Abstract
Background and Aims:
Mostly, institutions in India have single post-anaesthesia care unit (PACU) which follows traditional time-based discharge (TBD) method. Recently, it has been classified into PACU Phase I and Phase II, and criteria-based discharge (CBD) method has been used. This study primarily compares CBD versus TBD methods in moving patients through PACU, and other non-clinical factors causing delay in shifting.
Methods:
One hundred patients, aged 18–65 years, American Society of Anesthesiologist's physical status I and II, scheduled for elective minor surgeries under general anaesthesia were studied. White's fast-track score in operating room (OR) and modified Aldrete's score (CBD time) in PACU were recorded. Patients were scheduled to discharge at 60 min based on TBD method. The mean CBD time and actual discharge time from PACU were statistically compared with TBD time. Other non-clinical factors delaying the discharge were also studied.
Results:
Eighty-five percent of patients achieved acceptable White's fast-track score in OR. The TBD time (60 min) was compared with the mean CBD time (10.70 ± 2.56 min) and actual discharge time (79.75 ± 12.98 min), which were found to be statistically significant. Primarily, anaesthesiologists' busy schedule was accountable for delay in discharge.
Conclusion:
The study concluded that in patients undergoing ambulatory minor surgeries, discharge times based on Criterion Based Discharge scoring systems such as modified Aldrete's and White's-fast are significantly lower in PACU Phase I as compared to the traditional Time Based Discharge method.
Key words: Health resources, patient discharge, post-operative care, recovery room, scoring methods, workflow
INTRODUCTION
Recently, post-anaesthesia care unit (PACU) has been classified into PACU Phase I (costly and labour-intensive, high-dependency unit) and PACU Phase II (low-dependency, step-down unit) depending on the level of care required corresponding to the phases of recovery in the post-operative period.[1,2] In the recent years, with the advent of shorter and rapidly acting anaesthetic agents, it has been seen that some patients may be eligible to either bypass PACU Phase I (concept of fast tracking) or moved quickly from PACU Phase I unit to Phase II unit using physiological scoring systems.[1,2]
In India, most of the institutions follow the traditional time-based discharge (TBD) method in PACU, where patients get discharge after fixed interval of time by anaesthesiologist's orders when established clinical criteria are met.[3] Recent studies have shown that the modern clinical criteria-based discharge (CBD) method based on predetermined physiological scoring system has reduced the length of stay (LOS) in the PACU Phase I.[4,5,6] The modified Aldrete's and White's fast-track scoring systems have been widely used in discharging patients from PACU.[7,8,9,10] TBD method can vary from institution to institution, whereas CBD method has the ability to standardise the discharge criteria across institutions and has been shown to reduce the time spent in the PACU without affecting patient's safety.[5] Factors that influence LOS in PACU Phase I and the validity of any discharge criteria have not been studied much.[11]
We hypothesised that by creating a PACU Phase II and using CBD method to quickly move patients from operating rooms (ORs) to PACU Phase II, PACU I beds can be better utilised for more sick patients and it may have an economical impact on the healthcare system.
The primary outcome measures studied were time-based recovery versus criteria-/score-based recovery method in decreasing the LOS of patients in PACU I or fast-tracking PACU I, without compromising their post-operative care.
METHODS
This prospective observational study was conducted on 100 patients, aged 18–65 years, American Society of Anesthesiologist's (ASA) physical status I and II, scheduled for elective minor surgeries (ambulatory or outpatient surgeries that neither penetrate a body cavity nor encourage permanent impairment of any bodily functions and do not require overnight hospital stay) under general anaesthesia in OR. Patients suffering from major co-morbidities (e.g., significant cardiac, hepatic, renal, respiratory or central nervous system disorders) and undergoing emergency surgeries were excluded from the study.
After obtaining approval of the hospital's Ethics Committee, written and informed consent was taken from the patients. Pre-operative baseline vitals of each patient were noted. All patients were premedicated with fentanyl 2 μg/kg and general anaesthesia was induced with propofol 2 mg/kg and neuromuscular blockade was achieved with atracurium 0.5 mg/kg, and a laryngeal mask airway (LMA) Classic™ was inserted. Anaesthesia was maintained with air and oxygen (FiO2 0.4) along with sevoflurane 2%–6% (minimum alveolar concentration = 1.0) and atracurium 0.1 mg/kg every 30 min. Intravenous paracetamol 20 mg/kg and diclofenac 1.5 mg/kg were administered for analgesia after 45 min of induction. End-tidal CO2 was maintained between 35 and 40 mmHg. Ondansetron 0.1 mg/kg was given intravenously 30 min prior to removal of LMA. The residual neuromuscular blockade was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg.
Patients were not divided into different groups. Both modified Aldrete's and White's fast-track scores were calculated in each patient included in the study. However, all the patients were scheduled to discharge from PACU as per our institutional TBD method which was to discharge patients at a fixed interval of 60 min after getting discharge orders from anaesthesiologists, if other physiological parameters were within the normal range. White's fast-track score of each patient was recorded in OR before shifting to PACU. PACU nursing staff received the in-service teaching that explained the purpose of the study, the study protocol and the physiological discharge criteria. In PACU, the modified Aldrete's score of each patient was recorded at an interval of every 10 min and time to achieve a score of 9 or above was recorded as the CBD time.
Heart rate, blood pressure, SpO2 on room air, sedation score, respiratory rate, temperature, visual analogue score (VAS) and nausea/vomiting score of each patient were monitored at the interval of every 10 min, and the time was recorded for these parameters to achieve their normal range. Any adverse events or complications (such as airway obstruction, fall in SpO2 and haemodynamic instability) requiring nursing or medical intervention in the interval between CBD and TBD time were recorded.
The actual discharge time of patients from PACU (TBD time plus delay in discharge due to other non-clinical factors) was also recorded and statistically compared with the TBD time. Various non-clinical factors causing delay in discharge from PACU such as busy schedule of anaesthesiologists, housekeeping and PACU and ward nursing staff along with bed availability in ward were also recorded.
The sample size was calculated as 100 patients based on the assumption that modified Aldrete's scoring system-based discharge criteria will decrease the LOS in PACU by 10 min at 5% level of significance and 80% of power. Statistical testing was conducted with the Statistical Package for the Social Sciences system version 17.0 (Version 17.0; SPSS Inc., Chicago, IL, USA). Continuous variables are presented as mean ± standard deviation and categorical variables are presented as absolute numbers and percentages. The comparison of TBD time with mean CBD time and the mean actual discharge time was performed using paired Student's t-test. P < 0.05 was considered statistically significant.
RESULTS
The mean age of patients included in the study was 41.52 ± 11.47 years, among which 41 were females and 59 were males; 51 had ASA physical status I and 49 had ASA physical status II. The type of surgery-wise distribution of study population has been illustrated in Figure 1. The pre-operative baseline vitals of each patient were noted to be stable. There were no intraoperative complications noted in any of our patients. Eighty-five patients achieved White's fast-track score of 12 or above without scoring <1 in any individual category in OR before shifting to PACU.
Figure 1.
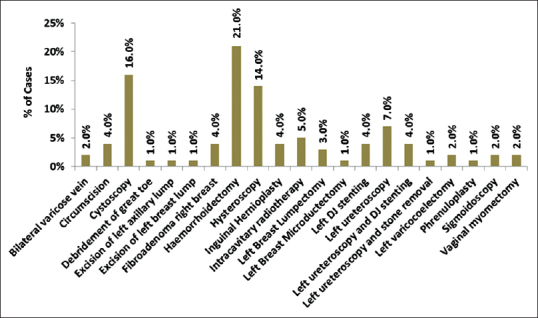
Type of surgery-wise distribution of study population
It was observed that 93 patients achieved the modified Aldrete's score of 9 or above in 10 min and the remaining 7 patients in 20 min. Therefore, CBD time was recorded as 10 min in 93 patients and 20 min in 7 patients. The mean CBD time (10.70 ± 2.56 min) and TBD time (60 min) when compared were found to be statistically significant (P < 0.001). There were no respiratory and haemodynamic complications observed in any patient in the interval between the CBD and TBD time.
It was found that there was a delay in discharge of patients from PACU to the ward due to various non-clinical factors. Sixteen patients were discharged without any delay; however, 68 and 16 patients were discharged between 60–90 min and 90–120 min, respectively. The mean delay in discharge was found to be 19.75 ± 12.98 min. The mean actual discharge time (79.75 ± 12.98 min) and TBD time (60 min) when compared were found to be statistically significant (P < 0.001).
It was observed that busy schedule of anaesthesiologists to write discharge orders (32%) and unavailability of housekeeping staff to shift patients from PACU to wards (34%) were the two key factors accountable for causing delay in discharge and increasing the LOS of patients in PACU. Other factors noted were busy schedule of PACU nursing staff (23%) and ward nursing staff (13%) followed by unavailability of beds in ward (18%). In our study, it was found that in all the patients, haemodynamic and respiratory parameters recovered the earliest followed by nausea/vomiting score and last the VAS of pain.
DISCUSSION
Traditionally, TBD method has been used to discharge patients from PACU which varies from institution to institution, whereas CBD method standardises and objectifies the discharge criteria across the institutions.[3] The mean CBD time calculated by modified Aldrete's score was found to be statistically significant (P < 0.001) when compared with TBD time. All the patients were breathing comfortably, maintaining SpO2 above 90% and haemodynamics was stable between CBD and TBD time.
This implies that modified Aldrete's scoring method of discharge may improve the workflow of patients by shifting them quickly and safely from PACU Phase I to Phase II without compromising their safety.
Our results were found to be consistent with the other studies which also illustrated that the CBD method significantly reduces the PACU LOS in comparison with the TBD method without observing any adverse events.[4,5]
The modified Aldrete's scoring system was found to be not adequate for fast-tracking patients undergoing surgery after general anaesthesia as it does not include common post-operative complications such as pain, nausea and vomiting which are usually treated in PACU Phase I.[12,13] Hence, fast-track scoring system was proposed that includes all the parameters of modified Aldrete's criteria as well as the assessment of pain and nausea.[9,10]
In our study, it was observed that nausea/vomiting and pain scores reached their targeted range later as compared to other parameters in PACU which shows that White's fast-tracking scoring method should be considered superior to modified Aldrete's scoring method in discharging patients safely from PACU Phase I. Earlier also it has been shown that the new fast-track scoring system offers advantages over the modified Aldrete's scoring system in evaluating the suitability for bypassing the PACU Phase I.[10] There is plenty of literature demonstrating fast tracking of patients from OR directly to PACU Phase II without affecting their safety.[14,15,16,17]
The mean actual discharge time (delay due to various non-clinical factors) was found to be statistically significant (P < 0.001) when compared with the TBD time. Busy schedule of anaesthesiologists and unavailability of housekeeping staff to shift patients from PACU were found to be the two main factors accountable for increasing PACU LOS. Similar results have been found in a number of other studies.[5,18,19,20]
This suggests that if an institution has two phases of PACU and the clinical scoring discharge systems are used for shifting patients objectively from PACU Phase I to Phase II, it may increase the productivity of both nurses and anaesthesiologists by saving their time to perform other activities and may cut down the hospital cost by better resource utilisation of expensive PACU Phase I. Other studies have also concluded that fast tracking is a suitable intervention to increase workflow efficiency and decrease both patient and hospital costs while promoting a more rapid discharge from the facility.[17]
Our study had few limitations. We could not assess the impact of other factors involved in maintaining the smooth flow of patients from OR till discharge to home on PACU LOS, for example, laboratory and radiological tests. We could not calculate the accurate cost benefits of using these discharge scoring criteria just by decreasing the LOS of patients in PACU Phase I because the total expenditure depends on various other factors which we were not able to scrutinise in our study.
CONCLUSION
In patients undergoing ambulatory minor surgeries, discharge times based on Criterion Based Discharge scoring systems such as modified Aldrete's and White's-fast are significantly lower in PACU Phase I as compared to the traditional Time Based Discharge method.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Marshall SI, Chung F. Discharge criteria and complications after ambulatory surgery. Anesth Analg. 1999;88:508–17. doi: 10.1097/00000539-199903000-00008. [DOI] [PubMed] [Google Scholar]
- 2.McGrath B, Chung F. Postoperative recovery and discharge. Anesthesiol Clin North Am. 2003;21:367–86. doi: 10.1016/s0889-8537(02)00080-9. [DOI] [PubMed] [Google Scholar]
- 3.Wig J. The current status of day care surgery. A review. Indian J Anaesth. 2015;49:459–466. [Google Scholar]
- 4.Truong L, Moran JL, Blum P. Post anaesthesia care unit discharge: A clinical scoring system versus traditional time-based criteria. Anaesth Intensive Care. 2004;32:33–42. doi: 10.1177/0310057X0403200106. [DOI] [PubMed] [Google Scholar]
- 5.Brown I, Jellish WS, Kleinman B, Fluder E, Sawicki K, Katsaros J, et al. Use of postanesthesia discharge criteria to reduce discharge delays for inpatients in the postanesthesia care unit. J Clin Anesth. 2008;20:175–9. doi: 10.1016/j.jclinane.2007.09.014. [DOI] [PubMed] [Google Scholar]
- 6.Awad IT, Chung F. Factors affecting recovery and discharge following ambulatory surgery. Can J Anaesth. 2006;53:858–72. doi: 10.1007/BF03022828. [DOI] [PubMed] [Google Scholar]
- 7.Aldrete JA, Kroulik D. A postanesthetic recovery score. Anesth Analg. 1970;49:924–34. [PubMed] [Google Scholar]
- 8.Aldrete JA. The post anesthesia recovery score revisited. J Clin Anesth. 1995;7:89–91. doi: 10.1016/0952-8180(94)00001-k. [DOI] [PubMed] [Google Scholar]
- 9.White PF. Criteria for fast-tracking outpatients after ambulatory surgery. J Clin Anesth. 1999;11:78–9. doi: 10.1016/s0952-8180(98)00119-6. [DOI] [PubMed] [Google Scholar]
- 10.White PF, Song D. New criteria for fast-tracking after outpatient anesthesia: A comparison with the modified Aldrete's scoring system. Anesth Analg. 1999;88:1069–72. doi: 10.1097/00000539-199905000-00018. [DOI] [PubMed] [Google Scholar]
- 11.Phillips NM, Street M, Kent B, Haesler E, Cadeddu M. Post-anaesthetic discharge scoring criteria: Key findings from a systematic review. Int J Evid Based Healthc. 2013;11:275–84. doi: 10.1111/1744-1609.12044. [DOI] [PubMed] [Google Scholar]
- 12.Song D, Joshi GP, White PF. Fast-track eligibility after ambulatory anesthesia: A comparison of desflurane, sevoflurane, and propofol. Anesth Analg. 1998;86:267–73. doi: 10.1097/00000539-199802000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Song D, van Vlymen J, White PF. Is the bispectral index useful in predicting fast-track eligibility after ambulatory anesthesia with propofol and desflurane? Anesth Analg. 1998;87:1245–8. doi: 10.1097/00000539-199812000-00006. [DOI] [PubMed] [Google Scholar]
- 14.Duncan PG, Shandro J, Bachand R, Ainsworth L. A pilot study of recovery room bypass (“fast-track protocol”) in a community hospital. Can J Anaesth. 2001;48:630–6. doi: 10.1007/BF03016195. [DOI] [PubMed] [Google Scholar]
- 15.Fredman B, Sheffer O, Zohar E, Paruta I, Richter S, Jedeikin R, et al. Fast-track eligibility of geriatric patients undergoing short urologic surgery procedures. Anesth Analg. 2002;94:560–4. doi: 10.1097/00000539-200203000-00015. [DOI] [PubMed] [Google Scholar]
- 16.Apfelbaum JL, Walawander CA, Grasela TH, Wise P, McLeskey C, Roizen MF, et al. Eliminating intensive postoperative care in same-day surgery patients using short-acting anesthetics. Anesthesiology. 2002;97:66–74. doi: 10.1097/00000542-200207000-00010. [DOI] [PubMed] [Google Scholar]
- 17.Rice AN, Muckler VC, Miller WR, Vacchiano CA. Fast-tracking ambulatory surgery patients following anesthesia. J Perianesth Nurs. 2015;30:124–33. doi: 10.1016/j.jopan.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 18.Waddle JP, Evers AS, Piccirillo JF. Postanesthesia care unit length of stay: Quantifying and assessing dependent factors. Anesth Analg. 1998;87:628–33. doi: 10.1097/00000539-199809000-00026. [DOI] [PubMed] [Google Scholar]
- 19.Seago JA, Weitz S, Walczak S. Factors influencing stay in the postanesthesia care unit: A prospective analysis. J Clin Anesth. 1998;10:579–87. doi: 10.1016/s0952-8180(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 20.Samad K, Khan M, Hameedullah, Khan FA, Hamid M, Khan FH, et al. Unplanned prolonged postanaesthesia care unit length of stay and factors affecting it. J Pak Med Assoc. 2006;56:108–12. [PubMed] [Google Scholar]


