Abstract
Background and Aims:
One of the reasons for continued routine pre-operative testing practice is the identification of hidden problems which may affect perioperative management. This study was aimed to assess the prevalence of abnormal test results, their impact on perioperative management and cost-effectiveness for detecting such abnormalities.
Methods:
This observational study was conducted by screening the files of the patients attending pre-anaesthetic check-up during December 2016–January 2017. Patients' physical status, surgery grade, normal and abnormal test results and different impacts were noted and expressed in absolute numbers/percentage. Number needed to investigate (NNI) to detect a significant abnormality was calculated.
Results:
Data of 414 patients (46.3% male) with mean ± standard deviation age 43.78 ± 17.24 years and 58.65 ± 12.93 kg weight were analysed. Patients were mostly American Society of Anesthesiologists II and underwent National Institute of Clinical and Health Excellence Grade 3 surgeries. Totally, 345 (11.6%) test results were abnormal. Only 56 (16.2%) abnormalities had an impact in terms of referral, further investigations or delay. Twenty were significant in terms of changing perioperative anaesthetic management. Laboratory abnormalities with non-significant impact resulted in median delay of 3 days (range 1 to 12 days). The NNI for a significant impact and detecting new abnormality was 21 and 28, respectively.
Conclusion:
Majority (57.2%) of the patients had at least one abnormal routine test result but only 1.8% abnormalities had significant impact. The NNI to find a significant impact or hidden comorbidity was more than 20.
Key words: Abnormality results, cost-effectiveness analysis, laboratory tests, outcome, pre-operative
INTRODUCTION
With continuous escalation in health-care costs, health-care providers and managers are now targeting cost-effective yet quality and safe health-care delivery. One of the areas which has been scrutinised from time to time is the usefulness of routine pre-operative laboratory testing as a part of pre-operative assessment.[1,2] The task forces of the American Society of Anesthesiologists (ASA) and National Institute of Clinical and Health Excellence (NICE) have provided guidance on the use of pre-operative laboratory tests before elective surgeries for last one and half decades.[3,4] The current evidence and guidance recommend against the practice of routine pre-operative laboratory tests. Despite these recommendations, the tradition of routine preoperative testing is still prevalent due many reasons.[5] Identifying hidden problems that may manifest for the very first time, and that may necessitate change in perioperative management is one such reason. The present study was aimed to assess the prevalence of abnormal test results and their impact on perioperative management among patients undergoing elective surgeries.
METHODS
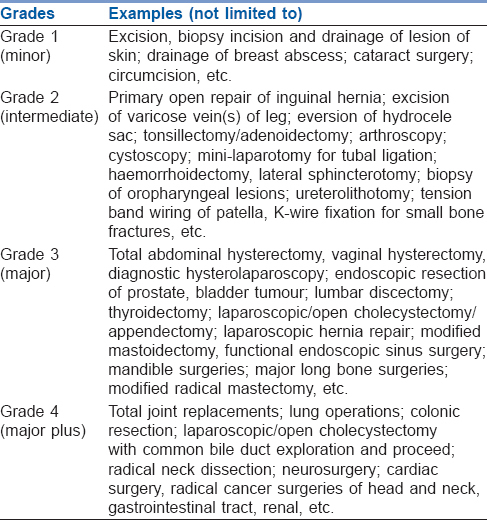
The present observational study was conducted in a tertiary care teaching hospital. With the approval from the Institute Ethics Committee, the data collection was done between December 2016 and January 2017. The study was planned with an expected 30% prevalence of abnormal test results which was based on the findings of 2-day pilot survey in the same institute. The sample size was then calculated using online tool OpenEpi (Open Source Epidemiologic Statistics for Public Health; http://www.openepi.com/SampleSize/SSPropor.htm) for an absolute precision of 5%, 95% confidence level and for a large (1 million) population which gave a sample size of 323. Considering a non-randomised sampling, a design effect of 1.25 was applied and a target sample of minimum 404 patients was taken. Case record files of 414 consecutive patients aged 12 years or more, of either sex, attending the outpatient pre-anaesthesia clinic (PAC) for pre-anaesthesia evaluation and risk stratification before planned elective non-cardiac surgeries were screened for data. Pregnant patients, bedridden or immobile patients whose body weight could not be assessed were excluded. Patients' demographic parameters, ASA physical status, grade of surgery as per adapted NICE classification, etc., were noted. The adapted NICE classification of surgical grades is presented in Table 1.[4] All investigations performed before the patient was declared fit for surgery after evaluation and risk stratification, and their results in terms of normal and abnormal tests were noted. To make it uniform and to minimise bias, it was decided that there would be no intervention by the primary investigator and data collector on determining the investigations required or to be asked for. Most patients attended PAC with routine pre-operative investigations as per the existing protocol of the hospital. An abnormal test result was said to be impactful if the abnormal test resulted in referral, delay, further investigations, retesting as well as changes in plan of anaesthetic management. Impact was considered to be significant only if it led to a change in the perioperative anaesthetic management (i.e., postponing the elective case for further optimisation, changes in the on-going management, altering the anaesthetic procedure and monitoring plan.) An abnormal test result which could have been expected in a patient from the history and clinical examination (e.g., blood urea, serum K+, creatinine in a patient with known kidney disease, anaemia in a clinically pale patient or with a history of menorrhagia, etc.) that led to a change in perioperative management, was not considered of impact as these pre-operative tests could not be defined as routine but as disease-specific investigations. Similarly, a new diagnosis of hypertension leading to an impact, whether significant or not, was not included in the study for analysis as the diagnosis and impact was based on clinical finding (i.e., blood pressure value), not pre-operative laboratory test values. Haemoglobin (Hb) level <12 g% was noted as anaemia in this study. For the other tests, results were considered abnormal if it was outside the normal reference range for the laboratory. The number of patients having Hb <10 g%, platelet counts <100,000/mm3 as well as <75,000/mm3, blood sugar >200 mg% and >250 mg%, abnormal thyroid hormone levels, etc., were also noted. Number of newly diagnosed comorbidity (disease) from the investigations was also noted. Numbers of abnormal tests as well their impact were expressed in absolute number and percentage scale. Number needed to investigate (NNI), the ratio of number of abnormal test results to the total number of tests, for detecting an abnormal test result with a significant impact was also calculated. Metric data were further analysed for measuring central tendencies and dispersions using INSTAT software (GraphPad Prism Software, La Jolla, CA, USA). P < 0.05 was taken a statistically significant.
Table 1.
Surgical grades and examples adapted from National Institute for Health and Care Excellence
RESULTS
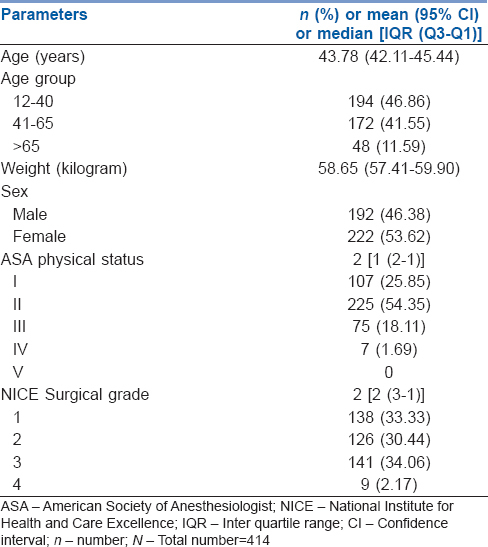
Data from a total of 414 patients' who had completed the PAC procedure for elective surgeries during the observation period were included for analysis. The patients were in the range of 12–95 (median 42) years of age and 24–106 (median 58) kilograms of weight. Majority of the patients were female and ASA physical status II. The age, sex, ASA physical status classes and NICE surgical grade wise distributions are shown in [Table 2]. One hundred seventy (41.1%) of the patients had at least one comorbid medical conditions (either known or newly diagnosed); anaemia (117 of 414; 28.3%) followed by hypertension (20.5%) being the most common. Fifty-seven (13.8%) of the patients had more than one comorbidity.
Table 2.
Demographic, physical status and surgical grade wise distributions of the cohort
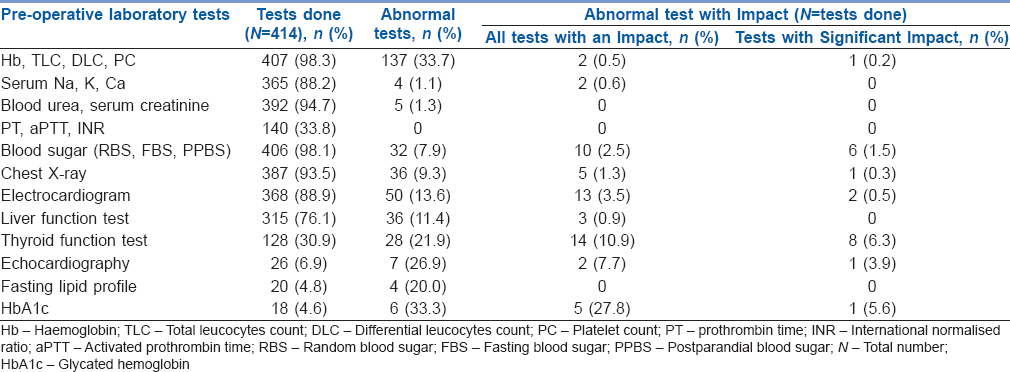
A total of 2972 (in an average more than 7 tests per patient) tests were done as a part of routine pre-operative work-up. A total of 237 (57.2%) patients had 345 (11.6%) abnormal test results; anaemia (Hb <12 g%) being the most common abnormality (117 of 345; 33.9%). Fifty-six (16.2%) abnormal tests had an impact; of these, 20 (35.7%) were significant as they lead to changes in perioperative management. The distribution of different routine tests done, respective number of abnormal test results and impacts are shown in Table 3. Although the mean age of female patients was lower as compared to male (42.07 ± 16.08 vs. 45.76 ± 18.35; P = 0.029), the incidence of abnormal tests among female and male were not different (10.8% vs. 12.3%, respectively; P = 0.274).
Table 3.
Distribution of routine tests done with respective results and impacts
A total of 227 out of 345 abnormal test results could be regarded as new or hidden and/or suggested a new diagnosis. However, only 15 (6.6%) of these were found to be significant. Low Hb was the commonest hidden abnormality found followed by abnormal electrocardiogram (ECG) (11.4% among the ECGs done). Although anaesthesiologists were mostly (70 out of 93; 75.3%) unable to detect mild anaemia (Hb 10 –12 g%) clinically, they were mostly (16 out of 23; 69.6%) able to clinically detect moderate (Hb 7–10 g%) and the only severe anaemia (Hb <7 g%) cases. The abnormality/new comorbidities and respective NNI are presented in Table 4.
Table 4.
Distribution of new comorbidities detected with respective impacts in terms of number needed to investigate
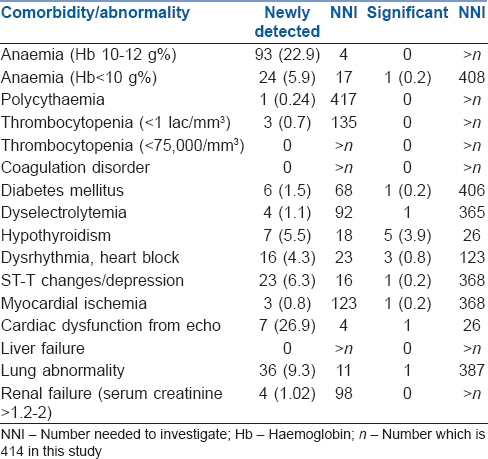
Only one (0.24%) patient with Hb <7 g% required pre-operative management of anaemia; No patient had platelet counts <75,000/mm3. One patient had creatinine >2 mg% and was a known case of chronic kidney disease. Six patients had blood sugar level >250 mg%; only one of them was new case of diabetes.
Thirty-six abnormal tests with an impact did not change the perioperative management. Eleven (19.6%) out of these patients were cleared on the same day without any delay, despite requiring consultation and reinvestigation; the other 25 (44.6%) impacts due to abnormal test results had a delay ranging between 1 and 12 days (median delay 3 days) before the patients final evaluation and risk stratification was completed.
DISCUSSION
Almost all patients presented with routine pre-operative tests done as advised by surgeons. While the majority of the patients (57.2%) had at least one abnormal test results; the prevalence of abnormal test results was 11.6%. Notably, only one out of six (16.2%) abnormal results had an impact indicating that anaesthesiologists considered more than 80% of abnormal test results as having no impact. Moreover, only one-third impacts actually led to changes in perioperative anaesthetic management. These results strongly question the necessity for routine preoperative tests.
The traditional practice of routine pre-operative tests before elective surgery is still very much prevalent both among anaesthesiologists and surgeons.[5] This leads to many unnecessary or unindicated tests and a huge cost burden.[6,7] The present study also found similar results. More than 60% of anaesthesiologist and more than 70% of surgeons believe that pre-operative tests will detect a hidden abnormality.[5] However, the question we need to consider is, do these hidden abnormal test results change the perioperative or anaesthetic management and outcome significantly? A multicentre study found 27% of the patients had some abnormal results in the pre-operative tests and 54.5% of these abnormal test results were newly detected.[8] In the National Surgical Quality Improvement Program database, there was at least one abnormal test recorded in 61.6% of patients who underwent elective, low-risk ambulatory surgery. However, surgeries were performed on the same day despite having these abnormalities.[9] A study conducted in patients of >70 years found that abnormal test values were not a predictor of post-operative adverse outcomes.[10]
In the present study, 237 (57.2%) of the patients had at least one abnormality in the tests done, which is higher than the 27% incidence in a previous study.[8] This is probably because of the difference in the population studied. The present study was done in an island of a developing country and a public hospital setup with patients belonging mostly to the poor socioeconomic status. Anaemia and thyroid hormone abnormalities were the major (>50%) abnormalities. Hb <12 gm% was taken as cut-off point for anaemia in patients aged > 12 years. A total of 16.2% of the total abnormal results led to an impact in terms of further testing, consultation and referrals, reporting, etc. However, only 20 of these impacts led to change in perioperative management. These data (20 significant impacts out of 414 patients) on the other hand indicate that the NNI for having a significant impact is 21. When it came to detecting/indicating comorbidity (disease), it detected a total 227 comorbidities; 117 (51.5%) of these were anaemia. Only 15 of these, 227 comorbidities could be regarded as significant. Again, these data (15 cases of significant new comorbidity out of 414 patients) indicate that the NNI for finding a significant impactful comorbid condition is 28. These NNI numbers (i.e., 21 and 28) may be looking rewarding and some of us may argue that it can work as screening point/tool. In this context, we have to remember that the use of the pre-operative tests as screening tool for detecting new hidden asymptomatic disease is also not advised by experts.[11] Again, cost-effectiveness for detecting one such significant case which will change perioperative anaesthetic management and outcome in terms of mortality reduction have to be considered.
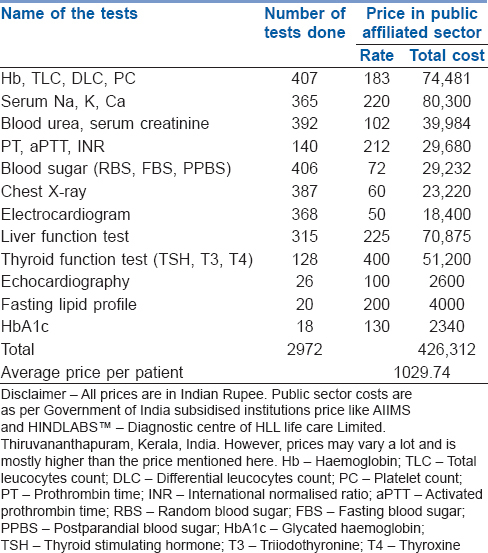
The average cost per patient even in government subsidized sector for routine preoperative testing was 1029.74 Indian rupees and is presented in Table 5. Considering the present study finding of detecting 3.6% (15 out of 414) comorbidities, we have to routinely investigate 28 patients to find one hidden comorbidity, which is going to cost 28,832 Indian rupees. In this context we have to also understand that when an asymptomatic, undetected and uncontrolled disease condition is detected by routine test and optimized, it may lead to the patient's ASA physical status changing from III to II.[12] At present with the advancement of anaesthesia practices and standards the anaesthesia related mortality is very low. Forty eight hour post-operative mortality of ASA II and III has been shown to be 0.002% and 0.028%–0.019%, respectively.[13,14] All these indicate that routine preoperative testing is not at all cost-effective in changing perioperative anaesthetic management and outcome.
Table 5.
Cost analysis of the routine tests
A limitation of this study is that it is based on a single centre finding and an observational research with extrapolative analysis. Institute to institute variation of practice is expected, and such study from few other centres or a multicentre study with different geographical and varied population will give us a better insight.
CONCLUSION
Majority (57.2%) of the patients had at least one abnormal test results on routine pre-operative tests, but only 56 (1.8%) of all tests performed had any impact in terms of referral, further testing, medication change, or delay. Only 0.67% of all tests had a significant impact in terms of changing perioperative anaesthetic management. Insignificant impacts however caused a median delay of 3 days. The Number Needed to Investigate to have a significant impact or detecting a hidden comorbidity was >20.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Fischer SP. Cost-effective preoperative evaluation and testing. Chest. 1999;115:96S–100S. doi: 10.1378/chest.115.suppl_2.96s. [DOI] [PubMed] [Google Scholar]
- 2.Ranasinghe P, Perera YS, Senaratne JA, Abayadeera A. Preoperative testing in elective surgery: Is it really cost effective? Anesth Essays Res. 2011;5:28–32. doi: 10.4103/0259-1162.84177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Committee on Standards and Practice Parameters, Apfelbaum JL, Connis RT, Nickinovich DG: American Society of Anesthesiologists Task Force on Preanesthesia Evaluation. Pasternak LR, Arens JF, et al. Practice advisory for preanesthesia evaluation: An updated report by the American society of anesthesiologists task force on preanesthesia evaluation. Anesthesiology. 2012;116:522–38. doi: 10.1097/ALN.0b013e31823c1067. [DOI] [PubMed] [Google Scholar]
- 4.National Collaborating Centre for Acute Care (UK). Preoperative Tests: The Use of Routine Preoperative Tests for Elective Surgery – Evidence, Methods and Guidance. London: National Institute of Clinical Excellence; 2003. [Last accessed on 2017 Mar 05]. Available from: http://www.ncbi.nlm.nih.gov/books/NBK48489/ [PubMed] [Google Scholar]
- 5.Karim HMR. Practice and reasons for routine pre-operative investigations among anaesthesiologists and surgeons: An online survey. Indian J Anaesth. 2017;61:933–5. doi: 10.4103/ija.IJA_92_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karim HM, Yunus M, Bhattacharyya P. An observational cohort study on pre-operative investigations and referrals: How far are we following recommendations? Indian J Anaesth. 2016;60:552–9. doi: 10.4103/0019-5049.187783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Keshavan VH, Swamy CM. Pre-operative laboratory testing: A prospective study on comparison and cost analysis. Indian J Anaesth. 2016;60:838–42. doi: 10.4103/0019-5049.193678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Perez A, Planell J, Bacardaz C, Hounie A, Franci J, Brotons C, et al. Value of routine preoperative tests: A multicentre study in four general hospitals. Br J Anaesth. 1995;74:250–6. doi: 10.1093/bja/74.3.250. [DOI] [PubMed] [Google Scholar]
- 9.Benarroch-Gampel J, Sheffield KM, Duncan CB, Brown KM, Han Y, Townsend CM, Jr, et al. Preoperative laboratory testing in patients undergoing elective, low-risk ambulatory surgery. Ann Surg. 2012;256:518–28. doi: 10.1097/SLA.0b013e318265bcdb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dzankic S, Pastor D, Gonzalez C, Leung JM. The prevalence and predictive value of abnormal preoperative laboratory tests in elderly surgical patients. Anesth Analg. 2001;93:301–8. doi: 10.1097/00000539-200108000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Wappler F. In reply: To questionable statement. Dtsch Arztebl Int. 2015;112:70. [Google Scholar]
- 12.American Society of Anesthesiologists. ASA Physical Status Classification System. Illinois: American Society of Anesthesiologists. 2014. [Last accessed on 2017 Mar 05]. Available from: https://www.asahq.org/resources/clinical-information/asa-physical-status-classification-system .
- 13.Whitlock EL, Feiner JR, Chen LL. Perioperative mortality, 2010 to 2014: A Retrospective cohort study using the national Anesthesia clinical outcomes registry. Anesthesiology. 2015;123:1312–21. doi: 10.1097/ALN.0000000000000882. [DOI] [PubMed] [Google Scholar]
- 14.Hopkins TJ, Raghunathan K, Barbeito A, Cooter M, Stafford-Smith M, Schroeder R, et al. Associations between ASA physical status and postoperative mortality at 48 h: A contemporary dataset analysis compared to a historical cohort. Perioper Med (Lond) 2016;5:29. doi: 10.1186/s13741-016-0054-z. [DOI] [PMC free article] [PubMed] [Google Scholar]


