Abstract
Background
A meta-analysis of studies from multiple countries has shown that the incidence of incisional hernia varies from 4% to 10% depending on the type of operation. No epidemiological surveys have been conducted so far. The worst possible complication of an incisional hernia if it is not treated surgically is incarceration. In this article, we present the main surgical methods of treating this condition. We also evaluate the available randomized and controlled trials (RCTs) in which open and laparoscopic techniques were compared and analyze the patients’ quality of life.
Methods
We selectively searched PubMed for relevant literature using the search terms “incisional hernia” and “randomized controlled trial.” 9 RCTs were included in the analysis. The endpoints of the meta-analysis were the number of reoperations, complications, and recurrences. The observed events were studied statistically by correlation of two unpaired groups with a fixed-effects model and with a random-effects model. We analyzed the quality of life in our own patient cohort preoperatively vs. 1 year postoperatively on the basis of data from the European Registry of Abdominal Wall Hernias (EuraHS).
Results
Open surgery and laparoscopic surgery for the repair of incisional hernias have similar rates of reoperation (odds ratio [OR] 0.419 favoring laparoscopy, 95% confidence interval [0.159; 1.100]; p = 0.077). The rates of surgical complications are also similar (OR 0.706; 95% CI [0.278; 1.783]; p = 0.461), although the data are highly heterogeneous, and the recurrence rates are comparable as well (OR 1.301; 95% CI [0,761; 2,225]; p = 0.336). In our own patient cohort in Würzburg, the quality of life was better in multiple categories one year after surgery.
Conclusion
The operative treatment of incisional hernia markedly improves patients’ quality of life. The currently available evidence regarding the complication rates of open and laparoscopic surgical repair is highly heterogeneous, and further RCTs on this subject would therefore be desirable. Moreover, new study models are needed so that well-founded individualized treatment algorithms can be developed.
The exact global incidence of incisional hernia is unknown. Presumably, the wide variation in abdominal approaches, comorbidities among patients and techniques for surgical closure of the abdominal wall leads to a broad range of incidence rates, significantly differing between the various patient populations. In 1985, Mudge and Hughes estimated the incidence of incisional hernia after abdominal surgery in a long-term prospective study to be 11%; however, at the end of the 10-year follow-up, only 60% of patients were available for analysis (1). In a meta-analysis on abdominal wall closure including 56 randomized controlled trials (RCTs) with altogether 14 618 patients of an international patient population, the incidence of incisional hernia occurring within 2 years after index surgery was calculated to be 12.8% (95% confidence interval [CI]: [11.4; 14.2]) (2). Since the surgical technique used for abdominal wall closure can significantly influence the incidence of incisional hernia, these data are to be interpreted on a relative basis (3– 5). Endoscopic surgery is associated with a lower incidence of incisional hernia: A meta-analysis of 34 RCTs including 3490 patients showed that incisional hernia is significantly less common after laparoscopic procedures compared to open surgery (4.3 vs. 10.1%; risk difference -0.06; 95% CI [-0.09; -0.03]; p = 0.0002]) (6).
For Germany, too, only estimates are available. Data of the German diagnosis-related groups (DRG) system do not allow to draw any conclusions about procedures per surgery day or anesthesia. Due to this lack of information, incidence and prevalence rates of incisional hernia in the general population can only be indirectly estimated. Data of the German Federal Statistical Office suggest that approximately 703 000 laparoscopic und approximately 743 000 open procedures with access via the abdominal wall were performed in 2015. These numbers include procedures of:
vascular surgery (e.g. open repair surgery for abdominal aortic aneurysm)
gynecology (e.g. diagnostic laparoscopies or -Meigs operation)
urology (e.g. transabdominal prostate resections or nephrectomies)
visceral surgery.
On the basis of the above-mentioned incidence rates for incisional hernia, approximately 104 000 newly diagnosed cases per year can be expected in Germany, provided each coded procedure is only to be allocated to one surgery day / abdominal approach.
In 2015, 50 521 incisional hernia repair procedures were coded in Germany, of which 10 732 were performed laparoscopically (21%). These figures at least show that data collected for the billing purposes are incomplete and do not allow to draw more precise conclusions on incisional hernia incidence and prevalence beyond the general statement that it is a common condition (7).
Clinical presentation and indication for surgery
A certain percentage of patients is not aware of their hernia (asymptomatic). In our experience, incisional hernia is often only diagnosed during cancer follow-up examinations. In personal communications, this observation has been confirmed by various European surgeons. Patients with incisional hernia usually report rather unspecific symptoms and occasionally experience pain and gastrointestinal problems, such as a postprandial feeling of fullness. Larger hernias may be associated with lesions of the skin overlying the hernia sac or with chronic spinal complaints. If the hernia sac is large, a portion of the small intestine may protrude through the abdominal wall, significantly complicating surgical repair.
It is not uncommon that patients with incisional hernia experience social exclusion and are limited in their ability to work. In addition, self-care may be substantially impaired.
The most severe complication which may occur in the natural course of untreated incisional hernia is incarceration which is estimated to affect 6 to 15% of cases (8). Presumably, the number of unreported cases is higher. In our own patient population of the University Hospital of Würzburg, 64 of 401 incisional hernias repaired between 2013 and 2016 were non-reducible (15.9%); of these, 26 (6.5%) required emergency surgery. Seven of the 26 patients who underwent emergency procedures (24.2%) required bowel resection compared to 34 (9.1%) among the 372 patients with elective incisional hernia repairs. The exact incidence of complicated incisional hernia is to be established in the future, using, for example, centralized data collection and analysis with data linked to patient identification numbers.
A Swedish RCT comparing open with laparoscopic incisional hernia repairs focused on quality of life preoperatively and 1 year after surgery. It found that 8 weeks after surgery all patients, regardless of the surgical technique used, reported a quality of life comparable to that of the general Swedish population. This gain in quality of life was still present after one year. Likewise, measurable symptom improvement was achieved by surgery: In the Swedish study, 81% of patients experienced symptoms preoperatively, compared to only 18% one year postoperatively (p<0.001). Surgery resulted in significant improvements in the following parameters (p<0.001, respectively):
movement restrictions
fatigue
visual analog scale (VAS) pain score.
However, at one year after surgery, 12% of patients continued to report daily complaints. 75% of patients were “definitively satisfied“ with the outcome, while 7% were “unsatisfied“ and 1% “definitively unsatisfied“ (9). Satisfaction after surgery was similar in the prospectively assessed own patient population of the European Registry of Abdominal Wall Hernias (EuraHS) (etable).
eTable. Quality of life according to EuraHS Quality of Life Score (e10) in the preoperative and postoperative course in our own patient population from Würzburg, Germany (2013–2016).
| Timing | Preoperative | 1-year postoperative | ||||||
| Qol category | QoL criterion | N | Mean | [95% CI] | N | Mean | [95% CI] | p |
| Pain *1 | at rest | 336 | 1.36 | [1.08; 1.64] | 125 | 0,43 | [0.18; 0.68] | 0.0005 |
| during motion | 336 | 2.35 | [2.04; 2.67] | 125 | 0,98 | [0.59; 1.36] | 0.0001 | |
| last week’s most severe pain | 336 | 2.71 | [2.35; 3.07] | 125 | 0,98 | [0.58; 1.37] | <0.0001 | |
| Impairment *2 | of activities at home | 331 | 3.24 | [2.89; 3.58] | 122 | 1,07 | [0.68; 1.45 | <0.0001 |
| of activities outside the home | 321 | 2.58 | [2.25; 2.91] | 120 | 0,87 | [0.51; 1.24 | <0.0001 | |
| of sporting activities | 163 | 2.10 | [1.64; 2.56] | 69*4 | 1,33 | [0.75; 1.90 | 0.0693 | |
| of hard physical work | 295 | 3.67 | [3.29; 4.04] | 105 | 1,29 | [0.80; 1.77 | <0.0001 | |
| Cosmetic*3 | Shape of abdomen | 336 | 6.04 | [5.80; 6.29] | 114 | 4,96 | [4.56; 5.35 | <0.0001 |
| Shape of hernia | 336 | 7.82 | [7.61; 8.04] | 124 | 3,74 | [3.30; 4.18 | <0.0001 | |
*1 Scale from 0–10: 0 = no pain to 10 = most severe pain
*2 Scale from 1–10: 0 = no impairment to 10 = unable to perform the activity
*3 Scale from 1–10: 0 = very satisfied to 5 = satisfied to 10 = very unsatisfied
*4 Almost half of the patients did not engage in sporting activities, neither preoperatively nor at 1 year postoperatively.
EuraHS, Hernia Registry of the European Hernia Society; CI, confidence interval; N, number of patients; p, paired, two-sided t-test; QoL, quality of life
However, at one year after surgery, 12% of patients continued to report daily complaints. 75% of patients were “definitively satisfied“ with the outcome, while 7% were “unsatisfied“ and 1% “definitively unsatisfied“ (9). Satisfaction after surgery was similar in the prospectively assessed own patient population of the European Registry of Abdominal Wall Hernias (EuraHS) (etable).
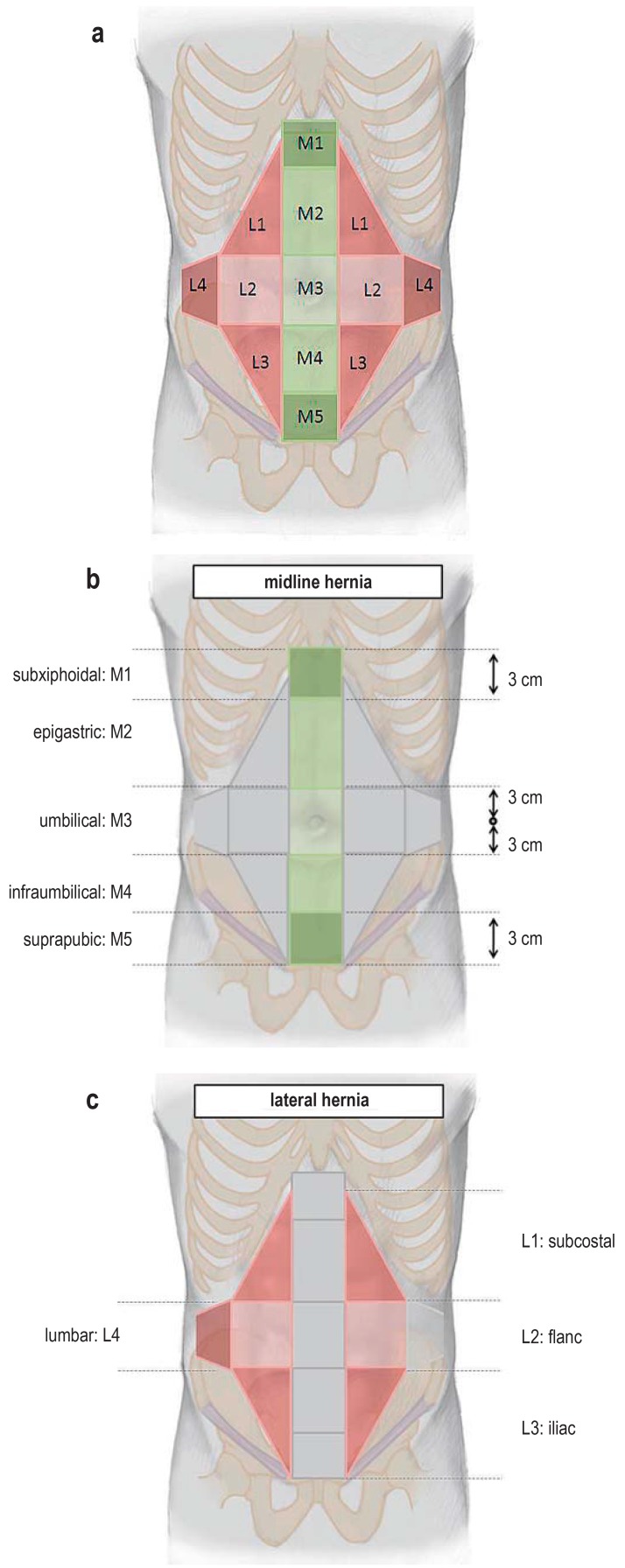
The overall evaluation of patient complaints and complication risk associated with the natural course of incisional hernia raises the question of whether watchful waiting could be an alternative to elective repair in certain patient groups. This question is currently being addressed in the German Research Foundation (DFG, Deutsche Forschungsgemeinschaft)-sponsored multicenter AWARE study which has so far screened more than 2000 patients and included more than 250 patients. However, it has already become apparent that the number of cross-over patients from the watchful-waiting arm to the surgery arm is high (10). Timing of surgery should not only be based on patient complaints, but also take into account the morphology/size of the abdominal wall defect and the risk profile of the individual patient (e.g., age, obesity and tobacco use). For this, standardized classification of clinical findings is of prognostic relevance (11, 12) (eFigure). The size of the abdominal wall defect is an independent factor for the incidence of postoperative complications and recurrences. The risk of mesh-related complications is directly proportional to the size of the mesh placed (13– 15). With regard to gain in quality of life, perioperative morbidity and likelihood of recurrence, there is evidence to support an early indication for surgery (also with smaller lesions). While quality of life as a subjective factor may theoretically be affected by regression-to-the-mean bias, low morbidity and recurrence rates are definite advantages of early elective surgery (16).
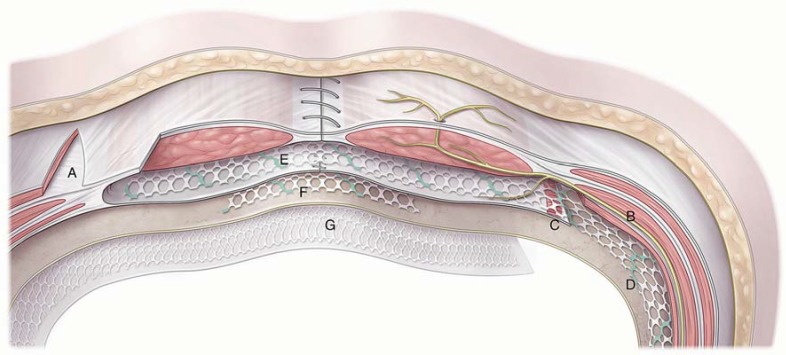
Figure 1.
Transverse section of the supraumbilical abdominal wall, showing relevant anatomical structures and mesh locations for incisional hernia repair. A) Releasing incision of the abdominal external oblique aponeurosis as part of the component separation technique described by Ramirez. B) Typical course of an intercostal nerve between the transversus abdominis muscle and the abdominal internal oblique muscle; the nerve enters at the lateral margin of the rectus sheath into the rectus abdominis muscle and gives off a cutaneous branch at its end. C) During transversus abdominis release (TAR) for positioning a mesh lateral to the rectus sheath, the course of this nerve has to be spared to prevent subsequent abdominal wall paralysis. D) With TAR, the mesh is placed between peritoneum and transversus abdominis muscle. E) Typical sublay mesh position (retromuscular). F) Underlay mesh position (preperitoneal). G) Intraperitoneal mesh position (IPOM = intraperitoneal onlay mesh). (Courtesy of Maren Hötten/Scientific Illustration)
Surgical techniques
Incisional hernia repair involves the use of a synthetic mesh and can be performed by conventional (open) surgery or minimally-invasive (laparoscopic) surgery (17, 18). Currently used surgical techniques as well as the Figures 1 and 2 are described in detail in the eSupplement Surgical Techniques.
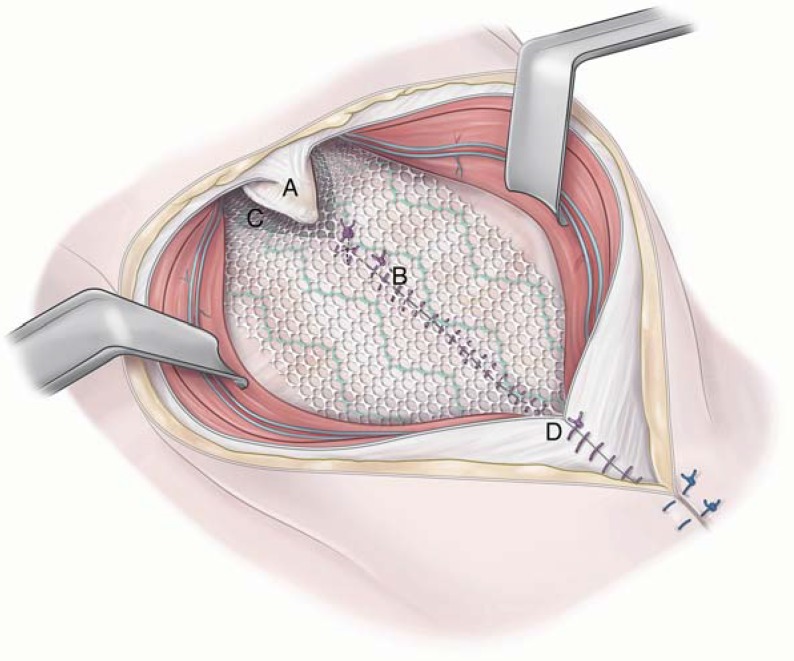
Figure 2.
With retromuscular mesh repair of midline incisional hernia, it is crucial to ensure a mesh overlap extending underneath the xiphoid to prevent recurrence. A) Xiphoid process; B) Posterior rectus sheath closed in the midline. Due to the midline xiphoid process insertion of the rectus sheath, a so-called fatty triangle (D) is created during the release of the posterior rectus sheath from the xiphoid. At the end of the mesh repair, this triangle is only secured by the synthetic mesh (D). With proper dissection, the mesh overlap underneath the xiphoid process extends several centimeters in cranial direction. C) Anterior rectus sheath. (Courtesy of Maren Hötten/Scientific Illustration)
Outcomes of the surgical techniques
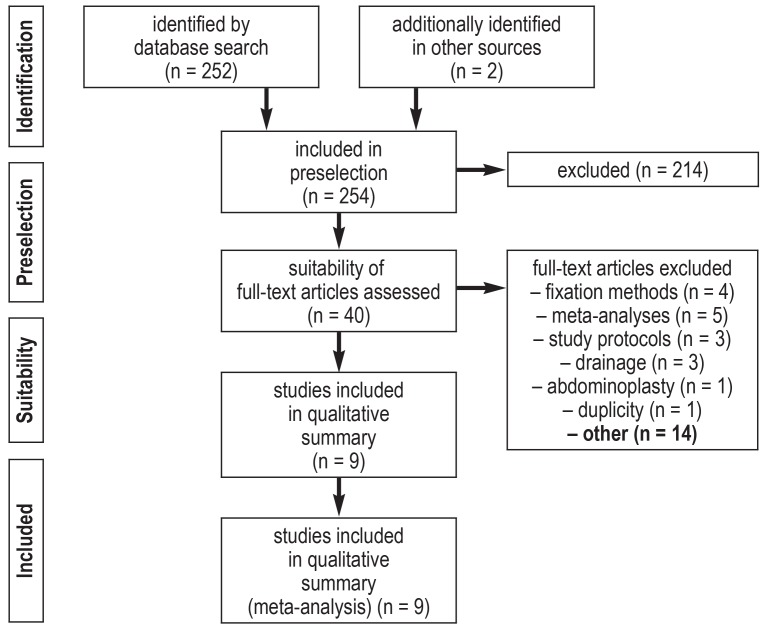
In some patients the question arises whether an open or laparoscopic technique should be used. To address this question, we performed a meta-analysis in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (19). A PubMed search was conducted for English-language articles published up to and including June 2017, using the MeSH terms “incisional hernia“ and “randomized controlled trial“ (efigure 1). In addition, the references sections of relevant meta-analyses were scrutinized for further RCTs. We included only RCTs in our meta-analysis (9, 20– 27). The endpoints were number of revision procedures, general complications and recurrence rate. Analyses were performed using the Comprehensive Meta-Analysis software (version 3.3.070). The data included were the events observed in the respective RCTs in correlation to two unpaired groups (open vs. laparoscopic), with a fixed-effects model. In case of high heterogeneity (I2>75%), a random-effects model was chosen.
eFigure 1.
PRISMA flow chart of literature search to identify publications comparing open versus laparoscopic incisional hernia repair (PRISMA, preferred reporting items for systematic review and meta-analyses)
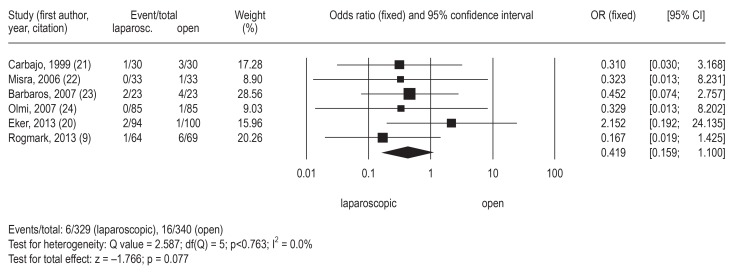
The reoperation rate associated with the index surgery is a measurable surrogate for complications. The comparison of the laparoscopic versus open approach found a trend in favor of the laparoscopic technique, lacking statistical significance (figure 1). In view of the overall result, the high reoperation rate after laparoscopic procedures reported in the study by Eker et al., exceeding those observed in all other RCTs, seems odd (28). With the Eker study excluded from the analysis, the reoperation rate after laparoscopic procedures is significantly lower compared to the rate after open surgery (odds ratio [OR] 0.307; 95% CI: [0.107; 0.880]; p = 0.028 [fixed-effects model]; I2= 0.0%).
With regard to complication rate, the available data are similar. In the study by Eker et al. (2013), the complication rate for laparoscopic procedures was disproportionately high compared to the complication rates in the literature (20). There are two possible explanations:
It was a multicenter trial with 9 participating centers in the early stage of the learning curve (patient inclusion interval: 1999–2006)
complications included, for example, postoperative pain, while in the other studies only problems related to surgical technique and surgical wound-healing disturbances were listed.
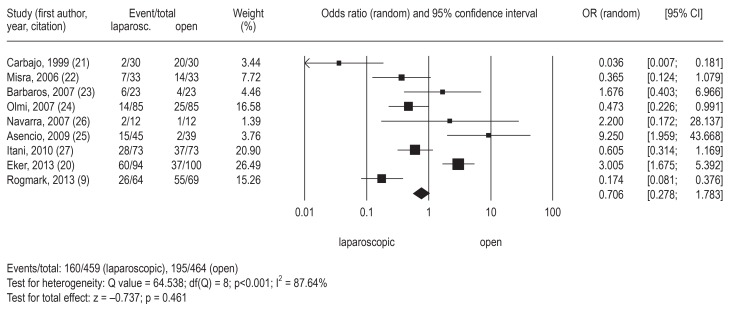
Due to the high degree of heterogeneity among complication data—which can be explained, on the one hand, by the fact that there is little overlapping of confidence intervals and, on the other hand, by the limited number of available RCTs—the advantage of laparoscopic procedures with regard to complications was not statistically significant, despite an OR of 0.706 (figure 4) If data from the Eker study are not included in the analysis, OR improves to 0.555 (95% CI: [0.234; 1.318]), but the heterogeneity remains high (I2= 80.26%) and the advantage is still not statistically significant in the random effects model (z = -1.335; p = 0.182) (figure 4). Further RCTs are clearly needed.
Figure 4.
Complications in the comparison of laparoscopic and open technique (p = 0.461). CI, confidence interval; OR, odds ratio; laparosc., laparoscopic
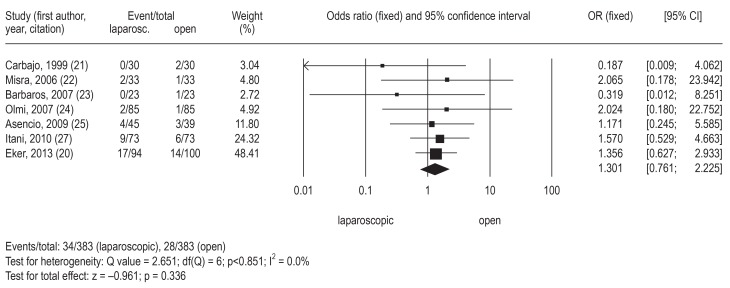
In line with the findings of other meta-analyses (28, 29), our current meta-analysis has shown that both surgical techniques had comparable recurrence rates over the postoperative course (figure 5). There is partial overlapping of our meta-analysis with those of Sajid et al. (28) and of Awaiz et al. (29): Our meta-analysis complements the first meta-analysis by including RTCs published between 2006 and 2013 and differs from the second meta-analysis in the way that we excluded the RCT by Rogmark et al. with regard to the “recurrence” outcome as it did not assess the “recurrence” endpoint in the first place (9).
Figure 5.
Recurrence rate in the comparison of laparoscopic and open technique (p = 0.336). CI, confidence interval; OR, odds ratio; laparosc., laparoscopic
Relevant to prognosis is the finding that after two years 8 to 12% of patients had developed a recurrence; consequently, we are not yet in the position to speak of “surgical cure by mesh”. However, recurrence rates after open repair tend to be lower compared to those after laparoscopic surgery (27).
The analysis of the quality of life (QoL) data of our own patient population from the European Registry of Abdominal Wall Hernias (EuraHS), comparing preoperative data with 1-year postoperative data, found significant improvements of satisfaction for the criteria “pain“, “restrictions of daily activities“ and “cosmetic discomfort“ (etable). The only exception is “sporting activity“ where satisfaction tended to increase; however, almost half of the patients does normally not engage in sporting activities. The primary factor to influence the gain in quality of life after surgery is postoperative pain. The mesh fixation technique may have an effect on pain. An RCT (n = 199) compared 3 different techniques of mesh fixation with regard to postoperative pain:
helical tacks (titanium)
absorbable transfascial sutures
non-absorbable transfascial sutures.
At the 3-month follow-up, no differences were found between the VAS pain scores (30). In a second RCT (n = 68), helical tack fixation in 2 concentric rows (titanium, double-crown technique) caused significantly more pain over a period of up to 3 months postoperatively compared to permanent transfascial sutures (polypropylene) (31). A more recent RCT evaluated another variant of fixation with regard to postoperative pain (VAS): (titanium) helical tack in double-crown technique versus a combination of (titanium) helical tacks and transfascial sutures. The prevalence of abdominal pain after 3 months was significantly lower in patients with helical tacks in double-crown technique (8.3% vs 31.4%) (32). These studies were monocentric trials from very different regions and it remains unknown whether one of the fixation technique causes less pain than the others. It is likely that with increasing number of fixation points the tensile forces acting on the mesh are distributed to more points, resulting in reduced pain regardless of the fixation technique used.
In our own patient population (N = 486), we addressed the question whether the complication rate of high-risk patients can be aligned to that of low-risk patients, using a heuristic approach. In order to reach this goal, high-risk patients were preferably treated with laparoscopic surgery, while younger patients and patients with less comorbidities preferably underwent morphological and functional abdominal wall reconstruction with sublay mesh repair. As due to the nature of the research question randomization was impossible, a propensity score analysis was performed. Following propensity score adjustment, the results showed for the first time that providing personalized advice about the most suitable surgical technique aligns the complication prognoses on a lower complication level (33). In the future, new statistical algorithms will have to provide instruments for advanced prospective clinical trials overcoming the methodological limitations of RCTs and focusing on variability and personalized treatment.
In Germany in 2015, lethality of open repair of incisional hernia was 2.24% (894 deaths/39 787 procedures) and of laparoscopic repair 0.298% (32 deaths /10 732 procedures) (7). It is possible that in some patients the incisional hernia closure was coded as a secondary procedure. This would have caused a false-positive increase in mortality rate.
There is insufficient evidence to support recommendations regarding the best time to resume full activity after surgery. Physical exertion increases the intraabdominal pressure and correspondingly the tensile forces distributed on the mesh reconstruction (34). While the universal recommendation to avoid lifting and carrying weights of >10 kg during the first 3 months appears to be adequate after open reconstruction, it may not be justified after laparoscopic surgery (35). Normally, we assume that 6 weeks after surgery the abdominal wall has healed enough to withstand higher intraabdominal pressure and we allow lifting and carrying as tolerated by the patient. Patients with office jobs often resume work after only 1 week.
Conclusion
The great challenge of incisional hernia surgery remains to reconcile the variability of the condition (e.g. risk factors and hernia characteristics) with the surgical options available (e.g. surgical techniques, surgical materials and expertise). As in all fields of medicine, the variability of the condition makes tailoring treatment to the patient and generating evidence difficult. However, this balancing act has been performed more successfully in recent years, as shown in the highly recommended review by Berger (36) which complements the topic. Reintegration of patients into the labor market is influenced by the following parameters:
clinical picture / signs and symptoms
impairment of quality of life
individual risk factors
morphology of the hernial orifice
size of the hernia sac and hernial orifice
restoration of abdominal wall function.
Advances in surgical techniques have opened a whole new range of possibilities: Both the use of hybrid/conventional-endoscopic procedures (e.g. EMILOS) (37) and surgical robots have enabled us for the first time to place mesh in a retromuscular position (e.g. r-TAR) (38). Last but not least, prevention of incisional hernia, e. g. by refining the technique of abdominal wall closure (3) or prophylactic mesh placement in high-risk patients (39), will be of particular importance in the future.
Supplementary Material
eSUPPLEMENT SURGICAL TECHNIQUES
Scar tissue has to be reinforced mechanically by placement of a mesh. The mesh can be placed in various ways. There is no generally superior surgical technique. It is essential to identify on an individual basis which surgical strategy (for example, surgical access) is required for a patient. The factors to be taken into account in the individual patient vary widely. Only the overall evaluation of the factors involved (symptoms, urgency, morphology of the hernial orifice, size of the defect, quality of the connective tissue, tobacco use, diabetes mellitus, obesity, and age, among others) will clearly identify the individual treatment concept (13, 16).
On the one hand, it may well be that a comparable incisional hernia is treated with open reconstruction in a young patient (with few risk factors for complications), while it should be treated laparoscopically in an older patient (with multiple risk factors for complications). On the other hand, even a patient with multiple risk factors for complication may require open surgery associated with a high risk of complications, if, for example, surgery had been delayed for too long and the hernia had become very large. Establishing the indication for surgery in an individual patient is always the result of harmonizing the following parameters:
The recurrence rate after incisional hernia repair with mesh is significantly lower compared to other suturing techniques. In a randomized controlled trial (RCT) by Burger et al., the recurrence rate associated with suture repair amounted to 67% compared to 17% after mesh repair (e1). With the publication of that study at the latest, the use of permanent, non-absorbable mesh to reinforce incisional hernia repair became the standard of care. Current long-term data from the Danish Hernia Register show that the recurrence rate is significantly lower after mesh repair (15). At present, meshes made of polypropylene (PP), polyester (PES), polyvinylidene fluoride (PVDF), and polytetrafluoroethylene (PTFE) are commercially available. These meshes can be anatomically placed in various layers of the abdominal wall (figure 1). The best long-term results with regard to the lowest risk of recurrence were achieved with the following locations for mesh placement: sublay/retromuscular (Figure 1e), preperitoneal (Figure 1f) and intraperitoneal (IPOM) (Figure 1g) (e2).
Sublay mesh placement is particularly suitable for midline incisional hernia repair and can be described as a morphologically and functionally reconstructive technique (Figure 1e): The posterior sheath of the rectus abdominis muscle is released bilaterally and sutured to the opposite side. A tailored mesh is then placed in this newly created retromuscular space. Subsequently, the anterior rectus sheath is closed above it. The mesh is held in place between the layers by the intraabdominal pressure and stabilizes the scar, provided sufficient overlapping of the midline (Figure 1e). Here, it is crucial to ensure adequate cranial extension of the mesh overlap underneath the xiphoid process to cover the so-called “fatty triangle” (figure 2) and caudal extension into the retropubic space (space of Retzius).
In Germany, the school of Aachen led by Volker Schumpelick and Joachim Conze has raised awareness of this procedure and advanced the surgical technique (e3). If the diameter of the hernial orifice is larger than 12 cm, it can be necessary to perform a lateral relaxation incision along the aponeurosis of the external oblique muscle as described by Oscar Ramirez (Figure 1a) (e4). In special cases, it is not possible to achieve adequate lateral mesh overlapping. In this situation, it is necessary to extend the dissection layer in the area of the lateral edge of the rectus sheath: With the transversus abdominis release (TAR) technique (e5, e6) (Figures 1c and 1d), it is possible to enter a lateral extraperitoneal compartment, while sparing the intercostal nerves (Figure 1b).
The great advantage of retromuscular mesh placement is the extraperitoneal location of the synthetic mesh. This helps to reduce or prevent adhesions affecting bowel function and the development of enteroprosthetic fistula as well as inflammatory mesh deterioration, as the mesh is extraperitonealized. The disadvantage of this reconstruction principle is that it requires extensive dissection with resulting insufficient blood supply to the skin (skin necrosis, impaired wound healing). It is also associated with an increased risk of revision surgery (e.g. post-operative hemorrhage). The meta-analysis by Holihan et al. provides a good overview of mesh locations used with open surgery (e2). Inlay and onlay mesh repair techniques are to be rejected as they are associated with significantly poorer outcomes with regard to recurrence rate and wound complications compared to sublay mesh repair (e2).
With the advent of minimally invasive surgery, the laparoscopic mesh repair technique was developed (synonym: Intraperitoneal Onlay Mesh Repair [IPOM]) (e7): The mesh is placed between the abdominal wall and the intestines or omentum (Figure 1g). With this technique, the hernial orifice is not necessarily closed; the mesh serves as an extension (or replacement) of the abdominal wall. The challenges of this technique are mesh fixation and proper mesh overlap which needs to be proportional to the size of the hernial orifice: the larger the hernial orifice, the wider the required radial mesh overlap (e8). Here, two additional factors play an important role:
Surgeons performing laparoscopic procedures should have special expertise in adhesiolysis which is often required. This is also highlighted in the guidelines of the International Endo-Hernia Society (e9).
urgency of surgery
patient expectations placed on surgery
dedicated surgical technique and materials, and
individual expertise of the surgeon (17).
proper parietalization of the anterior abdominal wall (i.e. release of the falciform ligament und infraumbilical folds) and
adequate transfascial mesh fixation and/or use of tackers (absorbable or permanent) (16).
Figure 3.
Reoperation rate in the comparison of laparoscopic and open technique (p = 0.077). CI, confidence interval; OR, odds ratio; laparosc., laparoscopic
Key Messages.
Incisional hernia occurs in 4 to 10% of patients after abdominal surgery and is usually asymptomatic. In Germany, the incidence of incisional hernia is estimated to be approximately 104 000..
Early surgical treatment even of asymptomatic incisional hernia appears to be appropriate since the smaller the hernia the lower morbidity and recurrence rate.
Incisional hernia repair involves placing a mesh and is performed either as an open procedure (morphological and functional abdominal wall reconstruction with sublay mesh placement) or as a minimally invasive procedure (laparoscopic surgery with mesh placed in the intraperitoneal onlay mesh [IPOM] position).
Comparison of the various surgical techniques found no significant differences, neither for reoperation rate nor for complication and recurrence rates. The best surgical technique for a patient has to be decided on an individual basis.
Surgical treatment of incisional hernia improves quality of life and satisfaction with the shape of the abdominal wall in patients. Depending on the size of the repair and the surgical technique, patients are allowed to resume full activity 3 to 6 weeks after surgery.
eFigure 2.
Consensus classification of incisional hernia of the European Hernia Society (EHS) (2009)
a) Morphologically, it is distinguished between midline (M1–5) and lateral (L1–4, right or left) hernias.
b) The location of midline hernias is allocated to the zones M1 to M5, based on the proximity of the hernia to the xiphoid process, umbilicus or symphysis pubis; a hernial orifice can extend over several areas, e.g. M1 to 3 or M3 to 5.
c) Anatomically, lateral hernias are allocated to the zones L1 to L4 and labelled according their side. For the purpose of standardization, hernias are to be classified intraoperatively. The size of the hernial orifice is measured in “length” and “width“. Since width is of particular prognostic relevance, the size of the hernial orifice is categorized according to width (W) in W1 (<4 cm), W2 (4–10 cm) or W3 (>10 cm).
(EuraHS, the Hernia Registry of the European Hernia Society uses this classification [www.eurahs.eu]; modified according to [12] and [e10]; courtesy of Springer-Verlag/the authors of the two articles [12] and [e10])
Acknowledgments
Translated from the original German by Ralf Thoene, MD.
Footnotes
Conflict of interest
The authors declare no conflict of interest.
References
- 1.Mudge M, Hughes LE. Incisional hernia: a 10 year prospective study of incidence and attitudes. Br J Surg. 1985;72:70–71. doi: 10.1002/bjs.1800720127. [DOI] [PubMed] [Google Scholar]
- 2.Bosanquet DC, Ansell J, Abdelrahman T, et al. Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14,618 Patients. PLoS ONE 10(9): doi: 10.1371/journal.pone.0138745. e0138745. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Millbourn D, Cengiz Y, Israelsson LA. Effect of stitch length on wound complications after closure of midline incisions: a randomized controlled trial. Arch Surg. 2009;144:1056–1059. doi: 10.1001/archsurg.2009.189. [DOI] [PubMed] [Google Scholar]
- 4.Deerenberg EB, Harlaar JJ, Steyerberg EW, et al. Small bites versus large bites for closure of abdominal midline incisions (STITCH): a double-blind, multicentre, randomised controlled trial. Lancet. 2015;386:1254–1260. doi: 10.1016/S0140-6736(15)60459-7. [DOI] [PubMed] [Google Scholar]
- 5.Muysoms FE, Antoniou SA, Bury K, et al. European Hernia Society guidelines on the closure of abdominal wall incisions. Hernia. 2015;19:1–24. doi: 10.1007/s10029-014-1342-5. [DOI] [PubMed] [Google Scholar]
- 6.Kössler-Ebs JB, Grummich K, Jensen K, et al. Incisional hernia rates after laparoscopic or open abdominal surgery—a systematic review and meta-analysis. World J Surg. 2016;40:2319–2330. doi: 10.1007/s00268-016-3520-3. [DOI] [PubMed] [Google Scholar]
- 7.Statistisches Bundesamt Gesundheit. Statistisches Bundesamt. Wiesbaden: 2016. DRG-Statistik 2015 - Vollstationäre Patientinnen und Patienten in Krankenhäusern. Operationen und Prozeduren (OPS Version 2015). A) Operationen und Prozeduren nach Altersgruppen, 5-380 bis 5-759, 6-Steller. B) Sterbefälle nach Alter: 5-536. [Google Scholar]
- 8.Conze J, Klinge U, Schumpelick V. Narbenhernien. Chirurg. 2005;76:897–910. doi: 10.1007/s00104-005-1072-4. [DOI] [PubMed] [Google Scholar]
- 9.Rogmark P, Petersson U, Bringman S, et al. Short-term outcomes for open and laparoscopic midline incisional hernia repair: a randomized multicenter controlled trial: the ProLOVE (prospective randomized trial on open versus laparoscopic operation of ventral eventrations) trial. Ann Surg. 2013;258:37–45. doi: 10.1097/SLA.0b013e31828fe1b2. [DOI] [PubMed] [Google Scholar]
- 10.Lauscher JC, Leonhardt M, Martus P, et al. Beobachtung vs. Operation Oligosymptomatischer Narbenhernien - Aktueller Stand der AWARE-Studie. Chirurg. 2016;87:47–55. doi: 10.1007/s00104-015-0011-2. [DOI] [PubMed] [Google Scholar]
- 11.Dietz UA, Hamelmann W, Winkler MS, et al. An alternative classification of incisional hernias enlisting morphology, body type and risk factors in the assessment of prognosis and tailoring of surgical technique. J Plast Reconstr Aesthet Surg. 2007;60:383–388. doi: 10.1016/j.bjps.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 12.Muysoms FE, Miserez M, Berrevoet F, et al. Classification of primary and incisional abdominal wall hernias. Hernia. 2009;13:407–414. doi: 10.1007/s10029-009-0518-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dietz UA, Winkler MS, Härtel RW, et al. Importance of recurrence rating, morphology, hernial gap size, and risk factors in ventral and incisional hernia classification. Hernia. 2014;18:19–30. doi: 10.1007/s10029-012-0999-x. [DOI] [PubMed] [Google Scholar]
- 14.Helgstrand F, Rosenberg J, Kehlet H, et al. Nationwide prospective study of outcomes after elective incisional hernia repair. J Am Coll Surg. 2013;216:217–228. doi: 10.1016/j.jamcollsurg.2012.10.013. [DOI] [PubMed] [Google Scholar]
- 15.Kokotovic D, Bisgaard T, Helgstrand F. Long-term recurrence and complications associated with elective incisional hernia repair. JAMA. 2016;316:1575–1582. doi: 10.1001/jama.2016.15217. [DOI] [PubMed] [Google Scholar]
- 16.Bland JM, Altman DG. Regression towards the mean. BMJ. 1994;308 doi: 10.1136/bmj.308.6942.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Dietz UA, Muysoms FE, Germer CT, Wiegering A. Technische Prinzipien der Narbenhernienchirurgie. Chirurg. 2016;87:355–365. doi: 10.1007/s00104-016-0158-5. [DOI] [PubMed] [Google Scholar]
- 18.Dietz UA, Wiegering A, Germer CT. Indikationen zur laparoskopischen Versorgung großer Narbenhernien. Chirurg. 2015;86:338–345. doi: 10.1007/s00104-014-2814-y. [DOI] [PubMed] [Google Scholar]
- 19.Ziegler A, Antes G, König IR. Bevorzugte Report Items für systematische Übersichten und Meta-Analysen: das PRISMA Statement. Dtsch Med Wochenschr. 2011;136:e9–e15. [Google Scholar]
- 20.Eker HH, Hansson BM, Buunen M, et al. Laparoscopic vs open incisional hernia repair: a randomized clinical trial. JAMA Surg. 2013;148:259–263. doi: 10.1001/jamasurg.2013.1466. [DOI] [PubMed] [Google Scholar]
- 21.Carbajo MA, Martín del Olmo JC, Blanco JI, et al. Laparoscopic treatment vs open surgery in the solution of major incisional and abdominal wall hernias with mesh. Surg Endosc. 1999;13:250–252. doi: 10.1007/s004649900956. [DOI] [PubMed] [Google Scholar]
- 22.Misra MC, Bansal VK, Kulkarni MP, et al. Comparison of laparoscopic and open repair of incisional and primary ventral hernia: results of a prospective randomized study. Surg Endosc. 2006;20:1839–1845. doi: 10.1007/s00464-006-0118-0. [DOI] [PubMed] [Google Scholar]
- 23.Barbaros U, Asoglu O, Seven R, et al. The comparison of laparoscopic and open ventral hernia repairs: a prospective randomized study. Hernia. 2007;11:51–56. doi: 10.1007/s10029-006-0160-9. [DOI] [PubMed] [Google Scholar]
- 24.Olmi S, Scaini A, Cesana GC, et al. Laparoscopic versus open incisional hernia repair: an open randomized controlled study. Surg Endosc. 2007;21:555–559. doi: 10.1007/s00464-007-9229-5. [DOI] [PubMed] [Google Scholar]
- 25.Asencio F, Aguiló J, Peiró S, et al. Open randomized clinical trial of laparoscopic versus open incisional hernia repair. Surg Endosc. 2009;23:1441–1448. doi: 10.1007/s00464-008-0230-4. [DOI] [PubMed] [Google Scholar]
- 26.Navarra G, Musolino C, De Marco ML, et al. Retromuscular sutured incisional hernia repair: a randomized controlled trial to compare open and laparoscopic approach. Surg Laparosc Endosc Percutan Tech. 2007;17:86–90. doi: 10.1097/SLE.0b013e318030ca8b. [DOI] [PubMed] [Google Scholar]
- 27.Itani KM, Hur K, Kim LT, et al. Comparison of laparoscopic and open repair with mesh for the treatment of ventral incisional hernia: a randomized trial. Arch Surg. 2010;145:322–328. doi: 10.1001/archsurg.2010.18. [DOI] [PubMed] [Google Scholar]
- 28.Sajid MS, Bokhari SA, Mallick AS, et al. Laparoscopic versus open repair of incisional/ventral hernia: a meta-analysis. Am J Surg. 2009;197:64–72. doi: 10.1016/j.amjsurg.2007.12.051. [DOI] [PubMed] [Google Scholar]
- 29.Awaiz A, Rahman F, Hossain MB, et al. Meta-analysis and systematic review of laparoscopic versus open mesh repair for elective incisional hernia. Hernia. 2015;19:449–463. doi: 10.1007/s10029-015-1351-z. [DOI] [PubMed] [Google Scholar]
- 30.Wassenaar E, Schoenmaeckers E, Raymakers J, et al. Mesh-fixation method and pain and quality of life after laparoscopic ventral or incisional hernia repair: a randomized trial of three fixation techniques. Surg Endosc. 2010;24:1296–1302. doi: 10.1007/s00464-009-0763-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bansal VK, Misra MC, Kumar S. A prospective randomized study comparing suture mesh fixation versus tacker mesh fixation for laparoscopic repair of incisional and ventral hernias. Surg Endosc. 2011;25:1431–1438. doi: 10.1007/s00464-010-1410-6. [DOI] [PubMed] [Google Scholar]
- 32.Muysoms F, Vander Mijnsbrugge G, Pletinckx P. Randomized clinical trial of mesh fixation with „double crown“ versus „sutures and tackers“ in laparoscopic ventral hernia repair. Hernia. 2013;17:603–612. doi: 10.1007/s10029-013-1084-9. [DOI] [PubMed] [Google Scholar]
- 33.Dietz UA, Fleischhacker A, Menzel S, et al. Risk-adjusted procedure tailoring leads to uniformly low complication rates in ventral and incisional hernia repair: a propensity score analysis and internal validation of classification criteria. Hernia. 2017;21:569–582. doi: 10.1007/s10029-017-1622-y. [DOI] [PubMed] [Google Scholar]
- 34.Gerten KA, Richter HE, Wheeler TL 2nd, et al. Intraabdominal pressure changes associated with lifting: implications for postoperative activity restrictions. Am J Obstet Gynecol. 2008;198:306.e1–306e5. doi: 10.1016/j.ajog.2007.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Buhck H, Untied M, Bechstein WO. Evidence-based assessment of the period of physical inactivity required after inguinal herniotomy. Langenbecks Arch Surg. 2012;397:1209–1214. doi: 10.1007/s00423-012-1008-7. [DOI] [PubMed] [Google Scholar]
- 36.Berger D. Evidence-based hernia treatment in adults. Dtsch Arztebl Int. 2016;113:150–158. doi: 10.3238/arztebl.2016.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Schwarz J, Reinpold W, Bittner R. Endoscopic mini/less open sublay technique (EMILOS)-a new technique for ventral hernia repair. Langenbecks Arch Surg. 2017;4021:73–80. doi: 10.1007/s00423-016-1522-0. [DOI] [PubMed] [Google Scholar]
- 38.Martin-Del-Campo LA, Weltz AS, Belyansky I, Novitsky YW. Comparative analysis of perioperative outcomes of robotic versus open transversus abdominis release. Surg Endosc. 2017 doi: 10.1007/s00464-017-5752-1. doi: 10.1007/s00464-017-5752-1 (Epub ahead of print) [DOI] [PubMed] [Google Scholar]
- 39.Muysoms FE, Dietz UA. Prophylaktische Netze an der Bauchdecke. Chirurg. 2016;87:751–761. doi: 10.1007/s00104-016-0245-7. [DOI] [PubMed] [Google Scholar]
- E1.Burger JW, Luijendijk RW, Hop WC, et al. Long-term follow-up of a randomized controlled trial of suture versus mesh repair of incisional hernia. Ann Surg. 2004;240:578–583. doi: 10.1097/01.sla.0000141193.08524.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E2.Holihan JL, Nguyen DH, Nguyen MT, et al. Mesh location in open ventral hernia repair: a systematic review and network meta-analysis. World J Surg. 2016;40:89–99. doi: 10.1007/s00268-015-3252-9. [DOI] [PubMed] [Google Scholar]
- E3.Conze J, Prescher A, Klinge U, et al. Pitfalls in retromuscular mesh repair for incisional hernia: the importance of the „fatty triangle“. Hernia. 2004;8:255–259. doi: 10.1007/s10029-004-0235-4. [DOI] [PubMed] [Google Scholar]
- E4.Ramirez OM, Ruas E, Dellon AL. “Components separation” method for closure of abdominal-wall defects: an anatomic and clinical study. Plast Reconstr Surg. 1990;86:519–526. doi: 10.1097/00006534-199009000-00023. [DOI] [PubMed] [Google Scholar]
- E5.Novitsky YW, Elliott HL, Orenstein SB, et al. Transversus abdominis muscle release: a novel approach to posterior component separation during complex abdominal wall reconstruction. Am J Surg. 2012;204:709–716. doi: 10.1016/j.amjsurg.2012.02.008. [DOI] [PubMed] [Google Scholar]
- E6.Pauli EM, Wang J, Petro CC, et al. Posterior component separation with transversus abdominis release successfully addresses recurrent ventral hernias following anterior component separation. Hernia. 2015;19:285–291. doi: 10.1007/s10029-014-1331-8. [DOI] [PubMed] [Google Scholar]
- E7.LeBlanc KA. Laparoscopic incisional and ventral hernia repair: complications-how to avoid and handle. Hernia. 2004;8:323–331. doi: 10.1007/s10029-004-0250-5. [DOI] [PubMed] [Google Scholar]
- E8.LeBlanc K. Proper mesh overlap is a key determinant in hernia recurrence following laparoscopic ventral and incisional hernia repair. Hernia. 2016;20:85–99. doi: 10.1007/s10029-015-1399-9. [DOI] [PubMed] [Google Scholar]
- E9.Bittner R, Bingener-Casey J, Dietz U, et al. Guidelines for laparoscopic treatment of ventral and incisional abdominal wall hernias (International Endohernia Society (IEHS)-part 1. Surg Endosc. 2014;28:2–29. doi: 10.1007/s00464-013-3170-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- E10.Muysoms F, Campanelli G, Champault GG, et al. EuraHS: the development of an international online platform for registration and outcome measurement of ventral abdominal wall hernia repair. Hernia. 2012;16:239–250. doi: 10.1007/s10029-012-0912-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eSUPPLEMENT SURGICAL TECHNIQUES
Scar tissue has to be reinforced mechanically by placement of a mesh. The mesh can be placed in various ways. There is no generally superior surgical technique. It is essential to identify on an individual basis which surgical strategy (for example, surgical access) is required for a patient. The factors to be taken into account in the individual patient vary widely. Only the overall evaluation of the factors involved (symptoms, urgency, morphology of the hernial orifice, size of the defect, quality of the connective tissue, tobacco use, diabetes mellitus, obesity, and age, among others) will clearly identify the individual treatment concept (13, 16).
On the one hand, it may well be that a comparable incisional hernia is treated with open reconstruction in a young patient (with few risk factors for complications), while it should be treated laparoscopically in an older patient (with multiple risk factors for complications). On the other hand, even a patient with multiple risk factors for complication may require open surgery associated with a high risk of complications, if, for example, surgery had been delayed for too long and the hernia had become very large. Establishing the indication for surgery in an individual patient is always the result of harmonizing the following parameters:
The recurrence rate after incisional hernia repair with mesh is significantly lower compared to other suturing techniques. In a randomized controlled trial (RCT) by Burger et al., the recurrence rate associated with suture repair amounted to 67% compared to 17% after mesh repair (e1). With the publication of that study at the latest, the use of permanent, non-absorbable mesh to reinforce incisional hernia repair became the standard of care. Current long-term data from the Danish Hernia Register show that the recurrence rate is significantly lower after mesh repair (15). At present, meshes made of polypropylene (PP), polyester (PES), polyvinylidene fluoride (PVDF), and polytetrafluoroethylene (PTFE) are commercially available. These meshes can be anatomically placed in various layers of the abdominal wall (figure 1). The best long-term results with regard to the lowest risk of recurrence were achieved with the following locations for mesh placement: sublay/retromuscular (Figure 1e), preperitoneal (Figure 1f) and intraperitoneal (IPOM) (Figure 1g) (e2).
Sublay mesh placement is particularly suitable for midline incisional hernia repair and can be described as a morphologically and functionally reconstructive technique (Figure 1e): The posterior sheath of the rectus abdominis muscle is released bilaterally and sutured to the opposite side. A tailored mesh is then placed in this newly created retromuscular space. Subsequently, the anterior rectus sheath is closed above it. The mesh is held in place between the layers by the intraabdominal pressure and stabilizes the scar, provided sufficient overlapping of the midline (Figure 1e). Here, it is crucial to ensure adequate cranial extension of the mesh overlap underneath the xiphoid process to cover the so-called “fatty triangle” (figure 2) and caudal extension into the retropubic space (space of Retzius).
In Germany, the school of Aachen led by Volker Schumpelick and Joachim Conze has raised awareness of this procedure and advanced the surgical technique (e3). If the diameter of the hernial orifice is larger than 12 cm, it can be necessary to perform a lateral relaxation incision along the aponeurosis of the external oblique muscle as described by Oscar Ramirez (Figure 1a) (e4). In special cases, it is not possible to achieve adequate lateral mesh overlapping. In this situation, it is necessary to extend the dissection layer in the area of the lateral edge of the rectus sheath: With the transversus abdominis release (TAR) technique (e5, e6) (Figures 1c and 1d), it is possible to enter a lateral extraperitoneal compartment, while sparing the intercostal nerves (Figure 1b).
The great advantage of retromuscular mesh placement is the extraperitoneal location of the synthetic mesh. This helps to reduce or prevent adhesions affecting bowel function and the development of enteroprosthetic fistula as well as inflammatory mesh deterioration, as the mesh is extraperitonealized. The disadvantage of this reconstruction principle is that it requires extensive dissection with resulting insufficient blood supply to the skin (skin necrosis, impaired wound healing). It is also associated with an increased risk of revision surgery (e.g. post-operative hemorrhage). The meta-analysis by Holihan et al. provides a good overview of mesh locations used with open surgery (e2). Inlay and onlay mesh repair techniques are to be rejected as they are associated with significantly poorer outcomes with regard to recurrence rate and wound complications compared to sublay mesh repair (e2).
With the advent of minimally invasive surgery, the laparoscopic mesh repair technique was developed (synonym: Intraperitoneal Onlay Mesh Repair [IPOM]) (e7): The mesh is placed between the abdominal wall and the intestines or omentum (Figure 1g). With this technique, the hernial orifice is not necessarily closed; the mesh serves as an extension (or replacement) of the abdominal wall. The challenges of this technique are mesh fixation and proper mesh overlap which needs to be proportional to the size of the hernial orifice: the larger the hernial orifice, the wider the required radial mesh overlap (e8). Here, two additional factors play an important role:
Surgeons performing laparoscopic procedures should have special expertise in adhesiolysis which is often required. This is also highlighted in the guidelines of the International Endo-Hernia Society (e9).
urgency of surgery
patient expectations placed on surgery
dedicated surgical technique and materials, and
individual expertise of the surgeon (17).
proper parietalization of the anterior abdominal wall (i.e. release of the falciform ligament und infraumbilical folds) and
adequate transfascial mesh fixation and/or use of tackers (absorbable or permanent) (16).