Abstract
Abdominal cocoon is one of the rare causes of intestinal obstruction. It is referred as complete or partial small bowel encapsulation caused by the thick fibrocollagenous membrane. It is most common in young adolescent girls. We present a 40-year-old male patient with idiopathic abdominal cocoon. Few cases of male patients suffering from idiopathic abdominal cocoon have been reported in literature.
Keywords: Abdomen, abdominal cocoon, computed tomography, intestinal obstruction
Introduction
Abdominal cocoon is referred as a complete or partial small bowel encapsulation caused by dense fibrocollagen membranes leading to acute or chronic small bowel obstruction. It was first termed as peritonitis chronic fibrosain capsulata by Owtschinnikow in 1907 and finally abdominal cocoon by Foo in 1978.[1] It is most commonly seen in adolescent girls of tropical and subtropical region though few cases of male have also been reported in literature.[1,2]
Case Report
A 40-year-old male patient presented with C/O abdominal pain for last few months. The patient had past H/O abdominal pain which was relieved by treatment. The patient also complained of difficulty in passing stools. There was no associated fever and vomiting. On physical examination, there was tenderness over the right iliac fossa.
The patient underwent computed tomography (CT) abdomen and pelvis (plain and contrast) which showed localized clumping of the small bowel in center of the abdomen with matting. The loops were seen within thin-walled sac-like structure containing localized fluid. Mostly duodenojejunal flexure and proximal part of jejunal loops were embedded within sac [Figures 1 and 2].
Figure 1.
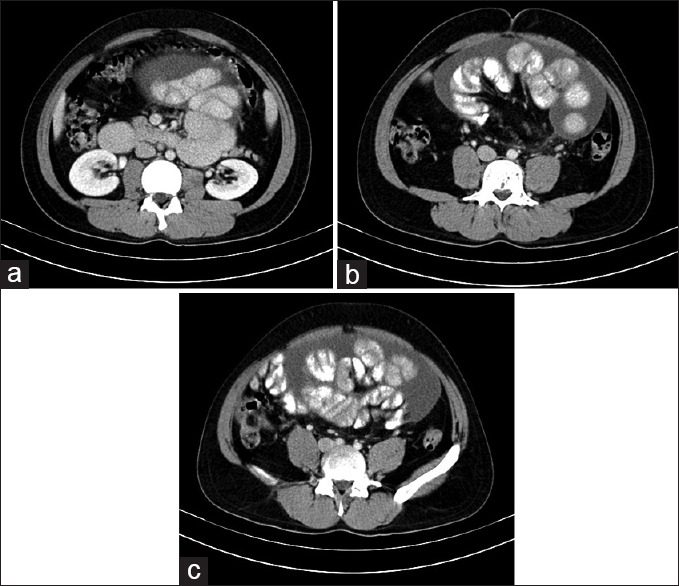
(a-c) Axial section showing clumping of duodenojejunal flexure and proximal part of jejunum embedded within thin-walled fluid filled sac-like structure
Figure 2.
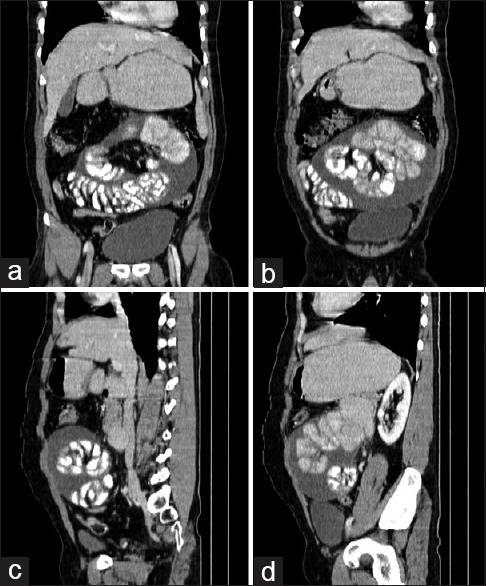
(a-d) Coronal and sagittal showing clumping of duodenojejunal flexure and proximal part of jejunum embedded within thin-walled fluid filled sac-like structure
Discussion
There are various etiologies of intestinal obstruction which includes external hernia, volvulus, tuberculosis (TB), and postoperative or inflammatory adhesion. All of these are common in India.[3] Abdominal cocoon is one of the rare condition causing acute to subacute intestinal obstruction.[4] The exact pathogenesis is not known, but it is assumed to be due to peritoneal irritation which further causes inflammation and fibrosis. As a result of inflammation, intraperitoneal fibrin-like material is released by fibrogenic cytokines forming thick shiny membranes encasing whole or part of bowel giving a characteristic appearance to the disease.[2,5]
Abdominal cocoon can be either primary or secondary. The primary etiology is idiopathic and tends to occur most commonly in adolescent girls in tropical and subtropical countries. The theory postulated behind the occurrence of primary cause is subclinical primary viral peritonitis either due to immunological reaction to gynecological infection or retrograde menstruation and retrograde infection of the fallopian tube.[6] Whereas secondary cause is generally linked with abdominal TB, continuous and automated peritoneal dialysis, liver cirrhosis, and practolol therapy.[7] Since our patient had no secondary cause, the diagnosis of primary cocoon was considered. Idiopathic form of abdominal cocoon rarely occurs in male patient as seen in our case.[1]
Radiological imaging plays a vital role in reaching the preoperative diagnosis of the abdominal cocoon. When CT scan was not available, barium study was the primary mode to identify the disease which showed serpentine- or concertina-like configuration of dilated small bowels in a fixed U-shaped cluster or cauliflower sign as described by Sieck et al. in 1983.[3] Abdominal ultrasound reveals echogenic mass with small bowel loop dilatation encircled by a thick rim of hypoechoic fibrous membrane.[3,8] Ultrasound sonography and X-ray are not as good as CT or magnetic resonance imaging (MRI) in diagnosing this condition. CT scan is the primary imaging modality to confirm the presence of abdominal cocoon.[9] CT shows clumping of the entire small bowel enclosed by soft tissue density mantle located at the midpoint of abdominal cavity.[10] Findings in MRI were similar to that of CT. Coronal MRI revealed similar pattern as in barium studies.[11]
Biopsy shows thickened fibrocollagenous tissue with or without long-term inflammation in form of lymphocytic and plasma cell infiltrates.[3,11] Its differential diagnosis includes congenital peritoneal encapsulation, peritonitis carcinomatosa, pseudomyxoma peritoneal mesothelioma, and tuberculous peritonitis.[5,12] In case of asymptomatic or patients with mild symptoms, it can be treated conservatively by intestinal rest, nasogastric intubation, and enteral or parenteral nutritional support.[6] Whereas in moderate to severe cases, both medical (corticosteroid and tamoxifen therapy) and surgical treatment are used. Ideally surgical excision with laparoscopic approach is better choice to excise encapsulating membrane with adhesiolysis thus leading favorable outcomes and excellent prognosis.[7]
Conclusion
Abdominal TB can lead to abdominal cocoon and thus cause intestinal obstruction and in patients presenting with intestinal obstruction, abdominal TB should be ruled out, especially at rural places where abdominal TB has high prevalence.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Solak A, Solak I. Abdominal cocoon syndrome: Preoperative diagnostic criteria, good clinical outcome with medical treatment and review of the literature. Turk J Gastroenterol. 2012;23:776–9. doi: 10.4318/tjg.2012.0500. [DOI] [PubMed] [Google Scholar]
- 2.Oran E, Seyit H, Besleyici C, Ünsal A, Alis H. Encapsulating peritoneal sclerosis as a late complication of peritoneal dialysis. Ann Med Surg (Lond) 2015;4:205–7. doi: 10.1016/j.amsu.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rastogi R. Abdominal cocoon secondary to tuberculosis. Saudi J Gastroenterol. 2008;14:139–41. doi: 10.4103/1319-3767.41733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uzunoglu Y, Altintoprak F, Yalkin O, Gunduz Y, Cakmak G, Ozkan OV, et al. Rare etiology of mechanical intestinal obstruction: Abdominal cocoon syndrome WJCC. World. 2014;2:728–31. doi: 10.12998/wjcc.v2.i11.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Acar T, Kokulu I, Acar N, Tavusbay C, Haciyanli M. Idiopathic encapsulating sclerosing peritonitis. Ulus Cerrahi Derg. 2015;31:241–3. doi: 10.5152/UCD.2015.2786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yavuz R, Akbulut S, Babur M, Demircan F. Intestinal obstruction due to idiopathic sclerosing encapsulating peritonitis: A case report. Iran Red Crescent Med J. 2015;17:e21934. doi: 10.5812/ircmj.17(5)2015.21934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sohail MZ, Hasan S, Dala-ali B, Ali S, Hashmi MA. Case Report Multiple Abdominal Cocoons: An Unusual Presentation of Intestinal Obstruction and a Diagnostic Dilemma. Hindawi Publishing Corporation; Case reports in surgery. 2015;2015:4–7. doi: 10.1155/2015/282368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Al Ani AH, Al Zayani N, Najmeddine M, Jacob S, Nair S. Idiopathic sclerosing encapsulating peritonitis (abdominal cocoon) in adult male. A case report. Int J Surg Case Rep. 2014;5:735–8. doi: 10.1016/j.ijscr.2014.07.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta S, Shirahatti RG, Anand J. CT findings of an abdominal cocoon. AJR Am J Roentgenol. 2004;183:1658–60. doi: 10.2214/ajr.183.6.01831658. [DOI] [PubMed] [Google Scholar]
- 10.Hur J, Kim KW, Park MS, Yu JS. Abdominal cocoon: Preoperative diagnostic clues from radiologic imaging with pathologic correlation. AJR Am J Roentgenol. 2004;182:639–41. doi: 10.2214/ajr.182.3.1820639. [DOI] [PubMed] [Google Scholar]
- 11.Menassa-Moussa L, Bleibel L, Sader-Ghorra C, Smayra T, Aoun NJ. MRI findings in intestinal cocoon. American Journal of Roentgenology. 2006;186:905–6. doi: 10.2214/AJR.05.0252. [DOI] [PubMed] [Google Scholar]
- 12.Tombak MC, Apaydın FD, Çolak T, Duce MN, Balcı Y, Yazıcı M, et al. An unusual cause of intestinal obstruction: Abdominal cocoon. American Journal of Roentgenology. 2010;194:W176–8. doi: 10.2214/AJR.09.3083. [DOI] [PubMed] [Google Scholar]


