Abstract
Introduction:
Chronic non communicable diseases in India have increased in magnitude with earlier onset and more likelihood of complications. Much emphasis is given to early diagnosis and timely treatment. Additionally, tertiary prevention through medication adherence is needed to limit disability and prevent early onset of complications. This study was aimed to assess the magnitude of medication and lifestyle adherence among elderly patients suffering from diabetes and hypertension in rural areas of Punjab.
Methodology:
This was a clinic based study in district Fatehgarh Sahib, Punjab. Patients were subjected to regular blood pressure and blood glucose monitoring. Thereafter they were offered free medications through weekly clinic held at Community Health Center, Bassi Pathana. Along with treatment, Public Health Nurse conducted counselling on diet and lifestyle. Frequency and process of taking medications was explained in local language and records duly maintained during visits.
Results:
Nearly 70% of study subjects were more than 50 years old. Males constituted 26% of the sample and 60% of subjects were illiterate. Large majority of study subjects did not consumed tobacco (98.08%) or alcohol (89.42%) in past thirty days. In-sufficient physical activity and poor compliance to diet was reported by 10.5% (Males: 7.4%, Females: 11.7%) and 23.5% (Males: 31.5%, Females: 20.8%) subjects. Nearly 46.15% of study subjects reported missing prescribed medications. Nearly 61.54% of study subjects were very sure that they will be able to take medicines as directed by physician.
Conclusion:
National Program for Control of Diabetes, Cardio-vascular Disease and Stroke relies on early diagnosis and treatment non- communicable diseases. However, with reported levels of adherence to medication and lifestyle interventions, there is an urgent need of exploring innovative ways to ensure compliance and improve treatment outcomes.
Keywords: Adherence, chronic, disease, geriatric, medication
Introduction
Chronic noncommunicable diseases (NCDs) have assumed much significance in adult population of developing and developed world alike. The magnitude of diseases has surged in India with earlier onset and more likelihood of complications.[1,2] Demographic transition, increasing life expectancy, modern trends of living, and changing family dynamics are likely to further increase disease burden in forthcoming years.
Management of patients with chronic illness requires strict lifestyle modifications and consistent intake of medicines for long durations, often extending for entire lifetime. Successful management of NCDs pertains to persistent adherence of prescribed medications and lifestyle recommendations. Adherence has been defined as the “the extent to which a person's behavior, e.g., taking medication, following a diet, and/or executing lifestyle changes, corresponds with agreed recommendations from a health care provider.” There is mounting evidence that nonadherence to the prescribed treatment is prevalent across various chronic conditions and is associated with adverse health outcomes, increased incidence of drug resistance, and higher costs of care.[3] As reported by the World Health Organization (WHO), medication adherence in patients with chronic diseases averages around 50% in developed countries and situation is worse in developing countries like India due to poor access to medications, health-care services, and illiteracy.[4]
Issues of medication adherence assume much significance in geriatrics as most are marginalized with poor family support and meager resources. Disability hinders treatment seeking by the elderly. Accessibility, affordability to treatment, and pill burden are major barriers in ensuring adherence, more so for residents in rural and underserved areas.[5]
The National Program for Diabetes, Cardiovascular Disease, and Stroke was introduced in 2008 on a pilot basis through the public health-care system of India. Much emphasis is on establishing NCD clinics and delivery of free preventive and curative services at primary level. However, appropriate measures need to be undertaken to address the issue of poor medication adherence.[6] Limited studies from India document adherence on medication and lifestyle for chronic noncommunicable diseases.[7,8,9] This study was thereby planned to assess the magnitude of medication and lifestyle adherence among elderly patients suffering from diabetes and hypertension in rural areas of Punjab.
Methodology
This is a clinic-based study in district Fatehgarh Sahib, Punjab. The Mehar Baba Charitable Trust, a nongovernmental organization, provides free diagnostic and therapeutic services for diabetic and hypertensive patients identified through opportunistic screening camps. Patients are subjected to regular blood pressure and blood glucose monitoring. Thereafter, they are offered free medications through weekly clinic held at Community Health Center, Bassi Pathana. Along with treatment provision, public health nurse conducted counseling on diet and lifestyle measures. Frequency and process of taking medications were explained at length in local language. Record of visit was duly maintained. All patients on treatment for a minimum period of 6 months were subjected to a pretested, semi-structured validated questionnaire after informed consent. Questionnaire assessed adherence to prescribed drugs and dietary restrictions. Reasons for nonadherence to prescribed medications, perception of patients, and familial support in treatment process were enquired. Reference period for assessing adherence to diet and medicines was 1 week. Those who violated regulations daily or alternate days were clubbed under “often,” those who did once or twice a week were classified in the category of “sometimes,” and those who never reported the same were under the “never” category. Recall period for questions on tobacco and alcohol was restricted to 1 month. In the study, sample size of 256 was calculated based on reported adherence of 40% and precision of 5%.
Data collected were entered into Epi Info version 7 (Manufactured by CDC and the software is available on public domain)for analysis. Univariate analysis was done to check for errors and missing data. Categorical data were analyzed using Chi-square test and analysis of quantitative data was done through mean, median, and mode.
Results
Nearly 70% of study patients were more than 50-year-old with no patient <30 years of age. Males constituted 26% of the sample. Nearly 60% of patients were illiterate. Only one-fourth (25%) of the patients were middle school pass. More than half (52.8%) of the patients were working at home, and daily wage agricultural work was reported by 5% patients. Seven percent reported inability to work due to old age [Table 1].
Table 1.
Sociodemographic details
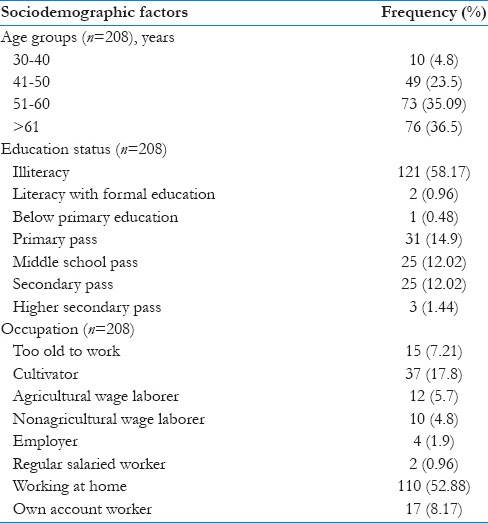
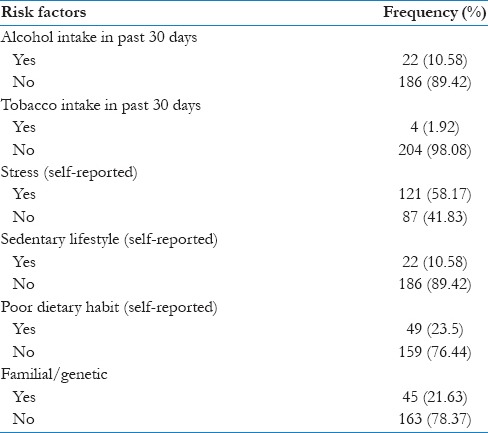
Table 2 shows exposure to identified risk factors of diet, tobacco, alcohol, and insufficient physical activity as reported by the respondents. Large majority of study patients did not consume tobacco (98.08%) or alcohol (89.42%) in the past 30 days. Less than 1% women reported consumption of products. Stress was reported by 58.17% (males: 61.1% and females: 57.14%) of respondents. Insufficient physical activity and poor compliance to diet were reported by 10.5% (males: 7.4%, females: 11.7%) and 23.5% (males: 31.5%, females: 20.8%) respondents, respectively. Familial or genetic history of diabetes or hypertension was known to 21% respondents.
Table 2.
Exposure to identified risk factors of noncommunicable diseases (n=208)
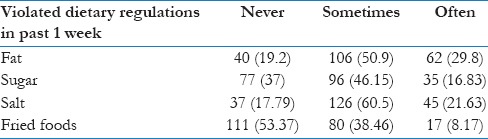
The extent of adherence to dietary measures as reported by respondents is shown in Table 3. More than half (53.37%) of the study patients did not consume fried foods in the past 1 week. Adherence to salt, fat, and sugar was sometimes violated by 60%, 51%, and 46.15% of the study patients, respectively. More than one-fourth of study patients (29.8%) often violated dietary regulations of fat. Significantly more men violated dietary regulations of sugar (male: 20.3%, female: 15.5%) and often consumed fried foods (male: 20.3%, female: 7.79%) [Table 3].
Table 3.
Adherence to medicine and lifestyles recommendations
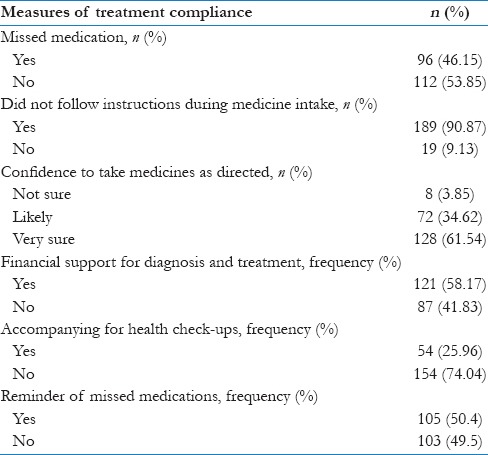
In Table 4, nearly 46.15% of study patients reported missing prescribed medications. More females (50%) missed medication compared to males (35%). The majority (90.8%) followed instructions delivered during consultation. Nearly 61.54% of study patients were very sure that they will be able to take medicines as directed by the physician. Perception to adhere to the medicines was present in 67.3% of study patients. Two percent of the study patients were not very sure of taking medicines. Confidence adhering to dietary regulations was present in nearly 59.4% of the study patients. More than half (58.17%) of the study patients reported having financial support for diagnosis and treatment. Half of the respondents (50.4%) were supported by family members in medications and dietary control. More males (79%) had financial support for medicines and blood tests compared to females (50.65%). Assistance to seek health-care services was not available to a majority of the respondents. Nearly 74% of the respondents did not have any person to accompany them for health visits. Thirty-three percent males were accompanied for health check-ups compared to 23.38% females.
Table 4.
Pattern of medication intake and treatment support measures
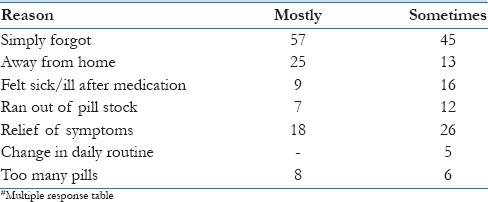
More than half of the respondents (59.3%) reported that they simply forgot taking pills most of the time. There were busy in household work or were sleeping and missed doses. Away from home was the reason for poor adherence in one-fourth of the respondents. Nearly 18.75% of respondents reported missing medications when they felt symptomatically better. Another reason for missing medication was side effects and nonavailability of medicine [Table 5].
Table 5.
Reason for missing medications
Discussion
Demographic and epidemiological transition is resulting in surge of NCDs in India.[10] Studies have documented urban areas with higher prevalence of NCDs compared to rural areas in India. Reported prevalence of diabetes and hypertension in rural areas of Tamil Nadu was 36% and 59%, respectively.[11] Similar study by Kokiwar et al. in 2012 reported prevalence of hypertension in rural part of central India to be 19.04%.[12] The Indian Council of Medical Research-INdia DIABetes study in 2011 found weighted prevalence of diabetes (both known and newly diagnosed) to be 13.6% in Chandigarh. A study in 2011 found nearly 62.4 million people with diabetes and 77.2 million people with prediabetes living in India.[13]
With the looming threat of epidemic and increasing life expectancy of population, prevention of complications assumes significance. Adherence to the prescribed medicines and lifestyle recommendations are essential for the same.[14] There is mounting evidence that nonadherence to prescribed treatment is associated with adverse health outcomes and higher costs of care.[4] The impact of social determinants, for example, sex, socioeconomic status, and education, influences medication compliance behavior. Female gender, poverty, and poor education are associated with poor adherence behavior among study participants.[4,15] Moreover, economic burden of nonadherence in case of chronic diseases has been significant with cost to savings ratio of 1:10 in the United States.[16]
In the current study, more than 70% are aged above 50 years, illiterate (60%), and reported working. Ho et al. found prevalence of medication adherence depend on type of population and medicine.[14] Less than half (46.15%) of the study respondents reported missing medications prescribed to them. In a compliance study of elderly population for hypertension by Rajpura and Nayak, nearly 66% of study participants were nonadherent with their medications.[17] Medication adherence at home after hospital discharge was assessed by Gray et al. wherein under-adherence was reported in nearly 30.6% of study the respondents.[18]
Analysis revealed that perceptions of illness and beliefs about medication played a significant role in predicting medication adherence. In our study, perception of adherence to medication and dietary modifications was 67.3% and 59.4%, respectively. This is relatively high considering the poor education status of our study participants. The majority (90.8%) followed instructions delivered during consultation. Nearly 61.54% of study respondents were very sure that they will be able to take medicines as directed by the physician. This clearly suggests the need of counseling services in the management of chronic diseases involving geriatric patients. Thorough counseling given at the time of consultation will motivate the patient for treatment adherence and empower them to contribute actively to their disease management.
Reasons for poor medication adherence must be understood for ensuring treatment compliance. A study found six key factors that may contribute to intentional nonadherence among older adults: Illness beliefs, the perceived risks (e.g., dependence, adverse effects), benefits and necessity of potential treatments, the patient–practitioner relationship, inter-current physical and mental illnesses, financial constraints, and pharmaceutical/pharmacological issues (poly-pharmacy/regimen complexity).[19,20] Gadkari and McHorney reported that among 62% adults who forgot to take medications, 37% fell short of medicines and 23% were careless about taking medications.[21] Among patients, forgetting was the most frequently reported reason for nonadherence.[22] Besides forgetfulness, other reasons reported in a study included perceived side effects (20%), high drug costs (17%), and perception that prescribed medication would have little effect on disease (14%).[23] Similarly, in our study, forgetfulness was the most common reason for missing medication followed by trips outside home and feeling better symptomatically. This indicates lack of felt need or seriousness among patients for continued intake of medicines and deficiencies in counseling delivered at the time of consultation.[24]
Along with poor adherence to medication, poor adherence to prescribed lifestyle modification was also observed in case of chronic diseases. In our study, dietary regulations of fat, salt, and sugar were often violated by 29.8%, 21.63%, and 16.83% of the participants, respectively. Confidence to adhere to dietary regulations was present in 59.4% of patients. Consumption of tobacco and alcohol was not reported by majority (90%) of the study patients. Of 22 patients reported consuming alcohol, nearly 11 were drinking alcohol frequently in a week. This can be attributed to Punjab being predominantly occupied by the Sikh community which prohibits tobacco consumption and social desirability bias for response to alcohol question. In a study by Bisiriyu et al., estimated rates of nonadherence to diet and exercise were 37.4% and 52% among diabetic patients in Botswana, respectively.[25] Collins described military health-care providers adherence to guidelines and found low compliance with weight loss measures (36%), limitation of alcohol use (57%), need to increase physical activity (38%), and reduce sodium intake (6%).[26] In a study among diabetic patients in Bangladesh, nonadherence rates were as follows: diet (88%), exercise (25%), routine blood glucose testing (32%), foot care (70%), smoking (6%), and betel quid chewing habit (25%).[27] A prospective study in Kuwait found 63.5% patients not adhering to diet regimen, 64.4% not participating in regular exercise, and 90.4% overweight and obese.[28]
Nearly 58.17% of study patients reported having financial support for diagnosis and treatment in the current study. Only 33% males and 23.38% females were accompanied by caregivers for health check-ups. This emphasizes on the need of having accessible and affordable health services in the rural areas. Public health-care system of India should be equipped with free diagnostics and drugs for NCDs.
Conclusion
The government of India has well realized the threat of NCDs to the population in India. Efforts to control the same are underway by launching the National Program for Control of Diabetes, Cardiovascular Disease, and Stroke in 2010. Availability of free testing and treatment at different levels of health care has been envisaged in the program. However, with reported low levels of adherence to medication, diet, and lifestyle, there arises an urgent need of exploring innovative ways to ensure compliance. Modification of behavioral risk factors needed opportunistic screening alone will increase the cohort of diagnosed cases without any improvement in health outcomes. Commitment is needed to ensure availability and intake of drugs in screened along with lifestyle modifications. The National AIDS Control program, the Revised National Tuberculosis Control Program, and the National Malaria Eradication Program have ways to ensure medication compliance among patients. Similar need is felt in this program or else it will just contribute to updating the statistics of current morbidity and its risk factors.
Limitations of this study
The study has limitations as it has self-reported data on adherence to diet and medications. Actual measurement of adherence might be lower than the obtained estimate. Moreover, there is a need to conduct intervention studies that ensure compliance to medication and lifestyle measures. Recently, the Global Action Plan for the Prevention and Control of NCDs by WHO aims to prioritize care delivery for NCDs and ensures objective measurement of the same. India needs to realize that tackling the behavioral risk factors of NCD needs far more concerted effort that the program currently provides.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Murray CJ, Lopez AD. Global Health Statistics: Global Burden of Disease and Injury Series. I, II. Boston: Harvard School of Public Health; 1996. [Google Scholar]
- 2.Ghaffar A, Reddy KS, Singhi M. Burden of non-communicable diseases in South Asia. BMJ. 2004;328:807–10. doi: 10.1136/bmj.328.7443.807. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization. Adherence to Long Term Therapies: Evidence for Action. World Health Organization; 2003. [Last accessed on 2014 Feb 13]. Available from: http://www.whqlibdoc.who.int/publications/2003/9241545992.pdf . [Google Scholar]
- 4.Haynes RB, McDonald H, Garg AX, Montague P. Interventions for helping patients to follow prescriptions for medications. Cochrane Database Syst Rev. 2002;2:CD000011. doi: 10.1002/14651858.CD000011. [DOI] [PubMed] [Google Scholar]
- 5.Chia LR, Schlenk EA, Dunbar-Jacob J. Effect of personal and cultural beliefs on medication adherence in the elderly. Drugs Aging. 2006;23:191–202. doi: 10.2165/00002512-200623030-00002. [DOI] [PubMed] [Google Scholar]
- 6.Ministry of Health and Family Welfare. National Program for Prevention and Control of Cancer, Cardiovascular Disease, Diabetes and Stroke. Operational Guidelines. [Last accessed on 2014 Feb 13]. Available from: http://www.health.bih.nic.in/Docs/Guidelines/Guidelines-NPCDCS.pdf .
- 7.Sankar UV, Lipska K, Mini GK, Sarma PS, Thankappan KR. The adherence to medications in diabetic patients in rural Kerala, India. Asia Pac J Public Health. 2015;27:NP513–23. doi: 10.1177/1010539513475651. [DOI] [PubMed] [Google Scholar]
- 8.Sathvik BS, Karibasappa MV, Nagavi BG. Self-reported medication adherence pattern of rural indian patients with hypertension. Asian J Pharm Clin Res. 2013;6(Suppl 1):49–52. [Google Scholar]
- 9.Hinchageri S S, Patil N, Karan K, Shalini B, Swarnakamala K. Assessment of medication adherence and factors affecting to medication adherence in asthma patients by clinical pharmacist. International Research Journal of Pharmacy. 2012;3:211–15. [Google Scholar]
- 10.Quigley MA. Commentary: Shifting burden of disease – Epidemiological transition in India. Int J Epidemiol. 2006;35:1530–1. doi: 10.1093/ije/dyl244. [DOI] [PubMed] [Google Scholar]
- 11.Radhakrishnan S, Balamurugan S. Prevalence of diabetes and hypertension among geriatric population in a rural community of Tamil Nadu. Indian J Med Sci. 2013;67:130–6. [PubMed] [Google Scholar]
- 12.Kokiwar PR, Gupta SS, Durge PM. Prevalence of hypertension in a rural community of central India. J Assoc Physicians India. 2012;60:26–9. [PubMed] [Google Scholar]
- 13.Anjana RM, Pradeepa R, Deepa M, Datta M, Sudha V, Unnikrishnan R, et al. Prevalence of diabetes and prediabetes (impaired fasting glucose and/or impaired glucose tolerance) in urban and rural India: Phase I results of the Indian Council of Medical Research-INdia DIABetes (ICMR-INDIAB) study. Diabetologia. 2011;54:3022–7. doi: 10.1007/s00125-011-2291-5. [DOI] [PubMed] [Google Scholar]
- 14.Ho PM, Bryson CL, Rumsfeld JS. Medication adherence: Its importance in cardiovascular outcomes. Circulation. 2009;119:3028–35. doi: 10.1161/CIRCULATIONAHA.108.768986. [DOI] [PubMed] [Google Scholar]
- 15.Chen SL, Lee WL, Liang T, Liao IC. Factors associated with gender differences in medication adherence: A longitudinal study. J Adv Nurs. 2014;70:2031–40. doi: 10.1111/jan.12361. [DOI] [PubMed] [Google Scholar]
- 16.Levine DA, Morgenstern LB, Langa KM, Piette JD, Rogers MA, Karve SJ. Recent trends in cost-related medication nonadherence among stroke survivors in the United States. Ann Neurol. 2013;73:180–8. doi: 10.1002/ana.23823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rajpura J, Nayak R. Medication adherence in a sample of elderly suffering from hypertension: Evaluating the influence of illness perceptions, treatment beliefs, and illness burden. J Manag Care Pharm. 2014;20:58–65. doi: 10.18553/jmcp.2014.20.1.58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gray SL, Mahoney JE, Blough DK. Medication adherence in elderly patients receiving home health services following hospital discharge. Ann Pharmacother. 2001;35:539–45. doi: 10.1345/aph.10295. [DOI] [PubMed] [Google Scholar]
- 19.Iuga AO, McGuire MJ. Adherence and health care costs. Risk Manag Healthc Policy. 2014;7:35–44. doi: 10.2147/RMHP.S19801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mukhtar O, Weinman J, Jackson SH. Intentional non-adherence to medications by older adults. Drugs Aging. 2014;31:149–57. doi: 10.1007/s40266-014-0153-9. [DOI] [PubMed] [Google Scholar]
- 21.Gadkari AS, McHorney CA. Unintentional non-adherence to chronic prescription medications: How unintentional is it really? BMC Health Serv Res. 2012;12:98. doi: 10.1186/1472-6963-12-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boskovic J, Leppée M, Culig J, Eric M. Patient self-reported adherence for the most common chronic medication therapy. Scand J Public Health. 2013;41:333–5. doi: 10.1177/1403494812471447. [DOI] [PubMed] [Google Scholar]
- 23.Boston Consulting Group. The hidden epidemic: Finding a cure for unfilled prescriptions and missed doses. 2003. [Last accessed on 2013 Sep 10]. Available from: http://www.bcg.com/documents/file14265.pdf .
- 24.Voils CI, Maciejewski ML, Hoyle RH, Reeve BB, Gallagher P, Bryson CL, et al. Initial validation of a self-report measure of the extent of and reasons for medication nonadherence. Med Care. 2012;50:1013–9. doi: 10.1097/MLR.0b013e318269e121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bisiriyu Non-Adherence to Lifestyle Modification. Recommendations (Diet and Exercise) Amongst Type 2 Diabetes Mellitus Patients Attending Extension II Clinic in Gaborone, Botswana. [Last accessed on 2014 Feb 13]. Available from: http://www.ul.netd.ac.za/bitstream/10386/259/1/Dr%20Ganiyu%20final.pdf .
- 26.Collins T. Uniformed Services Univ of the Health Sciences Bethesda, MD. Adherence to Hypertension Management Recommendations for Patient Follow-Up Care and Lifestyle Modifications Made by Military Healthcare Providers. 2000. [Last accessed on 2016 Oct 10]. Available from: https://www.google.co.in/url?sa=t&rct=j&q=&esrc=s&source=web&cd=1&cad=rja&ved=0CCkQFjAA&url=http%3A%2F%2Fwww.dtic.mil%2Fcgibin%2FGetTRDoc%3FAD%3DADA421146&ei= QWf8UovzOIuRrAeArIGgBA&usg=AFQjCNHFX2U81i8e9n3Chm5Zad9xVS87tw&sig2=i2SOckEIcHVgWlUvfW0KGA .
- 27.Mumu SJ, Saleh F, Ara F, Afnan F, Ali L. Non-adherence to life-style modification and its factors among type 2 diabetic patients. Indian J Public Health. 2014;58:40–4. doi: 10.4103/0019-557X.128165. [DOI] [PubMed] [Google Scholar]
- 28.Serour M, Alqhenaei H, Al-Saqabi S, Mustafa AR, Ben-Nakhi A. Cultural factors and patients’ adherence to lifestyle measures. Br J Gen Pract. 2007;57:291–5. [PMC free article] [PubMed] [Google Scholar]


