Abstract
The biological basis for the poor immunogenicity of unadjuvanted avian influenza A virus vaccines in mammals is not well understood. Here, we mutated the hemagglutinin (HA) of two H1N1 virus vaccines to determine whether virus receptor binding specificity contributes to the low immunogenicity of avian influenza virus vaccines. Mutations were introduced into the HA of an avian influenza virus, A/Duck/New York/15024–21/96 (Dk/96) which switched the binding preference from α2,3- to α2,6-linked sialic acid (SA). A switch in receptor specificity of the human A/South Carolina/1/18 (SC/18) virus generated a mutant virus with α2,3 SA (avian) binding preference. Inactivated vaccines were generated and administered to mice and ferrets intramuscularly. We found that the vaccines with human receptor binding preference induced slightly higher antibody titers and cell-mediated immune responses compared to their isogenic viruses with avian receptor binding specificity. Upon challenge with DK/96 or SC18 virus, differences in lung virus titers between the vaccine groups with different receptor-binding specificities were minimal. Overall, our data suggest that receptor binding specificity contributes only marginally to the immunogenicity of avian influenza vaccines and that other factors may also be involved.
Keywords: Influenza virus, Immunogenicity, Receptor binding specificity, Inactivated whole virus vaccine
Introduction
Avian influenza A subtype viruses continue to pose a significant threat to human health. Multiple subtypes of avian influenza viruses including H5, H6, H7, H9 and H10 have caused infection in humans primarily through direct transmission from infected poultry (Butt et al., 2005; Koopmans et al., 2004; Subbarao and Joseph, 2007; Yuan et al., 2013). Human infection with avian influenza viruses can be severe, causing high mortality (up to 58%) as reported for H5N1 virus infection (Beigel et al., 2005). In the spring of 2013, a new subtype of avian influenza A(H7N9) virus emerged in China (Gao et al., 2013), and as of February 28, 2014, the World Health Organization (WHO) had reported over 375 confirmed cases of human infection, with a case fatality rate of approximately 30% (http://www.who.int/en/). The increasing numbers of human avian influenza cases highlight the need to strengthen prevention and treatment efforts.
Vaccination has been the principal public health method for preventing and controlling seasonal influenza in humans and the design of more effective vaccines against avian influenza A viruses is an important part of pandemic preparedness. A variety of avian influenza virus vaccines, including inactivated (whole, split or subunit), live attenuated vaccines or recombinant protein vaccines have been developed, some of which have been tested in humans (Atmar et al., 2006; Bresson et al., 2006; Couch et al., 2012; Keitel et al., 2008; Patel et al., 2012; Tretyakova et al., 2013). Although the efficacy of avian influenza vaccines varies depending on the vaccine formulations and routes of administration, most of the studies agree that unadjuvanted avian influenza vaccines are poorly immunogenic compared to seasonal H1N1 and H3N2 influenza virus vaccines (Atmar et al., 2006; Bresson et al., 2006; Couch et al., 2012; Keitel et al., 2008; Patel et al., 2012). In one study, a two-dose regimen of 90 μg of H5 hemagglutinin (HA) subvirion vaccine resulted in only 58% of recipients showing a neutralizating antibody titer of 1:40 or greater (Treanor et al., 2006). In contrast, approximately 90% of adults demonstrated similar antibody titers when a single-dose of 15 μg of 2009 H1 HA vaccine was administered (Zhu et al., 2009). While these differences may, in part, be due to differences in priming, there remains a need for further research into improving the immunogenicity of vaccines that use avian influenza virus seed strains.
The HA is the major target of host immune recognition and an anti-HA antibody can provide protection against influenza virus infection by blocking viral attachment to the host cell (Han and Marasco, 2011). The HA glycoprotein is also responsible for both receptor binding and the subsequent fusion of viral and host endosomal membranes (Skehel and Wiley, 2000). HA recognizes a common ligand, the terminal sialic acid (SA) presented on either glycoproteins or glycolipids (Skehel and Wiley, 2000). Structurally, the HA receptor binding site is located in a shallow depression in the globular head region of the HA trimer protein and is composed of well-known structural elements such as the 220 loop, 130 loop, 150 loop and 190 helix (H3 numbering) (Skehel and Wiley, 2000). Although the overall structure of HA is conserved across all influenza A subtype viruses, the fine variations in the HA receptor binding pocket confer recognition specificity for the specific linkage between terminal SA and the penultimate galactose residue (Xu et al., 2013). In general, avian influenza viruses preferentially bind to α2,3-linked SA whereas human influenza viruses preferentially attach to host airway cells expressing α2,6-linked SA (Connor et al., 1994; Rogers and Paulson, 1983). Sequence alignments of influenza A HA genes have identified key receptor specificity determining residues and as few as one or two amino acid mutations are sufficient to alter the receptor-binding specificity of some influenza A viruses. For example, two residues at positions 226 and 228 in the HA of H2, H3 and H6 subtypes directly contribute to viral receptor specificity; L226/G228 for α2,6 SA binding, Q226/G228 for α2,3 SA binding and L226/S228 showing dual receptor binding (Chen et al., 2012; Connor et al., 1994; Rogers and Paulson, 1983). For influenza H1 subtype, the HA receptor specificity-determining residues are located at positions 190 and 225 (H3 numbering); human influenza viruses generally have an Asp amino acid residue at positions 190 and 225, whereas influenza viruses with Glu-190/Gly-225 confer binding specificity to an avian-type receptor (Glaser et al., 2005; Zhang et al., 2013). However, for other subtypes of influenza the key residues governing receptor binding specificity are less defined and it appears that the amino acids outside of the receptor binding pocket also affect receptor binding specificity as recently shown among avian H5N1 viruses (Herfst et al., 2012; Imai et al., 2012). Moreover, viral receptor binding specificity affects viral pathogenesis and transmissibility (Qi et al., 2009; Tumpey et al., 2007).
Recently, it was demonstrated that live attenuated influenza H2 and H6 vaccine viruses with dual receptor binding are able to elicit better immune responses in ferrets compared to viruses with α2, 3-SA binding specificity (Chen et al., 2012; Connor et al., 1994; Rogers and Paulson, 1983). In the current study, we evaluated the contribution of receptor binding specificity to the immunogenicity and effectiveness of inactivated influenza vaccines. We altered the receptor binding preference of two H1N1 viruses and compared both humoral and cell-mediated immune responses in mice and ferrets following vaccination and found that viruses with preferential affinity for α2,6-linked SA only moderately improved the immunogenicity of inactivated vaccines.
Results
Altering receptor binding specificity has no significant effect on viral fitness and antigenicity
It has been shown previously that the receptor binding preference of an avian influenza H1N1 (DK/96) virus can be altered by only two mutations at residues E190D and G225D of the HA gene (Van Hoeven et al., 2009). Before we generated inactivated DK/96-wt and DK/96 HA mutant (DK/96-Hu) virus vaccines, we characterized the binding properties of the rescued viruses and determined whether altering receptor binding specificity affects viral fitness. Both parental and mutant viruses were assessed for their ability to agglutinate turkey RBCs resialylated with either α2-3- or α2-6-linked sialosides. As expected, DK/96-wt virus was found to agglutinate α2,3 sialylated RBCs only, whereas DK/96-Hu virus showed preferential agglutination of α2,6 sialylated RBCs (not shown). Mice were infected with 106 or 103 EID50 of DK/96-wt or DK/96-Hu virus and viral titers in lung tissues at the peak of virus infection (day 4 post-inoculation) were compared. As shown in Fig. 1A, both viruses replicate efficiently in mouse lung tissues with the DK/96-wt virus showing slightly higher titers; however the differences are not significant at either inoculation dose.
Fig. 1.
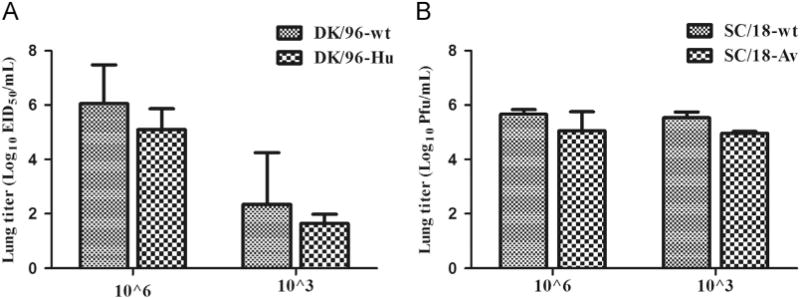
DK/96 and SC/18 virus replication in mouse lung tissues. Groups of 5 mice are intranasally (i.n.) inoculated with 106 EID50 or 103 EID50 of DK/96-wt or DK/96-Hu (HA-190D_225D) viruses (A) or with 106 PFU or 103 PFU of SC/18-wt or SC/18-Av (HA-190E-225G) viruses (B), and the viral titers in lung tissues at day 4 post-infection are titrated in eggs or MDCK cells and expressed as mean log10 EID50 or log10 PFU per ml+standard deviation (SD). There is no significance in viral titers between the wt groups and their respective isogenic control virus groups based on two-way analysis of variance (ANOVA, p > 0.05).
In a reciprocal experimental approach, the receptor binding preference of the human influenza H1N1 1918 (SC/18) virus was altered from human- to avian-like by two HA mutations at residues 190 and 225. It has been documented that these two point mutations in the HA gene are sufficient to change the receptor binding preference from α2,6- to α2,3-SA (Glaser et al., 2005). The HA and NA genes from SC/18-wt and α2,3 SA receptor binding mutant (SC/18-Av) virus, respectively, were rescued on the PR8 virus backbone. As expected, SC/18-wt was found to agglutinate α2,6 sialylated RBCs whereas SC/18-Av recombinant virus showed preferential agglutination of α2,3 sialylated RBCs (not shown). We found that altering receptor binding specificity for SC/18/PR8 virus did not significantly change the ability of the virus to replicate in mouse lungs; mice showed comparable virus titers on day 4 post-inoculation following either 106 or 103 PFU of SC/18-wt or SC/18-Av virus inoculation (Fig. 1B).
Next, we evaluated whether changing the receptor binding specificity had any effect on viral antigenicity following virus infection. The convalescent sera from mice inoculated with 106 EID50 of DK/96-wt or DK/96-Hu virus were collected at 21 days post-inoculation. No convalescent SC/18 sera were available for follow-up serology due to the high virulence of the virus in mice. The HI assays were initially conducted with both turkey and horse erythrocytes. Turkey red blood cells (TRBCs) were used to detect the serum HI titers against DK/96-Hu because the mutant virus failed to agglutinate horse red blood cells (HRBCs). Conversely, we found that using HRBCs to detect serum HI titer against DK/96-wt virus (expressing α2,3 SA) gave approximately 2-fold higher titers than that using TRBCs (data not shown), and therefore, the HI titers against DK/96-wt virus using HRBCs are shown (Table 1). Both DK/96-wt and DK/96-Hu virus inoculations induced robust serum antibody responses in mice. In general, the HI titers in response to infection correlated well with neutralizing antibody levels, although neutralizing antibody responses were consistently higher. The HI titers against DK-96-Hu virus antigen were consistently 2-fold lower than the titers against DK/96-wt virus regardless of the viruses used for infection (geometric mean titer [GMT] of 52 versus 121, 67 versus 134). In the neutralization assay, antibody titers against mutant DK/96-Hu and DK/96-wt were within 2-fold of each other (Table 1). Overall, our results demonstrated that changing receptor binding specificity for the H1N1 viruses had no significant effect on viral antigenicity or viral replication in mice.
Table 1.
Geometric mean of HI and neutralizing (neut) antibody titers from mouse seraa
| Virus antigen | HI titerb
|
Neut. titerb
|
||
|---|---|---|---|---|
| Sera raised against
|
Sera raised against
|
|||
| DK/96-WT | DK/96-Hu | DK/96-WT | DK/96-Hu | |
| DK/96-wt | 121(80–160) | 134(80–160) | 320(160–640) | 452(320–640) |
| DK/96-Hu | 52(20–80) | 67(40–80) | 425(160–640) | 761(640–1280) |
Convalescent serum samples from individual mice (5 per group) are collected 21 days post-inoculation with 106 EID50 of the virus indicated.
Samples are tested for HI and neutralization antibody activity against either DK/96-wt or mutant DK/96-Hu virus. Geometric mean titers (with range in parentheses) are shown as the reciprocal of the highest dilution of serum that completely inhibits haemagglutination (HI) or that neutralizes 100 PFU of infectious virus (neut).
Immunogenicity and protective efficacy of an inactivated avian influenza vaccine with α2,6 SA (human-like) binding preference
We next evaluated the contribution of receptor binding specificity to the immunogenicity and effectiveness of an inactivated avian influenza H1N1 virus vaccine. Formaldehyde-inactivated whole-virus vaccines derived from Dk/96-wt and DK/96-Hu viruses were used to vaccinate groups of mice in one or two dose vaccination regimen. In the single dose study, ten mice per group were inoculated with vaccine doses ranging from 0.25 to 10 μg. We found that at higher vaccine doses (10, 5, and 2.5 μg), DK/96-Hu vaccinated groups showed approximately 2–4 fold higher HI titers (Fig. 2A) and about 4-fold higher neutralization titers (Fig. 2B) against both homologous and Dk/96-wt viruses compared to antibody responses induced by DK/96-wt vaccine. At lower doses (0.5 and 0.25 μg), both Dk/96-wt and DK/96-Hu vaccines elicited weaker antibody responses and the difference in titers between the two vaccine groups was less evident compared to higher vaccine doses (Fig. 2A and B). The vaccine experiment was repeated once with a set of independently prepared DK/96 virus vaccines. At the same vaccine doses, we were able to confirm that the HI and neutralization titers were approximately 2–4 fold higher among those mice that received the DK/96-Hu vaccine (α2,6 SA binding preference) compared to Dk/96-wt (2,3 SA binding preference) vaccinated mice (data not shown).
Fig. 2.
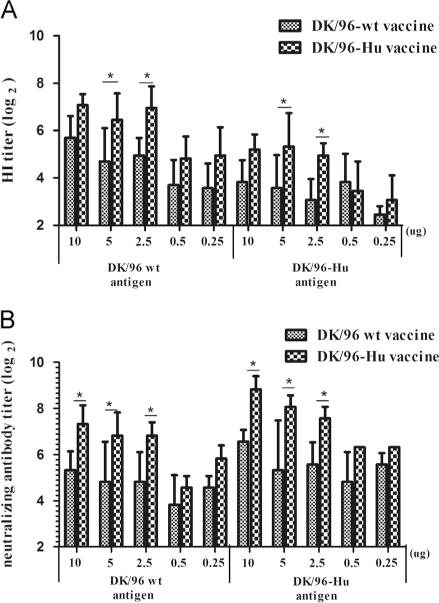
Cross-reactive antibody titers upon primary vaccination with DK/96 vaccine. Groups of 10 mice are vaccinated intramuscularly (i.m.) with 100 μl of PBS-diluted inactivated whole virus ranging from 0.25 μg to 10 μg (total protein) per mouse. The cross-reactive HI (A) and neutralizing antibody (B) titers of the vaccinated mouse sera at 28 days post-primary vaccination are tested against DK/96-wt and DK/96-Hu viruses. The graph represents the geometric mean value of the HI titers shown as log2 scale+SD. Statistical significance was determined by two-way ANOVA and Bonferroni post-test. An asterisk indicates that the antibody titers between DK/96-wt and DK/96-Hu vaccine groups at indicated dosage are significantly different with p<0.05.
We next compared the antibody titers after boost for the groups vaccinated with high doses of inactivated viruses. As shown in Table 2, both vaccine groups exhibited a significant increase in the HI titers following boost compared with primary vaccination, but the difference in antibody titers previously observed between two groups after single dose vaccination was diminished. Mouse sera obtained 30 days after vaccine boost, showed HI titers that ranged from 256 to 512 (GMT 274 to 320) for vaccine groups inoculated with doses of 10, 5, and 2.5 μg (Table 2). However, the differences in the HI and neutralization titers between the two vaccine groups were less evident compared to that observed in single-dose vaccine studies (Table 2 versus Fig. 2). One additional time-point of serum collection was taken at 200 days post-boost in attempt to show differences in antibody responses between DK/96-wt and DK/96-Hu vaccine groups. The antibody responses from the two virus groups dropped to similar levels over the extended period and there were no significant difference in HI titers (not shown). Our results suggest that the avian H1N1 virus vaccine with human receptor (α2,6 SA) binding preference had a modest advantage compared to the DK/96-wt vaccine in inducing antibody titers following primary vaccination; however, the response was less pronounced following prime-boost vaccination.
Table 2.
Geometric mean of hemagglutination-inhibition (HI) and neutralizing (neut) antibody titers of mice vaccinated with two-doses of DK/96-wt or DK/96-Hu inactivated virus vaccine.
| Virus antigen | Vaccine dose (μg) | HI titers of mouse sera againsta
|
|||
|---|---|---|---|---|---|
| DK/96-wt | DK/96-wtb
|
DK/96-Hub
|
|||
| HI titer | Neut. titer | HI titer | Neut. titer | ||
| 10 | 320 | 253 | 289 | 296 | |
| 5 | 293 | 172 | 320 | 242 | |
| 2.5 | 274 | nd | 320 | 320 nd | |
Mice receive a two-dose regimen of the indicated vaccine 4 weeks apart. Serum samples from individual mice (10 per group) are collected 30 days post-boost. Nd=not done.
Samples are tested for HI and neutralization antibody activity against DK/96-wt virus. Geometric mean titers are shown as the reciprocal of the highest dilution of serum that completely inhibits hemagglutination (HI) or that neutralizes 100 PFU of infectious virus (neut). There is no significance in titers between DK/96-wt and DK/96-Hu groups by two-way ANOVA and Bonferroni post-test.
Since the differences in antibody responses between DK/96-wt and DK/96-Hu vaccine groups were greatest after a single vaccination, the mice that received 5.0, 0.5 or 0.25 μg of vaccine were challenged with 106 EID50 of DK/96-wt virus at 32 days post-primary vaccination and lung titers were determined at day 4 p.c. As shown in Fig. 3, DK/96-wt virus replicates to approximately 107 EID50 in the lungs of control (PBS) mice. In general, vaccination with either DK/96-wt or DK/96-Hu virus provided some level of protection against viral replication in the lung at all vaccine doses tested. At vaccine doses of 5.0 and 0.5 μg, titers of infectious virus among DK/96-Hu immunized mice were reduced approximately 10-fold compared to DK/96-wt vaccine group; however, this did not reach statistical significance (p=0.08–0.1). At the lower vaccine dose (0.25 μg) the viral lung titers between vaccine groups were comparable, which was consistent with the negligible difference in antibody titers between DK/96-wt and DK/96-Hu vaccine groups at the same vaccine dose. Taken together, these results demonstrated that the inactivated avian H1 vaccine showing specific binding for α2,6 SA induced approximately 2–4 fold higher antibody response, which correlated with modestly improved protection against viral challenge.
Fig. 3.
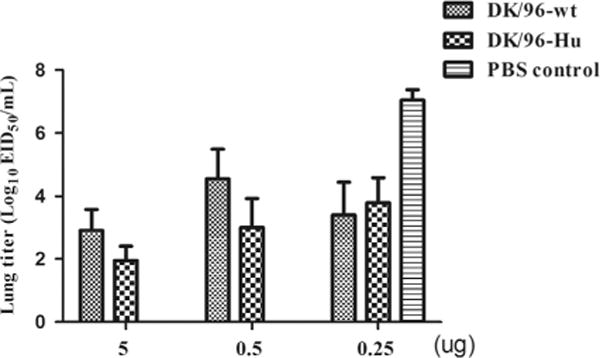
The protective efficacy of the vaccination with DK/96 virus upon challenge. Groups of 5 mice vaccinated with 5, 0.5 or 0.25 μg of DK/96-wt or DK/96-Hu virus vaccines are challenged with 106 EID50 of DK/96-wt virus at 30 days post-primary vaccination. Lungs were collected at day 4 post-challenge and titrated in eggs, expressed as mean log10 EID50 per ml+SD. There is no significance in viral titers between DK/96-wt and DK/96-Hu vaccine groups based on two-way ANOVA (p40.05).
Immunogenicity and protective efficacy of SC/18 virus with α2,3 SA (avian) binding preference
In a reciprocal experimental approach, inactivated virus vaccines were made from a recombinant virus containing the wt HA and NA genes from SC/18 virus (SC/18-wt) or its avian receptor mutant (SC/18-Av) virus. Mice (10 per group) were immunized once with 10, 2.5 or 0.25 μg of vaccine. The antibody responses were detected at 28 days post-vaccination by the HI assay. As shown in Fig. 4A, antibody titers induced by SC/18-wt are slightly higher than those induced by the SC/18 avian receptor mutant virus at dose levels of 10 and 2.5 μg, but the differences are generally less than two-fold and not statistically significant. At the low (0.25 μg) dose, both vaccines induced poor antibody responses and there were no differences in HI antibody titers. In both vaccine groups, antibody titers were boosted after a second immunization, however the titer differences between the two vaccines were negligible (data not shown).
Fig. 4.
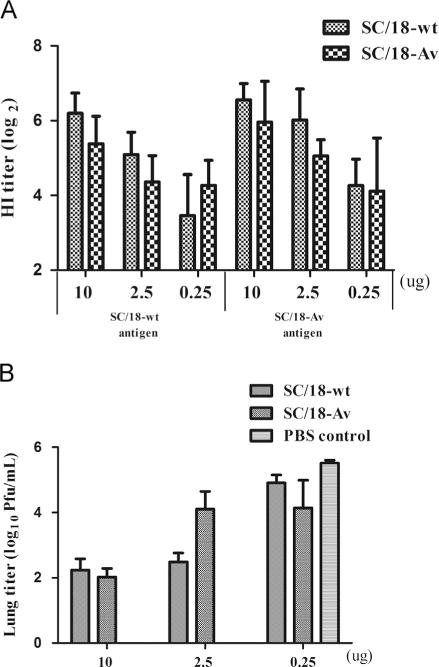
Cross-reactive antibody titers and the protective efficacy upon primary vaccination with SC/18 vaccine. (A) Groups of 10 mice are vaccinated with 100 μl of PBS-diluted inactivated whole virus vaccines at doses of 10 μg, 2.5 μg or 0.25 μg per mouse. The cross-reactive HI titers of the vaccinated mouse sera at 28 days post-primary vaccination are tested against SC/18-wt and SC/18-Av viruses. The graph represents the geometric mean value of HI antibody titers shown as log2 scale+standard deviation (SD). The HI titers between SC/18-wt and SC/18-Av at any vaccination dose are not statistically different as analyzed by two-way ANOVA and Bonferroni post-test (B). At 30 days post-primary vaccination, groups of 5 mice are challenged with 106 PFU of SC/18-wt virus and the lung titers at day 4 post-challenge are shown as the mean log10 PFU per ml+SD. There is no significance in lung titers between SC/18-wt and SC/18-Av vaccinated groups based on two-way ANOVA (p>0.05).
To compare the protective efficacy following SC/18-wt or avian receptor mutant (SC/18-Av) virus vaccination, immune and PBS-control mice were challenged with 106 PFU of SC/18-wt virus after primary vaccination. The mice from the PBS control group showed ruffled fur and weight loss by day 4 p.c. and virus in lung tissues reached mean peak titers of 105.8 PFU/ml (Fig. 4B). Vaccination with doses of 10 μg and 2.5 μg resulted in reduced viral titers compared to those of the PBS group; however, the difference in viral lung titers between SC/18-wt and SC/18-Av vaccine groups was not statistically significant. At vaccine dose of 0.25 μg, both vaccines failed to significantly reduce viral replication compared to that of the PBS control group. Overall, our results suggest that changing receptor binding specificity of SC/18 virus from human-to avian-like has minimal effect on viral immunogenicity of inactivated vaccines in mice.
The cellular immune responses of wild-type and mutant virus vaccinated mice
Next we compared the frequency of vaccine-induced antibody-secreting (ASC) B cells and cytokine secreting T cell responses among mice administered with one dose of 10 or 2.5 μg of Dk/96-wt and Dk/96-Hu vaccines. We used the ELISPOT assay, which has proven to be a sensitive tool for detecting cellular immunity following influenza vaccination (Lindemann et al., 2006) to measure the frequency of antigen-specific IgG secreting B cells from spleen tissues. As shown in Fig. 5A, the frequency of virus-specific IgG ASCs in spleen tissues significantly increases in mice immunized with 10 μg DK/96-Hu vaccine as compared to that of DK/96-wt vaccine. DK/96-Hu vaccination also increased the frequency of ASCs even at the lower vaccine dose of 2.5 μg. For the 1918/PR8 virus vaccine, 2.5 μg of SC/18-wt virus vaccine induced approximately 4-fold higher frequency of ASCs in comparison to the same dose of SC/18-Av vaccine (Fig. 5A; right panel). At the lower vaccine dose of 0.25 μg, both vaccines induced a relatively low frequency of ASCs and there was no difference between the two vaccine groups.
Fig. 5.
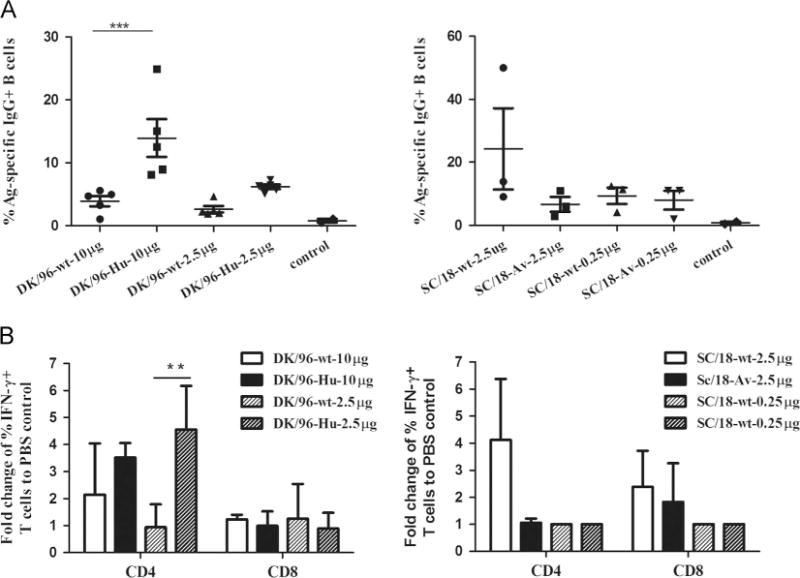
The cell-mediated immune response upon vaccination with 1918 virus. (A) Groups of 3–5 mice are vaccinated i.m. with DK/96-wt and DK/96-Hu (10 or 2.5 μg) or SC/18-wt and SC/18-Av (2.5 or 0.25 μg) vaccines. Fourteen days later, spleen tissues are harvested and the frequency of virus-specific IgG+ASCs are measured by ELISPOT assay. The number of virus-specific IgG+ASCs is normalized against the number of total IgG+secreting ASCs and presented as % Ag-specific IgG+B cells. (B) Mice are vaccinated with DK/96-wt and DK/96-Hu (10 or 2.5 μg) or SC/18-wt and SC/18-Av (2.5 or 0.25 μg). Fourteen days post-immunization, spleen are harvested and the frequency of IFN-γ-producing CD4+ and IFN-γ-producing CD8+ T cells from immunized mice is measured by intracellular cytokine staining following 5 days in vitro culture after infection for 1 h with DK/96 or SC/18 virus. Statistical significance is determined by two-way ANOVA. ** indicates statistical significance (p<0.01) between Dk/96-Hu and Dk/96-wt vaccine, *** p<0.001.
We next compared the frequency of virus-specific cytokine secreting CD4+ or CD8+ T cells upon antigen re-stimulation in vitro. As shown in Fig. 5B (left panel), mice immunized with 2.5 μg of DK/96-Hu vaccine show a higher frequency of IFN-γ secreting CD4 as compared to that of the DK/96-wt vaccine group. Similarly, the SC/18-wt vaccine (with human-like α2,6 SA) induced a higher frequency of IFN-γ secreting CD4+ cells, but not CD8+ cells, as compared to that of SC/18-Av mutant vaccine (Fig. 5B; right panel). However this difference was not observed at the other two vaccine doses. In addition, both vaccines induced a very low level of IFN-γ production by CD8+ T cells and no significant increased frequency of CD8+IFN-γ+ cells was observed among the groups (Fig. 5A and B). In summary, our data demonstrated that H1N1 influenza vaccines with human receptor binding preference (α2,6 receptor binding affinity) induced a somewhat higher frequency of ASC B cells and IFN-γ cytokine secreting CD4+, but not CD8+ T cells, as compared to their counterpart vaccines with avian receptor binding preference.
Immunogenicity and protective efficacy of DK/96-wt and DK/96-Hu virus vaccines in ferrets
Ferrets are considered to be the most suitable animal model for influenza vaccine efficacy studies (Belser et al., 2011). To further explore whether the viral receptor binding preference for α2,3 SA contributes to the relatively poor immunogenicity of avian influenza virus vaccines in humans, we compared the antibody responses of DK/96-wt and DK/96-Hu in ferrets. Groups of 4–6 adult ferrets were vaccinated with 90 μg or 30 μg of inactivated DK/96-wt or DK/96-Hu vaccine and the antibody responses were measured after 21 days. As shown in Fig. 6A, 3 of 6 ferrets that received 90 μg of DK/96-Hu mutant vaccine reached an HI titer of 40 or greater against both virus antigens (left and right panels). In contrast, HI responses among DK/96-wt (90 μg) vaccinated ferrets were significantly lower. HI titers among DK/96-wt vaccinated ferrets (against DK/96-wt virus antigen) were approximately 3-fold lower than that from the DK/96-Hu vaccine group (GMT=7 versus 25 at the 90 μg dose and GMT=5 versus 14 for 30 μg dose) (Fig. 6A; left panel). As observed above, in the HI assay, antibody titers measured against DK-96-Hu virus antigen were consistently lower than the HI titers against DK/96-wt antigen; only ferrets that received 90 μg of DK/96-Hu mutant vaccine induced a detectable HI response (Fig. 6A; right panel). Neutralizing antibody responses followed a similar pattern; neutralizing titers from DK/96-wt vaccinated animals were 2–3-fold lower (against both DK/96-wt and DK/96-Hu antigens) compared to antibody titers induced by DK/96-Hu vaccine at both doses (Fig. 6B; left and right panels).
Fig. 6.
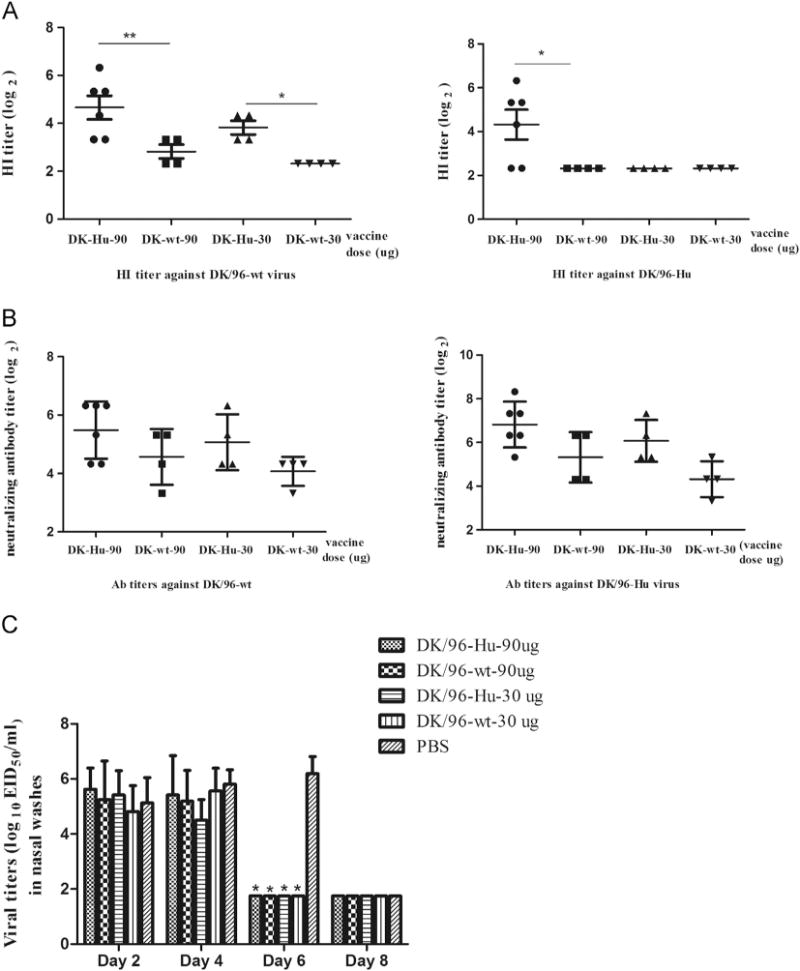
Vaccination of DK/96 vaccines in ferrets. Ferrets (4–6 per group) are vaccinated with 30 or 90 μg of inactivated whole DK/96-wt or DK/96-Hu virus vaccines or PBS mock control. Serum samples are collected at 21 days post-vaccination to determine anti-DK/96-wt or anti-DK/96-Hu specific HI (A) or neutralizing antibody titers (B). Individual symbols represent each experimental ferret, and horizontal lines represent the geometric means (GMT). The limit of detection for both HI and neutralizing tests is (or 10). If the titer is below detecting limit, it is assigned as (or 5). Statistical significances are determined by two-way ANOVA and Bonferroni post-test, and double asterisks indicate the significant difference in antibody titers with p<0.01 and a single asterisk indicates the significant difference in antibody titers with p<0.05. At 21 days post-vaccination, ferrets are challenged with 106 EID50 of DK/96-wt virus and nasal wash samples are collected at days 2, 4, 6 and 8 post-challenge. Mean viral titers of each group are shown as log10 EID50/ml+SD (C). Statistical significances are determined by two-way ANOVA and Bonferroni post-test. An asterisk indicates a statistically significant (p<0.05) reduction in virus titers compared to PBS mock group.
Next, we evaluated the vaccine protective efficacy following DK/96-wt virus challenge. Because viral challenge with 106 EID50 of DK/96-wt virus caused only mild, transient weight loss (3% mean maximum weight loss in PBS control group), viral titers in ferret nasal washes were the primary measurement of vaccine protection. On days 2 and 4 p.c., DK/96-wt and DK/96-Hu vaccine groups showed comparable viral titers in nasal washes, which were not significantly different from PBS mock controls (Fig. 6C). At day 6 p.c., all nasal washes from vaccinated groups were negative for infectious virus, whereas the PBS control group still shed high titers of virus. Taken together, these data suggest that avian H1N1 (DK/96) inactivated vaccine with human receptor binding specificity is able to induce slightly higher HI and neutralizing antibodies; however this does not correlate with increased protection in ferrets.
Discussion
Vaccines derived from avian influenza viruses have proved poorly immunogenic in mammals compared to seasonal influenza vaccines, which possess an “human-like” α2,6-SA binding preference (Atmar et al., 2006; Bresson et al., 2006; Couch et al., 2012; Keitel et al., 2008; Patel et al., 2012). Therefore, there is a need to develop improved avian influenza vaccines for optimal protection against human infection. In the past ten years, there have been many different approaches to increase the efficacy of avian influenza vaccines, including increasing HA content (Beigel et al., 2009; Treanor et al., 2006), incorporation of adjuvants (Bernstein et al., 2008) and modification of HA glycan composition (Wang et al., 2009). In our current study, we mutated the HA of two H1N1 viruses to determine whether α2,3-SA receptor binding specificity of avian influenza viruses contributes to the relatively poor immunogenicity of these vaccines. Our approach was to use viruses that were different only in the HA receptor binding site. We demonstrated in both mouse and ferret models that changing the receptor binding specificity from avian- to human-like of an avian H1N1 virus vaccine can increase antibody titers 2–4 fold and increase the expression of cytokine secreting CD4 T cells. Interestingly, in our reciprocal approach in which we altered the 1918 virus vaccine receptor binding specificity from human- to avian-like, we found that the difference in antibody titers induced by the two vaccines was less evident. Perhaps the intrinsic trait associated with each specific influenza virus might influence how the key residues in the receptor binding site contribute to viral immunogenicity. Although the enhanced immunogenicity resulting from changing receptor binding specificity was rather modest compared to the effects observed by adding adjuvants (Bernstein et al., 2008; Dong et al., 2012), it nevertheless might provide an additional approach to improve seroconversion rates among vaccinated subjects.
Influenza virus receptor binding specificity has been shown to be one of the main determinants in viral tropism and transmissibility (Pappas et al., 2010; Tumpey et al., 2007). It is generally believed that the respiratory tract tropism of human influenza viruses correlates with the abundance of α2,6-SA in upper respiratory tract of humans whereas avian influenza viruses prefer α2,3 linkages mostly located in the lower respiratory tract (Ito et al., 1998; Shinya et al., 2006). However, the concept that avian influenza viruses have a preference of viral infection for the lower respiratory tract of mammals is likely an oversimplification, and there may be a sufficient number of α2,3-linked SA receptors in the upper mammalian airway to support significant viral replication (Nicholls et al., 2007; Zeng et al., 2013). For example, avian H5N1 viruses with α2,3 receptor preference are capable of infecting human upper respiratory tract tissues and have been shown to replicate as efficiently as human influenza viruses in ferret tracheal epithelial (FTE) cells that predominantly express α2,6-SA (Zeng et al., 2013). Interestingly, in the aforementioned study, H5N1 virus replicated as efficiently as human influenza (H3N2 and H1N1) viruses in FTE cells despite its low initial infection rate and less abundant avian-like (α2,3-linked) receptors for H5N1 virus to initiate an infection. Moreover, although α2,3-SA had been shown to be dominant in mouse respiratory tracts (Ibricevic et al., 2006), we were able to demonstrate that changing receptor binding specificity for either DK/96 or SC/18H1N1 virus had no significant effect on viral titers in mouse lung tissues. Our finding is consistent with the recent study in which the authors reported that modulating receptor binding specificity for the 2009 pandemic virus from α2,6-SA binding to α2,3-SA binding did not enhance viral replication in mice (Lakdawala et al., 2013). Similar results have also been shown in ferrets, which share great similarities with humans in SA distribution in respiratory tracts (Jayaraman et al., 2012). Both studies with the SC/1918 virus and 2009 pandemic virus revealed that the viruses with either α2,3-SA or α2,6-SA binding preference showed no difference in viral replication in upper and lower respiratory tracts of ferrets (Lakdawala et al., 2013; Tumpey et al., 2007). However, there are other seemingly contradictory reports as well. Xu et al. showed that the recombinant mutant Solomon Island/3/06 (SI/06) virus (190A/226Q) with exclusive α2,6-SA binding specificity replicated in both upper and lower respiratory tracts, whereas the mutant virus (190D/226 R) with α2,3-SA binding preference only replicated in ferret nasal turbinate (Xu et al., 2010). Another study with H2 and H6 viruses also showed that the α2,6-SA binding viruses with either 226L/228G or 226Q/228S replicated significantly better in the upper respiratory tract of ferrets compared to the α2,3-SA binding virus with 226Q/228G amino acids (Chen et al., 2012). Taken together, it appears that the mutations that affect the receptor binding site for vaccine development do not affect viral fitness or result in an attenuated virus.
The data also demonstrated that changing receptor binding specificity of the DK/96 vaccine from avian- to human-like by substitution at residues 190 and 225 had no effect on viral antigenicity based on the cross-reactive HI responses. During the interpretation of HI results we consistently observed that the HI titers against DK-96-Hu virus antigen were approximately 2–4 fold lower than HI titers against DK/96-wt antigen regardless of the viruses used for immunization. This initially suggested to us that there were differences in antigenicity between the parental and mutant viruses. However, the neutralization antibody titers against DK/96-Hu virus were not lower but actually slightly higher (less than 2-fold) than the titers against DK/96-wt virus. Thus, a minor confounding issue with the HI assay in these studies is that turkey RBCs used to detect the HI titers against DK/96-Hu antigen are less sensitive than the horse RBCs used to detect DK/96-wt antigen. We speculated that the differences in cross-reactive antibody HI titers were mostly due to the changes in the sensitivity of the assays rather than the changes in viral antigenicity. Previous studies of live virus infection of ferrets demonstrated that changing receptor binding specificity through the specific residues (190/226 for H1 virus or 226/228 for H2 and H6 viruses) caused a change in viral antigenicity and an approximately 10-fold difference in antibody titers against homologous viruses in ferrets (Chen et al., 2012; Xu et al., 2010). Therefore, depending on virus subtypes, vaccine formats, and the specific residues targeted, the effect of changing receptor binding preference on viral antigenicity and immunogenicity may vary.
In our study, we observed that H1 subtype vaccines with human receptor binding preference induced slightly higher levels of humoral and cell-mediated responses. There are still many unknowns concerning the interaction of influenza HA and their receptors. In particular, the interaction of HA with sialic acid receptors of antigen presenting cells (e.g. dendritic cells [DCs], and macrophages) leading to activation of the immune response is not well understood. Although SA has long been identified as the primary receptor for influenza virus entry into host epithelium, where influenza viruses primarily replicate (Skehel and Wiley, 2000), there is growing evidence suggesting that several specific cell receptors are involved in virus entry into certain cell types, especially immune cells. DC-specific intercellular adhesion molecule-3-grabbing non-integrin (DC-SIGN) (Londrigan et al., 2011; Wang et al., 2008) along with other calcium-dependent (C-type) lectin receptors, including macrophage mannose receptor (MMR) (Reading et al., 2000), SIGNR (L-SIGN) (Londrigan et al., 2011) and macrophage galactose-specific -type lectin (MGL) (Upham et al., 2010) has been shown to be able to mediate viral entry in either SA-dependent or SA-independent manner depending on the cell types and the viruses used in the studies. The C-type lectin receptor-mediated interaction between immune cells and influenza glycoproteins has been shown to be important not only in cell tropism and pathogenesis, but also in inducing host immune responses. This has been demonstrated both in vitro with SIGN-R1-specific antibody and in vivo using multiphoton intra-vital imaging of DCs which showed that the uptake of inactivated PR8 virus via SIGN-R promoted humoral immunity (Gonzalez et al., 2010). In addition to C-type lectins, other unidentified receptors may also be involved in virus binding to immune cells as suggested from the recent work of Ramos et al. in which authors used two isogenic recombinant A/Vietnam/2004 (H5N1) viruses to study the effects of receptor binding specificity on the innate immune response. They found that the virus (226Q/228G) with avian-type receptor binding specificity induced higher levels of proinflammatory cytokines in comparison to the virus (226L/228S) with human receptor binding specificity (Ramos et al., 2011). The authors propose that the receptors on APCs that recognize α2,3-SA may be different from those that recognize α2,6-SA-binding viruses leading to distinct immune responses.
Although our results failed to demonstrate that receptor binding specificity contributes substantially to the immunogenicity of avian influenza vaccines, the research suggests that additional studies are needed to determine whether modifying the HA of current WHO avian influenza candidate vaccine viruses (www.who.int/en/) could improve the immunogenicity. It would be of interest to investigate whether the substitutions identified in transmissible H5N1 virus studies (Chen et al., 2012; Herfst et al., 2012; Imai et al., 2012) can lead to an improvement in vaccine immunogenicity. Furthermore, it would be interesting to evaluate whether α2,6 SA receptor binding mutant vaccines can be further improved by either additional modification of the glycan composition of the HA and/or addition of adjuvants.
Materials and methods
Inactivated virus vaccines
A set of eight reverse genetics plasmids cloned into the expression vector pDZ was used for rescuing the avian A/Duck/New York/15024–21/96 (Dk/96) H1N1 virus as described previously (Van Hoeven et al., 2009). The rescue plasmids encoding individual segments of A/Puerto Rico/8/1934 (PR8) virus were kindly provided by Adolfo García-Sastre (Mount Sinai School of Medicine, New York). The HA and NA genes of A/South Carolina/1/1918 (SC/18) H1N1 virus were amplified and cloned into a reverse genetics vector pPOL as previously reported (Tumpey et al., 2007). The Agilent QuikChange site-directed mutagenesis kit (Santa Clara, CA) was used to introduce mutations into pDZ-Dk/96-HA or pPOL-SC/18-HA at residues 190 and 225. The recombinant wild-type (wt) Dk/96 and mutant DK/96 virus with HA amino acid substitutions at 190D and 225D bound preferentially to the human-like (α2,6 SA) receptor (hereafter referred to as Dk/96-Hu) were previously described (Van Hoeven et al., 2009). A recombinant virus containing the wt HA and NA genes from SC/18 virus (PR8:1918-HA/NA; 6:2) (SC/18-wt) along with a α2,3 SA receptor binding mutant virus with HA mutations at positions 190E and 225G (PR8:1918-HA-Av/NA; 6:2) (SC/18-Av) was rescued on the PR8 virus backbone (Tumpey et al., 2007). The recombinant viruses were propagated in the allantoic cavities of 10-day-old embryonating chicken eggs at 35 °C for 48 h. The allantoic fluids were pooled, clarified by centrifugation and the HA and NA genes of each recombinant virus were confirmed by sequencing to ensure no undesired mutations.
Viruses used as vaccines were concentrated from allantoic fluid and purified by equilibrium density centrifugation through a 30–60% linear sucrose gradient as previously described (Shaw et al., 2008). The concentrations of purified virus vaccines were determined by a Bio-Rad protein assay kit (Bio-Rad Laboratories, Hercules, CA) and then diluted to 1 μg/ml before inactivation with 0.025% formalin at 4 °C for at least 48 h. Virus inactivation was confirmed by two passages in embryonated eggs. Proteins of the purified viruses were separated by 4–15% Mini-PROTEAN Tris/Glycine precast gel (Bio-Rad) and stained with Coomassie blue. The images were captured by Kodak Image Station 4000R Pro and analyzed by Kodak Molecular Imaging Software. The ratio of the HA proteins (HA0) to the total proteins (HA0, NP, M) was determined according to the method described previously (Harvey et al., 2008).
Hemagglutination assay
Hemagglutination assays using resialyated turkey red blood cells were performed as previously described (Glaser et al., 2005). Briefly, turkey red blood cells were enzymatically desialyated using Vibrio cholerae Sialidase (Roche-Applied Science, Indianapolis, IN) followed by resialylation using either α2-6-(N)-sialyltrans-ferase or α2-3-(N)-sialyltransferase (Sigma-Aldrich, St. Louis, MO). Hemagglutination assays were performed by using 8 hemaggluti-nation units (HAU) of virus.
Immunization and challenge of mice and ferrets
All animal experiments were performed under the guidance of the Centers for Disease Control and Prevention's Institutional Animal Care and Use Committee and were conducted in an Association for Assessment and Accreditation of Laboratory Animal Care International-accredited animal facility. Groups of 10 female BALB/c mice (Charles River Laboratories, Wilmington, MA), 6–8 weeks old, were vaccinated intramuscularly (i.m.) with 100 μl of PBS-diluted inactivated whole virus vaccine following anesthesia with 0.2 μl of 2,2,2-tribromoethanal in tert-amly alcohol (Avertin; Aldrich Chemical Co., Milwaukee, WI). The dose of each vaccine was determined by measurement of total protein content (described above) and adjusted based on the percentage of HA to total protein amount to ensure that wt and receptor mutant vaccines contained the same amount of the HA protein. The ratio of HA to total protein for two independently prepared vaccines (wt and receptor mutant viruses) varied over a narrow range of 30–40%. Vaccines were administered as one- or two-dose regimen given 4 weeks apart between primary and boost vaccination. Blood was collected using the cheek-pouch method and serum was isolated from individual mice at the indicated days post-vaccination. Vaccinated mice were challenged intranasally (i.n.) with 106 EID50 of Dk/96-wt or 106 PFU of SC/18-wt virus (50 μl) diluted in PBS. Homogenates from whole lungs, collected on day 4 post-challenge (p.c.), were prepared in 1 μl of PBS and viral titers were determined by a standard plaque assay in Madin-Darby canine kidney (MDCK) cells or in embryonating eggs to determine 50% egg-infectious dose (EID50) titers using a statistical method (Reed, 1938).
For ferret vaccinations, groups of 4–6 adult male Fitch ferrets, 5–8 months of age (Triple F farms, Sayre, PA), serologically negative by hemagglutination-inhibition (HI) assay for currently circulating influenza viruses, were used in this study. Ferrets were given 30 or 90 μg of inactivated whole-virus vaccine i.m. diluted in 1 μl of sterile PBS. Serum samples were collected at three weeks post-vaccination for serologic assays. The vaccinated ferrets were challenged i.n. with 1 μl of 106 EID50 of DK/96-wt virus diluted in PBS following anesthesia with a ketamine–xylazine–atropine cocktail given i.m. Nasal wash samples were collected on indicated days and titrated in embryonated eggs.
Serologic assays
Mouse and ferret sera were treated with receptor destroying enzyme (RDE) from Vibrio cholerae (Denka Seiken, Tokyo) overnight followed by heat treatment (56 °C, 30 min) and prediluted 1:10 before use in the HI assay or neutralization assay. HI assay was performed by standard methods using 0.5% turkey red blood cells for influenza viruses with human receptor binding specificity (SC/18-wt and DK/96-Hu) or with 1% of horse red blood cells for the H1N1 viruses with avian receptor binding specificity (SC/18-Av and DK/96-wt). HI titer was determined by reciprocal of the highest dilution of serum that completely inhibited haemagglutination. Neutralizing antibody titers were determined according to previously established methods (Mozdzanowska et al., 1997) and the titers were shown as the reciprocal of the highest dilution of serum that neutralized 100 plaque forming units (PFU) of virus in MDCK cell cultures.
Virus specific antibody-secreting cell (ASC) enzyme-linked immunosorbent spot (ELISPOT) assay
The frequency of virus-specific ASC cell ELISPOT assays was performed according to established methods (Jeisy-Scott et al., 2012). Briefly, PVDF multiscreen 96-well plates (Millipore, Billerica, MA) were coated with 5 μg/ml anti-mouse IgG antibody (Southern Biotech, Birmingham, AB) for measuring total IgG secreting B cells. In separate plates, inactivated WT or receptor mutants of DK/96 or SC/18 virus were adjusted to 100 HAU and incubated overnight at 4 °C. The plates were washed thrice with PBS and then blocked for 1 h at 37 °C with 200 μl/well of RPMI-1640 supplemented with 10% FBS, penicillin/streptomycin, L-glutamine, and 0.01 M HEPES buffer (cRPMI). Groups of five vaccinated mice were euthanized at 14 days post-primary vaccination and single cell suspensions of splenocytes were prepared after red blood cell lysis. Suspensions were adjusted to 10 106– 15 × 106 cells/ml and added onto homologous virus-coated plates and incubated overnight in a 37 °C, 5% CO2 incubator. The plates were washed 4 times with 0.5% Tween 20 in PBS (PBST) and incubated with biotinylated anti-mouse IgG antibodies (Southern Biotech) for 1 h at room temperature. Plates were washed 4 times with PBST, and incubated with alkaline phosphatase-conjugated streptavidin (Vector, Burlingame, CA) in PBST for 1 h at room temperature. Plates were washed 4 times and spot development was achieved by adding 100 μl of Vector Blue alkaline phosphatase substrate kit III (Vector, Burlingame, CA) to each well. Spot forming units were counted using ImmunoSpots (Cellular Technology Ltd., Cleveland, OH) and expressed as % Ag-specific IgG+B cells out of total IgG -secreting B cells.
Cytokine secreting CD4, CD8 T cells
Suspensions of 1 × 106 splenocytes were seeded in 100 μl RPMI medium in 96-well round bottom plates and infected by wt or receptor mutants of DK/96 or SC/18 virus at a multiplicity of infection (MOI) of 0.1, as described (Jeisy-Scott et al., 2012). After 1 h incubation with the virus, 50 μl RPMI containing 40% FBS and 400 U/ml Penicillin and 400 μg/ml streptomycin solution was added. Four days post-infection, the cells were collected and re-stimulated with plate-bound anti-CD3 (10 μg/ml; clone 145-2C11; eBioscience, San Diego, CA), and anti-CD28 (2 μg/ml, clone 37.51; eBioscience) for 6 h in the presence of BD GolgiStop™ and GolgiPlug™ protein transport inhibitors (BD Bioscience, San Jose, CA) to enhance intracellular cytokine staining. Cells were surface stained with PE-Cy™7-conjugated anti-CD4 (clone GK1.5; eBioscience) and Alexa Fluor 700-conjugated anti-CD8 (53-6.7; BD Bioscience) for 20 min at 4 °C. Cells were then made permeable with Cytofix/Cytoperm (BD Bioscience) followed by intracellular staining with PerCP-Cy5.5-conjugated anti-IFN-γ (BioLegend, San Diego, CA) for 45 min at 4 °C. Cells were washed twice with perm/wash and re-suspended in PBS/10% FBS. Samples were analyzed using an LSR II flow cytometer (BD Biosciences, Sam Jose, CA), and the cytometry data were analyzed using FlowJo software (TreeStar, Ashland, OR).
Acknowledgments
The authors thank Amelia Hofstetter for excellent technical assistance. The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention or the Agency for Toxic Substances and Disease Registry.
References
- Atmar RL, Keitel WA, Patel SM, Katz JM, She D, El Sahly H, Pompey J, Cate TR, Couch RB. Safety and immunogenicity of nonadjuvanted and MF59-adjuvanted influenza A/H9N2 vaccine preparations. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2006;43:1135–1142. doi: 10.1086/508174. [DOI] [PubMed] [Google Scholar]
- Beigel JH, Farrar J, Han AM, Hayden FG, Hyer R, de Jong MD, Lochindarat S, Nguyen TK, Nguyen TH, Tran TH, Nicoll A, Touch S, Yuen KY, Writing Committee of the World Health Organization Consultation on Human Influenza, A/H5 Avian influenza A (H5N1) infection in humans. N Engl J Med. 2005;353:1374–1385. doi: 10.1056/NEJMra052211. [DOI] [PubMed] [Google Scholar]
- Beigel JH, Voell J, Huang CY, Burbelo PD, Lane HC. Safety and immunogenicity of multiple and higher doses of an inactivated influenza A/H5N1 vaccine. J Infect Dis. 2009;200:501–509. doi: 10.1086/599992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belser JA, Katz JM, Tumpey TM. The ferret as a model organism to study influenza A virus infection. Dis Models Mech. 2011;4:575–579. doi: 10.1242/dmm.007823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernstein DI, Edwards KM, Dekker CL, Belshe R, Talbot HK, Graham IL, Noah DL, He F, Hill H. Effects of adjuvants on the safety and immunogenicity of an avian influenza H5N1 vaccine in adults. J Infect Dis. 2008;197:667–675. doi: 10.1086/527489. [DOI] [PubMed] [Google Scholar]
- Bresson JL, Perronne C, Launay O, Gerdil C, Saville M, Wood J, Hoschler K, Zambon MC. Safety and immunogenicity of an inactivated split-virion influenza A/Vietnam/1194/2004 (H5N1) vaccine: phase I randomised trial. Lancet. 2006;367:1657–1664. doi: 10.1016/S0140-6736(06)68656-X. [DOI] [PubMed] [Google Scholar]
- Butt KM, Smith GJ, Chen H, Zhang LJ, Leung YH, Xu KM, Lim W, Webster RG, Yuen KY, Peiris JS, Guan Y. Human infection with an avian H9N2 influenza A virus in Hong Kong in 2003. J Clin Microbiol. 2005;43:5760–5767. doi: 10.1128/JCM.43.11.5760-5767.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen Z, Zhou H, Kim L, Jin H. The receptor binding specificity of the live attenuated influenza H2 and H6 vaccine viruses contributes to vaccine immunogenicity and protection in ferrets. J Virol. 2012;86:2780–2786. doi: 10.1128/JVI.06219-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connor RJ, Kawaoka Y, Webster RG, Paulson JC. Receptor specificity in human, avian, and equine H2 and H3 influenza virus isolates. Virology. 1994;205:17–23. doi: 10.1006/viro.1994.1615. [DOI] [PubMed] [Google Scholar]
- Couch RB, Patel SM, Wade-Bowers CL, Nino D. A randomized clinical trial of an inactivated avian influenza A (H7N7) vaccine. PloS One. 2012;7:e49704. doi: 10.1371/journal.pone.0049704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong L, Liu F, Fairman J, Hong DK, Lewis DB, Monath T, Warner JF, Belser JA, Patel J, Hancock K, Katz JM, Lu X. Cationic liposome-DNA complexes (CLDC) adjuvant enhances the immunogenicity and cross-protective efficacy of a pre-pandemic influenza A H5N1 vaccine in mice. Vaccine. 2012;30:254–264. doi: 10.1016/j.vaccine.2011.10.103. [DOI] [PubMed] [Google Scholar]
- Gao R, Cao B, Hu Y, Feng Z, Wang D, Hu W, Chen J, Jie Z, Qiu H, Xu K, Xu X, Lu H, Zhu W, Gao Z, Xiang N, Shen Y, He Z, Gu Y, Zhang Z, Yang Y, Zhao JS, Zhou L, Li X, Zou S, Zhang Y, Li X, Yang L, Guo J, Dong J, Li Q, Dong L, Zhu Y, Bai T, Wang S, Hao P, Yang W, Zhang Y, Han J, Yu H, Li D, Gao GF, Wu G, Wang Y, Yuan Z, Shu Y. Human infection with a novel avian-origin influenza A (H7N9) virus. N Engl J Med. 2013;368:1888–1897. doi: 10.1056/NEJMoa1304459. [DOI] [PubMed] [Google Scholar]
- Glaser L, Stevens J, Zamarin D, Wilson IA, Garcia-Sastre A, Tumpey TM, Basler CF, Taubenberger JK, Palese P. A single amino acid substitution in 1918 influenza virus hemagglutinin changes receptor binding specificity. J Virol. 2005;79:11533–11536. doi: 10.1128/JVI.79.17.11533-11536.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez SF, Lukacs-Kornek V, Kuligowski MP, Pitcher LA, Degn SE, Kim YA, Cloninger MJ, Martinez-Pomares L, Gordon S, Turley SJ, Carroll MC. Capture of influenza by medullary dendritic cells via SIGN-R1 is essential for humoral immunity in draining lymph nodes. Nat Immunol. 2010;11:427–434. doi: 10.1038/ni.1856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Han T, Marasco WA. Structural basis of influenza virus neutralization. Ann N Y Acad Sci. 2011;1217:178–190. doi: 10.1111/j.1749-6632.2010.05829.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey R, Wheeler JX, Wallis CL, Robertson JS, Engelhardt OG. Quantitation of haemagglutinin in H5N1 influenza viruses reveals low hae-magglutinin content of vaccine virus NIBRG-14 (H5N1) Vaccine. 2008;26:6550–6554. doi: 10.1016/j.vaccine.2008.09.050. [DOI] [PubMed] [Google Scholar]
- Herfst S, Schrauwen EJ, Linster M, Chutinimitkul S, de Wit E, Munster VJ, Sorrell EM, Bestebroer TM, Burke DF, Smith DJ, Rimmelzwaan GF, Osterhaus AD, Fouchier RA. Airborne transmission of influenza A/H5N1 virus between ferrets. Science. 2012;336:1534–1541. doi: 10.1126/science.1213362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ibricevic A, Pekosz A, Walter MJ, Newby C, Battaile JT, Brown EG, Holtzman MJ, Brody SL. Influenza virus receptor specificity and cell tropism in mouse and human airway epithelial cells. J Virol. 2006;80:7469–7480. doi: 10.1128/JVI.02677-05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imai M, Watanabe T, Hatta M, Das SC, Ozawa M, Shinya K, Zhong G, Hanson A, Katsura H, Watanabe S, Li C, Kawakami E, Yamada S, Kiso M, Suzuki Y, Maher EA, Neumann G, Kawaoka Y. Experimental adaptation of an influenza H5 HA confers respiratory droplet transmission to a reassortant H5 HA/H1N1 virus in ferrets. Nature. 2012;486:420–428. doi: 10.1038/nature10831. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ito T, Couceiro JN, Kelm S, Baum LG, Krauss S, Castrucci MR, Donatelli I, Kida H, Paulson JC, Webster RG, Kawaoka Y. Molecular basis for the generation in pigs of influenza A viruses with pandemic potential. J Virol. 1998;72:7367–7373. doi: 10.1128/jvi.72.9.7367-7373.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jayaraman A, Chandrasekaran A, Viswanathan K, Raman R, Fox JG, Sasise-kharan R. Decoding the distribution of glycan receptors for human-adapted influenza A viruses in ferret respiratory tract. PloS One. 2012;7:e27517. doi: 10.1371/journal.pone.0027517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeisy-Scott V, Kim JH, Davis WG, Cao W, Katz JM, Sambhara S. TLR7 recognition is dispensable for influenza virus A infection but important for the induction of hemagglutinin-specific antibodies in response to the 2009 pandemic split vaccine in mice. J Virol. 2012;86:10988–10998. doi: 10.1128/JVI.01064-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keitel WA, Campbell JD, Treanor JJ, Walter EB, Patel SM, He F, Noah DL, Hill H. Safety and immunogenicity of an inactivated influenza A/H5N1 vaccine given with or without aluminum hydroxide to healthy adults: results of a phase I–II randomized clinical trial. J Infect Dis. 2008;198:1309–1316. doi: 10.1086/592172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koopmans M, Wilbrink B, Conyn M, Natrop G, van der Nat H, Vennema H, Meijer A, van Steenbergen J, Fouchier R, Osterhaus A, Bosman A. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet. 2004;363:587–593. doi: 10.1016/S0140-6736(04)15589-X. [DOI] [PubMed] [Google Scholar]
- Lakdawala SS, Shih AR, Jayaraman A, Lamirande EW, Moore I, Paskel M, Sasisekharan R, Subbarao K. Receptor specificity does not affect replication or virulence of the 2009 pandemic H1N1 influenza virus in mice and ferrets. Virology. 2013;446:349–356. doi: 10.1016/j.virol.2013.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lindemann M, Witzke O, Lutkes P, Fiedler M, Kreuzfelder E, Philipp T, Roggendorf M, Grosse-Wilde H. ELISpot assay as a sensitive tool to detect cellular immunity following influenza vaccination in kidney transplant recipients. Clin Immunol. 2006;120:342–348. doi: 10.1016/j.clim.2006.03.002. [DOI] [PubMed] [Google Scholar]
- Londrigan SL, Turville SG, Tate MD, Deng YM, Brooks AG, Reading PC. N-linked glycosylation facilitates sialic acid-independent attachment and entry of influenza A viruses into cells expressing DC-SIGN or L-SIGN. J Virol. 2011;85:2990–3000. doi: 10.1128/JVI.01705-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mozdzanowska K, Furchner M, Washko G, Mozdzanowski J, Gerhard W. A pulmonary influenza virus infection in SCID mice can be cured by treatment with hemagglutinin-specific antibodies that display very low virus-neutralizing activity in vitro. J Virol. 1997;71:4347–4355. doi: 10.1128/jvi.71.6.4347-4355.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicholls JM, Chan MC, Chan WY, Wong HK, Cheung CY, Kwong DL, Wong MP, Chui WH, Poon LL, Tsao SW, Guan Y, Peiris JS. Tropism of avian influenza A (H5N1) in the upper and lower respiratory tract. Nat Med. 2007;13:147–149. doi: 10.1038/nm1529. [DOI] [PubMed] [Google Scholar]
- Pappas C, Viswanathan K, Chandrasekaran A, Raman R, Katz JM, Sasisekharan R, Tumpey TM. Receptor specificity and transmission of H2N2 subtype viruses isolated from the pandemic of 1957. PloS One. 2010;5:e11158. doi: 10.1371/journal.pone.0011158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patel SM, Atmar RL, El Sahly HM, Guo K, Hill H, Keitel WA. Direct comparison of an inactivated subvirion influenza A virus subtype H5N1 vaccine administered by the intradermal and intramuscular routes. J Infect Dis. 2012;206:1069–1077. doi: 10.1093/infdis/jis402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qi L, Kash JC, Dugan VG, Wang R, Jin G, Cunningham RE, Taubenberger JK. Role of sialic acid binding specificity of the 1918 influenza virus hemagglutinin protein in virulence and pathogenesis for mice. J Virol. 2009;83:3754–3761. doi: 10.1128/JVI.02596-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ramos I, Bernal-Rubio D, Durham N, Belicha-Villanueva A, Lowen AC, Steel J, Fernandez-Sesma A. Effects of receptor binding specificity of avian influenza virus on the human innate immune response. J Virol. 2011;85:4421–4431. doi: 10.1128/JVI.02356-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reading PC, Miller JL, Anders EM. Involvement of the mannose receptor in infection of macrophages by influenza virus. J Virol. 2000;74:5190–5197. doi: 10.1128/jvi.74.11.5190-5197.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reed LJ, M H. A simple method of estimating fifty per cent endpoint. Am J Hyg. 1938;27:5. [Google Scholar]
- Rogers GN, Paulson JC. Receptor determinants of human and animal influenza virus isolates: differences in receptor specificity of the H3 hemagglu-tinin based on species of origin. Virology. 1983;127:361–373. doi: 10.1016/0042-6822(83)90150-2. [DOI] [PubMed] [Google Scholar]
- Shaw ML, Stone KL, Colangelo CM, Gulcicek EE, Palese P. Cellular proteins in influenza virus particles. PLoS Pathog. 2008;4:e1000085. doi: 10.1371/journal.ppat.1000085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shinya K, Ebina M, Yamada S, Ono M, Kasai N, Kawaoka Y. Avian flu: influenza virus receptors in the human airway. Nat. 2006;440:435–436. doi: 10.1038/440435a. [DOI] [PubMed] [Google Scholar]
- Skehel JJ, Wiley DC. Receptor binding and membrane fusion in virus entry: the influenza hemagglutinin. Annu Rev Biochem. 2000;69:531–569. doi: 10.1146/annurev.biochem.69.1.531. [DOI] [PubMed] [Google Scholar]
- Subbarao K, Joseph T. Scientific barriers to developing vaccines against avian influenza viruses. Nat Rev Immunol. 2007;7:267–278. doi: 10.1038/nri2054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treanor JJ, Campbell JD, Zangwill KM, Rowe T, Wolff M. Safety and immunogenicity of an inactivated subvirion influenza A (H5N1) vaccine. N Engl J Med. 2006;354:1343–1351. doi: 10.1056/NEJMoa055778. [DOI] [PubMed] [Google Scholar]
- Tretyakova I, Pearce MB, Florese R, Tumpey TM, Pushko P. Intranasal vaccination with H5, H7 and H9 hemagglutinins co-localized in a virus-like particle protects ferrets from multiple avian influenza viruses. Virology. 2013;442:67–73. doi: 10.1016/j.virol.2013.03.027. [DOI] [PubMed] [Google Scholar]
- Tumpey TM, Maines TR, Van Hoeven N, Glaser L, Solorzano A, Pappas C, Cox NJ, Swayne DE, Palese P, Katz JM, Garcia-Sastre A. A two-amino acid change in the hemagglutinin of the 1918 influenza virus abolishes transmission. Science. 2007;315:655–659. doi: 10.1126/science.1136212. [DOI] [PubMed] [Google Scholar]
- Upham JP, Pickett D, Irimura T, Anders EM, Reading PC. Macrophage receptors for influenza A virus: role of the macrophage galactose-type lectin and mannose receptor in viral entry. J Virol. 2010;84:3730–3737. doi: 10.1128/JVI.02148-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Hoeven N, Pappas C, Belser JA, Maines TR, Zeng H, Garcia-Sastre A, Sasisekharan R, Katz JM, Tumpey TM. Human HA and polymerase subunit PB2 proteins confer transmission of an avian influenza virus through the air. Proc Natl Acad Sci U S A. 2009;106:3366–3371. doi: 10.1073/pnas.0813172106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang CC, Chen JR, Tseng YC, Hsu CH, Hung YF, Chen SW, Chen CM, Khoo KH, Cheng TJ, Cheng YS, Jan JT, Wu CY, Ma C, Wong CH. Glycans on influenza hemagglutinin affect receptor binding and immune response. Proc Natl Acad Sci U S A. 2009;106:18137–18142. doi: 10.1073/pnas.0909696106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang SF, Huang JC, Lee YM, Liu SJ, Chan YJ, Chau YP, Chong P, Chen YM. DC-SIGN mediates avian H5N1 influenza virus infection in cis and in trans. Biochem Biophys Res Commun. 2008;373:561–566. doi: 10.1016/j.bbrc.2008.06.078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu Q, Wang W, Cheng X, Zengel J, Jin H. Influenza H1N1 A/Solomon Island/3/06 virus receptor binding specificity correlates with virus pathogeni-city, antigenicity, and immunogenicity in ferrets. J Virol. 2010;84:4936–4945. doi: 10.1128/JVI.02489-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xu R, Krause JC, McBride R, Paulson JC, Crowe JE, Jr, Wilson IA. A recurring motif for antibody recognition of the receptor-binding site of influenza hemagglutinin. Nat Struct Mol Biol. 2013;20:363–370. doi: 10.1038/nsmb.2500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuan J, Zhang L, Kan X, Jiang L, Yang J, Guo Z, Ren Q. Origin and molecular characteristics of a novel 2013 avian influenza A(H6N1) virus causing human infection in Taiwan. Clin Infect Dis: Off Publ Infect Dis Soc Am. 2013;57:1367–1368. doi: 10.1093/cid/cit479. [DOI] [PubMed] [Google Scholar]
- Zeng H, Goldsmith CS, Maines TR, Belser JA, Gustin KM, Pekosz A, Zaki SR, Katz JM, Tumpey TM. Tropism and infectivity of influenza virus, including highly pathogenic avian H5N1 virus, in ferret tracheal differentiated primary epithelial cell cultures. J Virol. 2013;87:2597–2607. doi: 10.1128/JVI.02885-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang W, Shi Y, Qi J, Gao F, Li Q, Fan Z, Yan J, Gao GF. Molecular basis of the receptor binding specificity switch of the hemagglutinins from both the 1918 and 2009 pandemic influenza A viruses by a D225G substitution. J Virol. 2013;87:5949–5958. doi: 10.1128/JVI.00545-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhu FC, Wang H, Fang HH, Yang JG, Lin XJ, Liang XF, Zhang XF, Pan HX, Meng FY, Hu YM, Liu WD, Li CG, Li W, Zhang X, Hu JM, Peng WB, Yang BP, Xi P, Wang HQ, Zheng JS. A novel influenza A (H1N1) vaccine in various age groups. N Engl J Med. 2009;361:2414–2423. doi: 10.1056/NEJMoa0908535. [DOI] [PubMed] [Google Scholar]


