Abstract
Background:
Promoting family planning practices aid considerably in attaining Millennium Development Goals by various mechanisms. Despite concerted health system efforts, adoption of especially reversible contraceptive methods such as intrauterine devices (IUDs) has remained negatively skewed in India, which is the pioneer country to implement Family Planning programme way back in 1952. Although few studies in India have looked into the reasons for its nonacceptance, literature from Odisha was scant and hence the study was undertaken.
Methodology:
A cross-sectional study using qualitative methods was done in the Mahanga Tehsil of Cuttack district. In-depth interviews were conducted with women of reproductive age (WRA) and focused group discussions (FGDs) among health workers and health professionals were held separately. Data analysis was done using thematic framework approach supported by Atlas Ti software.
Results:
There were 31 in-depth interviews with WRA, two FGDs with health workers, and one FGD with health professionals. Availability of IUD services was low and wherever available, being located far away affected its physical accessibility. Most women were reluctant to ask health workers about services owing to their shyness while many women felt using IUDs breached their autonomy and privacy. The existence of fear and misconceptions regarding its use rooting from lack of knowledge and poor service quality also impeded its adoption by women.
Conclusion:
There is a pressing need to enhance the demand of IUDs by dispelling the myths among women through effective information, education, and communication and also to improve the availability of IUDs.
Keywords: Contraceptive, health, intrauterine device, qualitative research, women
Introduction
Family planning helps women prevent unintended pregnancies, delay early childbearing, and space births at least 2 years apart.[1] Fostering family planning practice alleviates poverty, accelerates socioeconomic development, increases child schooling, promotes gender equality, and decreases maternal and infant mortality.[2] As per the United Nations Population Fund estimates, widespread use of family planning could lower Maternal Mortality Ratio (MMR) by 20% and Infant Mortality Rate by as much as 25–30% in developing countries. Thus, there is a growing consensus that a good approach to family planning would help in achieving the Millennium Development Goals (MDGs). An important cause for these high fertility rates is the low availability and use of family planning services.[3,4]
India is the second most populous country in the world and also was the pioneer to launch the Family Planning Programme as early as in 1952. Subsequently, its name got changed to Family Welfare Programme and then to Reproductive and Child Health Programme. This change was made to emphasize and increase the acceptance of contraceptive methods. Since its inception in 1951, the National Family Planning Programme has been dominated by demographic goals by focusing primarily on sterilization, largely obviating client choice, and limiting availability to a narrow range of services. In April 1996, the Indian government abolished method-specific family planning targets throughout the country. In October 1997, India reoriented the national program's approach to more broadly address health and family limitation needs. The new approach involved a more comprehensive set of reproductive and child health services and a focus on client choice, service quality, gender issues and underserved groups, including adolescents, men, and postmenopausal women. The Family Welfare Programme in India explains that small differences in the family size will have a tremendous impact on the population growth. Hence, the objective of Family Welfare Programme is that the people should adopt the small family norm to stabilize the country's population at the level of some 1533 million by the year 2050.[5]
Despite concerted efforts by the health system in promotion of family planning services, the unmet need for contraception still remains a problem. As per District Level Household and Facility Survey (DLHS)-3 estimates the Contraceptive Prevalence Rate (CPR) for India is 47.1 percent while the unmet need of contraception is 21.3%, with 7.9% for spacing, and 13.4 percent for limiting births.[2,6,7] The intrauterine device (IUD) is the most frequently used reversible family planning method worldwide. However, its acceptability and usage are low in many developing countries with a majority of women choosing female sterilization or oral contraceptive pills (OCP) for birth control.[8] According to Health and Family Welfare Statistics 2014–2015, there were 5,277,460 IUD insertions in India compared to 5,602,284°CP users.[9]
Odisha is the eleventh populous state in India having a MMR of 235 (SRS 2010–2012) which is much above the national average and obviously far away from the MDG-5 target.[10] The CPR in Odisha is 46.8% for any modern method according to Annual Health Survey 2011–2012 while according to DLHS-3, the unmet need for contraception in Odisha is about 19.8%, of which 6.5% is for spacing and 13.3% for limiting.[2,6,7] Again, according to Health and Family Welfare Statistics 2014–2015, in Odisha, there were 84,608 IUD insertions compared to 154,929 OCP users showing a very stark disparity.[9]
There are few studies in India examining the reasons for nonacceptance of IUDs and perceptions of women, but there is no study done in Odisha. Thus, this study aimed to explore the prevalent perspectives regarding IUD (CuT) from a multistakeholder perspective.
Methodology
Study design
We did a cross-sectional study using qualitative methods among three groups of people who were recruited using a purposive sampling.
Study setting
Mahanga tehsil of Cuttack district was chosen since it is the largest with 192 villages, 29 subcenters, and a population of 186,930 as per census 2011.
Data collection
The study was conducted from June to August 2014. All study tools were used in Odia language. First, women of reproductive age group (WRA), i.e., belonging to age group of 15–49 years from different villages under Mahanga Community Health Centre (CHC) were interviewed to find out the perception of the beneficiaries about the contraceptive services being provided to them. In-depth interviews were done for 31 beneficiaries selected through purposive sampling so as to have uniform representation of tribal and general population. We used an in-depth interview guideline including six structured questions for capturing the sociodemographic details. Second, health workers (Auxiliary Nurse Midwives or ANMs) were interviewed to know about the enablers and barriers of the contraceptive services, especially IUD being provided as experienced by them. Two focused group discussions (FGDs) comprising six members each were done with the health workers (ANMs) using an FGD guideline. Third, health professionals from different fields were interviewed to explore the challenges contraceptive services and come up with possible solutions. An FGD was conducted with 10 health professionals using a FGD guideline.
Data analysis
Grounded theory approach was used to sum-up the collected data. In-depth interviews and FGDs were transcribed and translated to English. Coding was done, and they were successively condensed into relevant subthemes and themes. Atlas Ti (Version 7 [Computer sofware], Berlin, Scientific Sofware Development)software was used, and ultimately representation was done using the thematic framework approach.
Ethical considerations
Informed consent was obtained from all the participants and thus the participation was purely voluntary. Adequate privacy was ensured while conducting interviews. Confidentiality and anonymity were maintained during the procedure. Necessary ethical approval was obtained from the Institutional Ethics Committee of the Indian Institute of Public Health-Bhubaneswar.
Results
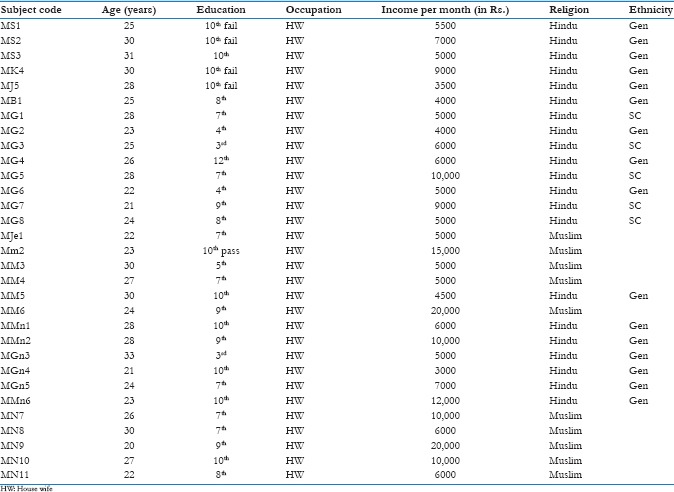
There were total 31 participants for in-depth interviews having median age of 26 years while the lowest was 20 years and highest being 33 years. All were homemakers and majority had low educational level. Sixteen women were of Hindu general caste; five women were of Hindu scheduled caste while ten women belonged to Muslim religion. The majority of women's household monthly income was below Rs. 10,000. Their detailed individual sociodemographic profiles are depicted in Annexure 1.
Key issues emerging from in-depth interviews, and FGDs were identified and then condensed into the following thematic areas.
Accessibility
Women felt the CHC was far away, and so services offered there were physically inaccessible to them. ANMs added that women had to arrange their transportation out of their pocket raising economic concerns. Women felt embarrassed to enquire and discuss the methods of contraception and sex-related topics freely with them leading to lack of information access.
“I had heard the word CuT but thought that it was an operative procedure, and as Accredited Social Health Activist (ASHA) is senior to me in age, I felt shy to ask her in detail about CuT” (Respondent MMn6).
“I feel bad to talk about this bad issue with others” (Respondent MS1).
Health professionals believed that the beneficiaries should be comfortable with the person who is distributing the contraceptives and outlets for distribution should be opened up at convenient places for improving access issues.
Availability
The beneficiaries said that the nearby subcenters though equipped for IUD services did not had trained staffs to deliver them. Most ANMs also reiterated the fact. Health professionals felt availability and accessibility were interrelated. They suggested that contraceptive services should be made universally available as a basket of choice so that people could access it easily.
Autonomy and privacy
Few women said that they enjoyed the freedom of getting oral pills from shops by not depending on ASHAs or ANMs, and they felt that in taking oral pills their privacy was not hampered where as in IUD service their privacy was hampered.
“I know CuT but my husband does not recommend CuT, so I cannot use” (Respondent MG5). ANMs too reported that women liked to preserve their autonomy and privacy and not depend on anyone while using contraceptive methods. Health professionals suggested, if the mother-in-law or the husband was motivated, they could help the woman in reaching out for the IUDs as well as maintain adequate privacy.
Misconceptions
The interviewed women harbored varying misconceptions regarding CuT like “it may or may not suit,” “it will melt inside body,” “it will go inside chest,” “it will go inside abdominal cavity,” “it will cause cancer,” “it will stick to the wall permanently.” ANMs further added that women felt that it results in white badly smelling discharge, permanently stay in abdomen, cause secondary infertility, swelling of abdomen, anemia, headache, head reeling, weakness, and irregular menses. Health professionals opined that although IUDs were very effective, wrong notions among women about it were major hurdles for their uptake and the service providers were yet to clarify the misconceptions effectively.
Fear
Women reported that they were afraid of instrumentation and also the side effects of IUDs postinsertion such as bleeding, abdominal cramps, and apprehensive of unusual reactions. ANMs seconded the women's fear. Health professionals discerned that fear and misconceptions were obvious to crop up, but these could be alleviated by the positive teachings of the health workers. They emphasized the importance of knowledge imparting periodically.
Awareness and knowledge
Many women lacked knowledge about IUDs because they said there was inadequate promotion of the method by health-care providers as well as their illiteracy. They felt partial dissemination of information by health-care providers often led to wrong perceptions in their minds. ANMs propounded that women were not aware of the contraceptive methods, and there were no information education and communication (IEC) and Behaviour Change Communication (BCC) programs running from government side for raising awareness. Health professionals felt that both the beneficiaries as well as the providers were often unaware of the government policies, and there must be initiatives to improve methods so as to impart more knowledge and awareness among all sections to reduce disparity.
Quality
Women raised concerns about service quality. They expected motivation from doctors and not just from ANMs or ASHAs. They also felt that Village Health and Nutrition Day (VHND) spots were not suitable places for them to gather and avail the service. Some women had an idea that IUD services were expensive. Most women said that ASHAs did not say much about CuT but promoted more about sterilization and oral pills. ANMs reiterated the lack of user-friendliness of VHND spots for women to interact with health providers and said beneficiaries took them less seriously and thus relied less on them. Health professionals highlighted that people preferred things which were beneficial, low cost, easily available as well as highly effective. They suggested that if all these could be possible only if government gave prior attention to the quality of services rather than forcing on things or simply trying to explain the benefits.
Thus, analyses brought forward various perspectives across multiple stakeholders, namely, WRA, health workers, and health professionals shrouding the issue of contraception, especially IUDs.
Discussion
According to the Health Belief Model (HBM), four factors influence an individual's protective health behaviors: perception of susceptibility to negative health outcomes, perception of the severity of the negative outcome, benefits of preventive behavior in relation to the potential negative outcome, barriers, and perceived barriers to implementing the protective behavior. Although some find the HBM to be outdated, the original constructs and concepts can still be considered in gaining insight into decision-making regarding sexual behaviors and risk-taking.[11,12]
In rural areas, many women were unaware of the contraceptive methods leading to low demand of this service from health-care providers. Most of the women thought contraception meant pills. Out of 31 women, 12 had never heard the word CuT. Eight out of 19 women, who had heard about CuT, knew no more than that. An operational research study done in Gujarat stressed the importance of IEC which improved client performance after the intervention.[13]
From among the 11 women who knew about IUDs in details, all had fear of side effects. They had less perceived benefits of CuT over oral pills. This might had been due to the differential dissemination of information by health-care providers. Moreover, the women narrated that the ASHAs motivated them more about sterilization and pills. This may be because there is no incentive for promoting IUDs while that for sterilization is incentivized. The studies by Rati et al. and Murarkar et al. mentioned that scattered knowledge of women regarding contraceptives led to myths and misconceptions resulting in nonacceptance of IUD as a spacing method.[14,15]
Loads of misconceptions existed in the minds of women. Discussing sex-related issues was a forbidden issue for them, and it had been a social norm to maintain secrecy regarding this matter. Thus, most women could not replace their myths with correct information. A hospital-based study in Bhopal also reiterated the fact of the presence of deep-rooted misconceptions dissuading them from accepting IUDs.[16]
Variation of autonomy in the selection of contraceptive methods arose due to the ignorance of the women, especially housewives, dominance of husbands and mother-in-laws, associated stigma, and lack of privacy. Similar results were found in a study by Yadav et al. on agreement and concordance regarding reproductive intentions and contraception between husbands and wives in rural Ballabgarh, India.[17]
Almost all ANMs admitted that many women did not take their advice seriously. VHND spots were neither user-friendly nor had privacy, which were essential for providing services. Women mostly of low income and low literacy status thought it to be a credit to manage spacing between pregnancies without using any method. These women either used calendar method or withdrawal method. Few bitter experiences from peer groups became propaganda, and even ASHAs were unable to persuade them in the right direction with proper information. Most Muslim women did not use contraceptive methods except some who used withdrawal technique and oral pills.
Thus, we can understand that the issue of family planning is deeply rooted in an array of individual and social factors making it relevant to family physicians since their practice involves considering the person as a whole.
Conclusion and Recommendations
This study focused on the exploration of factors influencing the acceptability of contraceptives, especially IUDs among WRA. Most of the rural women were not aware of the necessity of an effective contraception to avoid unwanted pregnancy. More than two-thirds of the interviewed women in rural settings did not know about the CuT method. Among those who knew about the method, most did not use it either due to fear of side effects or some prevalent myths. Some were reluctant about the method because they felt lack of autonomy and privacy. Some were unable to avail the services because of restrictions by their husbands and in-laws. In addition, such services were inaccessible and were not up to an acceptable quality.
Because of the above facts, there was low demand from the acceptors’ side. The findings that had emerged from this study thus provide some recommendations to increase the demand. Effective IEC, BCC should be promoted continuously with the help of health workers for better acceptance of CuT. VHND sessions should be improved in respect of site, logistics, and trained health providers.
At facility level, i.e., at subcenters, quality services should be made available. Doctors and health workers should be trained in large numbers for providing quality services.
Majority women recommended that interactive sessions between doctors and women should be undertaken at community level, maybe conducting “swasthya-melas” frequently. Improving education level of rural women might modify the sociocultural aspects of extreme shyness and maintaining social distances.
Thus, a concerted effort with collaboration and cooperation of various sectors and departments are warranted to fulfill the vision and mission more accurately.
Financial support and sponsorship
This study was a part of Postgraduate Diploma in Public Health Management dissertation work.
Conflicts of interest
There are no conflicts of interest.
Acknowledgments
We gratefully thank all the study participants comprising WRA, health workers, and health professionals. We also sincerely thank the Government of Odisha for nominating the candidate for the course.
Annexure 1: Sociodemographic profile of in.depth interviews participants
References
- 1.New Delhi: Policy Unit, NIHFW; 2014. National Institute Health and Family Welfare. Population and Development: A Discourse on Family Planning in Odisha. [Google Scholar]
- 2.Kols A. Reducing unmet need for family planning: Evidence-based strategies and approaches. Outlook. 2008;25:1. [Google Scholar]
- 3.Ringheim K, Gribble J, Foreman M. Integrating family planning and maternal and child health care: Saving lives, money, and time. Int Fam Plan Perspect. 2007;33:6–12. [Google Scholar]
- 4.Abrejo FG, Shaikh BT, Saleem S. ICPD to MDGs: Missing links and common grounds. Reprod Health. 2008;5:4. doi: 10.1186/1742-4755-5-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Visaria L, Jejeebhoy S, Merrick T. From family planning to reproductive health: Challenges facing India. Int Fam Plan Perspect. 1999;1:S44–9. [Google Scholar]
- 6.International Institute for Population Sciences (IIPS). National Family Health Survey (NFHS-3), 2005-06. Mumbai: International Institute for Population Sciences; 2007. [Google Scholar]
- 7.Mumbai: International Institute for Population Sciences; 2010. International Institute for Population Sciences (IIPS). District Level Household and family Survey (DLHS-3), 2007-08. [Google Scholar]
- 8.Ambadekar NN, Rathod KZ, Zodpey SP. Study of cu T utilization status and some of the factors associated with discontinuation of cu T in rural part of yavatmal district. Indian J Community Med. 2011;36:54–6. doi: 10.4103/0970-0218.80795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ministry of Health and Family Welfare. Family Welfare Statistics in India 2015. New Delhi: Ministry of Health and Family Welfare. 2016 [Google Scholar]
- 10.National Health Mission. Health Statistics. Department of Health and Family Welfare, Government of Odisha. [Last cited on 2016 Sep 13]. Available from: http://www.nrhmorissa.gov.in/frmhealthstatistics.aspx .
- 11.Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun. 2010;25:661–9. doi: 10.1080/10410236.2010.521906. [DOI] [PubMed] [Google Scholar]
- 12.Downing-Matibag TM, Geisinger B. Hooking up and sexual risk taking among college students: A health belief model perspective. Qual Health Res. 2009;19:1196–209. doi: 10.1177/1049732309344206. [DOI] [PubMed] [Google Scholar]
- 13.Khan ME, Kar SS, Desai VK, Patel P, Itare BP, Barge S. Increasing the Accessibility, Acceptability and Use of the IUD in Gujarat, India. Frontiers Final Report; May. 2008 [Google Scholar]
- 14.Rati MS, Jawadagi MS, Pujari MJ. A study to assess the factors affecting acceptance of intrauterine device (IUD) among rural women of Hirebagewadi, Belgaum. IOSR J Nurs Health Sci. 2014;3:37–52. [Google Scholar]
- 15.Murarkar SK, Soundale SG, Lakade RN. Study of contraceptive practices and reasons for not accepting contraceptives in rural India: Chanai village as a case study. Indian J Sci Technol. 2011;4:915–6. [Google Scholar]
- 16.Gadre SS, Ahirwar R. Level of acceptance of IUCD insertion in Indian women-a cross-sectional mixed research from central India. Int J Reprod Contracept Obstet Gynecol. 2015;4:1079–85. [Google Scholar]
- 17.Yadav K, Singh B, Goswami K. Agreement and concordance regarding reproductive intentions and contraception between husbands and wives in rural Ballabgarh, India. Indian J Community Med. 2010;35:19–23. doi: 10.4103/0970-0218.62548. [DOI] [PMC free article] [PubMed] [Google Scholar]


