fecal diversion. Risk factors influencing morbidity and mortality rates include hypotension, massive transfusion, the degree of intra-abdominal contamination, associated organ injuries, shock, left-sided colon injury, and multiple comorbid conditions. Patients who are not suitable for anastomosis by 36 hours after damage control may be best managed with a diverting stoma. Failures are more likely related to ongoing instability, and the management strategy of colorectal injury should be based mainly on the patient's overall condition.
Keywords: damage control laparotomy, abdominal trauma, colon trauma, ostomy, anastomosis
A common saying in war is that the only winner is medicine, and this has certainly been demonstrated throughout recent history. Colon injury was associated with mortality surpassing 90% leading up to the American Civil War (1861–1865), decreasing to around 40% in the Second World War (1941 1945) and 10% in the Vietnam war (1955–1975). 1 Since then, considerable improvements have taken place; however, mortality remains close to 3% with a 20% risk of abdominal sepsis. 2
Prior to the First World War, management of colonic injuries was mostly nonoperative and mortality rates reached 100%. However, with advancements in casualty evacuation and prehospital care as well as the high volume of penetrating injury, surgeons tended to abandon the nonoperative approach in favor of laparotomy and primary repair. 3 4 Even with the high risk of failure of this approach, there was a notable decrease in mortality. 5 6 The next paradigm shift in the management of colorectal injuries occurred during the Second World War following Ogilvie's study on the management of colon injuries from the North African campaign of 1942. 7 He strongly promoted fecal diversion for all colon injuries by either exteriorization or resection and repair with diversion, which prompted the British and American forces to mandate such treatment. 8 9 In the Vietnam War period, anatomical distinctions were made, whereby right-sided colon injuries were treated with resection and primary anastomosis and left-sided and rectal injuries employed exteriorization and/or colostomy. The peace period that ensued allowed refined studies to take place, generating adequate data for managing colorectal trauma.
Types of Colon Injuries
Several factors are important in describing colon injuries, as they have implications on management. Injuries can be either penetrating or blunt, destructive or nondestructive, and the specific anatomic location may influence treatment. Second to the small bowel, the colon is the most commonly affected organ in penetrating abdominal trauma, occurring in up to 20% of patients. 10 11 The vast majority of colon injuries are penetrating in nature and mainly caused by gunshot wounds (GSWs), with the ascending and transverse colon most frequently injured. 1 12 GSWs can be high-speed, more common with military trauma, or low-speed, seen mostly with civilian trauma. Stab wounds, on the other hand, affect the descending and sigmoid colon, as most people are right-handed, thus injuring the left colon predominantly. Around 60 to 93% of penetrating colon injuries are treated primarily or by resection and anastomosis. 13
Only 4% of colon injuries are caused by blunt trauma, most of them being motor vehicle collisions. 14 Typically, they involve high-energy transfers and are usually associated with other life-threatening injuries affecting the spleen, liver, small bowel, head, or chest, thus making their diagnosis obscured. 15 Blunt injuries usually include serosal tears, contusions, and devascularizations affecting the transverse and sigmoid colon more frequently, as they are intraperitoneal and more susceptible to traction injury than other parts of the colon. Resection is performed in roughly 60% of these cases, so diversion is more common. 16
Destructive colon injuries may be classified by either the Flint grading system or colon injury scale (CIS). A Flint grade 3 injury (severe tissue loss, devascularization, or heavy contamination) or CIS grades 4 or 5 (circumferential and/or vascular injury) would require resection and anastomosis and/or diversion. In nondestructive injuries, which can be defined by a damage affecting less than 50% of the circumference, primary repair can be readily performed.
Damage Control Laparotomy
After World War II, fecal diversion became the widely accepted standard of care for colon injuries. 17 The first prospective randomized study to tackle the safety of primary repair in traumatic colon injury was published in 1979, advocating its implementation as it was shown to be at least as safe as colostomy and had significantly fewer complications. 18 This paved the way for primary repair to become the standard of care in the mid-1980s owing to its associated lower costs and lower morbidity. However, many studies did not include high-risk patients and with the advent of damage control surgery and its increasing popularity, diversion versus primary repair became a true dilemma for the trauma surgeon.
Severely injured patients often do not have the physiologic reserve to tolerate definitive surgery. Damage control surgery serves to attend to immediately life-threatening conditions, while definitive management of these and other non–life-threatening injuries is delayed until after appropriate resuscitation, thus avoiding the lethal triad of hypothermia, coagulopathy, and acidosis. After accomplishing the initial objectives of controlling hemorrhage and preventing further contamination, patients can be resuscitated and stabilized in the intensive care unit before proceeding with the definitive surgical repair. The strategy of damage control laparotomy (DCL) was popularized in the early 1990s and has become a cornerstone of operative trauma management in the severely injured patient. The bowel can be left in discontinuity for up to 3 days before edema ensues; however, the optimal repair window for definitive surgery remains 12 to 48 hours. After DCL, delayed anastomosis performed at the take-back operation or stoma formation has been reported with variable results. 19 20 21 22 23 24 25 26 As the existing patient practice guidelines were established before damage control was readily performed, they do not specifically address destructive colon injuries in the setting of DCL.
Anastomosis or Ostomy: The Evidence
The first report on the safety of delayed anastomosis after damage control surgery was published in 2007 by Miller et al. 19 One subset of his analysis compared 11 patients who underwent delayed anastomosis to 6 patients who were managed with a colostomy following DCL. Although they had relatively small numbers, both groups were similar with regard to serum lactate, injury severity scores, abscess formation rate, colon-related mortality, and overall mortality. They suggested that a colostomy be created as a last resort, as delayed anastomosis avoids the morbidity of the subsequent operation to restore intestinal continuity.
Vertrees et al published a retrospective review of colon injuries sustained by soldiers during Operation Iraqi Freedom and Operation Enduring Freedom from March 2003 to August 2006. 20 They included 65 patients in total, 27 (42%) of whom were managed by damage control surgery. In their subsequent operations, 17 (63%) were managed by a stoma and 10 (27%) underwent anastomosis. None of those anastomosed had a left colon injury; trauma was to the right (9) and transverse colon (1). The transverse colonic injury was the only anastomotic failure in this group. In the stoma group, five (29%) had a right colon injury, eight (47%) were left, two (12%) were both, and two (12%) were transverse. Thirty-eight patients underwent definitive management at initial operation, whereas 25 (66%) had resection: 10 patients (40%) were managed by an ostomy, whereas 15 (60%) had an anastomosis. The failure rate was 25% (four in total, equally split between the transverse and left colon). They also analyzed outcomes of primary anastomosis versus ostomy in general. However, they failed to address the same question after damage control. They concluded that a delay in anastomosis was not a likely factor in the primary repair or primary anastomosis failure rate. Importantly, anastomoses formed after damage control surgery showed a significantly lower failure rate than those created during the initial laparotomy (10 vs. 25%). Failures usually had concomitant injury to the diaphragm, stomach, spleen, pancreas, and kidney. The location of injury also influenced the type of management, whereby stomas were more likely to be created for the left colon. 20
In 2009, Kashuk et al advocated the use of primary repair after DCL in civilian trauma patients. 21 Out of 29 patients undergoing damage control surgery performed for a concomitant colon injury, 25 (86%) had resection and anastomosis performed at day 2.6 ± 2, whereas 4 had repair at the time of initial injury. An ostomy was subsequently constructed on 7 of the 25 patients; 4 were due to a definite leak, 1 for a suspected leak, and 2 were prophylactic. One of those who had primary repair was diverted for a suspected leak at day 5. The authors deemed anastomotic leak as “the penalty” of performing primary repair after damage control surgery, as opposed to ostomy creation. In this series, primary repair or ostomy had equivalent intensive care unit (ICU) length of stay and ventilator days; however, the presence of an anastomotic leak actually doubled them, p = 0.01 and p = 0.04, respectively. The majority (72%) of their patients requiring DCL had successful restoration of bowel continuity at reoperation. Diverting loop ileostomy is also advocated, as it offers the advantage of avoiding a repeat laparotomy.
Weinberg et al discussed their experience with colon injuries over a 7-year period. 22 Out of 157 patients, 56 were managed by damage control and were stratified by management: 16 had primary repair, 33 had resection and anastomosis, and 7 had resection and colostomy. Comparing resection and anastomosis with resection and colostomy, the only significant difference was the injury severity score (ISS) that was higher in the anastomosis group. Morbidity and mortality were higher in the anastomosis group; however, it was not statistically significant. Of the patients who had an anastomosis, those who developed a leak were compared to those who did not; penetrating trauma was the only factor associated with such complication. Their data do not support diversion as the preferred choice for managing colon injury after damage control, especially in light of the high morbidity rate associated with eventual colostomy closure. 27 28 29 30
Sobering data were reported by Ott and colleagues on 174 trauma colectomies; 79 were treated with damage control of which 44 had an anastomosis and 35 ended up with a colostomy. 23 Of the 44 managed with anastomosis, 12 (27%) experienced a leak. Their data showed that length of hospital stay in this subgroup is increased from 13 to 38 days ( p = 0.004) and length of ICU stay increased from 6 to 21 ( p = 0.04). Furthermore, those who leaked received on average 17 transfusions compared with 2 in those who did not leak ( p = 0.01) and the left colon was injured in 58% of leaks versus 19% in those without one. They found no differences when comparing anastomosis ( n = 44) to stoma ( n = 35) in damage control with regard to mortality, hospital and ICU length of stay, and ventilator-free days. Although the authors concluded that since almost 75% of patients were managed successfully by an anastomosis and thus avoided the morbidity of a stoma and its take-down, the 27% leak rate should raise concern among surgeons in patients deemed at higher risk for anastomosis. A slightly lower (but still substantial) leak rate was reported by Ordoñez et al in 60 patients with colon trauma. This study compared outcomes between 27 patients treated by damage control with delayed anastomosis and 33 who underwent a single laparotomy with primary repair ( n = 26) or colostomy ( n = 7). 24 They found no difference between the groups with regard to mortality, leaks, intra-abdominal abscesses, and fasciitis. They inferred that a delayed anastomosis in the setting of damage control surgery is reliable and feasible with a success rate of 81%.
Timing of Fascial Closure and Implications on Bowel Repair
Whether prolonged delay in definitive abdominal closure results in adverse outcomes has been studied in a limited manner. In one study that included 61 patients with traumatic colon injuries requiring DCL, Georgoff et al associated the development of an anastomotic leak with failure of achieving abdominal closure. 25 Patients in whom the fascia was not closed by postinjury day 5 had a 16.8-fold higher risk of anastomotic leak relative to the entire cohort (18 vs. 2%, p = 0.03). Patients at greatest risk for leak included those with preexisting comorbidities, massive resuscitation, and high degree of fecal contamination. Burlew et al confirmed this finding, whereby fascial closure on or after day 5 resulted in a fourfold increase in odds of developing a leak ( p = 0.02). 26 They concluded that for all patients requiring DCL with an associated colon injury, primary repair or anastomosis should be considered even in a delayed manner, except those who are high risk with an open abdomen for more than 5 days. Another study compared colon injuries treated with a single laparotomy, damage control with fascial closure on first take-back, and damage control with multiple reoperations. 31 Inability to achieve fascial closure by the first reoperation increased the rate of intra-abdominal abscesses from 31 to 50% and anastomotic leaks from 2 to 19%, both p < 0.001. Taken together, these studies support the early restoration of colonic continuity (within 48 hours postinjury), and if this is not feasible, then fecal diversion should be performed.
Right versus Left Colon Injuries
It is generally accepted that left-sided colon injuries are associated with a higher incidence of anastomotic failure, especially after damage control surgery. 8 20 23 26 32 33 Several studies have tackled this dogma and have showed that primary repair of left- or right-sided colon injuries are similar in terms of morbidity and mortality regardless of the method of management used. 34 Surgeons tend to employ primary repair or resection and anastomosis for right colon injuries more often than left-sided injuries where diversion is preferred. 8 35 36 This tendency more likely reflects sound surgical judgment rather than abiding to a protocol or management algorithm. As leak rates and infectious complications do not appear to be different in right- and left-sided colon injuries, the location of injury must not affect surgical management. 37 How damage control surgery influences this decision remains unknown.
Summation of Data
There remains a paucity of high-quality data guiding management decisions on whether an anastomosis or a stoma should be performed after DCL. These data are inconsistent to guide operative decision making in the setting of damage control. Questions regarding how to best identify high-risk patients and minimize the number of anastomosis-associated complications remain unanswered. Recent information suggests that delayed anastomosis of colon injuries after DCL is safe in select patients, but determining who constitutes this group of patients remains unclear. At present, there are no standardized guidelines to aid in the decision making on whether a delayed anastomosis should be performed after DCL. A handful of studies have examined colon reconstruction after DCL, with varying and conflicting results. The damage control patient is physiologically and anatomically compromised and definitive reconstruction should be delayed in this unstable, hypothermic, and coagulopathic patient. Consequently, an anastomotic leak can be catastrophic in this subset of trauma patients and is associated with significant morbidity, including increased length of ICU stay, total number of abdominal surgeries, and a decreased likelihood of fascial closure. However, at least three-quarters of the damage control patients can be successfully reconstructed, avoiding the morbidity and expense of a second hospitalization for colostomy reversal. 23 This presents the surgeon with a strategic dilemma at the time of second-look surgery: how to minimize the risk of anastomotic leak while achieving the benefits of colon reconstruction.
The answer is to stratify patients into high- and low-risk groups for anastomotic failure. As mentioned earlier, a handful of studies address the management of colorectal injury in the setting of DCL, but there is no overall consensus on the subject. Although the quality and quantity of evidence on this subject are scarce, the medical literature does report good outcomes in those undergoing anastomosis after damage control surgery. However, most of the studies appear to point to a subgroup of trauma patients considered to be “high risk” and who may benefit from fecal diversion rather than anastomosis. Based on the analyses published, risk factors influencing morbidity and mortality rates after colon injuries and primary repair following DCL include hypotension, massive transfusion, the level of intra-abdominal contamination at the time of surgery, associated organ injuries, the need for vasopressor support, left-sided colon injury, and multiple comorbid conditions. 20 22 23 26 In addition, in the majority of studies conducted thus far, patients underwent anastomosis within 12 to 36 hours after initial damage control procedure. It is more likely that a patient who is not suitable for anastomosis by the 36-hour mark due to factors such as persistent hemodynamic instability, a bowel that appears unhealthy, or technical difficulties is best managed with a diverting stoma. All patients with hemodynamic instability, signs of coagulopathy, and hypothermia with destructive colon injuries warrant damage control resection and the bowel should be left in discontinuity. Fig. 1 shows our suggested management algorithm in that setting for subsequent operations.
Fig. 1.
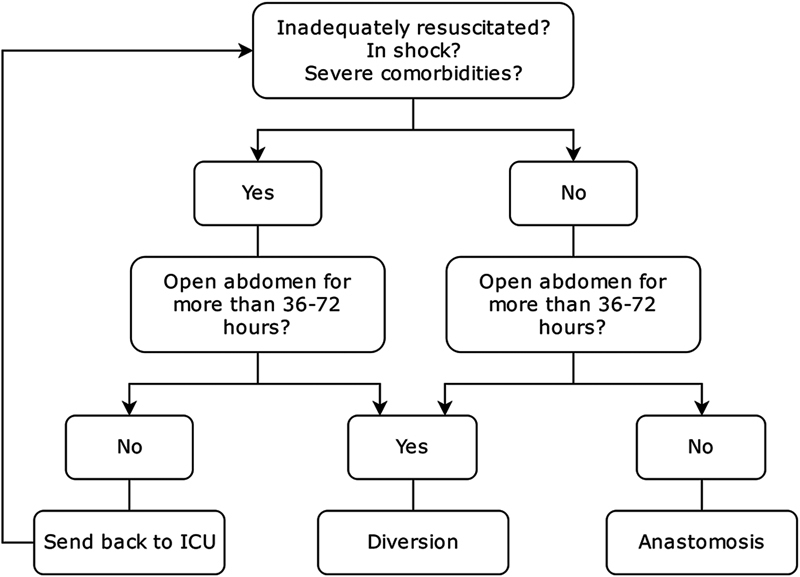
Suggested algorithm for the management of the discontinuous colon at subsequent operations after damage control laparotomy.
Failures are more likely related to ongoing instability, and the management strategy of colorectal injury should be based more on the patient's overall condition rather than on whether they initially underwent a damage control procedure. Caution should be exercised in the management of those in shock, those having a high transfusion requirement, and those with significant comorbidities. Sound surgical judgment is required in these settings and the evaluation of whether the patient can tolerate a complication after anastomotic failure should be heavily weighed against the benefits of avoiding a colostomy. Though it appears that most patients can tolerate a primary anastomosis after DCL, there still remains a subset of patients who may benefit from stoma creation and it is up to the surgeon to be thoughtful in determining who this may be.
References
- 1.Choi W J. Management of colorectal trauma. J Korean Soc Coloproctol. 2011;27(04):166–172. doi: 10.3393/jksc.2011.27.4.166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Demetriades D. Colon injuries: new perspectives. Injury. 2004;35(03):217–222. doi: 10.1016/j.injury.2003.11.004. [DOI] [PubMed] [Google Scholar]
- 3.Bennett J D. Abdominal surgery in war--the early story. J R Soc Med. 1991;84(09):554–557. doi: 10.1177/014107689108400917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Derby A C. Wounds of the abdomen. Part 1: In war. Can J Surg. 1988;31(04):213–218. [PubMed] [Google Scholar]
- 5.Bowlby A, Wallace C.The development of British surgery at the front BMJ 19171(2944):705–721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Rignault D P. Abdominal trauma in war. World J Surg. 1992;16(05):940–946. doi: 10.1007/BF02066996. [DOI] [PubMed] [Google Scholar]
- 7.Ogilvie W H. Abdominal wounds in the Western Desert. Bull US Army Med Dep. 1946;6(04):435–445. [PubMed] [Google Scholar]
- 8.Miller P R, Fabian T C, Croce M A et al. Improving outcomes following penetrating colon wounds: application of a clinical pathway. Ann Surg. 2002;235(06):775–781. doi: 10.1097/00000658-200206000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ogilvie W H.Surgical lessons of war applied to civil practice BMJ 19451(4400):619–623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carrillo E H, Somberg L B, Ceballos C E et al. Blunt traumatic injuries to the colon and rectum. J Am Coll Surg. 1996;183(06):548–552. [PubMed] [Google Scholar]
- 11.Stewart R M, Rosenthal D. Philadelphia, PA: Lippincott Williams & Wilkins; 2005. Colorectal trauma; pp. 427–449. [Google Scholar]
- 12.Johnson E K, Steele S R. Evidence-based management of colorectal trauma. J Gastrointest Surg. 2013;17(09):1712–1719. doi: 10.1007/s11605-013-2271-9. [DOI] [PubMed] [Google Scholar]
- 13.Cleary R K, Pomerantz R A, Lampman R M. Colon and rectal injuries. Dis Colon Rectum. 2006;49(08):1203–1222. doi: 10.1007/s10350-006-0620-y. [DOI] [PubMed] [Google Scholar]
- 14.Lee E. St. Louis, MO: Quality Medical Publishers; 1999. Traumatic injuries; pp. 1235–1261. [Google Scholar]
- 15.Ng A K, Simons R K, Torreggiani W C, Ho S G, Kirkpatrick A W, Brown D R. Intra-abdominal free fluid without solid organ injury in blunt abdominal trauma: an indication for laparotomy. J Trauma. 2002;52(06):1134–1140. doi: 10.1097/00005373-200206000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Miller B J, Schache D J. Colorectal injury: where do we stand with repair? Aust N Z J Surg. 1996;66(06):348–352. doi: 10.1111/j.1445-2197.1996.tb01208.x. [DOI] [PubMed] [Google Scholar]
- 17.Cirocchi R, Abraha I, Montedori A et al. Damage control surgery for abdominal trauma. Cochrane Database Syst Rev. 2010;(01):CD007438. doi: 10.1002/14651858.CD007438.pub2. [DOI] [PubMed] [Google Scholar]
- 18.Stone H H, Fabian T C. Management of perforating colon trauma: randomization between primary closure and exteriorization. Ann Surg. 1979;190(04):430–436. doi: 10.1097/00000658-197910000-00002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller P R, Chang M C, Hoth J J, Holmes J H, IV, Meredith J W.Colonic resection in the setting of damage control laparotomy: is delayed anastomosis safe? Am Surg 20077306606–609., discussion 609–610 [DOI] [PubMed] [Google Scholar]
- 20.Vertrees A, Wakefield M, Pickett C et al. Outcomes of primary repair and primary anastomosis in war-related colon injuries. J Trauma. 2009;66(05):1286–1291. doi: 10.1097/TA.0b013e31819ea3fc. [DOI] [PubMed] [Google Scholar]
- 21.Kashuk J L, Cothren C C, Moore E E, Johnson J L, Biffl W L, Barnett C C.Primary repair of civilian colon injuries is safe in the damage control scenario Surgery 200914604663–668., discussion 668–670 [DOI] [PubMed] [Google Scholar]
- 22.Weinberg J A, Griffin R L, Vandromme M J et al. Management of colon wounds in the setting of damage control laparotomy: a cautionary tale. J Trauma. 2009;67(05):929–935. doi: 10.1097/TA.0b013e3181991ab0. [DOI] [PubMed] [Google Scholar]
- 23.Ott M M, Norris P R, Diaz J J et al. Colon anastomosis after damage control laparotomy: recommendations from 174 trauma colectomies. J Trauma. 2011;70(03):595–602. doi: 10.1097/TA.0b013e31820b5dbf. [DOI] [PubMed] [Google Scholar]
- 24.Ordoñez C A, Pino L F, Badiel Met al. Safety of performing a delayed anastomosis during damage control laparotomy in patients with destructive colon injuries J Trauma 201171061512–1517., discussion 1517–1518 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Georgoff P, Perales P, Laguna B, Holena D, Reilly P, Sims C. Colonic injuries and the damage control abdomen: does management strategy matter? J Surg Res. 2013;181(02):293–299. doi: 10.1016/j.jss.2012.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Burlew C C, Moore E E, Cuschieri J et al. Sew it up! A Western Trauma Association multi-institutional study of enteric injury management in the postinjury open abdomen. J Trauma. 2011;70(02):273–277. doi: 10.1097/TA.0b013e3182050eb7. [DOI] [PubMed] [Google Scholar]
- 27.Bulger E M, McMahon K, Jurkovich G J. The morbidity of penetrating colon injury. Injury. 2003;34(01):41–46. doi: 10.1016/s0020-1383(02)00090-6. [DOI] [PubMed] [Google Scholar]
- 28.Crass R A, Salbi F, Trunkey D D. Colostomy closure after colon injury: a low-morbidity procedure. J Trauma. 1987;27(11):1237–1239. doi: 10.1097/00005373-198711000-00008. [DOI] [PubMed] [Google Scholar]
- 29.Livingston D H, Miller F B, Richardson J D. Are the risks after colostomy closure exaggerated? Am J Surg. 1989;158(01):17–20. doi: 10.1016/0002-9610(89)90306-1. [DOI] [PubMed] [Google Scholar]
- 30.Pachter H L, Hoballah J J, Corcoran T A, Hofstetter S R. The morbidity and financial impact of colostomy closure in trauma patients. J Trauma. 1990;30(12):1510–1513. doi: 10.1097/00005373-199012000-00012. [DOI] [PubMed] [Google Scholar]
- 31.Anjaria D J, Ullmann T M, Lavery R, Livingston D H.Management of colonic injuries in the setting of damage-control laparotomy: one shot to get it right J Trauma Acute Care Surg 20147603594–598., discussion 598–600 [DOI] [PubMed] [Google Scholar]
- 32.Adesanya A A, Ekanem E E. A ten-year study of penetrating injuries of the colon. Dis Colon Rectum. 2004;47(12):2169–2177. doi: 10.1007/s10350-004-0726-5. [DOI] [PubMed] [Google Scholar]
- 33.Murray J A, Demetriades D, Colson M et al. Colonic resection in trauma: colostomy versus anastomosis. J Trauma. 1999;46(02):250–254. doi: 10.1097/00005373-199902000-00009. [DOI] [PubMed] [Google Scholar]
- 34.Thompson J S, Moore E E, Moore J B. Comparison of penetrating injuries of the right and left colon. Ann Surg. 1981;193(04):414–418. doi: 10.1097/00000658-198104000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Fealk M, Osipov R, Foster K, Caruso D, Kassir A. The conundrum of traumatic colon injury. Am J Surg. 2004;188(06):663–670. doi: 10.1016/j.amjsurg.2004.08.057. [DOI] [PubMed] [Google Scholar]
- 36.Steele S R, Wolcott K E, Mullenix P S et al. Colon and rectal injuries during Operation Iraqi Freedom: are there any changing trends in management or outcome? Dis Colon Rectum. 2007;50(06):870–877. doi: 10.1007/s10350-007-0235-4. [DOI] [PubMed] [Google Scholar]
- 37.Steele S R, Maykel J A, Johnson E K. Traumatic injury of the colon and rectum: the evidence vs dogma. Dis Colon Rectum. 2011;54(09):1184–1201. doi: 10.1007/DCR.0b013e3182188a60. [DOI] [PubMed] [Google Scholar]


