Abstract
Background:
Ingestion of excess fluoride can cause fluorosis which adversely affects teeth and bones. Fluorosis is a major public health problem in the state of Rajasthan with all its 32 districts having variable fluoride contamination, and many initiatives are currently implemented in this region to mitigate the fluorosis burden.
Objective:
The objective of this study was to assess fluorosis, its risk factors, and the awareness among school students and teachers in endemic villages of Jodhpur district, Rajasthan.
Materials and Methods:
A representative sample of 300 students of age 12–15 years were enrolled for cross-sectional study in selected villages. Data were collected regarding awareness, behavioral and preventive practices about fluorosis and clinical assessment and fluoride estimation in water and urine samples was done.
Results:
Dental fluorosis through Dean's index was observed in 24.5% of students. The awareness and practices for fluorosis prevention and its risk factors were poor among both students and teachers. Intake of piped water supply was reported by majority of students (95.8%). High fluoride concentration was found in 35 (81.3%) out of 43 urine samples.
Conclusion:
Improvement in drinking water supply in the endemic village of Rajasthan has decreased the burden of fluorosis, but low level of awareness and prevailing dietary and behavioral practices still pose them at risk of high fluoride intake. This signifies the need to address nonconventional sources of fluoride intake (diet and toothpaste) and early screening of disease by involving teachers and family physicians in fluoride mitigation efforts.
Keywords: District Fluorosis Control Program, evaluation, fluorosis, Jodhpur, Rajasthan, school
Introduction
The availability of safe potable water remains challenging in rural settings, where 72% of Indian population reside with high reliance on alternative water sources (ground well, hand pumps, and tube wells) posing increased risk for ingestion of excess fluoride and fluorosis. Moderate fluoride leads to dental effects, but long-term exposure or large amounts can lead to skeletal problems. The global prevalence of fluorosis is very high, ranging from 57,000 in Eritrea to as high as 18,197,000 in countries like India.[1] Based on 11th Five Year Plan estimates, about 66 million Indian citizens are residing in fluoride endemic areas across 200 districts in 17 states.[2,3] Bhasin et al. have estimated that about 18,197,000 are affected with dental fluorosis and 7,889,000 with skeletal fluorosis at present in India.[4]
In tropical regions such as state of Rajasthan, people consume more water and thus are at a higher risk of fluorosis. All the 32 districts in Rajasthan have high fluoride levels in groundwater, especially western and southern parts which are conventionally described as “high fluoride” areas[5,6] including Jodhpur which has a mean concentration of 2.75 mg/L (0.25–22.0 mg/L).[7]
High consumption of fluoride through food and toothpaste can amount to 30%–40% of intake[8,9] in the form of regular consumption of rock salt (kala namak) in all tastemakers, betel leaf (pan), areca nut (supari), tobacco, gutka, powdered tea, and ingestion of toothpaste by children.[10,11,12] This can be detrimental in areas with high fluoride levels as the permissible limit in drinking water ranges from 0.6 to 1.5 mg/L.[13,14]
The current study was conducted in a rural endemic block of Jodhpur to evaluate the burden and risk factors of fluorosis among schoolchildren and to assess the awareness of affected population and school teachers about the endemic disease.
Materials and Methods
Study area and population
This cross-sectional study was conducted in a government secondary school of Jhanwar and Kadumbanada villages of Luni block, Jodhpur district, for 3 months (August–September, 2015). The study population comprised students aged 12–15 years of age.[15] With estimated prevalence of dental fluorosis of 25%, a sample size of 300 children was studied,[16] and students from class 6th to 9th of requisite age criterion were approached. The study area was chosen as per data on fluorosis endemic areas available with district health authorities. Voluntary participating school teachers of the sampled school were assessed regarding awareness about fluorosis and its determinants. Students who were unable to provide signed informed consent from their parents after two repeated requests were excluded from the study.
Tools and techniques
A pretested self-designed questionnaire in Hindi was administered to assess knowledge and practices regarding fluorosis and its risk factors.
Sign and symptoms screened for fluorosis among schoolchildren
School children were assessed regarding:
Nonspecific symptoms
Symptoms persisting for more than 3 months and considered to be early warning signs of fluorosis: stomach ache, loss of appetite, constipation, diarrhea, headache, excessive urination and thirst, and fatigue.
Skeletal fluorosis
Inability to perform one or more exercises (touching of chest with chin; bend forward and touch the toes and stretch the arms sideways and touch the back of head).
Dental fluorosis
A dental assessment of the students was conducted and was classified, based on Dean's classification,[17] into five grades based on the status of dental enamel: normal, questionable, very mild, mild, moderate, and severe.
Laboratory testing
The fluoride concentration in water and urine samples was measured electrochemically using a fluoride ion-selective electrode technique. The results were later categorized into concentration intervals (0.1–1 ppm, 1–2 ppm, 2–3 ppm, and >3 ppm).
Data collection and analysis
The school was visited during working hours for data collection, and a spot urine sample for fluoride estimation was taken from a randomly selected volunteering subsample (n = 43) of students. Three water samples were collected from the different sites of drinking water sources (one piped water and two hand pumps) in precleaned polyethylene bottles with necessary precautions. Data were entered into a Microsoft Excel 2013 spreadsheet and imported to SPSS 21.0 version (IBM Corp. Released 2012. IBM SPSS Statistics for Windows, Version 21.0. Armonk, NY: IBM Corp.) for analysis. Appropriate statistical tests were used, and P < 0.05 was considered the level of significance.
Ethical considerations
Approval to conduct this study was taken from the Institutional Ethics Committee of the All India Institute of Medical Sciences (AIIMS), Jodhpur, and district health authorities and principal/head of selected schools. All children were given written consent and assent form to be approved by their parents, and informed consent was obtained from the participating teachers.
Results
A total of 306 students participated from the selected schools of Jhanwar (58.8%) and Kadumbanada (39.21%). The majority of students (99.7%) were residing for the past 10 years or more and were from nuclear families (55.5%) and reported parents having poor educational status, i.e., illiterate mothers (79.7%) and fathers primary educated (48.6%). Agriculture work was the most common reported occupation (59.4%).
Awareness regarding fluorosis, behavioral risk factors, and practices among students
None of the students had any knowledge about fluorosis, its signs and symptoms, and risk factors [Table 1].
Table 1.
Fluorosis-related knowledge and behavioral practices among the students
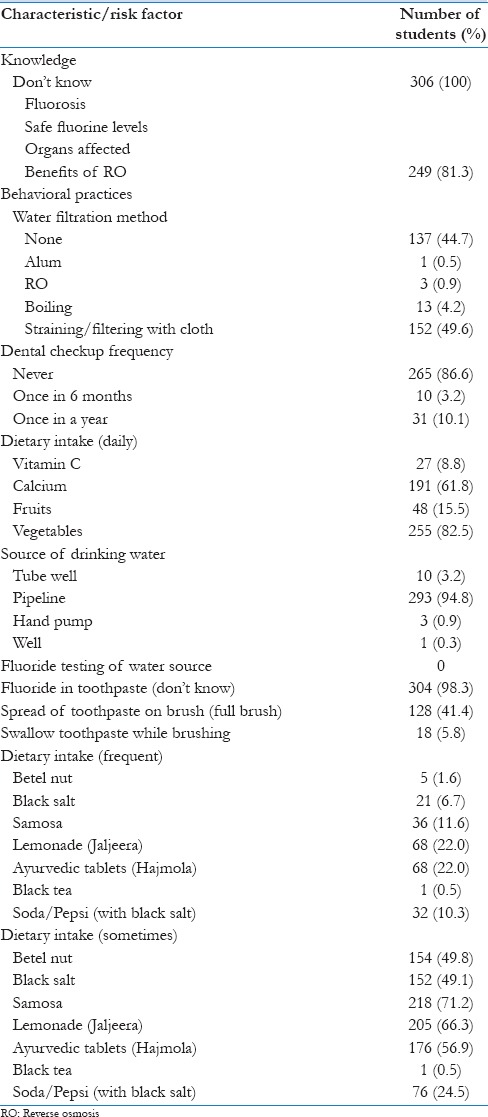
Source of drinking water
The most common source of drinking water was piped water (95.8%), but the use of tube well (3.2%), hand pump (1%), and well (0.3%) was also reported. Few subjects (18.6%) were aware of the benefits of reverse osmosis (RO) process in water filtration. Although many students (55.9%) reported using filtered water for drinking, majority (88.9%) were using cloth for straining water and only fewer subjects reported boiling (4.2%), RO (1%), and alum (0.3%) as filtration method [Table 1].
Behavioral risk factors and practices
Frequency of dental checkup
The majority (86.6%) of students never had any dental examination and only few reported annual (10.1%) and biannual (3.3%) dental checkups [Table 1].
Dietary intake of calcium, Vitamin C, fruits, and vegetables
The majority of students (62.4%) reported daily consumption of calcium-rich diet through dairy products. Infrequent intake (<2–3 times/month) of calcium-rich diet was seen in 15%, while Vitamin C-rich products intake was infrequent (only 1–2 times a week) in about one-half (48.4%) of the students. Consumption of cooked vegetables was high among with majority of students (83.3%) reporting daily intake [Table 1].
Intake of fluoride-rich food items
Occasional or regular consumption of fluoride-rich food items was seen for supari (51.9%), rock salt or chat masala (56.6%), fried and spicy foods such as samosa (83%), lemonade/Jaljeera (89.2%), ayurvedic preparations as Hajmola (79.7%), tea without milk (0.6%), and use of rock salt or soda in cold drinks (35.3%) [Table 1].
Amount of toothpaste on brush
More than recommended amount of toothpaste for brushing was reported as 41.8% applied it over whole brush surface, and 2.9% participants conveyed swallowing of toothpaste while brushing [Table 1].
Status of fluorosis
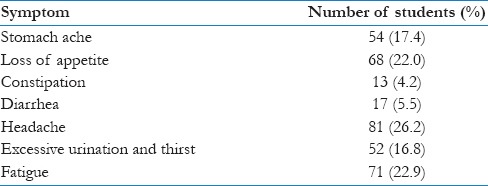
Early warning signs
Nonspecific symptoms were reported by few students in the form of a persistent headache (26.5%), persistent fatigue (23.2%), loss of appetite (22.3%), stomach ache (17.6%), excessive thirst (17%), diarrhea (5.6%), and constipation (3.6%) [Table 2].
Table 2.
Prevalence of nonspecific symptoms of fluorosis among the students
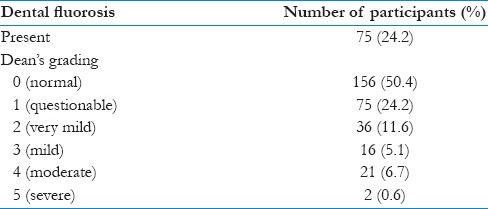
Dental and skeletal fluorosis
The dental assessment revealed that majority of students (75.5%) had no signs of dental fluorosis, while remaining 24.5% had various grades (very mild [11.8%], mild [5.25], moderate [6.9%], and severe grade [0.7%]). Only two students were not able to perform one or more exercises in skeletal fluorosis assessment, while none conveyed any difficulty in walking. The students who were positive for dental and skeletal fluorosis were referred to AIIMS, Jodhpur, for further work-up and management [Table 3].
Table 3.
Status of dental fluorosis among the students (Dean's grades)
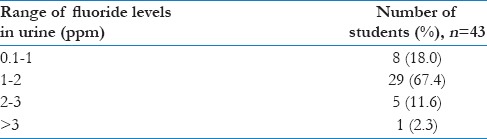
Fluoride estimation of urine and water samples
The urine examination (n = 43) revealed that 35 (81.3%) students had excess levels of urine fluoride, i.e., 29 (1–2 ppm), 5 (2–3 ppm), and 1 (>3 ppm). All the three sources of water samples in the area had normal range 0.1–1 ppm of fluoride concentration [Table 4].
Table 4.
Urine fluoride levels of the sampled students
Feedback from teachers regarding disease, prevention, and control methods
Knowledge about fluorosis
Eight of ten teachers conveyed being aware of fluorosis disease, but only five of eight correctly reported that it was due to high fluoride content in water.
Identifying a child suffering from fluorosis and body parts affected
Five of ten teachers knew about the detection of fluorosis through dental status, while four of ten conveyed bone deformity as the diagnostic indicator.
Prevention of fluorosis
Nine of ten teachers reported ingestion of safe drinking water for preventing fluorosis. While three of ten reported that diet rich in calcium and fruits has beneficial effects, two teachers conveyed that avoidance of tobacco and nicotine products helps in preventing fluorosis. None of the teachers was aware of their role in the early screening of fluorosis among school students.
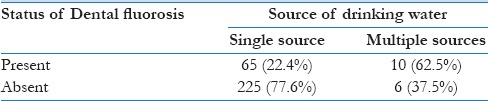
A significant association was observed between the status of dental fluorosis and source of drinking water with students having more than one source of drinking water having a significantly higher proportion of dental fluorosis present (P < 0.05) [Table 5].
Table 5.
Association of dental fluorosis with source of drinking water
Discussion
The prevalence of dental fluorosis observed in our study was about 24.5%, much lower compared to 69.4% reported by Arif et al. from Nagaur, Rajasthan.[6] This difference is due to the presence of piped water supply with optimal fluoride levels in our study area supplied from Indira Gandhi Canal project, signifying the success of fluorosis mitigating efforts under the Rajasthan Integrated Fluorosis Mitigation Program (2004) and the National Rural Drinking Water Quality Monitoring and Surveillance Program (2006).
The presence of dental fluorosis in 12–13-year-old children irrespective of levels of fluoride concentration in drinking water has been previously reported (25.4%)[16] as seen in our study and may be due to behavioral risk factors, consumption of food items rich in fluoride and toothpastes which are reported to be major risk factors in areas with optimal fluoride concentration in drinking water.[7,18] The suboptimal consumption of Vitamin C (91.2%), fruits, vegetables, and dairy products and higher intake of black salt (~5%–20%) were also observed in the current study.
In spite of great emphasis on health education as a strategy to control fluorosis, awareness of fluorosis disease, organs affected and source of fluorosis, diet editing, and diet counseling was found to be negligible both among school students and teachers. Straining of drinking water through cloth was reported to be the most common mode of water filtration method and conveys the extreme reliance of population on district authorities to provide them safe drinking water supply through pipes.
The new guidelines under the National Programme for Prevention and Control of Fluorosis Program lay emphasis on the education of teachers as a measure to control fluorosis.[18] The current study reveals that the measures to involve teachers as important source of information about fluorosis and their role in the screening of affected population are still lacking and need due emphasis.
Fluorosis mitigation programs continue to apply the conventional approach of providing piped water supply in the endemic area and highlight the limited effectiveness of state-run programs in tackling the issue comprehensively as observed in literature review done on aboriginal children in Australia.[19] Further, dental fluorosis is an early developmental defect affecting the teeth before calcification (before 10 years of age). Early exposure to excess fluorides leads to disturbances of enamel development owing to its cariostatic and hypomineralization effects which manifest later.[20] The severity of dental fluorosis is also dependent on fluoride dose, timing, and duration of fluoride exposure. Therefore, early fluorosis detection in young children by family physicians needs to be emphasized as a prudent strategy to halt the disease development in future years.
Conclusion
Persistent gaps in the implementation of the fluorosis control program in the form of behavioral risk factors and high level of ignorance even in endemic regions warrant need of proactive mitigation approaches to be strategized in the program. This demands funding of practical, culturally appropriate, and sustainable strategies involving school teachers and family physicians in fluorosis screening and control efforts.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
The authors thank the students and the teachers who participated in the study and the Jodhpur district authorities for their guidance.
References
- 1.Fewtrell L, Smith S, Kay D, Bartram J. An attempt to estimate the global burden of disease due to fluoride in drinking water. J Water Health. 2006;4:533–42. [PubMed] [Google Scholar]
- 2.II. New Delhi: Published by Oxford University Press; 2008. Planning Commission. Eleventh Five Year Plan (2007-2012) Social Sector. [Google Scholar]
- 3.National Program for Prevention and Control of Fluorosis (NPPCF). Revised Guidelines (2014) Directorate General of Health Services. Ministry of Health and Family Welfare. Government of India. 2014 [Google Scholar]
- 4.Bhasin JK, Jain A, Bansiwal AK, Gupta SK. Nutritional Value of Food Consumed by Villagers in Rajasthan; Relevance of Fluoride and its Control. National Workshop on Control and Mitigation of Fluoride in Drinking Water; February. 2004:5–7. [Google Scholar]
- 5.Choubisa SL, Choubisa L, Choubisa DK. Endemic fluorosis in Rajasthan. Indian J Environ Health. 2001;43:177–89. [PubMed] [Google Scholar]
- 6.Arif M, Husain I, Hussain J, Kumar S. Assessment of fluoride level in groundwater and prevalence of dental fluorosis in didwana block of Nagaur district, Central Rajasthan, India. Int J Occup Environ Med. 2013;4:178–84. [PubMed] [Google Scholar]
- 7.Saxena KL, Sewak R. Fluoride consumption in endemic villages of India and its remedial measures. Int J Eng Sci Invent. 2015;4:58–73. [Google Scholar]
- 8.Bhargava D, Bhardwaj N. Study of fluoride contribution through water and food in human population in fluoride endemic villages of North – Eastern Rajasthan. Afr J Basic Appl Sci. 2009;1:55–8. [Google Scholar]
- 9.Gautam R, Bhardwaj N, Saini V. Fluoride accumulation by vegetables and crops grown. In Nawa Tehsil of Nagaur district, Rajasthan. Indian J Physiol. 2010;2:80–5. [Google Scholar]
- 10.Bentley EM, Ellwood RP, Davies RM. Fluoride ingestion from toothpaste by young children. Br Dent J. 1999;186:460–2. doi: 10.1038/sj.bdj.4800140. [DOI] [PubMed] [Google Scholar]
- 11.Jiménez-Farfán MD, Hernández-Guerrero JC, Juárez-López LA, Jacinto-Alemán LF, de la Fuente-Hernández J. Fluoride consumption and its impact on oral health. Int J Environ Res Public Health. 2011;8:148–60. doi: 10.3390/ijerph8010148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Beltrán-Valladares PR, Cocom-Tun H, Casanova-Rosado JF, Vallejos-Sánchez AA, Medina-Solís CE, Maupomé G. Prevalence of dental fluorosis and additional sources of exposure to fluoride as risk factors to dental fluorosis in schoolchildren of Campeche, Mexico. Rev Invest Clin. 2005;57:532–9. [PubMed] [Google Scholar]
- 13.Raghavachari S, Tripathi RC, Bhupathi RK. Endemic fluorosis in five villages of the Palamau district, Jharkhand, India. Fluoride. 2008;41:206–11. [Google Scholar]
- 14.Institute of Medicine (IOM). Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington DC: National Academy Press; 1997. [PubMed] [Google Scholar]
- 15.World Health Organization. Oral Health Surveys: Basic Methods. 5th ed. Geneva: World Health Organization; 2013. [Google Scholar]
- 16.Solanki S, Dundappa J, Nagendra BK. Prevalence of dental fluorosis in school children of Jodhpur City. Indian J Dent Adv. 2011:563–7. [Google Scholar]
- 17.3rd ed. Geneva: World Health Organization; 1997. World Health Organization. Oral Health Survey-Basic Methods. [Google Scholar]
- 18.Susheela AK. Dental fluorosis and its extended effects. Indian J Pediatr. 2013;80:715–7. doi: 10.1007/s12098-013-1100-1. [DOI] [PubMed] [Google Scholar]
- 19.Christian B, Blinkhorn AS. A review of dental caries in Australian aboriginal children: The health inequalities perspective. Rural Remote Health. 2012;12:2032. [PubMed] [Google Scholar]
- 20.Shanthi M, Reddy BV, Venkataramana V, Gowrisankar S, Reddy BV, Chennupati S. Relationship between drinking water fluoride levels, dental fluorosis, dental caries and associated risk factors in 9-12 years old school children of Nelakondapally Mandal of Khammam district, Andhra Pradesh, India: A cross-sectional survey. J Int Oral Health. 2014;6:106–10. [PMC free article] [PubMed] [Google Scholar]


